Abstract
Background:
Although child mortality is decreasing, more than half of all deaths in childhood occur in children with a life-limiting condition whose death may be expected.
Aim:
To assess trends in place of death and identify characteristics of children who died in the community after discharge from paediatric intensive care unit.
Design:
National data linkage study.
Setting/participants:
All children resident in England and Wales when admitted to a paediatric intensive care unit in the United Kingdom (1 January 2004 and 31 December 2014) were identified in the Paediatric Intensive Care Audit Network dataset. Linkage to death certificate data was available up to the end of 2014. Place of death was categorised as hospital (hospital or paediatric intensive care unit) or community (hospice, home or other) for multivariable logistic modelling.
Results:
The cohort consisted of 110,328 individuals. In all, 7709 deaths occurred after first discharge from paediatric intensive care unit. Among children dying, the percentage in-hospital at the time of death decreased from 83.8% in 2004 to 68.1% in 2014; 852 (0.8%) of children were discharged to palliative care. Children discharged to palliative care were eight times more likely to die in the community than children who died and had not been discharged to palliative care (odds ratio = 8.06 (95% confidence interval = 6.50–10.01)).
Conclusions:
The proportion of children dying in hospital is decreasing, but a large proportion of children dying after discharge from paediatric intensive care unit continue to die in hospital. The involvement of palliative care at the point of discharge has the potential to offer choice around place of care and death for these children and families.
Keywords: Paediatric intensive care unit, palliative care, place of death, hospice, child
What is already known about the topic?
Child mortality is decreasing, but more than half of all deaths in childhood are for children with a life-limiting condition whose death may be expected.
What this paper adds?
Although the proportion of children dying in the community after discharge from paediatric intensive care unit (PICU) has increased over time, most children continue to die in hospital or PICU.
Children who died after the involvement of palliative care were eight times more likely to die in the community rather than hospital than children who died and were not discharged to palliative care.
Implications for policy, practice or theory
Further provision of hospital-based specialist paediatric palliative care teams should be a priority to enable further integration of specialist palliative care services with other specialities, particularly Paediatric Critical Care.
Introduction
Child mortality has decreased in high-income countries including the United Kingdom over the last 30 years,1 but reductions in the United Kingdom have been less marked than similar countries.2 Mortality rates in paediatric intensive care units (PICUs) have also decreased over time,3 but some children do continue to die both in PICU4 and after discharge. It is estimated that more than 50% of deaths in children and young people in the United Kingdom are related to life-limiting conditions; therefore, their deaths may be expected5 and since the World Health Organization (WHO) definition of children’s palliative states that ‘It begins when illness is diagnosed, and continues regardless of whether or not a child receives treatment directed at the disease’,6 you may expect that discussions regarding choice of place of care/death may have occurred in this population.
The notion that an out-of-hospital death is better than an in-hospital death as a universally valued goal is becoming contentious in both children7,8 and adults,9 as the evidence on patient and families’ preference7 and importance of place of death is mixed. However, admissions to PICU are known to be stressful,10 and it has been known for some time that parents and siblings of children who died in hospital show more psychological symptoms11 and poorer adjustment12 than if their child or sibling had died at home. In particular, fathers showed higher levels of stress, depression and anxiety if their child had died in hospital compared to home.13 It should also be noted that within the National Health Service (NHS) in England, the proportion of people dying in hospital is currently used as a measure of quality.14 However, facilitating choice of place of care can only occur where resources are made available.15,16
In the United States, an increasing number of children with complex chronic conditions died at home rather than in hospital when comparing 1989–1993 to 1999–2003, but still more than 80% of these deaths occurred in the hospital.17
A previous descriptive study in the United Kingdom showed a difference in place of death in those discharged from PICU to palliative care and those not discharged to palliative care; but other clinical and demographic factors were not accounted for and no assessment of trends over time could be undertaken.18 A large multicentre study from the United States has showed that children with complex chronic conditions had longer lengths of stay in PICU and higher mortality than other children, but mortality data after discharge from PICU were not available.19
This study aimed to assess the trends in place of death for children who died after discharge from PICU and the clinical and demographic factors which were associated with death in the community rather than hospital.
Materials and methods
Dataset
Paediatric Intensive Care Audit Network data
All children admitted to a PICU in the United Kingdom between 1 January 2004 and 31 December 2014 were identified in the Paediatric Intensive Care Audit Network (PICANet) dataset.20 Only children who were resident in England and Wales were included in the cohort for analyses, as only their deaths would be recorded on the Office for National Statistics (ONS) death records. Linkage to the ONS death certificate dataset was undertaken by the Health and Social Care Information Centre, using their standard algorithm which uses NHS number, date of birth, sex and postcode. These data were available with a censor date of 1 November 2015, but due to the delays that can occur in registering deaths, only data up to the end of 2014 were included in these analyses.
Clinical variables
Clinical diagnoses for each admission were coded using Clinical Terms 3 (The Read Codes) which were aggregated into 12 primary diagnostic groups.21
The Paediatric Index of Mortality (version 2; PIM2) is used within UK PICUs to assess severity of illness at the point of admission and therefore the risk of mortality in PICU. It is based on physiological measurements in the first hour of admission, specific interventions and diagnoses.22 PIM2 used in this study was recalibrated coefficients calculated using admission data submitted to PICANet for the years 2011–2013.3 PIM2 was categorised into five categories of risk <1%, 1%–<5%, 5%–<15%, 15%–<30% and 30%+.
The number of PICU admissions was categorised as single admission, two admissions, three admissions and four or more admissions.
PICANet defined discharge for palliative care as ‘withdrawal of care at the current level if it is deemed that the admission can no longer benefit’. This variable identifies when a child was discharged from a PICU to a palliative care area.21 In this study, an individual patient was assigned as discharged for palliative care if they had been discharged for palliative care after any PICU admission.
Death data were obtained from the ONS death certificate system.23 Date of death and place of death data were used in these analyses. Place of death was categorised into PICU, hospital (excluding PICU), home, hospice or other based on the recorded address of death.
Demographic variables
Age at admission to PICU was categorised as <1 year, 1–4 years, 5–10 years, 11–15 years and ⩾16 years. Sex was included in the analysis only where it was non-ambiguous (male or female). An Index of Multiple Deprivation (2010; IMD)24 category was assigned to each individual based upon their Lower Super Output Area (LSOA) of residence. An LSOA is a census geographical area built up of Output Areas. There are 34,753 LSOAs (2011 Census) in England with a population of 1000–3000 per LSOA.25 These data were split into five categories for analyses with category 1 being the least deprived.
The ethnicity variable in PICANet is incomplete therefore South Asian ethnicity, the commonest ethnic minority group in England,26 was determined using two South Asian names analysis programs. These programs, Nam Pehchan27,28 and the South Asian Names and Group Recognition Algorithm,29 classified individual children as South Asian (Pakistani, Indian or Bangladeshi) or not. The results from these programs were corrected manually for known misclassification errors.30
Statistical analyses
Descriptive statistics were undertaken overall and by palliative care discharge status. Differences between groups were assessed by chi-squared or t-test.
Random effects logistic regression was undertaken to account for inter PICU variation in the outcome. A binary place of death variable was the dependent variable: community (home, hospice or other) or hospital (PICU and Hospital). Apart from the palliative care variable, all data in the model pertained to the last PICU admission prior to death for each individual. Variables were included in the model in a forced entry method with variables retained if p < 0.05 or they improved the model fit assessed using the Bayesian information criterion (BIC).
All analyses were carried out using STATA version 13, and all tests of statistical significance were at p ⩽ 0.05.
Ethical approval
Collection of personally identifiable data has been approved by the Patient Information Advisory Group (now the NHS Health Research Authority Confidentiality Advisory Group; see http://www.hra.nhs.uk/documents/2015/12/piag-register-8.xls), and ethics approval was granted by the Trent Medical Research Ethics Committee (ref. 05/MRE04/17 +5).
Results
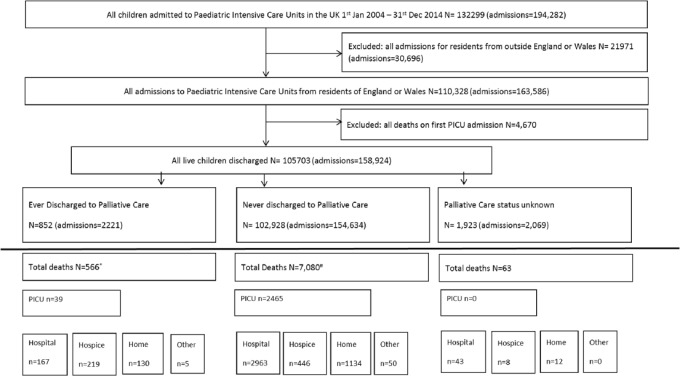
The cohort consisted of 110,328 individuals with 163,586 PICU admissions (Figure 1). A total of 4670 deaths occurred in PICU on first admission and were not included in the analyses. In all, 7709 deaths occurred after discharge from PICU and form the cohort for this study (Table 1). Of the individuals, 37.4% (n = 2885) had a single PICU admission, 30.2% (n = 2327) had two PICU admissions, 13.8% (n = 1060) had three PICU admissions and 18.6% (n = 1437) had more than four PICU admissions.
Figure 1.
Study flowchart.
Table 1.
Descriptive statistics of children resident in England and Wales who died after PICU discharge (2004–2014).
| Variables | Total deaths excluding first PICUa | Palliative | Never | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 7709 | 566 | 7080 | ||||
| Gender | ||||||
| Male | 4225 | 54.8 | 311 | 54.9 | 3877 | 54.8 |
| Female | 3480 | 45.1 | 253 | 44.7 | 3201 | 45.2 |
| Missing | 4 | <0.1 | 2 | 0.4 | 2 | <0.1 |
| Age category | ||||||
| <1 year | 3320 | 43.1 | 237 | 41.9 | 3061 | 43.2 |
| 1–4 years | 1868 | 24.2 | 137 | 23.7 | 1711 | 24.2 |
| 5–10 years | 1063 | 13.8 | 80 | 14.1 | 979 | 13.8 |
| 11–15 years | 1087 | 14.1 | 88 | 15.5 | 985 | 13.9 |
| 16+ | 371 | 4.8 | 24 | 4.2 | 344 | 4.9 |
| Diagnostic groupb | ||||||
| Neurological | 957 | 12.4 | 115 | 20.3 | 833 | 11.8 |
| Cardiac | 1821 | 23.6 | 73 | 12.9 | 1735 | 24.5 |
| Respiratory | 2092 | 27.1 | 207 | 36.6 | 1869 | 26.4 |
| Oncology | 794 | 10.3 | 52 | 9.2 | 728 | 10.3 |
| Infection | 452 | 5.9 | 37 | 6.5 | 412 | 5.8 |
| Musculoskeletal | 200 | 2.6 | 9 | 1.6 | 191 | 2.7 |
| Gastrointestinal | 473 | 6.1 | 18 | 3.2 | 452 | 6.4 |
| Other | 366 | 4.7 | 14 | 2.5 | 351 | 5.0 |
| Blood and lymph | 86 | 1.1 | <5 | <0.9 | 81 | 1.1 |
| Trauma | 40 | 0.5 | <5 | <0.9 | 39 | 0.6 |
| Endocrine/metabolic | 322 | 4.2 | 32 | 5.7 | 290 | 4.1 |
| Multisystem | 16 | 0.2 | <5 | <0.9 | 13 | 0.2 |
| Body wall and cavities | 90 | 1.2 | <5 | <0.9 | 86 | 1.2 |
| Risk of mortality (PIM2)b | ||||||
| <1% | 1233 | 16.0 | 23 | 4.1 | 1191 | 16.8 |
| 1–<5% | 3415 | 44.3 | 254 | 44.9 | 3130 | 44.2 |
| 5–<15% | 1996 | 25.9 | 195 | 34.5 | 1792 | 25.3 |
| 15–<30% | 618 | 8.0 | 61 | 10.8 | 556 | 7.9 |
| 30%+ | 447 | 5.8 | 33 | 5.8 | 411 | 5.8 |
| South Asian | ||||||
| No | 6427 | 83.4 | 475 | 83.9 | 5894 | 83.2 |
| Yes | 1282 | 16.6 | 91 | 16.1 | 1186 | 16.8 |
| Length of stay (days) | ||||||
| Mean | 8.7 | 12.1 | 8.5 | |||
| SD | 19.2 | 40.9 | 16.4 | |||
| Median | 3.4 | 6.2 | 3.1 | |||
| IQR | 1.0–9.4 | 2.1–13.9 | 1.0–9.1 | |||
| Missing | 2 | 0 | 2 | |||
| Year of death | ||||||
| 2004 | 437 | 5.7 | 39 | 6.9 | 394 | 5.6 |
| 2005 | 639 | 8.3 | 61 | 10.8 | 577 | 8.1 |
| 2006 | 696 | 9.0 | 39 | 6.9 | 655 | 9.3 |
| 2007 | 742 | 9.6 | 46 | 8.1 | 692 | 9.8 |
| 2008 | 729 | 9.5 | 21 | 3.7 | 702 | 9.9 |
| 2009 | 761 | 9.9 | 57 | 10.1 | 699 | 9.9 |
| 2010 | 782 | 10.1 | 56 | 9.9 | 718 | 10.1 |
| 2011 | 718 | 9.3 | 47 | 8.3 | 656 | 9.3 |
| 2012 | 775 | 10.1 | 66 | 11.7 | 698 | 9.9 |
| 2013 | 728 | 9.4 | 66 | 11.7 | 659 | 9.3 |
| 2014 | 702 | 9.1 | 68 | 12.0 | 630 | 8.9 |
| Place of deathb | ||||||
| Hospital | 3173 | 41.2 | 167 | 29.5 | 2963 | 41.9 |
| Hospice | 673 | 8.7 | 219 | 38.7 | 446 | 6.3 |
| Home | 1276 | 16.6 | 130 | 23.0 | 1134 | 16.0 |
| Other | 55 | 0.7 | 5 | 0.9 | 50 | 0.7 |
| PICU | 2504 | 32.5 | 39 | 6.9 | 2465 | 34.8 |
| Not known | 28 | 0.4 | 6 | 1.1 | 22 | 0.3 |
| No. of PICU admissionsb | ||||||
| One admission | 2885 | 37.4 | 263 | 46.5 | 2569 | 36.3 |
| Two admissions | 2327 | 30.2 | 123 | 21.7 | 2197 | 31.0 |
| Three admissions | 1060 | 13.8 | 69 | 12.2 | 990 | 14.0 |
| Four and more admissions | 1437 | 18.6 | 111 | 19.6 | 1324 | 18.7 |
| Deprivation (IMD 2010) score | ||||||
| Category 1 (least deprived) | 927 | 12.0 | 66 | 11.7 | 861 | 12.2 |
| Category 2 | 955 | 12.4 | 72 | 12.7 | 883 | 12.5 |
| Category 3 | 1253 | 16.3 | 100 | 17.7 | 1153 | 16.3 |
| Category 4 | 1696 | 22.0 | 118 | 20.8 | 1578 | 22.3 |
| Category 5 (most deprived) | 2499 | 32.4 | 185 | 32.3 | 2314 | 32.7 |
| Missing | 379 | 4.9 | 25 | 4.4 | 291 | 4.1 |
IMD2010: Index of Multiple Deprivation 2010; PICU: paediatric intensive care unit; PIM2: Paediatric Index of Mortality (version 2); SD: standard deviation; IQR: interquartile range.
Palliative care status was missing for 63 individuals who had died; therefore, palliative and never columns do not total 7709.
Chi2 results: p < 0.001 between palliative and non-palliative groups.
The numbers of children dying each year after discharge from PICU varied between 640 and 782, apart from the first year (2004) which had a lower number of deaths due to left censoring of the dataset.
Of the children admitted to PICU, 852 (0.8%) were discharged for palliative care, of which 566 (7.3% of all deaths) had died at the censor point. Therefore, only 7.4% of children who died had been referred for palliative care.
There were some statistically significant differences in clinical characteristics between those who died after being discharged for palliative care and those who died and who had not been discharged for palliative care (Table 1), but no significant differences in gender, age, ethnicity or deprivation scores.
A higher percentage of those in the palliative care group had a primary neurological (20.3% vs 11.8%) or respiratory (36.6% vs 26.4%) diagnoses, and a lower percentage had a cardiac diagnosis (12.9% vs 24.5%; chi2 = 113.4, p < 0.001).
The length of stay in PICU was higher in those from the palliative care group (median length of stay 6.2 days vs 3.1 days). Those children from the palliative care group were less likely to have more than one PICU admission (53.5% vs 63.7%, chi2 = 31.1, p < 0.001). A smaller percentage of the palliative care group had a <1% chance of mortality within PICU on their last PICU admission (4.1% vs 16.0%; chi2 = 76.4, p < 0.001).
Place of death differed significantly between the two groups with a higher percentage of those in the palliative care group dying at home (23% vs 16.0%) or hospice (38.7% vs 6.3%) and a lower percentage dying in a hospital ward (29.5% vs 41.9%) or PICU (6.9% vs 34.8%) (chi2 = 797.2, p < 0.001).
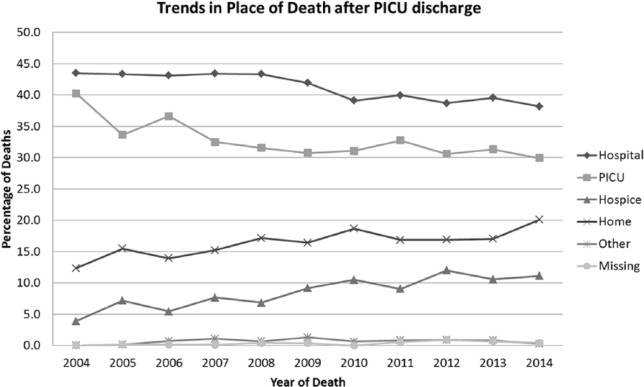
Place of death
Overall, 41.2% of the deaths occurred in hospital, 32.5% in PICU, 16.6% at home, 8.7% in hospice and 0.7% elsewhere. Deaths in hospital decreased from 43.5% in 2004 to 38.2% in 2014. Death in PICU decreased from 40.3% to 29.9%, while deaths in hospice rose from 3.9% to 11.1% and deaths at home rose from 12.4% to 20.1% (Figure 2) during the same time period.
Figure 2.
Trends in place of death.
Modelling
Table 2 shows the results of the random effects logistic modelling with community death (home, hospice or other) compared to hospital setting (hospital including PICU) as the outcome variable. All age groups were significantly more likely to die in the community rather than the hospital setting compared to the under 1 year age group. Children with neurological (odds ratio (OR) = 1.71 (95% confidence interval (CI) = 1.41–2.08)) or oncology diagnoses (OR = 3.30 (95% CI = 2.65–4.09)) were significantly more likely to die in the community than those with respiratory diagnoses. Conversely, children with cardiac (OR = 0.49 (95% CI = 0.39–0.61)) or musculoskeletal diagnoses (OR = 0.57 (95% CI = 0.38–0.84)) were significantly less likely to die in the community than those with respiratory diagnoses.
Table 2.
Random effects logistic regression with community death as dependent variable of children resident in England and Wales who died after PICU discharge (2004–2014).
| Variables | Odds ratio | p value | 95% CI | |
|---|---|---|---|---|
| Age category | ||||
| <1 year | REF | |||
| 1–4 years | 1.83 | <0.001 | 1.54 | 2.17 |
| 5–10 years | 2.46 | <0.001 | 2.02 | 2.99 |
| 11–15 years | 2.47 | <0.001 | 2.04 | 2.96 |
| 16+ | 1.77 | <0.001 | 1.34 | 2.34 |
| Sex | ||||
| Male | REF | |||
| Female | 0.90 | 0.09 | 0.79 | 1.02 |
| Diagnostic group | ||||
| Respiratory | REF | |||
| Neurological | 1.71 | <0.001 | 1.41 | 2.08 |
| Cardiac | 0.49 | <0.001 | 0.39 | 0.61 |
| Oncology | 3.30 | <0.001 | 2.65 | 4.09 |
| Infection | 0.98 | 0.90 | 0.74 | 1.31 |
| Musculoskeletal | 0.57 | 0.01 | 0.38 | 0.84 |
| Gastrointestinal | 0.77 | 0.07 | 0.58 | 1.02 |
| Other | 1.30 | 0.09 | 0.98 | 1.73 |
| Blood and lymph | 1.06 | 0.95 | 0.60 | 1.88 |
| Trauma | 0.46 | 0.09 | 0.19 | 1.13 |
| Endocrine/metabolic | 1.28 | 0.12 | 0.94 | 1.75 |
| Multisystem | 3.48 | 0.05 | 1.02 | 11.9 |
| Body wall and cavities | 0.66 | 0.25 | 0.33 | 1.34 |
| Risk of mortality (PIM2) | ||||
| <1% | REF | |||
| 1–<5% | 0.69 | <0.001 | 0.58 | 0.82 |
| 5–<15% | 0.44 | <0.001 | 0.36 | 0.54 |
| 15–<30% | 0.40 | <0.001 | 0.30 | 0.54 |
| 30%+ | 0.24 | <0.001 | 0.16 | 0.35 |
| Ever discharged to palliative care | ||||
| No | REF | |||
| Yes | 8.06 | <0.001 | 6.50 | 10.01 |
| Length of PICU stay (days) | 0.99 | 0.03 | 0.99 | 1.00 |
| Number of PICU admissions | ||||
| One admission | REF | |||
| Two admissions | 0.41 | <0.001 | 0.35 | 0.48 |
| Three admissions | 0.41 | <0.001 | 0.34 | 0.51 |
| Four and more admissions | 0.34 | <0.001 | 0.28 | 0.41 |
| South Asian ethnicity | ||||
| No | REF | |||
| Yes | 0.48 | <0.001 | 0.39 | 0.58 |
| Deprivation category (IMD2010) | 0.99 | <0.001 | 0.99 | 0.99 |
| Category 1 (least deprived) | REF | |||
| Category 2 | 0.87 | 0.22 | 0.69 | 1.09 |
| Category 3 | 0.81 | 0.06 | 0.65 | 1.01 |
| Category 4 | 0.80 | 0.04 | 0.65 | 0.99 |
| Category 5 (most deprived) | 0.63 | <0.001 | 0.51 | 0.77 |
| Year of death | 1.06 | <0.001 | 1.04 | 1.08 |
IMD2010: Index of Multiple Deprivation 2010; PICU: paediatric intensive care unit; PIM2: Paediatric Index of Mortality (version 2); CI: confidence interval.
n = 7303, Wald chi2 = 1227, p < 0.001, rho = 0.022, sigma = 0.27.
Children with a higher risk of mortality, calculated by the PIM2 score, were all significantly less likely to die in a community setting compared to those with the lower risk of mortality. Those with more than one PICU admission were also significantly less likely to die in the community than those who only had one PICU admission. Children discharged for palliative care were eight times more likely to die in the community (OR = 8.06 (95% CI = 6.50–10.01)).
Children from a South Asian background were significantly less likely to die outside the hospital than non-South Asian children (OR = 0.48 (95% CI = 0.39–0.58)). Children living in the two most deprived categories were significantly less likely to die outside the hospital than children living in the least deprived areas (category 4 OR = 0.80 (95% CI = 0.65–0.99) and category 5 (most deprived) OR = 0.63 (95% CI = 0.51–0.77)).
There was a significant trend over time of dying in the community with an increase of 6% per year (OR = 1.06 (95% CI = 1.04–1.08)). Interaction terms between palliative care status, length of stay, diagnostic group and number of PICU admissions were not retained within the model as they were not significant and did not improve the model fit.
The result of the sensitivity analyses excluding the deprivation variable in the random effects logistic model shows that the interpretation of the main variables of interest remains the same (data not shown).
Discussion
The proportion of children dying in hospital and PICU has decreased over the period of this study in England and Wales, but 68.1% of children who died after PICU admission still died in hospital in 2014. Discharge for palliative care had the largest effect on whether a child died in the community setting rather than hospital after a PICU admission, with children referred for palliative care having eight times the odds of dying in the community compared to children who had not been discharged for palliative care.
Children older than 1 year of age were more likely than the under 1 year age group to die in the community. The prevalence of life-limiting conditions in children is by far the highest in the under 1 year age group,31 and admission rates to PICU are also higher in the under 1 year age group. Overall mortality2 and within PICU mortality are also significantly higher in the under 1 year age group;3 therefore, they should be seen as a priority group for input from specialist palliative care services. Although choice of place of death should be available for neonates and infants, given the relatively well-developed palliative care services and established guidelines in the United Kingdom, it may not be offered.32
The underlying diagnoses had an effect on whether the child died in the community or hospital setting. Different diagnostic groups may have different disease trajectories and more reliance on services currently provided by hospitals, for example, cardiac and respiratory conditions. Children with an oncology diagnoses were 3.5 times more likely than children with respiratory diagnoses to die in the community. Children’s cancer services are configured differently than other children’s health services in the United Kingdom, and they are usually well provided with community care specialist nursing teams, which can be critical to enabling a death outside of the hospital setting. A recent paper has shown that consistently, since 1993, 40% of children who died from cancer in England died at home, but the children with haematological malignancies were more likely to die in hospital.33 More specialist resources may be required to care these children at home compared to other dying children, and their disease trajectories are often more unpredictable, but choice should still be facilitated where possible.
While it should not be assumed that all children and families, if given a choice, would choose for a child to die at home,7 if true choice was available then we should see a higher percentage of children dying in the community than was found in this study. More than 60% of these children who died had more than one PICU admission, and although not all of these deaths would have been expected, many would be, therefore opportunities for involving palliative care in the care of these children and families may have been missed. There are some examples in England of integration of palliative care and PICU services but there are also hospitals in England where hospital-based specialist paediatric palliative care services do not exist.34 Previous research with paediatric intensive care specialists has shown that there are mixed opinions on the role and usefulness of paediatric palliative care teams.35
Inequity in the place of death has been shown in this study with children from the most deprived areas in England and Wales being less likely than those in the least deprived areas to die in a non-hospital setting. A previous study from PICANet data showed that deprivation was not significantly associated with whether or not a child was discharged for palliative care;36 therefore, these inequities may also exist within place of death even when palliative care services are involved.
Children with a South Asian background were less likely to die outside the hospital setting than non-South Asian children. These differences in place of death by ethnic group are similar to a study from the United States which showed that Black and Hispanic children were 50% less likely to die at home than the White population.17 Previous work using the PICANet dataset showed that they were no less likely to be referred to palliative care but they were more likely to receive this care in hospital rather than in the community.36 This is a complex issue, and flexibility of services to provide culturally competent care is key and some children’s hospices have well-established reputations at engaging the South Asian community.37
It is important to note that high-quality palliative care should be available in all settings, so if a child and family wish to die in hospital, or an alternative setting is not possible, that they should still be offered access to specialist paediatric palliative care services.
Strengths/limitations
These analyses were undertaken on a national, mandatory dataset with full population coverage over an 11-year period. This dataset was enhanced to provide mortality data after discharge by linkage to official death record statistics. Place of death was derived from recorded address in these data, and in this study, in only 0.4% of cases was this unable to be assigned. Address of death is validated via postcodes.38 There are known delays to recording deaths of children particularly if coroners require to be notified. A total of 199 children who died in PICU (7.9% PICU deaths) did not have a matched ONS record. The majority of these were children who had died in the years 2012–2014. The analyses have been rerun only including children up to 2011 with no difference in the results.
The PICANet data are estimated as 99.9% complete, and the data are validated online including validation of the NHS number which is vital for linkage with other datasets.3
The definition of discharge for palliative care used within the PICANet dataset is quite restrictive: ‘withdrawal of care at the current level if it is deemed that the admission can no longer benefit’.21 As paediatric palliative care services care for children throughout their illness, not just at the end of life, some children may have been receiving palliative care but not recorded on the PICANet dataset. This narrow definition may also influence the decisions of PICU clinicians regarding referral to palliative care.
There were missing data on palliative care status for a small number of the children who had died (0.8%). Importantly, we had no objective information available on the relationship between individual PICU units and the availability of palliative care services in their catchment areas and no information on situations in which palliative care was discussed and a referral was not made.
The ONS death certificate data cover children who died in England and Wales. Therefore, if a child had moved to another country and subsequently died, we would not have their information. However, we expect those to be a very small number of children.
Conclusion
Over the last 11 years, the proportion of children dying in hospital in England is decreasing, but a large proportion of children dying after discharge from PICU continue to die in hospital. A very small percentage of these children who died had been referred to specialist palliative care. Involvement of palliative care before the point of discharge has the potential to offer choice around place of care and death for these children and families. Further provision of hospital-based specialist paediatric palliative care teams should be a priority to enable further integration of specialist palliative care services with other specialities, particularly Paediatric Critical Care.
Acknowledgments
The PICANet Audit is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit Programme (NCA). HQIP is led by a consortium of the Academy of Medical Royal Colleges, the Royal College of Nursing and National Voices. Its aim is to promote quality improvement and in particular to increase the impact that clinical audit has on healthcare quality in England and Wales. HQIP holds the contract to manage and develop the NCA Programme, comprising more than 30 clinical audits that cover care provided to people with a wide range of medical, surgical and mental health conditions. The PICANet Audit is funded by NHS England, the Welsh Government, NHS Lothian/National Service Division NHS Scotland, the Royal Belfast Hospital for Sick Children, The National Office of Clinical Audit (NOCA), Republic of Ireland and HCA Healthcare.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This paper is an independent research arising from a Postdoctoral Fellowship supported by the National Institute for Health Research. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. This study was funded by Research Trainees Coordinating Centre (Grant/Award Number: PDF-2013-06-001).
References
- 1. Hardelid P, Dattani N, Davey J, et al. Overview of child deaths in the four UK countries. Child Health Reviews – UK. London: Royal College of Paediatrics and Child Health, 2013. [Google Scholar]
- 2. Viner RM, Hargreaves DS, Coffey C, et al. Deaths in young people aged 0–24 years in the UK compared with the EU15+countries, 1970–2008: analysis of the WHO Mortality Database. Lancet 2014; 384: 880–892. [DOI] [PubMed] [Google Scholar]
- 3. PICANet. PICANet 2015 annual report. Leeds: PICANet, 2015. [Google Scholar]
- 4. Ramnarayan P, Craig F, Petros A, et al. Characteristics of deaths occurring in hospitalised children: changing trends. J Med Ethics 2007; 33: 255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sidebotham P, Fraser J, Fleming P, et al. Child death in high-income countries 2 Patterns of child death in England and Wales. Lancet 2014; 384: 904–914. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization. WHO definition of palliative care. Geneva: WHO, 1998. [Google Scholar]
- 7. Bluebond-Langner M, Beecham E, Candy B, et al. Preferred place of death for children and young people with life-limiting and life-threatening conditions: a systematic review of the literature and recommendations for future inquiry and policy. Palliative Med 2013; 27: 705–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bluebond-Langner M, Beecham E, Candy B, et al. Problems with preference and place of death for children too. BMJ 2015; 351: h6123. [DOI] [PubMed] [Google Scholar]
- 9. Pollock K. Is home always the best and preferred place of death? BMJ 2015; 351: h4855. [DOI] [PubMed] [Google Scholar]
- 10. Balluffi A, Kassam-Adams N, Kazak A, et al. Traumatic stress in parents of children admitted to the pediatric intensive care unit. Pediatr Crit Care Med 2004; 5: 547–553. [DOI] [PubMed] [Google Scholar]
- 11. Mulhern RK, Lauer ME, Hoffmann RG. Death of a child at home or in the hospital: subsequent psychological adjustment of the family. Pediatrics 1983; 71: 743–747. [PubMed] [Google Scholar]
- 12. Lauer ME, Mulhern RK, Wallskog JM, et al. A comparison study of parental adaptation following a child’s death at home or in the hospital. Pediatrics 1983; 71: 107–112. [PubMed] [Google Scholar]
- 13. Goodenough B, Drew D, Higgins S, et al. Bereavement outcomes for parents who lose a child to cancer: are place of death and sex of parent associated with differences in psychological functioning? Psychooncology 2004; 13: 779–791. [DOI] [PubMed] [Google Scholar]
- 14. NHS England. CCG improvement and assessment framework 2016/17. Leeds: NHS England, 2016. [Google Scholar]
- 15. Noyes J, Edwards RT, Hastings RP, et al. Evidence-based planning and costing palliative care services for children: novel multi-method epidemiological and economic exemplar. BMC Palliat Care 2013; 12: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Public Health England. Cost-effective commissioning of end of life care. London: Public Health England, 2017. [Google Scholar]
- 17. Feudtner C, Feinstein JA, Satchell M, et al. Shifting place of death among children with complex chronic conditions in the United States, 1989–2003. JAMA 2007; 297: 2725–2732. [DOI] [PubMed] [Google Scholar]
- 18. Fraser LK, Miller M, Draper ES, et al. Place of death and palliative care following discharge from paediatric intensive care units. Arch Dis Child 2011; 96: 1195–1198. [DOI] [PubMed] [Google Scholar]
- 19. Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Chronic conditions among children admitted to U.S. pediatric intensive care units: their prevalence and impact on risk for mortality and prolonged length of stay. Crit Care Med 2012; 40: 2196–2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. PICANeT. Paediatric intensive care audit. Leeds: PICANeT, 2015. [Google Scholar]
- 21. PICANet. PICANet admission dataset definitions manual version 5.0. Leeds: PICANeT, 2014. [Google Scholar]
- 22. Slater A, Shann F, Pearson G, et al. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med 2003; 29: 278–285. [DOI] [PubMed] [Google Scholar]
- 23. Health and Social Care Information Centre. Mortality data from the Office for National Statistics. Leeds: Health and Social Care Information Centre, 2016. [Google Scholar]
- 24. Department for Communities and Local Government. English indices of deprivation. London: Department for Communities and Local Government, 2010. [Google Scholar]
- 25. Office for National Statistics. Super output areas. Newport: Office for National Statistics, 2013. [Google Scholar]
- 26. Office for National Statistics. 2011 census analysis: ethnicity. Newport: Office for National Statistics, 2012. [Google Scholar]
- 27. Bradford Health Authority and City of Bradford Metropolitan District Council. Nam Pehchan computer program for the identification of names of south Asian ethnic origin. Bradford: Bradford Health Authority and City of Bradford Metropolitan District Council, 2002. [Google Scholar]
- 28. Cummins C, Winter H, Cheng KK, et al. An assessment of the Nam Pehchan computer program for the identification of names of south Asian ethnic origin. J Public Health Med 1999; 21: 401–406. [DOI] [PubMed] [Google Scholar]
- 29. Nanchahal K, Mangtani P, Alston M, et al. Development and validation of a computerized South Asian Names and Group Recognition Algorithm (SANGRA) for use in British health-related studies. J Public Health Med 2001; 23: 278–285. [DOI] [PubMed] [Google Scholar]
- 30. Parslow RC, Tasker RC, Draper ES, et al. Epidemiology of critically ill children in England and Wales: incidence, mortality, deprivation and ethnicity. Arch Dis Child 2009; 94: 210–215. [DOI] [PubMed] [Google Scholar]
- 31. Fraser LK, Miller M, Hain R, et al. Rising national prevalence of life-limiting conditions in children in England. Pediatrics 2012; 129: E923–E929. [DOI] [PubMed] [Google Scholar]
- 32. Craig F, Mancini A. Can we truly offer a choice of place of death in neonatal palliative care? Semin Fetal Neonatal Med 2013; 18: 93–98. [DOI] [PubMed] [Google Scholar]
- 33. Gao W, Verne J, Peacock J, et al. Place of death in children and young people with cancer and implications for end of life care: a population-based study in England, 1993–2014. BMC Cancer 2016; 16: 727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. NHS England. 2013/14 NHS standard contract for paediatric medicine: palliative care. Leeds: NHS England, 2013. [Google Scholar]
- 35. Jones PM, Carter BS. Pediatric palliative care: feedback from the pediatric intensivist community. Am J Hosp Palliat Care 2010; 27: 450–455. [DOI] [PubMed] [Google Scholar]
- 36. Fraser LK, Fleming T, Miller M, et al. Palliative care discharge from paediatric intensive care units in Great Britain. Palliat Med 2010; 24: 608–615. [DOI] [PubMed] [Google Scholar]
- 37. Taylor LK, Miller M, Joffe T, et al. Palliative care in Yorkshire, UK 1987–2008: survival and mortality in a hospice. Arch Dis Child 2010; 95: 89–93. [DOI] [PubMed] [Google Scholar]
- 38. Office for National Statistics. Mortality statistics, quality and methodology information. Newport: Office for National Statistics, 2016. [Google Scholar]