Abstract
Introduction:
Proximal humerus fractures are common in the elderly. The evaluation and management of these injuries is often controversial. The purpose of this study is to review recent evidence and provide updated recommendations for treating proximal humerus fractures in the elderly.
Methods:
A literature review of peer-reviewed publications related to the evaluation and management of proximal humerus fractures in the elderly was performed. There was a focus on randomized controlled trials and systematic reviews published within the last 5 years.
Results:
The incidence of proximal humerus fractures is increasing. It is a common osteoporotic fracture. Bone density is a predictor of reduction quality and can be readily assessed with anteroposterior views of the shoulder. Social independence is a predictor of outcome, whereas age is not. Many fractures are minimally displaced and respond acceptably to nonoperative management. Displaced and severe fractures are most frequently treated operatively with intramedullary nails, locking plates, percutaneous techniques, or arthroplasty.
Discussion:
Evidence from randomized controlled trials and systematic reviews is insufficient to recommend a treatment; however, most techniques have acceptable or good outcomes. Evaluation should include an assessment of the patient’s bone quality, social independence, and surgical risk factors. With internal fixation, special attention should be paid to medial comminution, varus angulation, and restoration of the calcar. With arthroplasty, attention should be paid to anatomic restoration of the tuberosities and proper placement of the prosthesis.
Conclusion:
A majority of minimally displaced fractures can be treated conservatively with early physical therapy. Treatment for displaced fractures should consider the patient’s level of independence, bone quality, and surgical risk factors. Fixation with percutaneous techniques, intramedullary nails, locking plates, and arthroplasty are all acceptable treatment options. There is no clear evidence-based treatment of choice, and the surgeon should consider their comfort level with various procedures during the decision-making process.
Keywords: upper extremity surgery, geriatric trauma, fragility fractures, trauma surgery, osteoporosis
Introduction
Proximal humerus fractures account for 6% of all fractures in the Western world.1 Following the distal radius and vertebra, it is the third most common osteoporotic fracture.2 Around 85% occur in people older than 50, and the incidence peaks in the 60- to 90-year-old age-group with a female to male ratio of 70:30.1(p. 691-697) A 2006 Finnish study estimated the incidence of fall-related proximal humerus fractures has tripled since 1970.3 Management of this common injury is often challenging and controversial.
Patients are most frequently treated nonoperatively, but some complex fractures require surgery. Recent surveys suggest shoulder arthroplasty and operative fixation are favored by a large number of surgeons over a range of fracture types in the elderly, especially by shoulder and elbow specialists.4,5 This practice is questionable.6-8 The purpose of this article is to review the evaluation and management of proximal humerus fractures in elderly patients.
Applied Anatomy
The glenohumeral joint is stabilized by the articular cartilage, labrum, ligaments, rotator cuff, and deltoid. Most humeral heads have a diameter between 4 and 5 cm, and the head is slightly offset medially and posteriorly in relation to the humeral shaft.9 The pectoralis major tendon inserts 5 to 6 cm from the top of the humeral head, which is a reliable tool for estimating prosthetic stem length in severe fractures without landmarks. Humeral shortening greater than 1 cm can impair deltoid function, whereas humeral lengthening and retroversion can impair tuberosity healing.10
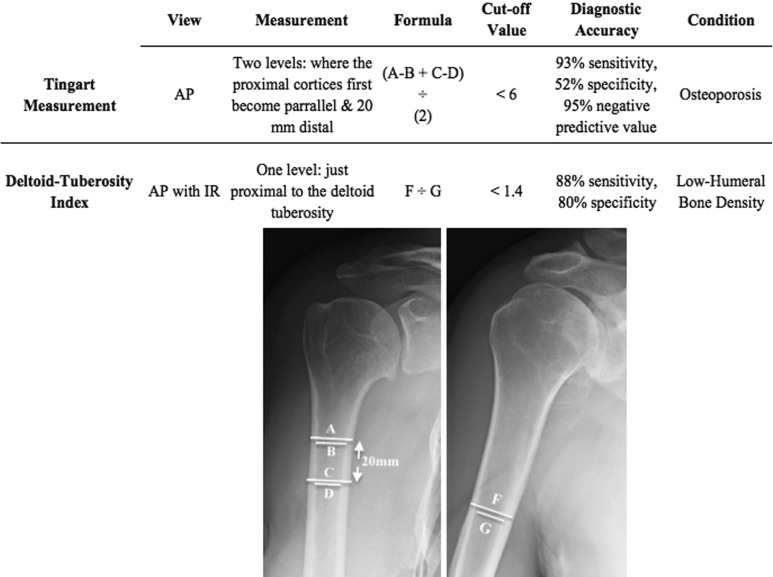
Tendons produce reliable deforming forces on bone fragments. The supraspinatus and teres minor insert on the greater tuberosity and produce a posterosuperior deformity. The subscapularis inserts on the lesser tuberosity and produces medial deformity. The pectoralis major inserts into the medial humeral shaft and deforms medially, while the deltoid inserts into the lateral humerus and deforms laterally (Figure 1).6
Figure 1.
Anteroposterior view of the shoulder demonstrating tendinous attachments to the proximal humerus and the associated direction of fragment displacement. GT denotes greater tuberosity; LT, lesser tuberosity.
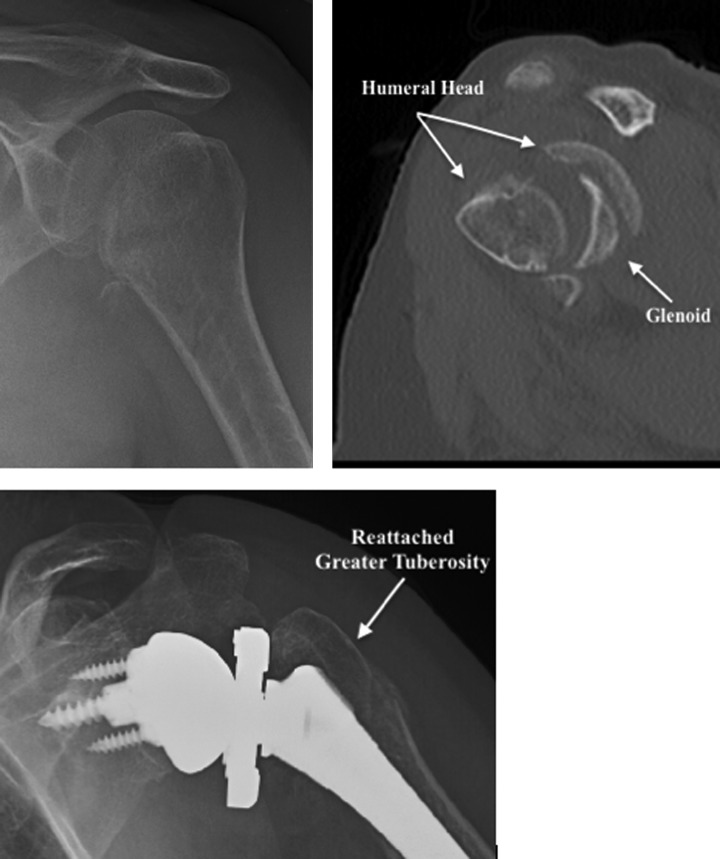
The proximal humeral blood supply is from the anterior and posterior humeral circumflex branches of the axillary artery, which are closely associated with the surgical neck and medial calcar (Figure 2). The arcuate artery is the terminal, ascending branch of the anterior humeral circumflex artery and enters the humeral head near the anatomic neck.6,11 Fractures with short calcar fragments (<8 mm), a disrupted medial hinge, and anatomic neck involvement are most prone to ischemia.12 Gross axillary artery injury is exceedingly rare; however, in cases of significant shoulder trauma with a loss of Doppler signals and an enlarging axillary mass, vascular surgery should be consulted and a computed tomography angiogram ordered. More than 90% of the reported cases occur in patients 50 years and older, possibly due to the loss of elasticity secondary to atherosclerosis.13
Figure 2.
Anteroposterior view of the shoulder illustrating the vascular supply to the proximal humerus. The arcuate artery is a branch of the anterior humeral circumflex artery and ascends along the intertubercular groove before entering the humeral head. The posterior humeral circumflex artery travels with the axillary nerve.
Some degree of electromyographically detectable axonal loss occurs in 67% of patients with low energy proximal humerus fractures. The most commonly injured nerves in descending order are the axillary, suprascapular, radial, musculocutaneous, median, and ulnar nerves. These are most commonly traction injuries that fully recover.14 During surgery, the axillary nerve can be difficult to identify, particularly in scarred shoulders. It is about 4.5 to 7 cm from the proximal humerus and 0.5 to 4 cm from the surgical neck,15 traveling through the quadrilateral space with the posterior humeral circumflex artery. Care should be taken with incisions greater than 5 cm in length distal to the acromion. With anterolateral plating, the axillary nerve is most frequently in danger when placing screws near the surgical neck through the middle segment of the plate.16
The Neer Classification
The Neer classification for proximal humerus fractures is based on 4 fracture parts: the greater tuberosity, the lesser tuberosity, the humeral head, and the humeral shaft. A full description of the classification and its subtypes can be found in an article by Carofino and Leopold.17 For practical purposes, fractures are discussed based on the number of Neer parts involved. A fragment is considered displaced if it is separated more than 1 cm or angulated more than 45°; however, there is no evidence-based indication for this definition of displacement. The Neer classification has shown moderate rater reliability. Outcomes and rates of rotator cuff injury correlate with the classification.18
Evaluation and General Considerations
The typical presentation of a proximal humerus fracture is an elderly female who falls and sustains a minimally displaced or 2-part fracture (Figure 3). Around 1 in 10 will present with an additional fracture.19 Important historical elements include the patient’s level of independence, functional demands, and any preexisting rotator cuff conditions. Evaluation should begin with inspection of the soft tissues and skin, as elderly patients are susceptible to poor wound healing. A full neurologic examination can be difficult following trauma, but function of the fingers, wrist, and elbow can often be evaluated. Axillary nerve innervation of the deltoid needs to be tested as reverse shoulder arthroplasty (RTSA) is a viable treatment option that requires an intact and innervated deltoid.
Figure 3.
Anteroposterior views of 3 shoulders demonstrating the most commonly encountered fracture patterns: minimally displaced (left) and surgical neck fractures (middle, right) with variable impaction and comminution.
True anteroposterior (AP), lateral, and axillary X-rays of the glenohumeral joint should be ordered. Computed tomography is recommended for complex fracture patterns or when fracture lines cannot be clearly visualized. Magnetic resonance imaging (MRI) may be useful for assessing rotator cuff integrity when considering nonoperative treatment. In a prospective study of 30 patients, nearly 40% of proximal humerus fractures were associated with rotator cuff tears.18 In another MRI cohort study of 76 patients with proximal humerus fractures, 22 had cuff tears at the time of injury, and 10 developed tears at 1 year. Functional loss correlated with tears at the time of injury.20
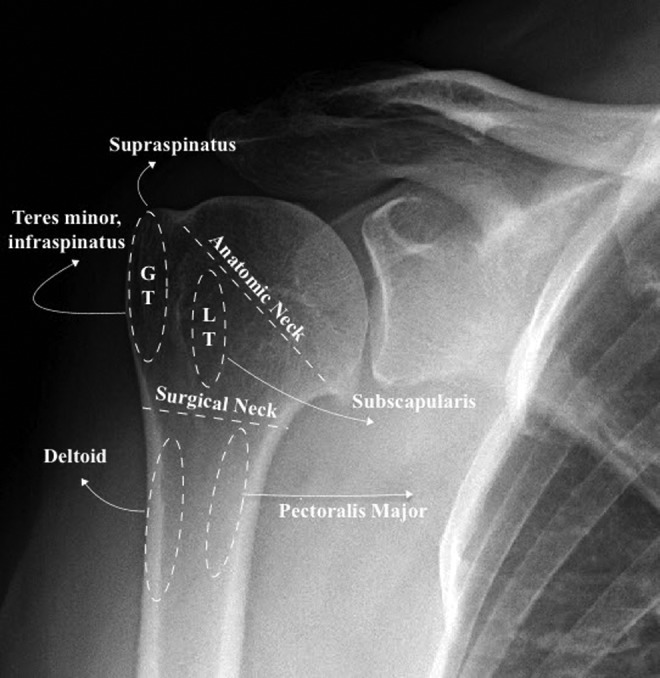
Bone density is a predictor of surgical reduction quality and screw cutout.21,22 Density can be assessed with cortical bone thickness measurements on AP views of the shoulder. Two techniques are detailed in Figure 4: the Tingart measurement23 and the deltoid tuberosity index.24 Bone quality and social independence can serve as indicators of physiologic age, which is more important than chronologic age when weighing treatment options. Several studies have shown no difference in outcomes between elderly patients and younger patients following surgical fixation of proximal humerus fractures.25-27 Further, a 1-year outcome study of 637 proximal humerus fractures showed that social independence, not age, was a predictor of outcome.19
Figure 4.
Anteroposterior views of the shoulder demonstrating the Tingart and DTI methods for measuring bone density. An explanation is provided in the table. DTI denotes deltoid tuberosity index.
Management
Treatment of proximal humerus fractures is controversial. A 2012 Cochrane review of 23 randomized controlled trials concluded there is insufficient evidence to provide reccomendations.7 There is significant heterogeneity among studies, so making conclusions is difficult. In general, minimally displaced fractures, poor surgical candidates, and low demand patients are treated conservatively. Displaced, comminuted, or angulated fractures occurring in good surgical candidates are treated with percutaneous techniques, intramedullary nailing, plating, or arthroplasty.
Minimally Displaced Fractures
Around 50% to 65% of all proximal humerus fractures are minimally displaced fractures of the greater tuberosity and/or surgical neck that respond well to nonoperative management.28,29(p) The shoulder should be placed in a sling followed by early physical therapy. Isometric, pendulum, or passive range of motion exercises should be started within a few days of injury. The sling can be worn until healing is evident, which usually occurs by 4 to 6 weeks. Around this time, active strengthening exercises can begin.30,31 Recently, a study by Clement et al included 211 minimally displaced proximal humerus fractures in patients aged 65 to 98. At 1 year, the mean Constant-Murley score was 68.8 (greater than 55 was considered an acceptable outcome).19
Two-Part Surgical Neck Fractures
Approximately 20% to 30% of proximal humerus fractures are 2-part surgical neck fractures.28,29 Many of these patients will respond acceptably to nonoperative management,7,19,32 which should be considered in osteoporotic patients with high physiological age, low demand, and minimal displacement. Surgery can be considered for fractures with significant displacement and patients with acceptable bone quality.
Percutaneous techniques
A retrospective 2015 study by Tamimi et al compared functional outcomes among conservative treatment, nailing, percutaneous wiring, and plating. Percutaneous wiring was associated with superior outcomes in elderly patients, with a mean Constant score of 68.7.33 Percutaneous wiring generally utilizes a starting point just above the deltoid insertion, where 2 threaded wires are directed proximally into the humeral head. Next, using a starting point on the greater tuberosity, 2 additional threaded wires are directed distally into the humeral shaft (Figure 5). Nonthreaded wires can be used to manipulate the fracture site prior to fixation with threaded wires. Specific techniques are described for valgus angulated fractures by Seyhan et al34 and varus angulated fractures by Eid et al.35 Although technically demanding, the results are excellent with Constant-Murley scores of 90 to 94 at 1 to 3 years of follow-up.
Figure 5.
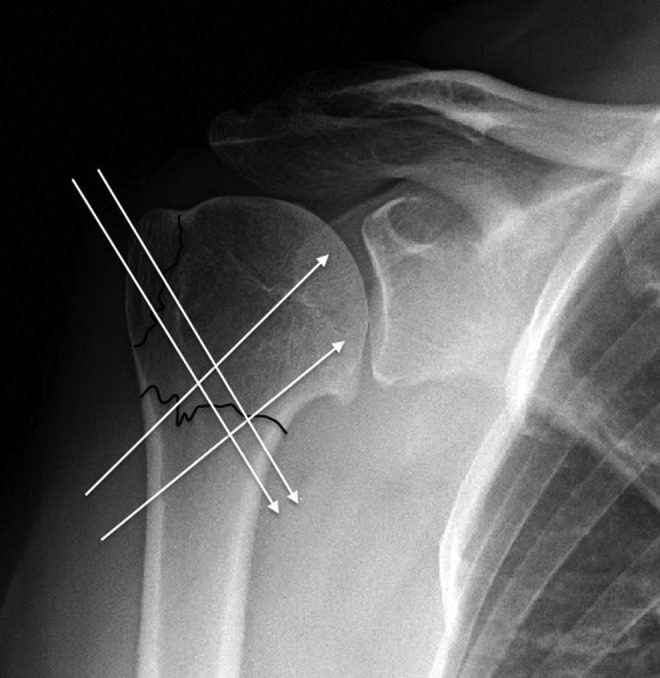
Illustration of common pin or wire trajectories utilized for percutaneous fixation or manipulation of 2- and 3-part fractures. Nonthreaded wires can be provisionally inserted and used to “joystick” fragments prior to placing threaded pins or a lateral plate.
The Humerus Block (Synthes, Oberdorf, Switzerland) is a relatively new percutaneous technique using Kirschner’s wires secured by a metal block. First, the block is screwed into the lateral humeral cortex. Using a guide device, 2 wires are then sent through the block at a 35° angle to the humeral shaft and a 25° angle to each other. Once the fracture is manipulated into a reduced position, the wires are fixed into the head fragment and then locked into the metal block. Additional fragments can be secured with screws. Results in elderly patients are good, with Constant scores around 80% to 90% of the contralateral arm; however, the device is bulky and needs to be removed with a second operation.36,37
Intramedullary nailing
Intramedullary nails can be used in surgical neck fractures, but the starting point is often compromised in 3-part fractures. The nail starting point is slightly medial to the greater tuberosity and cuff tendon insertions. It’s preferable to go through the supraspinatus muscle belly at the lateral edge of the articular surface instead of splitting the tendon.38 Intramedullary nails have demonstrated acceptable results with Constant-Murley scores ranging from 60 to 85.39-43 Straight nails are preferred over curved nails because they are less likely to violate the rotator cuff44 and have a lower reoperation rate with better functional outcomes.39-41
Locking plates
Locking plates are commonly used for surgical neck fractures, but they tend to be associated with high rates of reoperation ranging from 16% to 30%. This is primarily due to screw cutout.45,46 Biomechanical studies suggest plates have inferior failure rates compared to nails in both 2-part47 and 3-part fractures.48 Plate weakness is primarily on the medial side, and therefore, special attention should be paid to varus angulation and medial comminution. These factors are associated with reduction loss. Bone void fillers, divergent screws, and medial calcar support (Figure 6) may prevent some of the complications associated with using plates in osteoporotic bone.22,49
Figure 6.

Postoperative AP view of a 3-part fracture treated with a locking plate. Note the screw traversing the inferomedial humeral head, which is important for providing a medial support in the calcar region (dotted circle). With significant medial bone loss, graft material, fibular struts, or cement can be used to augment the construct. Tuberosities can be captured with screws or sutured to the plate. AP denotes anteroposterior.
Two-Part Tuberosity Fractures
Isolated greater tuberosity fractures account for 12% to 17% of proximal humerus fractures.28,50 Minimally displaced, isolated fractures of the greater tuberosity respond well to nonoperative management, but full recovery can take up to a year.51,52 Displaced fractures, particularly those with posterosuperior displacement, may benefit from fixation.53 Reduction techniques include screws or wires perpendicular to the fracture plane or suturing the fragment through bone tunnels (Figure 7). If the fragment is small or comminuted, suturing is recommended.
Figure 7.

Preoperative and postoperative X-rays illustrating a 2-part greater tuberosity fracture reduced with 2 lag screws. This technique works well for large fragments, but small fragments may be more stable with suture fixation.
Fractures of the lesser tuberosity rarely occur in isolation. They more commonly occur in association with a posterior dislocation (0.2% of fractures) or a surgical neck fracture (0.3% of fractures).29(p) When associated with a posterior dislocation, they can be closed reduced with immobilization in slight external rotation. Large, displaced fragments or fragments involving the articular surface warrant fixation (Figure 8).11 Screws can be used for fixation if the fragment is large. For smaller fragments, fixation with sutures is recommended.
Figure 8.
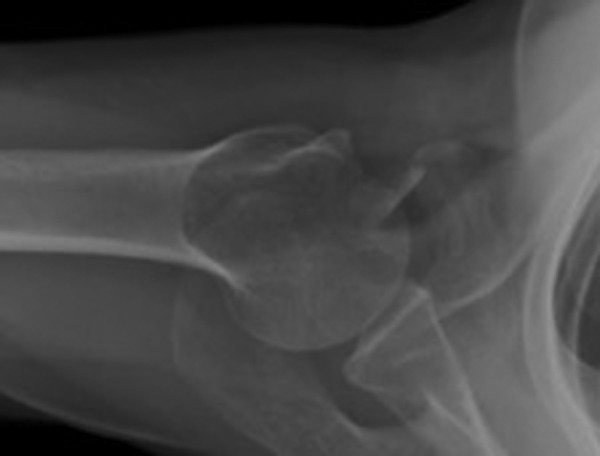
Axillary shoulder X-ray demonstrating a displaced fracture of the lesser tuberosity. This fragment is amenable to suture fixation.
Three- and Four-Part Fractures
Three- and four-part fractures account for 21% to 23% of proximal humerus fractures.29,50 Closed reduction with nonoperative management is an option; however, the functional results tend to be poor with Constant scores ranging from 47 to 62. Despite low functional scores, pain is uncommon and some patients are satisfied with the outcome of nonoperative treatment.19,54 At 5 years, the Proximal Fracture of the Humerus: Evaluation by Randomisation (PROFHER) trial has not found a significant difference in outcomes between operative and nonoperative treatment in 2-, 3-, or 4-part fractures.8 Although current evidence suggests nonoperative outcomes are satisfactory, a majority of surgeons perform locking plate reduction or arthroplasty in patients with severe fractures.4,5
Locking plates
Open reduction with plates can be considered in patients with good bone quality, but this may not be possible with complex fracture patterns. Some trials comparing plates to nonoperative treatment in 3- and 4-part fractures have shown no difference in outcome,55 and several studies have shown no difference between locking plates and hemiarthroplasty (HA).56,57 When plating complex fractures, suture fixation of the tuberosities and medial augmentation with cement, bone graft, and calcar screws is suggested (Figure 6). Fractures with valgus impaction have better outcomes than patients with varus impaction in both 3-and 4-part fractures,58-60 so attention to medial support is important. A randomized study comparing complex fractures treated with and without a medial support screw showed superior Constant scores (79 vs 70) and reduced failure rate (3.4% vs 23.1%) in the group that had a medial support screw placed.61
Plate fixation is thought to have a higher risk of avascular necrosis secondary to periosteal stripping. This may be obviated by newer minimally invasive designs, which have achieved Constant-Murley scores of 63 to 75.59,62 Several other plating advancements have been made with relatively lower complications than historically reported. A recent 1-year follow-up study of 54 patients treated with the S3 angular stable plate reported a mean Constant score of 75 with only 5 complications and no need for revision procedures.63 A 2-year follow-up study using the radiolucent carbon fiber-reinforced polyetheretherketone plate reported a mean constant score of 71.3.64
The use of a fibular graft strut to augment locking plate constructs has shown promising results in patients with osteoporosis. This technique involves intramedullary placement of a 6- to 8-cm segment of fibula, with 2 to 3 cm of the graft proximal to the surgical neck. Using screws, the intramedullary graft is “pushed” into position, reducing the medial cortex and providing calcar support.65 The endosteal strut can also be positioned for lateral augmentation. Using the fibular strut technique in elderly patients, Hinds et al demonstrated a mean Constant score of 82.7. This score was not significantly different from the score achieved in young patients.26 A recent systematic review of 4 fibular strut studies found that the rate of screw penetration and reoperation was only 3.7% and 4.4%,66 respectively, much lower than that reported with traditional plating techniques.45,46 Another recent study of 27 elderly patients by Hettrich et al found maintenance of reduction with no evidence of avascular necrosis and no reoperations at a mean 63.1-week follow-up.67
Arthroplasty
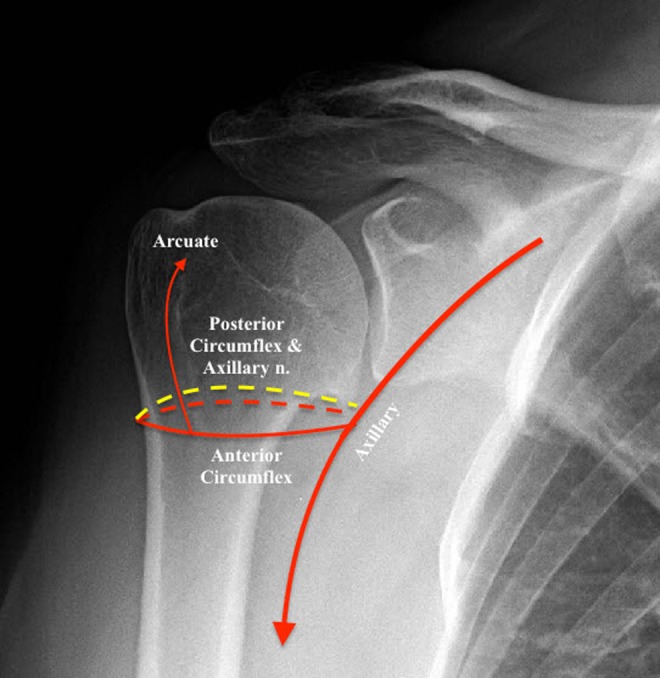
Hemiarthroplasty or RTSA is frequently used in situations of severe comminution, concern for humeral head ischemia, and poor bone quality. The prosthesis can be augmented with autograft prepared from excised bone. After placement of graft material, the greater and lesser tuberosity are sutured first around the implant and second to the humeral cortex (Figure 9). This is typically done with horizontal cerclage sutures placed through tunnels in the greater and lesser tuberosity. The horizontal sutures are wrapped around the prosthetic stem and tightened. Next, vertical sutures attach the tuberosities through bone tunnels in the anterolateral humeral cortex.68
Figure 9.
Preoperative and postoperative views of a patient sustaining a comminuted head splitting fracture. Top left: AP view of the shoulder illustrating a fracture through the anatomic neck. Top right: sagittal CT slice clearly demonstrating the humeral head in multiple pieces. Bottom: Postoperative images of a reverse shoulder prosthesis illustrating the reattached greater tuberosity. AP denotes anteroposterior; CT, computed tomography.
Hemiarthroplasty
Hemiarthroplasty was historically the treatment of choice for complex fractures, but results are mixed and dependent on tuberosity healing. Recent HA studies have failed to show benefits over nonoperative treatment.69,70 A systematic review of 808 patients revealed a mean Constant score of 57 with significant functional limitations (106° elevation and 92° abduction) but few reports of pain.71 The technique is technically challenging and requires a functional rotator cuff with good reduction of the tuberosities. Excessive lengthening and retroversion are associated with poor outcomes, so attention to humeral lengthening and head retroversion are important. Boileau et al suggest the worst combination is an excessively proud, retroverted prosthesis with a greater tuberosity attached too inferiorly.72
Reverse total shoulder arthroplasty
Results from RTSA are promising. A 2013 systematic review concluded RTSA outcomes are superior to HA outcomes,73 whereas an early 2014 systematic review found improved forward flexion in RTSA but decreased external rotation.74 More recent nonrandomized75,76 and randomized77 trials have demonstrated superiority of the reverse prosthesis, with Constant scores 12 to 14 points higher than HA. Reverse arthroplasty can be valuable as both a primary procedure and as a secondary procedure for failed open reductions. Outcomes from primary procedures have been superior to revision cases.78 Constant scores range from 44 to 67 with forward elevation between 97° and 138°.79-84 A recent 2016 study by Grubhofer et al included 51 patients with 3 years of follow-up who demonstrated Constant scores at 86% of the contralateral shoulder.85 Postoperative scapular notching and component loosening remain an issue with unknown clinical significance,79,82,86 but there is evidence to suggest it is associated with base plate loosening and poor outcomes. Notching can be prevented by proper placement of the glenoid component.87,88
Conclusion
Proximal humerus fractures in the elderly are common. A majority of minimally displaced fractures can be treated conservatively with early physical therapy. Treatment for displaced fractures should consider the patient’s level of independence, bone quality, and surgical risk factors. Fixation with percutaneous techniques, intramedullary nails, locking plates, and arthroplasty are all acceptable treatment options. With internal fixation, special attention should be paid to medial comminution, varus angulation, and restoration of the calcar. With arthroplasty, attention should be paid to anatomic restoration of the tuberosities and proper placement of the prosthesis. There is no clear evidence-based treatment of choice, and the surgeon should consider their comfort level with various procedures during the decision-making process.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi:10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2. Calvo E, Morcillo D, Foruria AM, Redondo-Santamaría E, Osorio-Picorne F, Caeiro JR. Nondisplaced proximal humeral fractures: high incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J Shoulder Elbow Surg. 2011;20(5):795–801. doi:10.1016/j.jse.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 3. Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop. 2006;442:87–92. [DOI] [PubMed] [Google Scholar]
- 4. Savin DD, Zamfirova I, Iannotti J, Goldberg BA, Youderian AR. Survey study suggests that reverse total shoulder arthroplasty is becoming the treatment of choice for four-part fractures of the humeral head in the elderly. Int Orthop. 2016;40(9):1919–1925. doi:10.1007/s00264-016-3227-y. [DOI] [PubMed] [Google Scholar]
- 5. Okike K, Lee OC, Makanji H, Harris MB, Vrahas MS. Factors associated with the decision for operative versus non-operative treatment of displaced proximal humerus fractures in the elderly. Injury. 2013;44(4):448–455. doi:10.1016/j.injury.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 6. McLaurin TM. Proximal humerus fractures in the elderly are we operating on too many? Bull Hosp Jt Dis N Y N. 2004;62(1-2):24–32. [PubMed] [Google Scholar]
- 7. Handoll HHG, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2012;12:CD000434 doi:10.1002/14651858.CD000434.pub3. [DOI] [PubMed] [Google Scholar]
- 8. Handoll HH, Keding A, Corbacho B, Brealey SD, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J. 2017;99-B(3):383–392. doi:10.1302/0301-620X.99B3.BJJ-2016-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boileau P, Walch G. The three-dimensional geometry of the proximal humerus. J Bone Joint Surg Br. 1997;79-B(5):857–865. [DOI] [PubMed] [Google Scholar]
- 10. Murachovsky J, Ikemoto RY, Nascimento LGP, Fujiki EN, Milani C, Warner JJP. Pectoralis major tendon reference (PMT): a new method for accurate restoration of humeral length with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2006;15(6):675–678. doi:10.1016/j.jse.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 11. Rockwood CA, ed. The Shoulder. 4th ed Philadelphia, PA: Saunders/Elsevier; 2009. [Google Scholar]
- 12. Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13(4):427–433. doi:10.1016/S1058274604000795. [DOI] [PubMed] [Google Scholar]
- 13. Thorsness R, English C, Gross J, Tyler W, Voloshin I, Gorczyca J. Proximal humerus fractures with associated axillary artery injury. J Orthop Trauma. 2014;28(11):659–663. doi:10.1097/BOT.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 14. Visser CP, Coene LN, Brand R, Tavy DL. Nerve lesions in proximal humeral fractures. J Shoulder Elbow Surg. 2001;10(5):421–427. doi:10.1067/mse.2001.118002. [DOI] [PubMed] [Google Scholar]
- 15. Bono CM, Grossman MG, Hochwald N, Tornetta P. Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop. 2000;(373):259–264. [PubMed] [Google Scholar]
- 16. Ninck J, Heck S, Gick S, Koebke J, Pennig D, Dargel J. Treatment of proximal humerus fractures: relative position of different locking plates to the axillary nerve. Unfallchirurg. 2013;116(11):1000–1005. doi:10.1007/s00113-012-2242-8. [DOI] [PubMed] [Google Scholar]
- 17. Carofino BC, Leopold SS. Classifications in brief: the Neer classification for proximal humerus fractures. Clin Orthop. 2013;471(1):39–43. doi:10.1007/s11999-012-2454-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gallo RA, Sciulli R, Daffner RH, Altman DT, Altman GT. Defining the relationship between rotator cuff injury and proximal humerus fractures. Clin Orthop. 2007;458:70–77. doi:10.1097/BLO.0b013e31803bb400. [DOI] [PubMed] [Google Scholar]
- 19. Clement ND, Duckworth AD, McQueen MM, Court-Brown CM. The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Joint J. 2014;96-B(7):970–977. doi:10.1302/0301-620X.96B7.32894. [DOI] [PubMed] [Google Scholar]
- 20. Fjalestad T, Hole MØ, Blücher J, Hovden IAH, Stiris MG, Strømsøe K. Rotator cuff tears in proximal humeral fractures: an MRI cohort study in 76 patients. Arch Orthop Trauma Surg. 2010;130(5):575–581. doi:10.1007/s00402-009-0953-2. [DOI] [PubMed] [Google Scholar]
- 21. Spross C, Zeledon R, Zdravkovic V, Jost B. How bone quality may influence intraoperative and early postoperative problems after angular stable open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2017;26(9):1566–1572. doi:10.1016/j.jse.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 22. Jung S-W, Shim S-B, Kim H-M, Lee J-H, Lim H-S. Factors that influence reduction loss in proximal humerus fracture surgery. J Orthop Trauma. 2015;29(6):276–282. doi:10.1097/BOT.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 23. Mather J, MacDermid JC, Faber KJ, Athwal GS. Proximal humerus cortical bone thickness correlates with bone mineral density and can clinically rule out osteoporosis. J Shoulder Elbow Surg. 2013;22(6):732–738. doi:10.1016/j.jse.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 24. Spross C, Kaestle N, Benninger E, et al. Deltoid tuberosity index: a simple radiographic tool to assess local bone quality in proximal humerus fractures. Clin Orthop. 2015;473(9):3038–3045. doi:10.1007/s11999-015-4322-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Grawe B, Le T, Lee T, Wyrick J. Open reduction and internal fixation (ORIF) of complex 3- and 4-part fractures of the proximal humerus: does age really matter? Geriatr Orthop Surg Rehabil. 2012;3(1):27–32. doi:10.1177/2151458511430662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hinds RM, Garner MR, Tran WH, Lazaro LE, Dines JS, Lorich DG. Geriatric proximal humeral fracture patients show similar clinical outcomes to non-geriatric patients after osteosynthesis with endosteal fibular strut allograft augmentation. J Shoulder Elbow Surg. 2015;24(6):889–896. doi:10.1016/j.jse.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 27. Goch AM, Christiano A, Konda SR, Leucht P, Egol KA. Operative repair of proximal humerus fractures in septuagenarians and octogenarians: does chronologic age matter? J Clin Orthop Trauma. 2017;8(1):50–53. doi:10.1016/j.jcot.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bergdahl C, Ekholm C, Wennergren D, Nilsson F, Möller M. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish Fracture Register. BMC Musculoskelet Disord. 2016;17:159 doi:10.1186/s12891-016-1009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365–371. doi:10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 30. Lill H, Ellwein A, Katthagen C, Voigt C. Osteoporotische Frakturen am proximalen humerus. Chirurg. 2012;83(10):858–865. doi:10.1007/s00104-012-2337-3. [DOI] [PubMed] [Google Scholar]
- 31. Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79(2):203–207. [DOI] [PubMed] [Google Scholar]
- 32. Chun J-M, Groh GI, Rockwood CA. Two-part fractures of the proximal humerus. J Shoulder Elbow Surg. 1994;3(5):273–287. doi:10.1016/S1058-2746(09)80071-2. [DOI] [PubMed] [Google Scholar]
- 33. Tamimi I, Montesa G, Collado F, et al. Displaced proximal humeral fractures: when is surgery necessary? Injury. 2015;46(10):1921–1929. doi:10.1016/j.injury.2015.05.049. [DOI] [PubMed] [Google Scholar]
- 34. Seyhan M, Kocaoglu B, Nalbantoglu U, Aydin N, Guven O. Technique of Kirschner wire reduction and fixation of displaced two-part valgus angulated proximal humerus fractures at the surgical neck. J Orthop Trauma. 2012;26(6):e46–e50. doi:10.1097/BOT.0b013e3182254ecc. [DOI] [PubMed] [Google Scholar]
- 35. Eid A, Osman M, Fekry H-E. Percutaneous fixation with Schanz screws for displaced two- and three- part fractures of the proximal humerus in patients above fifty years of age. Int J Shoulder Surg. 2011;5(2):38–43. doi:10.4103/0973-6042.83195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vundelinckx BJ, Dierickx CA, Bruckers L, Dierickx CH. Functional and radiographic medium-term outcome evaluation of the humerus block, a minimally invasive operative technique for proximal humeral fractures. J Shoulder Elbow Surg. 2012;21(9):1197–1206. doi:10.1016/j.jse.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 37. Bogner R, Hübner C, Matis N, Auffarth A, Lederer S, Resch H. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br. 2008;90(12):1602–1607. doi:10.1302/0301-620X.90B12.20269. [DOI] [PubMed] [Google Scholar]
- 38. Dilisio MF, Nowinski RJ, Hatzidakis AM, Fehringer EV. Intramedullary nailing of the proximal humerus: evolution, technique, and results. J Shoulder Elbow Surg. 2016;25(5):e130–e138. doi:10.1016/j.jse.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 39. Lopiz Y, Garcia-Coiradas J, Garcia-Fernandez C, Marco F. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. J Shoulder Elbow Surg. 2014;23(3):369–376. doi:10.1016/j.jse.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 40. Nolan BM, Kippe MA, Wiater JM, Nowinski GP. Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elbow Surg. 2011;20(8):1241–1247. doi:10.1016/j.jse.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 41. Popescu D, Fernandez-Valencia JA, Rios M, Cuñé J, Domingo A, Prat S. Internal fixation of proximal humerus fractures using the T2-proximal humeral nail. Arch Orthop Trauma Surg. 2009;129(9):1239–1244. doi:10.1007/s00402-008-0789-1. [DOI] [PubMed] [Google Scholar]
- 42. Zhu Y, Lu Y, Shen J, Zhang J, Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am. 2011;93(2):159–168. doi:10.2106/JBJS.J.00155. [DOI] [PubMed] [Google Scholar]
- 43. Rajasekhar C, Ray PS, Bhamra MS. Fixation of proximal humeral fractures with the Polarus nail. J Shoulder Elbow Surg. 2001;10(1):7–10. doi:10.1067/mse.2001.109556. [DOI] [PubMed] [Google Scholar]
- 44. Kancherla VK, Singh A, Anakwenze OA. Management of acute proximal humeral fractures. J Am Acad Orthop Surg. 2017;25(1):42–52. doi:10.5435/JAAOS-D-15-00240. [DOI] [PubMed] [Google Scholar]
- 45. Olerud P, Ahrengart L, Söderqvist A, Saving J, Tidermark J. Quality of life and functional outcome after a 2-part proximal humeral fracture: a prospective cohort study on 50 patients treated with a locking plate. J Shoulder Elbow Surg. 2010;19(6):814–822. doi:10.1016/j.jse.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 46. Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20(5):747–755. doi:10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 47. Hessmann MH, Hansen WSM, Krummenauer F, Pol TF, Rommens PM. Locked plate fixation and intramedullary nailing for proximal humerus fractures: a biomechanical evaluation. J Trauma. 2005;58(6):1194–1201. [DOI] [PubMed] [Google Scholar]
- 48. Kitson J, Booth G, Day R. A biomechanical comparison of locking plate and locking nail implants used for fractures of the proximal humerus. J Shoulder Elbow Surg. 2007;16(3):362–366. doi:10.1016/j.jse.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 49. Newman JM, Kahn M, Gruson KI. Reducing postoperative fracture displacement after locked plating of proximal humerus fractures: current concepts. Am J Orthop (Belle Mead NJ). 2015;44(7):312–320. [PubMed] [Google Scholar]
- 50. Tamai K, Ishige N, Kuroda S, et al. Four-segment classification of proximal humeral fractures revisited: a multicenter study on 509 cases. J Shoulder Elbow Surg. 2009;18(6):845–850. doi:10.1016/j.jse.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 51. Mattyasovszky SG, Burkhart KJ, Ahlers C, et al. Isolated fractures of the greater tuberosity of the proximal humerus: a long-term retrospective study of 30 patients. Acta Orthop. 2011;82(6):714–720. doi:10.3109/17453674.2011.618912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rath E, Alkrinawi N, Levy O, Debbi R, Amar E, Atoun E. Minimally displaced fractures of the greater tuberosity: outcome of non-operative treatment. J Shoulder Elbow Surg. 2013;22(10):e8–e11. doi:10.1016/j.jse.2013.01.033. [DOI] [PubMed] [Google Scholar]
- 53. Verdano MA, Aliani D, Pellegrini A, Baudi P, Pedrazzi G, Ceccarelli F. Isolated fractures of the greater tuberosity in proximal humerus: does the direction of displacement influence functional outcome? An analysis of displacement in greater tuberosity fractures. Acta Biomed. 2014;84(3):219–228. [PubMed] [Google Scholar]
- 54. Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury. 1998;29(5):349–352. [DOI] [PubMed] [Google Scholar]
- 55. Fjalestad T, Hole MØ, Hovden IAH, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26(2):98–106. doi:10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- 56. Khurana S, Davidovitch RI, Kwon YK, Zuckerman JD, Egol KA. Similar function and improved range of shoulder motion is achieved following repair of three- and four-part proximal humerus fractures compared with hemiarthroplasty. Bull Hosp Jt Dis (2013). 2016;74(3):212–218. [PubMed] [Google Scholar]
- 57. Çelik C, Gümüştaş SA, Çeçen GS, Bulut G, Bekler Hİ. Mid-term follow-up evaluation of plate osteosynthesis and hemiarthroplasty results in multipart fractures of the proximal humerus. Ulus Travma Acil Cerrahi Derg. 2016;22(4):379–385. [DOI] [PubMed] [Google Scholar]
- 58. Gavaskar AS, Karthik BB, Tummala NC, Srinivasan P, Gopalan H. Second generation locked plating for complex proximal humerus fractures in very elderly patients. Injury. 2016;47(11):2534–2538. doi:10.1016/j.injury.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 59. Solberg BD, Moon CN, Franco DP, Paiement GD. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23(2):113–119. doi:10.1097/BOT.0b013e31819344bf. [DOI] [PubMed] [Google Scholar]
- 60. Ponce BA, Thompson KJ, Raghava P, et al. The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. J Bone Joint Surg Am. 2013;95(16):e113 (1-7). doi:10.2106/JBJS.K.00202. [DOI] [PubMed] [Google Scholar]
- 61. Zhang L, Zheng J, Wang W, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. 2011;35(11):1655–1661. doi:10.1007/s00264-011-1227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Xu J, Zhang C, Wang T. Avascular necrosis in proximal humeral fractures in patients treated with operative fixation: a meta-analysis. J Orthop Surg. 2014;9:31 doi:10.1186/1749-799X-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Rodia F, Theodorakis E, Touloupakis G, Ventura A. Fixation of complex proximal humeral fractures in elderly patients with a locking plate: a retrospective analysis of radiographic and clinical outcome and complications. Chin J Traumatol. 2016;19(3):156–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Schliemann B, Hartensuer R, Koch T, et al. Treatment of proximal humerus fractures with a CFR-PEEK plate: 2-year results of a prospective study and comparison to fixation with a conventional locking plate. J Shoulder Elbow Surg. 2015;24(8):1282–1288. doi:10.1016/j.jse.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 65. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22(3):195–200. doi:10.1097/BOT.0b013e31815b3922. [DOI] [PubMed] [Google Scholar]
- 66. Saltzman BM, Erickson BJ, Harris JD, Gupta AK, Mighell M, Romeo AA. Fibular strut graft augmentation for open reduction and internal fixation of proximal humerus fractures: a systematic review and the authors’ preferred surgical technique. Orthop J Sports Med. 2016;4(7):23259 67116656829. doi:10.1177/2325967116656829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hettrich CM, Neviaser A, Beamer BS, Paul O, Helfet DL, Lorich DG. Locked plating of the proximal humerus using an endosteal implant. J Orthop Trauma. 2012;26(4):212–215. doi:10.1097/BOT.0b013e318243909c. [DOI] [PubMed] [Google Scholar]
- 68. Jobin CM, Galdi B, Anakwenze OA, Ahmad CS, Levine WN. Reverse shoulder arthroplasty for the management of proximal humerus fractures. J Am Acad Orthop Surg. 2015;23(3):190–201. doi:10.5435/JAAOS-D-13-00190. [DOI] [PubMed] [Google Scholar]
- 69. Boons HW, Goosen JH, van Grinsven S, van Susante JL, van Loon CJ. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop. 2012;470(12):3483–3491. doi:10.1007/s11999-012-2531-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20(7):1025–1033. doi:10.1016/j.jse.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 71. Kontakis G, Koutras C, Tosounidis T, Giannoudis P. Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br. 2008;90(11):1407–1413. doi:10.1302/0301-620X.90B11.21070. [DOI] [PubMed] [Google Scholar]
- 72. Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Molé D. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11(5):401–412. [DOI] [PubMed] [Google Scholar]
- 73. Mata-Fink A, Meinke M, Jones C, Kim B, Bell J-E. Reverse shoulder arthroplasty for treatment of proximal humeral fractures in older adults: a systematic review. J Shoulder Elbow Surg. 2013;22(12):1737–1748. doi:10.1016/j.jse.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 74. Ferrel JR, Trinh TQ, Fischer RA. Reverse total shoulder arthroplasty versus hemiarthroplasty for proximal humeral fractures: a systematic review. J Orthop Trauma. 2015;29(1):60–68. doi:10.1097/BOT.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 75. Alentorn-Geli E, Guirro P, Santana F, Torrens C. Treatment of fracture sequelae of the proximal humerus: comparison of hemiarthroplasty and reverse total shoulder arthroplasty. Arch Orthop Trauma Surg. 2014;134(11):1545–1550. doi:10.1007/s00402-014-2074-9. [DOI] [PubMed] [Google Scholar]
- 76. Baudi P, Campochiaro G, Serafini F, et al. Hemiarthroplasty versus reverse shoulder arthroplasty: comparative study of functional and radiological outcomes in the treatment of acute proximal humerus fracture. Musculoskelet Surg. 2014;98(suppl 1):19–25. doi:10.1007/s12306-014-0322-3. [DOI] [PubMed] [Google Scholar]
- 77. Sebastiá-Forcada E, Cebrián-Gómez R, Lizaur-Utrilla A, Gil-Guillén V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23(10):1419–1426. doi:10.1016/j.jse.2014.06.035. [DOI] [PubMed] [Google Scholar]
- 78. Dezfuli B, King JJ, Farmer KW, Struk AM, Wright TW. Outcomes of reverse total shoulder arthroplasty as primary versus revision procedure for proximal humerus fractures. J Shoulder Elbow Surg. 2016;25(7):1133–1137. doi:10.1016/j.jse.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 79. Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res. 2009;95(1):48–55. doi:10.1016/j.otsr.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 80. Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br. 2007;89(4):516–520. doi:10.1302/0301-620X.89B4.18435. [DOI] [PubMed] [Google Scholar]
- 81. Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PAW. Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma. 2008;22(10):698–704. doi:10.1097/BOT.0b013e31818afe40. [DOI] [PubMed] [Google Scholar]
- 82. Cazeneuve JF, Cristofari D-J. The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg Br. 2010;92(4):535–539. doi:10.1302/0301-620X.92B4.22450. [DOI] [PubMed] [Google Scholar]
- 83. Gallinet D, Adam A, Gasse N, Rochet S, Obert L. Improvement in shoulder rotation in complex shoulder fractures treated by reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(1):38–44. doi:10.1016/j.jse.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 84. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop. 2011;469(12):3324–3331. doi:10.1007/s11999-011-2055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Grubhofer F, Wieser K, Meyer DC, et al. Reverse total shoulder arthroplasty for acute head-splitting, 3- and 4-part fractures of the proximal humerus in the elderly. J Shoulder Elbow Surg. 2016;25(10):1690–1698. doi:10.1016/j.jse.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 86. Longo UG, Petrillo S, Berton A, Denaro V. Reverse total shoulder arthroplasty for the management of fractures of the proximal humerus: a systematic review. Musculoskelet Surg. 2016;100(2):83–91. doi:10.1007/s12306-016-0409-0. [DOI] [PubMed] [Google Scholar]
- 87. Roche CP, Stroud NJ, Martin BL, et al. The impact of scapular notching on reverse shoulder glenoid fixation. J Shoulder Elbow Surg. 2013;22(7):963–970. doi:10.1016/j.jse.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 88. Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89(3):588–600. doi:10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]