Abstract
Background:
Little is known about career length after anterior cruciate ligament (ACL) reconstruction in Major League Soccer (MLS), the top men’s professional soccer league in the United States. Further, it is unspecified whether athletes returning to soccer after ACL reconstruction are at a higher risk for injuries, beyond new knee injuries.
Purpose:
To examine career length and the incidence of lower extremity injuries in MLS athletes after ACL reconstruction in comparison with age-matched controls.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Injuries and athletic exposures (AEs; games and training sessions) were recorded in the HealtheAthlete database, the injury surveillance system of MLS. All athletes who had undergone ACL reconstruction and returned to MLS were identified and age-matched with controls. Multivariate analyses of variance were used to compare career length and percentage of regular/postseason games that athletes started, substituted, or did not play. Generalized linear model regressions were used to examine the injury risk.
Results:
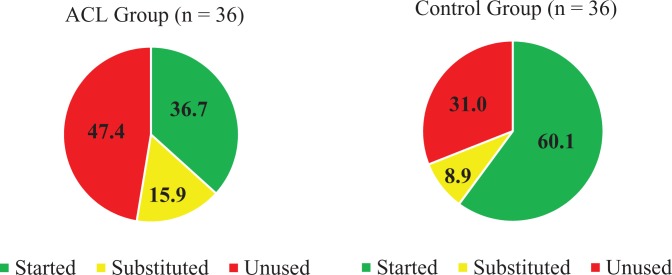
Athletes in the ACL group had shorter careers (1.3 ± 1.3 years) than those in the control group (2.5 ± 1.3 years) (P < .01), but while they were playing, athletes in the ACL group participated in a similar number of AEs as those in the control group (169.9 ± 129.0 vs 171.6 ± 124.9 AEs, respectively; P = .95). Athletes in the ACL group started fewer regular/postseason games (36.7% ± 34.3% vs 60.1% ± 33.8%, respectively; P < .01) and did not play in more regular/postseason games (47.4% ± 35.5% vs 31.0% ± 34.4%, respectively; P = .03) compared with those in the control group. The ACL group was not at a significantly greater risk for lower extremity injuries compared with the control group (relative risk, 0.87; 95% CI, 0.55-1.37).
Conclusion:
Although MLS athletes after ACL reconstruction are not at a greater risk for lower extremity injuries, this study suggests that they are not utilized in regular/postseason games as frequently and that their careers in MLS are shorter than age-matched controls. Further research is necessary to elucidate reasons for these athletes’ shortened MLS careers. This study supports the view of return to sport not as a single time point but as a continuum from return to participation to return to play and return to performance.
Keywords: soccer, return to sport, injury, risk, career length, anterior cruciate ligament
Anterior cruciate ligament (ACL) injuries are one of the more common severe injuries that occur in soccer, with an incidence of approximately 0.07 per 1000 hours, or 0.43 injuries per team per season.24 Returning to play and career longevity after ACL reconstruction are of great concern to professional athletes, as sport is their job and income source. An athlete’s return to sport is also of great concern to a club, as the athlete’s return affects the coach’s staffing options, the team’s financial interests, and the win-loss record.15 The career length after ACL reconstruction in men’s professional sports in the United States (US), such as the National Basketball Association, National Hockey League, and National Football League, is approximately 3 to 5 years.5,6,9,11,16 A study of National Football League offensive linemen found that athletes with a history of ACL reconstruction were 2 times more likely to have a shorter career than those with no history.4
Return to sport in European men’s professional soccer is very high, with 97% of Union of European Football Associations (UEFA) Champions League athletes returning to game play at their preinjury level of competition after ACL reconstruction. However, only 65% of these athletes continue to play at that same level 3 years later.24 This truncated career length seems startling; however, it is difficult to interpret without reference to the mean career length in Champions League soccer. Injury trends and return to sport may also be different in American and European men’s professional soccer. A study of Major League Soccer (MLS), the highest men’s professional soccer league in the US, found that 77% were able to return to their preinjury level of competition, with a mean career length after ACL reconstruction of 4 ± 3 years.10 Using publicly available data, the study found no significant difference in MLS career survival in the first 5 years after return to sport between athletes after ACL reconstruction and healthy controls.
In men’s professional soccer, a musculoskeletal injury increases an athlete’s risk 3-fold for a new musculoskeletal injury in the subsequent season.13 Hamstring, groin, and knee injuries, in particular, increase the risk for an identical injury in the subsequent season by 2 to 3 times.13 Athletes after ACL reconstruction have been reported to be at 6 times higher risk for a second ACL injury (ipsilateral or contralateral) compared with athletes having no history of an ACL injury.19 In men’s soccer, a history of ACL injury, reconstruction, and return to sport not only increases the risk for a second ACL injury but may also increase the risk for all new knee injuries, especially overuse knee injuries.23 Nonetheless, risks for other lower extremity injuries, outside the knee joint, upon return to sport after ACL reconstruction have not been reported.
The purpose of this study was to examine career length and the incidence of lower extremity injuries in athletes returning to MLS after ACL reconstruction. There were 3 hypotheses in this study. First, we hypothesized that athletes with a history of ACL reconstruction who returned to play in MLS would have shorter careers and participate in fewer games compared with age-matched control athletes with no history of ACL injuries. Second, we hypothesized that athletes after ACL reconstruction would have a higher incidence of lower extremity, noncontact, muscle, thigh, hamstring, knee, and overuse injuries compared with controls. Third, we hypothesized that athletes after ACL reconstruction would miss more days due to injury and experience more severe injuries than controls.
Methods
This was a matched-cohort study approved by the University of Delaware Institutional Review Board and the MLS Medical Research Committee (M-MARC). Data were collected prospectively by the certified athletic trainers of each MLS team and entered into the HealtheAthlete database, a database used by MLS for injury surveillance. Demographic, injury, and exposure data for all MLS athletes from January 1, 2011, to March 8, 2016, were extracted from the database. All athletes who sustained an ACL injury were identified. Athletes were excluded if they had a partial ACL injury, concomitant grade III ligamentous injury (such as a medial collateral ligament, lateral collateral ligament, or posterior cruciate ligament injury), chondral defect ≥1 cm2, or history of ACL injury before the study period. Athletes who had an ACL injury and returned to play but then sustained a second ACL injury were included. For injury incidence calculations, the date of the athlete’s second ACL injury was used as the end of his career to focus the analysis only on the risk associated with primary ACL injuries.
The ACL-reconstructed athletes were matched with controls based on age. Age was chosen as a matching variable because of the changes in injury incidence that occur as a player gets older8,14 and because age could serve as a proxy for playing experience. Further, holding injury variables the same, theoretically, 2 athletes of the same age should have a similar career length. As the HealtheAthlete database did not contain information on players before 2011 or before their entrance into MLS, previous playing experience was unknown. Control athletes were identified through participation records in the HealtheAthlete database. A control athlete was chosen as a match by being closest in age to his respective ACL group athlete and participating in a training session or game on the same day that the ACL group athlete returned to MLS training. This date, for both groups, was referred to as the return-to-play date.
Career length was defined as the period between the return-to-play date and the date on which the player left or retired from MLS. This definition was established, as there was no information in the HealtheAthlete database on players once they left MLS. This definition leaves open the possibility that players could still be playing professionally somewhere after leaving MLS. However, few players move to the top division of leagues in other countries when they leave MLS17; thus, this definition of career length captured a player’s ability to return to and maintain play at his preinjury level of competition. Career length was measured in years, athletic exposures (AEs; any game or training session), number of games, and games–to–training sessions ratio. Games included preseason, reserve team, regular-season, and postseason games. The games–to–training sessions ratio was used rather than the raw number of training sessions to capture the amount of training that the athlete was undergoing relative to the number of games that he played. For example, a small games–to–training sessions ratio would indicate that an athlete was training quite a bit but not playing in games.
In addition to career length, a matched period was also defined to capture the window of time after the athlete’s return to sport when participation or subsequent injuries could be related to his ACL reconstruction. The matched period extended from the return-to-play date for 2 years or until the ACL group athlete left MLS, whichever occurred first. The matched period was measured in AEs, games, and games–to–training sessions ratio as well as the percentage of regular/postseason games that the athlete started, substituted, or did not play. The percentage of regular/postseason games that each player started, substituted, or did not play was calculated using both the HealtheAthlete database and publicly available data (www.mlssoccer.com). The MLS website provided information on whether the athlete started, substituted, or did not play. For each game that an athlete did not play, the HealtheAthlete database clarified if he did not play because he was unavailable as a result of an injury or if he was available for selection (ie, healthy/fit) but not chosen to start or substitute. The percentage of regular/postseason games started was calculated by dividing the number of regular/postseason games that the athlete started by the total number of regular/postseason games in the matched period that the athlete was available for selection. A similar calculation was performed for the percentage of regular/postseason games substituted or not played.
We used the UEFA consensus statement’s injury definitions (Table 1).12 The injury incidence of each group during the matched period was calculated by dividing the total number of injuries by the number of AEs and then multiplying by 1000 AEs. The total number of days missed due to injury by each player was calculated, and each athlete’s injuries were categorized by severity.
TABLE 1.
Injury Definitions Useda
| Term | Definition |
|---|---|
| Lower extremity injury | Any complaint related to the hip/groin, thigh, knee, lower leg, ankle, or foot sustained by a player during a soccer game or training session and which caused the athlete to seek medical attention |
| Time-loss injury | An injury that caused an athlete to miss a subsequent training session or game |
| Noncontact injury | An injury that was not the result of a collision with another player or object |
| Injury severity | The number of days away from soccer: minimal (1-3 days), mild (4-7 days), moderate (8-28 days), or severe (>28 days) |
aAll injury definitions used in this article follow the Union of European Football Associations (UEFA) consensus statement.12
All statistical analyses were performed in SPSS version 24 (IBM). Demographics were compared between the ACL and control groups using t tests, and multivariate analyses of variance were used to determine if there were differences between the groups in career length. All athletes, including those still playing in MLS, were included in the analysis. The career length for those athletes still playing in MLS was calculated using the last day of the study as the last day of their career. Multivariate analyses of variance were used to determine if there were differences between the groups in AEs, games, and games–to–training sessions ratio in the matched period as well as if there were differences between the groups in the percentage of games started, substituted, or not played.
An athlete’s potential MLS career was defined as the time from the athlete’s return-to-sport date to the end of the study period (March 8, 2016). As a means of examining survival, the percentage of an athlete’s potential MLS career that he played was calculated by dividing the athlete’s MLS career length by his time in the study. For example, if an athlete played from his return-to-sport date to the end of the study, he would have played 100% of his potential MLS career. If an athlete played for 6 months but there was a year between his return-to-sport date and the end of the study, the athlete would have played 50% of his potential MLS career. A chi-square test was used to determine if there was a difference between the 2 groups in the number of athletes who played 100% of their potential MLS careers.
Generalized linear model regressions with Tweedie distributions and logit link functions were used to calculate the relative risk and 95% CI for lower extremity, time-loss lower extremity, noncontact, muscle, thigh, hamstring, knee, and overuse injuries. Similar regression models were also used to determine the relative risk for each category of injury severity (minimal, mild, moderate, severe). The control group was used as the reference in all models. Analysis of variance was used to determine if there were differences between the groups in the number of days missed due to injury.
Cohen d effect sizes were calculated and classified as small (d = 0.20), medium (d = 0.50), and large (d = 0.80).7 Power calculations were performed a priori using preliminary data and G*Power software version 3.1.0 (Universität Düsseldorf). The control group had a preliminary incidence of knee injuries of 0.9 per 1000 AEs; using a generalized linear model with Tweedie distributions and logit link functions, with P = .05 and power of 0.80, it was determined that a relative risk of 1.1 could be detected with a total sample size of 40.
Results
We identified 64 athletes who sustained 66 ACL injuries (Figure 1 and Table 2). Three athletes were excluded because of concomitant lateral collateral ligament avulsions, 1 because the injury was a partial ACL rupture, 2 because they had a history of ACL injuries before the study period (information detailed in the HealtheAthlete database), and 4 because they were still undergoing rehabilitation at the end of the study period (Figure 1). This left 54 athletes (all of whom had undergone ACL reconstruction), 40 of whom returned to MLS (74%) and were included in the analysis (Table 2). Two athletes returned to play but sustained graft ruptures (1 bone–patellar tendon–bone [BPTB] autograft, 1 BPTB allograft). Both athletes returned to MLS after undergoing ACL revision (one for 4 months and the other for 1 season and was still playing at the end of the study period).
Figure 1.
Flow diagram showing the inclusion and exclusion of athletes in the study.
TABLE 2.
Anthropometrics and Demographics of the ACL and Control Groupsa
| ACL Group (n = 40) | Control Group (n = 40) | P Value | |
|---|---|---|---|
| Height, m | 1.83 ± 0.06 | 1.80 ± 0.07 | .06 |
| Weight, kg | 79.2 ± 8.3 | 77.4 ± 9.7 | .38 |
| Age at beginning of MLS career, y | 24.1 ± 4.3 | 24.9 ± 3.8 | .42 |
| Age at date of return to play, y | 26.8 ± 4.1 | 26.7 ± 3.8 | .85 |
| Graft type, n | |||
| BPTB autograft | 25 | — | — |
| BPTB allograft | 6 | — | — |
| Hamstring autograft | 6 | — | — |
| Graft type information missing | 3 | — | — |
aValues are expressed as mean ± SD unless otherwise specified. ACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone; MLS, Major League Soccer.
Of the 40 athletes in each group, 12 athletes in the ACL group and all 40 athletes in the control group were still playing in MLS at the end of the study period. There was a significant difference between the groups in MLS career length (Table 3) when measured in years (P < .01, d = 0.94), AEs (P < .01, d = 0.97), and games (P < .01, d = 0.79). However, there was no difference in the games–to–training sessions ratio (P = .54, d = 0.14). There were no differences between the groups in AEs (P = .95, d = 0.00), games (P = .44, d = 0.18), or games–to–training sessions ratio (P = .87, d = 0.00) during the matched period (Table 3).
TABLE 3.
Differences Between Groups According to MLS Career Length and Matched Period Exposuresa
| ACL Group (n = 40) | Control Group (n = 40) | P Value | Effect Size (d) | |
|---|---|---|---|---|
| Career length | ||||
| Years | 1.3 ± 1.3 | 2.5 ± 1.3 | <.01 | 0.94 |
| Athletic exposures | 209.0 ± 199.7 | 421.4 ± 255.5 | <.01 | 0.97 |
| Games | 49.2 ± 51.8 | 92.2 ± 58.5 | <.01 | 0.79 |
| Games–to–training sessions ratio | 0.30 ± 0.2 | 0.27 ± 0.1 | .54 | 0.14 |
| Matched period | ||||
| Athletic exposures | 169.9 ± 129.0 | 171.6 ± 124.9 | .95 | 0.00 |
| Games | 36.8 ± 28.7 | 42.4 ± 34.7 | .44 | 0.18 |
| Games–to–training sessions ratio | 0.31 ± 0.22 | 0.30 ± 0.12 | .87 | 0.00 |
aValues are expressed as mean ± SD unless otherwise specified. Games include preseason, regular-season, reserve team, and postseason games. ACL, anterior cruciate ligament; MLS, Major League Soccer.
Four athletes in the ACL group returned to training and participated in reserve team and/or preseason matches but did not return to regular/postseason games. As a result, these athletes in the ACL group and their matched athletes in the control group were not included in the analysis of the percentage of regular/postseason games started, substituted, or not played. Athletes in the ACL group had a significantly lower percentage of regular/postseason games started compared with athletes in the control group (36.7% ± 34.3% vs 60.1% ± 33.8%, respectively; P < .01, d = 0.76) and a significantly higher percentage of regular/postseason games that they did not play (47.4% ± 35.5% vs 31.0% ± 34.4%, respectively; P = .03, d = 0.54) (Figure 2). There were significantly more athletes in the control group (40/40) who played 100% of their potential MLS careers (ie, athletes who played the entire duration of time from their return-to-sport date to the end of the study) compared with those in the ACL group (12/40; P < .01) (Figure 3).
Figure 2.
Pie charts representing the mean percentage of regular/postseason games started, substituted, or not played for each group.
Figure 3.
Number of athletes stratified by percentage of their potential Major League Soccer (MLS) careers (N = 80).
In the matched period, the ACL group had 114 lower extremity injuries in 6798 AEs (lower extremity injury incidence rate of 16.8/1000 AEs). The control group had 132 lower extremity injuries in 6868 AEs (lower extremity injury incidence rate of 19.2/1000 AEs). Table 4 details the number of injuries, incidence rate, and relative risk for each category of injury studied. The ACL group had a relative risk of 1.88 (95% CI, 0.59-5.94; P = .28) for noncontact lower extremity injuries, a relative risk of 0.36 (95% CI, 0.10-1.22; P = .10) for hamstring injuries, and a relative risk of 0.45 (95% CI, 0.13-1.56; P = .21) for thigh injuries compared with the control group (Table 4). Regarding knee injuries, the ACL group had a relative risk of 3.07 (95% CI, 0.67-14.12; P = .15) compared with the control group.
TABLE 4.
Number, Incidence Rate, and Relative Risk of Injuries During the Matched Period for the ACL and Control Groupsa
| Raw No. of Injuries (Rate per 1000 AEs) | Relative Risk (95% CI) | P Value | ||
|---|---|---|---|---|
| ACL Group | Control Group | |||
| Lower extremity injuries | 114 (16.77) | 132 (19.23) | 0.87 (0.55-1.40) | .57 |
| Time-loss lower extremity injuries | 62 (9.12) | 55 (8.01) | 1.02 (0.51-2.07) | .95 |
| Noncontact lower extremity injuries | 28 (4.12) | 14 (2.04) | 1.88 (0.59-5.94) | .28 |
| Muscle/tendon injuries | 30 (4.41) | 34 (4.95) | 0.60 (0.23-1.57) | .30 |
| Thigh injuries | 22 (3.23) | 26 (3.79) | 0.45 (0.13-1.56) | .21 |
| Hamstring injuries | 8 (1.17) | 18 (2.62) | 0.36 (0.10-1.22) | .10 |
| Knee injuries | 17 (2.50) | 10 (1.46) | 3.07 (0.67-14.12) | .15 |
| Overuse injuries | 5 (0.74) | 6 (0.87) | 0.57 (0.11-2.91) | .50 |
aACL, anterior cruciate ligament; AE, athletic exposure.
There was no significant difference between the groups in the mean number of days missed due to injury (P = .27, d = 0.26), with the ACL group missing, on average, 39.8 ± 55.1 days and the control group missing 26.5 ± 61.2 days. The ACL group had a relative risk of 1.89 for severe injuries (95% CI, 0.76-4.69; P = .17) (Table 5).
TABLE 5.
Number of Time-Loss Injuries According to Injury Severity and Relative Risk for the ACL and Control Groupsa
| No. of Time-Loss Injuries | Relative Risk (95% CI) | P Value | ||
|---|---|---|---|---|
| ACL Group | Control Group | |||
| Minimal (1-3 days) | 7 | 9 | 0.78 (0.26-2.35) | .66 |
| Mild (4-7 days) | 14 | 12 | 1.17 (0.53-2.55) | .70 |
| Moderate (8-28 days) | 29 | 24 | 1.32 (0.63-2.15) | .64 |
| Severe (>28 days) | 17 | 9 | 1.89 (0.76-4.69) | .17 |
aACL, anterior cruciate ligament.
Discussion
In this study, 74% of athletes returned to MLS after primary ACL reconstruction. Athletes who returned to play had significantly shorter MLS careers than their counterparts with no history of ACL injuries by approximately half. Although the first hypothesis was supported with regard to career length, there were interesting findings with regard to game play. During the matched period (the 2 years after return to play or until the athlete in the ACL group left MLS, whichever occurred first), there were no differences in AEs or games played (games included all preseason, reserve team, regular-season, and postseason games), indicating that athletes were participating to the same extent. However, athletes in the ACL group started significantly fewer regular/postseason games and did not play in significantly more regular/postseason games than athletes in the control group. The findings of the second hypothesis regarding the injury incidence were mixed. There were no differences between the groups in the risk of lower extremity injuries, but within specific categories, there were trends for increased (noncontact, knee injuries) and decreased (hamstring, thigh injuries) risks for the ACL group. For the third hypothesis regarding injury severity, we found no difference in the number of days missed due to injury, but the ACL group may have sustained more severe injuries compared with the control group. The results of this study indicate that ACL reconstruction may have a major impact on the performance and careers of MLS athletes. Such performance and career effects suggest that further improvements in surgical technique, rehabilitation, and/or psychological support are needed for MLS players who sustain ACL injuries.
In 2016, Waldén et al24 reported that after ACL reconstruction, 100% of athletes playing for UEFA Champions League teams returned to training, and 97% returned to game play at their preinjury level of competition. This study found that return to MLS was lower than UEFA, with only 74% of players returning to MLS training and 69% returning to game play. However, the findings of this study are similar to the rate previously reported in MLS of 77%.10 More work examining the reasons why there are differences in return-to-sport rates between the leagues in Europe and the US is needed. We hypothesize that one major factor could be club resources, as there are differences in both the financial and staffing resources between the many European and US teams.2,22 Other reasons could include financial pressure from salaries and contracts, team obligations, or differences in the level of play between leagues.2,22
The striking finding of this study was that athletes in the ACL group had careers only half as long as those in the control group. Only 5 of the 40 athletes in the ACL group (12.5%) played in MLS for longer than 3 years after their ACL reconstruction. As these athletes after ACL reconstruction did not seem to be at a higher risk of injuries, their shorter MLS careers may be a result of other factors such as player performance, as indicated by the regular/postseason playing data. Waldén et al24 also found that not all athletes after ACL reconstruction continued to play at their preinjury levels of competition; however, they found that a much larger percentage maintained the preinjury level. Sixty-five percent of UEFA Champions League athletes after ACL reconstruction were still playing at their preinjury levels of competition 3 years later.24 Waldén et al did not comment on the reasons for players’ not remaining at their preinjury levels. Perhaps the preinjury level factors in, but further investigation into why so few MLS players are able to continue at their preinjury levels of competition is needed.
The career length results of this study are also in contrast to those of Erickson et al,10 who found that the mean MLS career length after ACL reconstruction was 4.0 ± 2.8 years and that approximately 52% were still playing after 3 years. Different data sources as well as study dates may underlie some of the contrasting results. The decision in this study to include athletes who were still active in MLS influenced the findings of this study. Yet, if the results of this study had been held until all of these players had concluded their MLS careers, the control group’s mean career length would have been even longer than 2.5 ± 1.3 years and the contrast to the ACL group’s mean career length (1.3 ± 1.3 years) even greater. Further, this analysis only included athletes who returned to MLS. If athletes who had not returned were also included, the career length statistics for the ACL group would look even more disparate.
Although the athletes in the ACL group had shorter careers, they participated in a similar number of AEs while they were playing. There were no significant differences between the groups in the number of AEs or games (games included preseason, reserve team, regular season, and postseason). Nor was there a difference in the games–to–training sessions ratio during the matched period, indicating that athletes were training a similar amount relative to the number of games that they were playing in. Viewing these results from the perspective of return to sport not as one specific time point but rather as a continuum,1 the similarities between the groups in AEs seem to indicate that after ACL reconstruction, athletes returned to participation and returned to play. However, the differences between the groups in the percentage of regular/postseason games started and the percentage not played may indicate that the athletes in the ACL group did not make a full return to performance.1 Even though athletes in the ACL group played a similar number of games (when including preseason and reserve team games), they started significantly fewer and did not play in significantly more regular/postseason games than those in the control group. An athlete’s not playing in a game means that he was available (cleared medically and fit to play) and selected to the game-day roster but did not start the game or was substituted onto the field. A professional athlete being unused frequently, especially in important games such as during the postseason, may have negative impacts on his leverage during contract negotiations, potentially leading to a premature ending of his MLS career. Although it requires additional attention and collaboration between the medical, strength and conditioning, and coaching staff to continue to focus on and support an athlete even once he has returned to play, the results of this study suggest a greater need for return-to-performance training.
With regard to the risk for lower extremity injuries, a positive finding for MLS athletes after ACL reconstruction was a potentially lower risk for hamstring and thigh injuries compared with those in the control group. Deficits in quadriceps and hamstring muscle strength, dependent on graft type, have been observed after ACL reconstruction.25 Furthermore, quadriceps strength asymmetries after ACL reconstruction have negative functional and biomechanical repercussions.20,21 As a result, quadriceps and hamstring strengthening is a primary focus of many ACL reconstruction rehabilitation protocols. It is possible that the decreased risk for thigh and hamstring injuries seen in the ACL group could be a result of this focused training and effort. Further studies are needed to examine if there is a direct link between quadriceps and hamstring exercises performed during ACL reconstruction rehabilitation and decreased thigh and hamstring injury rates upon return to sport; however, this study seems to support the view that continued focus on these 2 muscle groups during rehabilitation may positively affect the quadriceps and hamstring risk upon returning to the field.
This study found that athletes in the ACL group were at 1.9 times higher risk for severe injuries (injuries causing an absence of >28 days), 1.9 times higher risk for noncontact injuries, and 3.1 times higher risk for a new knee injury. Although these relative risks were not statistically significant, all indicate that these athletes may require more secondary-injury prevention efforts. A higher risk for a new knee injury is not surprising, given the known high risk for second ACL injuries.18,19 In a Swedish cohort of men’s professional soccer players, athletes after ACL reconstruction were at 7.9 times higher risk for a new knee injury.23 Differences in the risk between the 2 studies may be because of the time period examined after ACL reconstruction. However, these findings indicate a need for further study into the types of noncontact and severe injuries that athletes in the ACL group sustained and how to prevent them. Where the career length results of this study indicate a need to support athletes even after their return to play with regards to performance, these injury incidence results indicate these athletes may also need continued attention with regard to prevention.
This study is not without limitations. As the Healthe-Athlete database did not contain information on athletes’ playing experience before joining MLS or before 2011, it was not possible to match athletes based on playing experience, only age. Athletes come to MLS from all over the world, making it very difficult to reliably ascertain information on each of them. Further, although the HealtheAthlete database included a history of ACL injuries, it contained limited surgical and imaging information. A study of National Football League athletes found that the presence of concomitant meniscal lesions affected career length after an ACL injury.3 Although imaging and/or operative reports were available on some athletes, they were not available on others, preventing this study from analyzing such variables. Future studies are needed to examine the implications of meniscal lesions on career length after ACL reconstruction in MLS.
This study chose to define career length as the time from the return-to-sport date until the athlete left MLS or retired. The definition was created because we wanted to focus on athletes’ ability to return to and maintain a career at their preinjury level of competition. Within this definition, an athlete could leave MLS but still be playing professional soccer. Few players leave MLS to play in the top division of leagues in other countries; thus, this definition assumes that upon leaving MLS, players would be departing their preinjury level of competition. We acknowledge the limits to this assumption but believe that the findings of this study still herald attention, even if 1 or 2 additional players continue to play at their preinjury level of competition. Further, as this definition of career length focused on only the athletes who returned to MLS, if athletes who had not returned were included in career length calculations (ie, a career length of 0 years), the resulting career length after ACL reconstruction would be even more dire.
A strength of this study is that it was able to capture every ACL injury within a professional men’s soccer league. Although this is only one league, and the results indicate that there may be differences when comparing men’s professional soccer leagues around the world, this study is the first to examine the lower extremity injury risk after ACL reconstruction beyond just the knee joint. Future studies with larger populations, such as that of the UEFA Champions League, with 78 teams,24 could allow for a more thorough examination of risk as well as the influence of previous lower extremity injuries and playing experience.
Conclusion
In this study, athletes who returned to play after ACL reconstruction had significantly shorter MLS careers, by approximately half, compared with age-matched healthy peers. Despite the fact that the ACL group and control group had similar AEs, athletes in the ACL group started in a smaller percentage and did not play in a larger percentage of regular/postseason games compared with their healthy peers. Athletes in the ACL group seemed to have a lower risk for hamstring and thigh injuries compared with those in the control group but may have had a higher risk for noncontact, knee, and more severe injuries. These results highlight the importance of viewing return to sport as a continuum and continuing to focus on athletes’ needs even upon return to play to maximize their potential to return and maintain their preinjury level of performance.
Acknowledgment
The authors thank the M-MARC for its support of this research project and especially Natalie Akula and Joe Atkinson for their help administratively. The authors thank all of the MLS-certified athletic trainers for their record keeping and input of data into the HealtheAthlete database. They also thank MLS and the MLS Players Union for approving this study and Cerner for its help in accessing the data.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was funded by a Legacy Grant from the Sports Section of the American Physical Therapy Association. A.J.H.A. also received support for her work from the National Institutes of Health (R01 AR048212 and R44 HD068054) as well as a Promotion of Doctoral Studies I Scholarship from the Foundation for Physical Therapy. H.J.S.-G. also received support for some of her work from the National Institutes of Health (R44 HD068054).
Ethical approval for this study was waived by the University of Delaware.
References
- 1. Ardern CL, Glasgow P, Schneiders A, et al. 2016. consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50:853–864. [DOI] [PubMed] [Google Scholar]
- 2. Barnard M, Ross C, Savage J, Winn C. Ahead of the Curve: Deloitte Annual Review of Football Finance. Manchester, UK: Deloitte; 2017. [Google Scholar]
- 3. Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF. Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes. Am J Sports Med. 2009;37(11):2102–2107. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768–775. [DOI] [PubMed] [Google Scholar]
- 5. Busfield BT, Kharrazi FD, Starkey C, Lombardo SJ, Seegmiller J. Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthroscopy. 2009;25(8):825–830. [DOI] [PubMed] [Google Scholar]
- 6. Cinque ME, Hannon CP, Bohl DD, et al. Return to sport and performance after anterior cruciate ligament reconstruction in National Football League linemen. Orthop J Sports Med. 2017;5(6):2325967117711681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed New York: Routledge; 1988. [Google Scholar]
- 8. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 9. Erickson BJ, Harris JD, Cole BJ, et al. Performance and return to sport after anterior cruciate ligament reconstruction in National Hockey League players. Orthop J Sports Med. 2014;2(9):2325967114548831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male Major League Soccer players. Orthop J Sports Med. 2013;1(2):2325967113497189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Erikson BJ, Harris JD, Heninger JR, et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728–e734. [DOI] [PubMed] [Google Scholar]
- 12. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med. 2006;40(3):193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hägglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hägglund M, Waldén M, Ekstrand J. UEFA injury study: an injury audit at European Championships 2006 to 2008. Br J Sports Med. 2009;43:483–489. [DOI] [PubMed] [Google Scholar]
- 15. Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):738–742. [DOI] [PubMed] [Google Scholar]
- 16. Harris JD, Erickson BJ, Bach BR, et al. Return-to-sport and performance after anterior cruciate ligament reconstruction in National Basketball Association players. Sports Health. 2013;5(6):562–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Major League Soccer. MLS Transfer Window Tracker: winter 2016/17. Available at: https://www.mlssoccer.com/transactions/2017/winter-transfer-window-tracker. Accessed September 20, 2017.
- 18. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sports Med. 2012;22(2):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schmitt L, Paterno MV, Hewett T. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after ACL reconstruction. Med Sci Sport Exer. 2014;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith C. Major League Soccer’s most valuable teams. Available at: https://www.forbes.com/sites/chrissmith/2017/08/16/major-league-soccers-most-valuable-teams-2/3/#3733c36241e2. Accessed September 20, 2017.
- 23. Waldén M, Hägglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med. 2006;40(2):158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744–750. [DOI] [PubMed] [Google Scholar]
- 25. Xergia S, McClelland J, Kvist J, Vasiliadis H, Georgoulis A. The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg Sport Traumatol Arthrosc. 2011;19(5):768–780. [DOI] [PubMed] [Google Scholar]