Abstract
Objective:
The purpose of this article was to assess the satisfaction of adult patients who received mental health services (MHS) in healthcare networks staffed by multidisciplinary professionals and offering a range of MHS, and to identify variables associated with patient satisfaction.
Methods:
This cross-sectional study included 325 patients with mental disorders (MDs) among 4 Quebec health service networks. Data were collected using 9 standardized instruments and participant medical records. A 3-factor conceptual framework (predisposing, enabling, and needs-related factors) based on Andersen’s Behavioral Model was used, integrating sociodemographic, clinical, needs-related, service utilization, social support, and quality-of-life (QOL) variables. An adjusted multiple linear regression model was performed.
Results:
The global mean score for patient satisfaction was 4.11 (minimum: 2.0; maximum: 5.0). Among the enabling factors, continuity of care, having a case manager, and help received from services were positively associated with patient satisfaction, whereas being hospitalized was negatively associated. Among the needs-related factors, the number of needs was negatively associated with satisfaction.
Conclusions:
Findings demonstrated higher levels of satisfaction among patients who received good continuity of care and well-managed, frequent services in relation to their needs. Dissatisfaction was higher for patients with serious unmet needs or those hospitalized, which underlines the importance of taking these particular variables into account in the interest of improving MHS delivery and patient recovery.
Keywords: patient satisfaction, mental health services, service utilization, mental disorders, Andersen’s Behavioral Model
Abstract
Objectif :
Le but de cet article était d’évaluer la satisfaction des patients adultes qui recevaient des services de santé mentale dans des réseaux de la santé dont le personnel compte des professionnels multidisciplinaires et qui offrent une gamme de services de santé mentale. L’objectif était aussi d’identifier les variables associées à la satisfaction des patients.
Méthodes :
Cette étude transversale incluait 325 patients souffrant de troubles mentaux (TM) dans 4 réseaux de santé du Québec. Les données ont été recueillies à l’aide de 9 instruments normalisés et des dossiers médicaux des participants. Un cadre conceptuel en 3 facteurs (prédisposant, habilitant, et facteurs liés aux besoins) basé sur le modèle comportemental d’Andersen a été utilisé, intégrant les variables sociodémographiques, cliniques, liées aux besoins, d’utilisation des services, de soutien social, et de la qualité de vie (QDV). Un modèle ajusté de régression linéaire multiple a été effectué.
Résultats :
Le score moyen global de la satisfaction des patients était de 4,11 (minimum 2,0 ; maximum 5,0). Parmi les facteurs habilitants, la continuité des soins, avoir un gestionnaire de cas et l’aide reçue des services étaient positivement associés à la satisfaction des patients, alors qu’être hospitalisé était négativement associé. Parmi les facteurs liés aux besoins, le nombre des besoins était négativement associé à la satisfaction.
Conclusions :
Les résultats ont démontré des niveaux plus élevés de satisfaction chez les patients qui recevaient une bonne continuité des soins, et des services fréquents, bien gérés en relation avec leurs besoins. L’insatisfaction était plus élevée pour les patients dont les besoins sérieux n’étaient sérieusement pas comblés et pour ceux qui étaient hospitalisés, ce qui souligne l’importance de prendre en compte ces variables particulières dans le but d’améliorer la prestation des services de santé mentale et le rétablissement des patients.
Introduction
Patient satisfaction related to health services has been increasingly studied during the past 20 years, because satisfaction is a good indicator of quality in service delivery and individual healthcare. Patients satisfied with the effectiveness of interventions are more treatment compliant and tend to take better advantage of services.1 A high level of satisfaction among patients using mental health services (MHS) also increases involvement in treatment and supports recovery.1,2 Yet patient satisfaction with mental health (MH) care is particularly challenging among those with multiple and diverse needs. Healthcare reforms aimed at increasing quality in health systems have viewed patient satisfaction as an important consideration.
Studies have demonstrated that men,3–5 the elderly,4,6–8 and educated patients3 are relatively more satisfied with MHS. Ethnicity also has an effect on patient satisfaction; that is, belonging to an ethnic group may be associated with variability in conceptualizations of satisfaction and in expectations associated with care.2,9,10 Other research showed a decrease in patient satisfaction among people with severe mental disorders (MDs) (e.g. schizophrenia and schizophrenia spectrum disorders) following the experience of pharmacological disturbances,9,11–13 although the association between severe MDs and satisfaction did not reach significance.14,15 As underlined in the literature, the needs of patients in treatment, whether directly related to MH, are more vital research considerations than clinical characteristics are. Studies have also observed that fewer unmet needs related to an adequate support in different life domains were related to better patient MH recovery,6,16–18 increasing satisfaction with MHS in turn.1,2
Good communication between patients and professionals19,20 as well as rapid and effective patient health management were also identified as determinants of high satisfaction.13,21 Positive attitudes among service providers, professionalism,9,22 and professional competence22–24 also had a positive impact on satisfaction. Moreover, research has identified the importance of an appropriate and adequate environment for providing patient care.15 In this connection, patients who received services outside of hospitals, in public or community care programs, were particularly satisfied with their treatment compared to hospitalized patients.24 Continuity of care and longer treatment duration, among more vulnerable patients especially, were other important determinants of increased patient satisfaction.8,24,25 Finally, quality of life (QoL), which includes satisfaction in life domains related to housing, money, and relationships, as well as family and social networks, also related positively to patient satisfaction.7,25–31
Many studies have analyzed patient satisfaction for specific populations and for particular types of services. Patient satisfaction has been evaluated for different population groups, including adults,32 children and adolescents,1,20–22,33 geriatric patients,34 and veterans.25 Other studies analyzed patient satisfaction for specific clinical diagnoses, including schizophrenia and major depression.11,26,35 Regarding different types of MHS, studies have assessed satisfaction following admission to public hospitals6,12,13,19,20,22,36,37 as well as services received through public clinics or community programs.1,9,38–43 Comparisons of patient satisfaction among those who received hospital treatment versus outpatient treatment demonstrated patient preferences for community-based services.14,44 Finally, patient satisfaction has generally been evaluated in particular geographic areas, whether urban21 or rural,7,40 in both European and Middle Eastern countries14,22 and in the United States.10 Few studies on service utilization and patient satisfaction have been conducted in Quebec, Canada. However, the available studies have used cohorts of immigrants recruited exclusively from the island of Montreal,45 or from single settings (e.g. outpatient settings) in urban areas.46–48
Several tools have been developed to optimize the evaluation of patient satisfaction, including the Verona Service Satisfaction Scale (VSSS: VSSS-54, VSSS-32, and VSSS-EU), partly adapted from the Service Satisfaction Scale (SSS), which measures satisfaction with MHS received during the previous year.14,19,23,26,44,49–53 The Client Satisfaction Questionnaire (CSQ/CSQ-8) also estimates general satisfaction with services,1,36,39,54 whereas the Barker instrument assesses care received from psychiatrists.38 Many studies have adapted these instruments9,11,15,32,55 or developed others with qualitative, quantitative, or mixed-method approaches in line with study objectives.3,4,10,40,41,56,57 Among previous studies conducted in Quebec that used standardized tools,46,47 however, none assessed the overall impact of service utilization or types of professionals on patient satisfaction. Moreover, to the best of our knowledge, no study has evaluated patient satisfaction with MHS in Quebec, taking into account both urban and semirural areas, and including the full range of MH diagnoses.
This study is based on Andersen’s Behavioral Model,58 the most frequently used tool for identifying factors associated with health service use. This model distinguishes variables according to predisposing, enabling, and needs factors. Predisposing factors are sociocultural characteristics of individuals existing prior to diagnosis, such as gender and age. Enabling factors represent the logistical aspects of obtaining MH care, including facilitators to healthcare use. Needs factors, based on a variety of functional and health-related problems, are considered the most immediate motivational factors in seeking help from MHS. Although previous studies have established relationships between specific sociodemographic and diagnostic variables, and predisposing and needs factors, certain other variables such as type of housing, help desired, help received from services, and help received from relatives, as enabling factors, have received little attention. Moreover, no study has tested variables in the multidimensional Andersen model for associations with patient satisfaction or with MHS utilization.
This study aims to assess satisfaction with MHS utilization among adults with various MDs, including both severe and common (e.g. anxiety and depression) conditions, living in communities and using a variety of services and professionals. A second objective is to identify variables associated with patient satisfaction. Based on studies of MHS utilization using the Andersen model, we hypothesize that needs-related variables and predisposing factors, in that order, will better explain levels of patient satisfaction with MHS. The unique contribution of this study was to systematically examine sociodemographic, clinical, needs, QoL, and social support variables, as well as service use variables including continuity of care, in association with global satisfaction within a network of diversified services. Using the Andersen model and integrating variables not previously tested for patient satisfaction, the study will identify potential variables related to patient satisfaction or dissatisfaction with MHS.
Method
Setting
The study occurred in 4 health service networks located in Quebec, including 3 urban areas and 1 semi-urban area. Populations ranged from 135,000 to 300,000 inhabitants. Networks included service delivery by general hospital psychiatric departments and psychiatric hospitals, inpatient and outpatient MH teams, primary care clinics including general practitioners (GPs) and psychologists, addiction centers, community health and social service centers (CLSCs), and community-based MH organizations offering day centers, crisis services, self-help groups, supported housing, and employment programs for consumers with MDs and with co-occurring problems. The study coincided with implementation of the Quebec Mental Health Reform (2005–2015),59,60 which aimed to improve the accessibility, quality, and continuity of healthcare by developing primary care and optimizing integrated service networks.
Study Design, Sample, and Data Collection
The study was cross-sectional. Participants were 18–70 years old and diagnosed with schizophrenia spectrum disorders or other conditions, including mood, anxiety, obsessive–compulsive, personality, attention-deficit hyperactivity, or stressor-related disorders, according to the DSM-V. Patients too clinically fragile to provide informed consent and complete data collection were excluded, as were those hospitalized during the study period, anyone under involuntary treatment by judicial order, or anyone affected by a severe intellectual disability. Various recruitment strategies were used, including self-referral in response to posters displayed at hospitals or in CLSCs. Data were collected from June 2013 to August 2014. A professional interviewer trained by a research coordinator conducted two 90 min interviews at 1 week intervals with each participant. All participants were required to sign a consent form. The study was approved by the Ethics Board of the Douglas Mental Health University Institute (ref. no. 07/35). Recruitment strategies and data collection are more fully described in Roux et al. (2016).61
Conceptual Framework, Variables, and Instruments
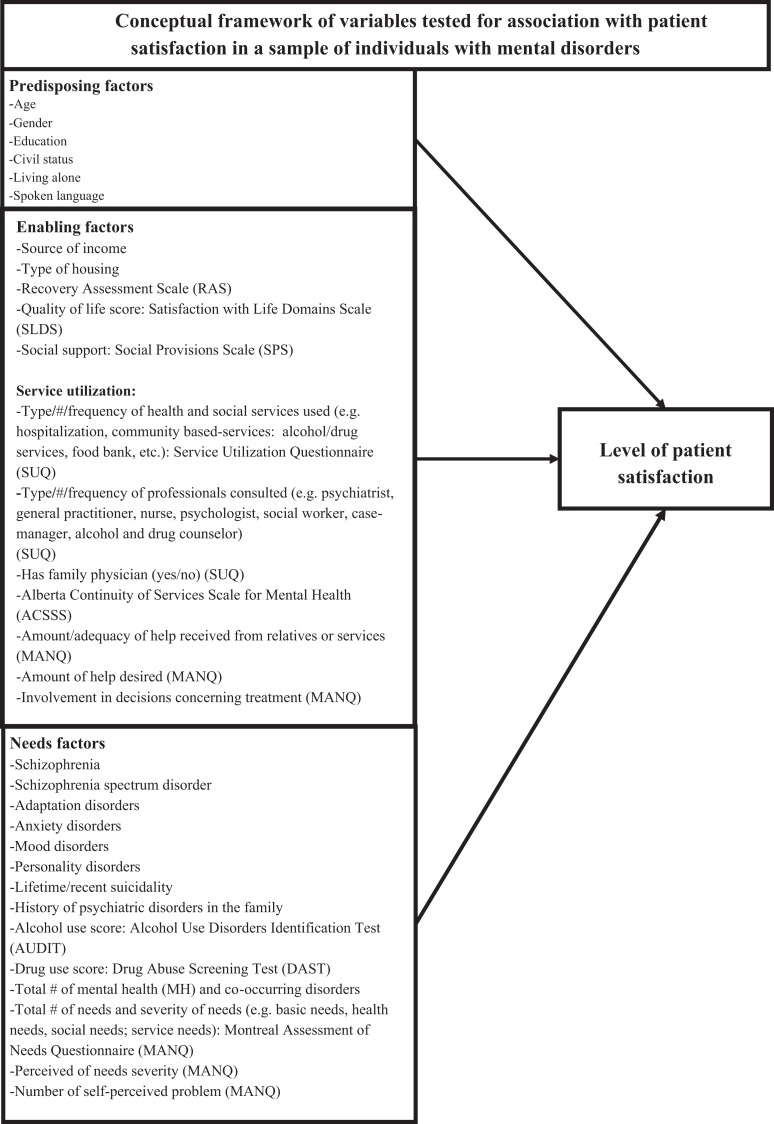
The analytical framework based on Andersen’s Behavioral Model is presented in Figure 1 . Variables were selected for potential association with patient satisfaction, the dependent variable, including those identified in previous studies. Table 1 describes standardized instruments used to measure each variable. The dependent variable was measured with the Service Utilization Questionnaire (SUQ),62 completed by each patient. The SUQ measured the type, number, and frequency of MHS and professionals consulted (e.g. hospitalization; community-based services: crisis centers, day centers, self-help groups, and employment integration programs; as well as psychiatrists, general practitioners [GPs, including family physicians], nurses, psychologists, social workers, case managers, and alcohol and drug counselors). The questionnaire also asked about professionals consulted (e.g. in hospitals, walk-in clinics, medical clinics, CLSCs, and specialized service centers). For every MHS or professional consulted, a single follow-up question on satisfaction was asked: “What is your level of satisfaction with the service you received?” Responses were recorded on a 5-point Likert-type scale ranging from “very unsatisfied” to “very satisfied.” A global score for patient satisfaction with the use of all MHS and professionals was calculated for construction of the dependent variable (range: 3.0 to 59.0).
Figure 1.
Conceptual framework of variables tested for association with patient satisfaction in a sample of individuals with mental disorders.
Table 1.
Instruments.
| Name | Variables | Description | Cronbach’s α |
|---|---|---|---|
| Service Utilization Questionnaire (SUQ) | Type and frequency of professionals and services used in previous 12 months 143 items | Descriptive only | NA |
| Recovery Self-Assessment Scale (RSA) | Personal recovery 32 items | 5-point scale (1 to 5) Rating: 41 to 205; higher = greater perceived recovery | 0.94 |
| Recovery Assessment Scale (RAS) | Personal recovery (dependent variable) (personal confidence and hope, willingness to ask for help, goal and success orientation, reliance on others, and no domination by symptoms) 41 items | 5-point scale (1 to 5) Rating: 41 to 205; higher = greater perceived recovery | 0.93 |
| Satisfaction with Life Domains Scale (SLDS) | Subjective quality of life 20 items | 5-point scale (1 to 5) Rating: 20 to 140; higher = better quality of life | 0.92 |
| Social Provisions Scale (SPS) | Social support (attachment, reassurance of worth, social integration, reliable alliance, guidance, and nurturance) 25 items | 4-point scale (1 to 4) Rating: 25 to 100; higher = more social support | 0.92 |
| Alberta Continuity of Services Scale for Mental Health (ACSS-MH) | Continuity of services (access, team functioning, and interpersonal aspects) 43 items | 5-point scale (1 to 5) Rating: 43 to 215; higher = greater continuity of services | 0.78 to 0.92 |
| Alcohol Use Disorders Identification Test (AUDIT) | Alcohol abuse 10 items | 5-point scale (1 to 5) Rating: 10 to 50; higher = greater level of substance use disorder (SUD) | 0.88 |
| Drug Abuse Screening Test (DAST) | Drug abuse 20 items | 2-point scale (no: 0; yes = 1) Rating: 0 to 20; higher = greater drug abuse | 0.74 |
| Montreal Assessment of Needs Questionnaire (MANQ) | Number of need areas (26 in 5 categories: basic [e.g. food, daytime activities], health [e.g. alcohol use, drug use], functioning [e.g. self-care, money], social [e.g. company, intimate relationships], and services [e.g. benefits, involvement in treatment decisions]) Severity of needs Amount of help received from relatives Amount of help received from services Adequacy of help received (quantity and quality) | 11-point scale Rating: 0 to 10 Min: 0; Max: 260: Severity of needs: higher = higher severity of needs Amount of help received from services: higher = more help received Min: 0; Max: 520: Amount of help received from services: higher = more help received Adequacy of help received from services (0 to 260 for quantity; 0 to 260 for quality): lower = better adequacy | 0.91 |
The independent variables are presented in Figure 1 and were organized according to 3 factors based on the Andersen model.58 Predisposing factors included age, sex, education, civil status, accommodation (living alone), and spoken language. Enabling factors included income source (welfare/other), type of housing, recovery orientation of services and personal recovery, QoL, social support, service utilization (type, number, and frequency), continuity of care, amount and adequacy of help received from relatives and/or services, amount of help desired, and involvement in treatment decisions. Recovery orientation of services was evaluated with the Recovery Self-Assessment Scale, revised person-in-recovery version (RSA; 32 items, 5-point Likert-type scale responses, Cronbach’s α = 0.94),63 whereas personal recovery was assessed with the Recovery Assessment Scale (RAS; 41 items, 5-point Likert-type scale responses, Cronbach’s α = 0.76–0.97).64 QoL was assessed with the Satisfaction with Life Domains Scale (SLDS; 20 items, 7 Likert-type scale response levels, Cronbach’s α = 0.92),65 and social support with the Social Provisions Scale (SPS; Cronbach’s α = 0.92).66 Continuity of care was measured with the Alberta Continuity of Services Scale for MH (ACSS-MH; 43 items, 5-point Likert-type scale responses, Cronbach’s α = 0.78–0.92),67 whereas adequacy of help, help desired, and involvement in treatment were assessed using the Montreal Assessment of Needs Questionnaire (MANQ; based on 26 areas of need and scored with 11 Likert-type scale response levels, Cronbach’s α = 0.70–0.73).68 The MANQ was derived from the Camberwell Assessment of Needs (CAN).69
Needs factors included diagnosis, number of MDs and co-occurring disorders, lifetime and recent suicidality, family history of MDs, and both number and severity of needs. The Alcohol Use Disorders Identification Test (AUDIT; 10 items, 4-point Likert-type scale responses, Cronbach’s α = 0.88)70 evaluated alcohol consumption and use, whereas the Drug Abuse Screening Test (DAST-20; 20 items, yes/no responses, Cronbach’s α = 0.74)71 evaluated drug use. The number of patient needs and their level of severity were assessed using the MANQ.68
Analyses
Missing values were detected using SPSS’s72 missing value analysis feature, which shows the number of participants with missing values, the total number of missing values, and the pattern of missing values (random vs. systematic). Variables with more than 5% missing were discarded. The few variables with missing values were treated by imputing the most likely value using regression analyses (multiple imputation). We have also tested post-hoc bivariate and multivariate analyses using a database with missing values replaced by mean values, instead of multiple imputations. Using box plot graphs, no outliers were detected. Univariate analyses were run, including frequency distributions for categorical variables, and central tendency measures (mean and standard deviations) for continuous variables. The overall patient satisfaction score was assessed for normality assumptions (skewness and kurtosis). Bivariate analyses were then run using t-test ANOVA, assessing statistical associations between each independent variable separately, and with patient satisfaction (α value at p = 0.10). Variables found to be significant were used to build an adjusted multiple linear regression model (α value at p = 0.05). The model was assessed for the total variance explained and goodness of fit. SPSS 24th edition was used to run analyses.72
Results
Overall, 339 participants were recruited for a response rate of 81.2%. After removing missing values, this study included 325 patients. Comparative analyses between respondents and nonrespondents with regard to age and gender yielded nonsignificant results (Age: ANOVA t-test: F=620; P=0.453; Gender: Pearson χ2 = 0.522; P = 0.829). Mean patient age ( Table 2 ) was 48 years (SD: 12), and participants were equally divided by gender. Most were single (85%), and 43% reported living alone. Fewer than half had more than a high school education (47%), and 83% lived in autonomous (nonsupervised) housing. The most prevalent MDs were mood disorders (44%), schizophrenia (30%), personality disorders (29%), and anxiety disorders (19%).
Table 2.
Participant Characteristics (N = 325).
| n/Mean | %/SD | Min | Max | |||
|---|---|---|---|---|---|---|
| Predisposing factors | Age (Mean, SD) | 48.30 | 11.72 | 19.00 | 95.00 | |
| Gender (n. %) | Females | 163 | 50.15 | |||
| Education (n. %) | Secondary or less | 174 | 53.54 | |||
| Civil status (n. %) | Single | 275 | 84.62 | |||
| Living alone (n. %) | Yes | 139 | 42.77 | |||
| Spoken language (n. %) | French | 259 | 79.69 | |||
| English | 51 | 15.69 | ||||
| Other | 15 | 4.62 | ||||
| Enabling factors | Source of income (n. %) | Welfare | 163 | 50.15 | ||
| Type of housing (n. %) | Autonomous | 271 | 83.38 | |||
| Amount of help desired (rating: 0–260) | 42.13 | 32.80 | 0.00 | 180.00 | ||
| Total help received from services (rating: 0–260) | 27.35 | 22.54 | 0.00 | 140.00 | ||
| Total help received from relatives (rating: 0–260) | 23.26 | 23.86 | 0.00 | 111.00 | ||
| Total help received from relatives and services (rating: 0–520) | 50.61 | 39.34 | 0.00 | 216.00 | ||
| Adequacy of help received from services and relatives (rating: 0–520) | 70.25 | 53.17 | 0.00 | 282.00 | ||
| Services utilization | Community-based services visited (n. %) | Crisis center | 18 | 5.54 | ||
| Women help center | 7 | 2.15 | ||||
| Drug detox center | 10 | 3.08 | ||||
| Alcohol detox center | 12 | 3.69 | ||||
| Game addiction treatment center | 2 | 0.62 | ||||
| Violence help center | 2 | 0.62 | ||||
| Help group center | 74 | 22.77 | ||||
| Day center | 81 | 24.92 | ||||
| Human rights help center | 31 | 9.54 | ||||
| Community follow-up center | 65 | 20 | ||||
| Job integration center | 49 | 15.08 | ||||
| Community treatment center | 23 | 7.08 | ||||
| Help for accommodation center | 35 | 10.77 | ||||
| Community crisis center | 54 | 16.62 | ||||
| Food bank | 97 | 29.85 | ||||
| Hospitalization (n. %) | 72 | 22.15 | ||||
| Has a family physician (n. %) | 275 | 84.62 | ||||
| Mental health professionals (MHPs) consulted (n. %) | Psychiatrist | 241 | 74.15 | |||
| General practitioner | 97 | 29.85 | ||||
| Case manager | 163 | 50.15 | ||||
| Nurse | 206 | 63.38 | ||||
| Social worker | 167 | 51.38 | ||||
| Psychologist | 73 | 22.46 | ||||
| Alcohol and drug counselor | 19 | 5.85 | ||||
| Number of services used (Mean, SD) | 4.23 | 1.62 | 1.00 | 9.00 | ||
| Frequency of visits to MHS (Mean, SD) | 94.57 | 157.83 | 0.00 | 1046.00 | ||
| Number of visits to community-based services (Mean, SD) | 1.52 | 1.59 | 0.00 | 8.00 | ||
| Number of MHPs consulted (Mean, SD) | 3.29 | 1.10 | 0.00 | 6.00 | ||
| Number of case manager follow-ups per year (Mean, SD) | 11.38 | 27.80 | 0.00 | 216.00 | ||
| Continuity of care – Alberta Continuity of Services Scale (ACSS) for Mental Health (Mean, SD; rating: 0–215) | 132.29 | 16.00 | 67.00 | 195.00 | ||
| Recovery Self-Assessment Scale (RAS) score (Mean, SD) | 164.62 | 23.49 | 41.00 | 310.38 | ||
| Global patient satisfaction score (Mean, SD) | 4.11 | 0.62 | 2.00 | 5.00 | ||
| Needs factors | Number of needs (rating: 0–26) | 8.47 | 4.43 | 0.00 | 21.00 | |
| Total score of needs severity (rating: 0–260) | 48.42 | 31.74 | 0.00 | 143.00 | ||
| Mental disorders (n. %) | Adaptation disorder | 30 | 9.23 | |||
| Recent suicidal ideations | 37 | 11.38 | ||||
| Schizophrenia spectrum | 26 | 8 | ||||
| Schizophrenia | 97 | 29.85 | ||||
| Anxiety disorder | 61 | 18.77 | ||||
| Personality disorder | 93 | 28.62 | ||||
| Attention deficit disorder | 16 | 4.92 | ||||
| Delusion disorder | 24 | 7.38 | ||||
| Mood disorder | 143 | 44 | ||||
| Number of mental disorders (Mean, SD) | 1.82 | 1.07 | 0.00 | 6.00 | ||
| Alcohol Use Disorders Identification Test (AUDIT) score (Mean, SD; rating: 0–50) | 5.16 | 6.42 | 0.00 | 37.00 | ||
| Drug Abuse Screening Test (DAST) score (Mean, SD; rating: 1–20) | 2.76 | 2.53 | 0.00 | 15.00 | ||
| Number of somatic disorders (Mean, SD) | 2.43 | 1.94 | 0.00 | 12.00 | ||
| Has any somatic disorder (Mean, SD) | 266 | 81.85 | ||||
All participants had used at least 1 MHS or professional in the previous 12 months; 85% reported having a family physician, and 22% had been hospitalized ( Table 2 ). Patients had visited more than 4 MHS and consulted 3 MH professionals, on average, in the previous year, mainly psychiatrists (74%), nurses (63%), and social workers (51%). The most frequently visited community services were food banks (30%), day centers (25%), and organizations offering self-help groups (23%). Psychiatrists, psychologists, and nurses were most often consulted in hospitals; GPs in private medical clinics; social workers in CLSCs; and alcohol or drug counselors in addiction rehabilitation centers (data not shown). The global patient satisfaction score ranged from 2.0 to 5.0 with a mean of 4.11, and it was normally distributed (skewness: 0.369; kurtosis: 0.320).
Variables Associated with Satisfaction
Variables associated with overall patient satisfaction in the bivariate analysis are presented in Table 3 . The multiple linear regression model built from the bivariate results yielded a total explained variance of 28% and had acceptable goodness of fit. With regard to enabling factors ( Table 4 ), continuity of care (p < 0.001), having a case manager (p = 0.034), and help received from services (p = 0.048) were positively associated with patient satisfaction, whereas hospitalization was negatively associated (p < 0.001). Need factors produced 1 variable negatively associated with patient satisfaction: number of needs (p < 0.001). No predisposing variables were related to satisfaction.
Table 3.
Satisfaction: Bivariate Analyses.
| Unstandardized Coefficients | Standardized Coefficients | ||||
|---|---|---|---|---|---|
| Variables | B | SE | P_value | β | |
| Predisposing factors | Living alone (Yes/No) | −0.136 | 0.069 | 0.049 | −0.108 |
| Enabling factors | Amount of help desired | −0.006 | 0.001 | 0.001 | −0.302 |
| Total help received from services | −0.003 | 0.001 | 0.013 | −0.118 | |
| Total help received from relatives | −0.003 | 0.001 | 0.045 | −0.100 | |
| Total help received from relatives and services | −0.002 | 0.001 | 0.007 | −0.128 | |
| Having a case manager (Yes/No) | 0.129 | 0.070 | 0.064 | 0.103 | |
| Number of mental health professionals (MHPs) consulted | −0.048 | 0.019 | 0.014 | −0.124 | |
| Number of visits to community-based services | −0.053 | 0.021 | 0.011 | −0.136 | |
| Continuity of care – Alberta Continuity of Services Scale (ACSS) for Mental Health | 0.015 | 0.002 | 0.001 | 0.373 | |
| Recovery Self-Assessment Scale (RAS) | 0.004 | 0.002 | 0.020 | 0.159 | |
| Hospitalization (Yes/No) | −0.321 | 0.085 | 0.001 | −0.214 | |
| Needs factors | Number of needs | −0.049 | 0.007 | 0.001 | −0.349 |
| Total score of needs severity | −0.007 | 0.001 | 0.001 | −0.341 | |
| Number of mental disorders | −0.078 | 0.035 | 0.027 | −0.133 | |
| Anxiety disorder | −0.187 | 0.085 | 0.028 | −0.117 | |
| Personality disorder | −0.160 | 0.070 | 0.023 | −0.116 | |
| Attention deficit disorder | −0.313 | 0.131 | 0.017 | −0.109 | |
Table 4.
Variables Associated with Satisfaction: Multiple Linear Regression Model.
| Model | Coefficient | SE | P_value | 95% Confidence interval | ||
|---|---|---|---|---|---|---|
| Enabling factors | Continuity of care − Alberta Continuity of Services Scale (ACSS) for Mental Health | 0.011 | 0.002 | 0.001 | 0.008 | 0.015 |
| Having a case manager (Yes/No) | 0.128 | 0.060 | 0.034 | 0.010 | 0.246 | |
| Total help received from services | 0.003 | 0.002 | 0.048 | 0.000 | 0.007 | |
| Number of mental health professionals (MHPs) consulted | 0.011 | 0.021 | 0.605 | −0.030 | 0.051 | |
| Hospitalization (Yes/No) | −0.366 | 0.088 | 0.001 | −0.540 | −0.193 | |
| Needs factors | Number of needs | −0.047 | 0.009 | 0.001 | −0.065 | −0.028 |
| Anxiety disorder | −0.102 | 0.073 | 0.159 | −0.244 | 0.040 | |
R 2 = 0.278; adj_R 2 = 0.262; P < 0.001.
Discussion
This study was the first to assess patient satisfaction with MHS based on Andersen’s Behavioral Model. Our results demonstrated a high level of patient satisfaction, revealing 5 variables associated with patient satisfaction and 2 marginally significant variables. The global mean score for patient satisfaction in our study was similar to results in most other studies.13,19,38,40,37 In previous studies, however, satisfaction scores have generally been based on single services, programs, and professionals, and studies were based on particular clinical populations. By contrast, our results reflect the evaluation of patient satisfaction among a variety of services and professionals. Our model also established that enabling factors were most strongly associated with patient satisfaction, which invalidates our research hypothesis. This result differs from previous findings in studies using the Andersen model,73–75 in which needs factors were most promising as potential predictors of service use. Yet it should be noted that these studies focused on the utilization of MHS without considering patient satisfaction in the analysis.
Continuity of care and having a case manager emerged as the most important variables among the enabling factors. Continuity of care is a multidimensional concept that takes in a number of care-related dimensions, such as delivery, accessibility, and enduring relationships between patient and professional.76,77 Care is individualized in the context of a long-term treatment plan that encompasses multiple services and service providers as required.77 Adequate continuity of care insures a seamless transition between services as needs and problems evolve, in particular for patients with chronic conditions, and also tends to reduce acute MH interventions.78 Continuity of care was also found to enhance QoL and community functioning, while reducing symptom severity and increasing patient satisfaction.79,80 The case manager ensures continuity of care and facilitates more frequent and flexible follow-up, offering support to patients as well as a bridge between service delivery and holistic patient needs.25,78,81
Help received from services (enabling factors) was also related to patient satisfaction. Patients with MDs have multiple biopsychosocial needs that services must address. Our study used a validated tool to measure patient needs, for instance in the areas of self-care, food, daytime activities, money, adaptation to stress, social exclusion, and job integration. Findings revealed that help received from health and social services that contributed to meeting daily needs or to social life was particularly important for increasing satisfaction, particularly among patients with severe MDs or serious problems in various areas (e.g. physical health, daytime activities, and food).82 The responsiveness of services throughout the entire spectrum of needs is important for facilitating recovery and community integration, reducing unmet needs, and increasing patient satisfaction with MHS.16 According to the American Psychiatry Association (APA),83 diversified MHS, for example medication-based treatment in combination with psychotherapy, reinforces recovery for patients with moderate or severe depression. Others studies have noted that patient satisfaction increases when treatments are integrated into various MHS, both inside and outside of hospitals, or in multidisciplinary teams.14,40
By contrast, patients with severe or chronic MDs, with multiple unmet needs, or lacking good case management have a greater likelihood of hospitalization. Patients with MDs are recognized as high service users, particularly in emergency departments, or tend to consult hospital-based professionals during crises.84 Our study suggested that hospitalization in the previous year led to greater dissatisfaction with MHS. Many studies reported that receiving hospital inpatient services or compulsory treatment during hospitalization4,24,40 significantly reduced patient satisfaction. Patients with MDs preferred to receive local outpatient services40 or community-oriented approaches and crisis intervention outside the hospital,14 because these services could be integrated into daily routines, provide more information about health status, and ensure better long-term follow-up.44
Having to resort to hospitalization reflects a lack of service effectiveness in meeting chronic or severe needs among patients. Studies illustrate that, as mentioned, patients with MDs have multiple needs that services must address. As this study highlights, the more patients with MDs fail to receive support in their various spheres of life, the more and the greater their dissatisfaction with MHS received.1,2 This result is consistent with literature claiming that reductions in the number of needs among patients with MDs increase compliance with treatment, recovery, QoL, and satisfaction with services.6,7,16–18 Most studies have shown that the most serious patient needs are correspondingly difficult to meet.16,73 Lack of specialized services in specific areas, and weak coordination among MHS and other health or social services,65 may explain the difficulty in reducing unmet needs. Moreover, some patients have needs that are both serious and recurrent, and are likely viewed as “unmeetable.”16 Unmet needs have been linked to decreased recovery and QoL among patients, and, by extension, lower patient satisfaction with MHS.7,16
Limitations
This study has limitations that should be noted. First, as a cross-sectional study, causal inferences about the findings cannot be made. Second, because the sample was not randomly selected, satisfaction scores should be interpreted with caution. Our results, however, remain consistent with the literature. Third, our study analyzed satisfaction based on a single question measured with a 5-point Likert-type scale, a strategy that did not allow us to investigate subdimensions of satisfaction, as in certain other studies that used standardized questionnaires. Yet patient satisfaction as analyzed in the present study included a broad range of services and professionals consulted during a 12-month period, as well as a full range of MH diagnoses, which would have largely offset this limitation and provided a robust analysis of overall patient satisfaction with MHS. Fourth, this study did not assess satisfaction within specific settings, such as community organizations or hospitals, nor were variables specifically related to patient satisfaction evaluated. These issues could provide a topic for further research. Moreover, the context of this study, including 4 local MH networks, may limit the generalizability of the findings. Our model would require further testing in other healthcare systems. Finally, the results may not be applicable to samples based on single MDs (e.g. schizophrenia only).
Conclusion
This study is the first to evaluate overall patient satisfaction with MHS among adults representing a diverse clinical population from 4 MH service networks, and to simultaneously test multiple variables associated with patient satisfaction using Andersen’s Behavioral Model. The high level of patient satisfaction that emerged from our analysis suggests that patients are generally satisfied with MHS, in particular when they received good continuity of care and well-managed and frequent service delivery in relation to their needs. Case management and assertive community treatment should be better deployed to respond more adequately to the diverse biopsychosocial needs of patients with MDs. By contrast, dissatisfaction was observed among patients presenting serious unmet needs and those hospitalized. Findings highlight the importance of attending to these variables in providing care as a way of improving patient satisfaction with MHS and with their recovery.
Acknowledgments
We would like to thank the coinvestigators and patients who participated in this research.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) declared receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Fonds de la recherche en santé du Québec (FRSQ; grant no. 22367); we gratefully acknowledge the support of this agency.
References
- 1. Urben S, Gloor A, Baier V, et al. Patients’ satisfaction with community treatment: a pilot cross-sectional survey adopting multiple perspectives. J Psychiatr Mental Health Nurs. 2015;22(9):680–687. [DOI] [PubMed] [Google Scholar]
- 2. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286–292. [DOI] [PubMed] [Google Scholar]
- 3. Bener A, Ghulum S. Gender difference on patients’ satisfaction and expectation towards mental health care. Niger J Clin Pract. 2013:16(3):285–291. [DOI] [PubMed] [Google Scholar]
- 4. Kuosmanen L, Hätönen H, Jyrkinen AR, et al. Patient satisfaction with psychiatric inpatient care. J Adv Nurs. 2006:55(6):655–663. [DOI] [PubMed] [Google Scholar]
- 5. de Hann L, Kramer L, van Raay B, et al. Priorities and satisfaction on the help needed and provided in a first episode of psychosis. A survey in five European Family Associations. Eur Psychiatry. 2002;17(8):425–433. [DOI] [PubMed] [Google Scholar]
- 6. Soergaard KW, Nivison M, Hansen V, et al. Treatment needs and acknowledgement of illness – importance for satisfaction with psychiatric inpatient treatment. BMC Health Serv Res. 2008;8:103 doi:10.1186/1472-6963-8-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blenkiron P, Hammill CA. What determines patients’ satisfaction with their mental health care and quality of life? Postgrad Med J. 2003;79(932):337–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rosenheck R, Wilson NJ, Meterko M. Influence of patient and hospital factors on consumer satisfaction with inpatient mental health treatment. Psychiatr Serv. 1997;48(12):1553–1561. [DOI] [PubMed] [Google Scholar]
- 9. Yimer S, Yohannis Z, Getinet W, et al. Satisfaction and associated factors of outpatient psychiatric service consumers in Ethiopia. Patient Prefer Adherence. 2016;10:1847–1852 Published online 2016 Sep 19. doi:10.2147/PPA.S115767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim G, Parton JM, Ford KL, et al. Geographic and racial-ethnic differences in satisfaction with and perceived benefits of mental health services. Psychiatr Serv. 2014;65(12):1474–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Köhler S, Unger T, Hoffmann S, et al. Patient satisfaction with inpatient psychiatric treatment and its relation to treatment outcome in unipolar depression and schizophrenia. Int J Psychiatry Clin Pract. 2015;19(2):119–123. [DOI] [PubMed] [Google Scholar]
- 12. Gebhardta S, Wolakb AM, Hubera MT. Patient satisfaction and clinical parameters in psychiatric inpatients—the prevailing role of symptom severity and pharmacologic disturbances. Compr Psychiatry. 2013;54(1):53–60. [DOI] [PubMed] [Google Scholar]
- 13. Eytan A, Bovet L, Gex-Fabry M, et al. Patients’ satisfaction with hospitalization in a mixed psychiatric and somatic care unit. Eur Psychiatry. 2004;19(8):499–501. [DOI] [PubMed] [Google Scholar]
- 14. Ruggeri M, Salvi G, Perwanger V, et al. Satisfaction with community and hospital-based emergency services amongst severely mentally ill service users A comparison study in South-Verona and South-London. Soc Psychiatry Psychiatr Epidemiol. 2006;41(4):302–309. [DOI] [PubMed] [Google Scholar]
- 15. Katsakou C, Bowers L, Amos Y, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286–292. [DOI] [PubMed] [Google Scholar]
- 16. Fleury MJ, Bamvita JM, Grenier G, et al. Adequacy of help received by individuals with severe mental disorders after a major healthcare reform in Quebec: predictors and changes at 5-years follow-up. Adm Policy Mental Health. 2016;43(5):799–812. [DOI] [PubMed] [Google Scholar]
- 17. Broadbent E, Kydd R, Sanders D, et al. Unmet needs and treatment seeking in high users of mental health services: role of illness perceptions. Aust N Z J Psychiatry. 2008;42(2):147–153. [DOI] [PubMed] [Google Scholar]
- 18. Piat M, Sabetti J, Bloom D. The transformation of mental health services to a recovery-oriented system of care: Canadian decision maker perspectives. Int J Soc Psychiatry. 2010;56(2):168–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zahid MA, Ohaeri JU, Al-Zayed AA. Factors associated with hospital service satisfaction in a sample of Arab subjects with schizophrenia. BMC Health Serv Res. 2010;10:294 https://doi.org/10.1186/1472-6963-10-294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kitts RL, Gallagher K, Ibeziako P, et al. Parent and young adult satisfaction with psychiatry consultation services in a children’s hospital. Psychosomatics. 2013;54(6):575–584. [DOI] [PubMed] [Google Scholar]
- 21. Lee J, Korczak D. Factors associated with parental satisfaction with a Pediatric Crisis Clinic (PCC). J Can Acad Child Adolesc Psychiatry. 2014;23(2):118–127. [PMC free article] [PubMed] [Google Scholar]
- 22. Mohamed EY, Sami W, Alotaibi A, et al. Patients’ satisfaction with primary health care centers’ services, Majmaah, Kingdom of Saudi of Saudi Arabia. Int J Health Sci. 2015;9(2):163–170. [PMC free article] [PubMed] [Google Scholar]
- 23. Ruggeri M, Lasalvia A, Salvi G, et al. Applications and usefulness of routine measurement of patients satisfaction with community-based mental health care. Acta Psychiatr Scand. 2007;116(437):53–65. [DOI] [PubMed] [Google Scholar]
- 24. McCullum SL, Andrews JM, Gaughwin MD, et al. Patient satisfaction with treatment for alcohol use disorders: comparing patients with and without severe mental health symptoms. Patient Prefer Adherence. 2016;10:1489–1500. doi:10.2147/PPA.S92902. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kasprov WJ, Frisman L, Rosenheck RA. Homeless veterans’ satisfaction with residential treatment. Psychiatr Serv. 1999;50(4):540–545. [DOI] [PubMed] [Google Scholar]
- 26. Lanfredi M, Candini V, Buizza C, et al. The effect of service satisfaction and spiritual well-being on the quality of life of patients with schizophrenia. Psychiatry Res. 2014;216(2):185–191. [DOI] [PubMed] [Google Scholar]
- 27. Ruggeri M, Nosè M, Bonetto C, et al. Changes and predictors of change in objective and subjective quality of life: multiwave follow-up study in community psychiatric practice. Br J Psychiatry. 2005;187:121–130. [DOI] [PubMed] [Google Scholar]
- 28. Fitzgerald PB, de Castella AR, Filia K, et al. A longitudinal study of patient-and observer-rated quality of life in schizophrenia. Psychiatry Res. 2003;119(1-2):55–62. [DOI] [PubMed] [Google Scholar]
- 29. Lam JA, Rosenheck RA. Correlates of improvement in quality of life among homeless persons with serious mental health illness. Psychiatr Serv. 2000;51(1):116–118. [DOI] [PubMed] [Google Scholar]
- 30. Hansson L, Sandlund M, Bengtsson-Tops A, et al. The relationship of needs and quality of life in persons with schizophrenia living in the community. A Nordic multi-center study. Nord J Psychiatry. 2003;57(1):5–11. [DOI] [PubMed] [Google Scholar]
- 31. Fleury MJ, Grenier G, Bamvita JM, et al. Adequacy of help received among individuals with severe mental disorders. Adm Policy Ment Health. 2014;41(3):302–316. [DOI] [PubMed] [Google Scholar]
- 32. Holikati PC, Kar N, Mishra A, et al. A study on patient satisfaction with psychiatric services. Indian J Psychiatry. 2012;54(4):327–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kapp C, Perlini T, Jeanneret T, et al. , Identifying the determinants of perceived quality in outpatient child and adolescent mental health services from the perspectives of parents and patients. Eur Child Adolesc Psychiatry. 2017;4(05):1–9. [DOI] [PubMed] [Google Scholar]
- 34. de Lima Silva V, de Medeiros CA, Guerra GC, et al. Quality of Life, Integrative Community Therapy, Family Support, and Satisfaction with Health Services Among Elderly Adults with and without Symptoms of Depression. Psychiatr Q. 2017;88(2):359–369. doi:10.1007/s11126-016-9453-z. [DOI] [PubMed] [Google Scholar]
- 35. Caqueo-Urızar A, Gutierrez-Maldonado J. Satisfaction with mental health services in a Latin American community of carers of patients with schizophrenia. Community Ment Health J. 2009;45(4):285–289. [DOI] [PubMed] [Google Scholar]
- 36. Smith D, Roche E, O’Loughlin K, et al. Satisfaction with services following voluntary and involuntary admission. J Ment Health, 2014;23(1):38–45. [DOI] [PubMed] [Google Scholar]
- 37. Krupchanka D, Khalifeh H, Abdulmalik J, et al. Satisfaction with psychiatric in-patient care as rated by patients at discharge from hospitals in 11 countries. Soc Psychiatry Psychiatr Epidemiol. 2017;52(8):989–1003. [DOI] [PubMed] [Google Scholar]
- 38. Jabbar, et al. What do you think of us? Evaluating patient knowledge of and satisfaction with a psychiatric outpatient service. Ir J Med Sci. 2011;180(1):195–201. [DOI] [PubMed] [Google Scholar]
- 39. Eklund M, Sandlund M. Predictors of valued everyday occupations, empowerment and satisfaction in day centres: implications for services for persons with psychiatric disabilities. Scand J Caring Sci. 2014;28(3):582–590. [DOI] [PubMed] [Google Scholar]
- 40. Ruud T, Aarre TF, Broeskov B, Husvåg PS, Klepp R, Kristiansen SA, Sandvik J. Satisfaction with primary care and mental health care among individuals with severe mental illness in a rural area: a seven-year follow-up study of a clinical cohort. Int J Ment Health Syst. 2016;10:33 doi:10.1186/s13033-016-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Klingaman EA, Park SG, Fang L, et al. Consumer satisfaction with psychiatric services: the role of shared decision making and the therapeutic relationship. Psychiatr Rehabil J. 2015;38(3):242–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Keung Wong DF, Kit Lam AY, Chan SK, et al. Quality of life of caregivers with relatives suffering from mental illness in Hong Kong: roles of caregiver characteristics, caregiving burdens, and satisfaction with psychiatric services. Health Qual Life Outcomes. 2012;10:15 Published online 2012 Jan 31. doi:10.1186/1477-7525-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lara-Cabrera ML, Salvesen O, Nesset MB, et al. The effect of a brief educational programme added to mental health treatment to improve patient activation: a randomized controlled trial in community mental health centres. Patient Educ Couns. 2016;99(5):760–768. [DOI] [PubMed] [Google Scholar]
- 44. Hendersen C, Phelan M, Loftus L, et al. Comparison of patient satisfaction with community-based vs. hospital services. Acta Psychiulr Scand. 1999;99(3):188–195. [DOI] [PubMed] [Google Scholar]
- 45. Whitley R, Wang JW, Fleury MJ, et al. Mental health status, health care utilisation, and service satisfaction among immigrants in Montreal: an epidemiological comparison. Can J Psychiatry. 2017;62(8):570–579. doi:10.1177/0706743716677724. Epub 2016 Nov 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Perreault M, Leichner P. Patient satisfaction with outpatient psychiatric services. Eval Program Plann. 1993;16:109–118. [Google Scholar]
- 47. Perreault M, Rogers WL, Leichner P, et al. Patients’ requests and satisfaction with services in an outpatient psychiatric setting. Psychiatr Serv. 1996;47(3):287–292. [DOI] [PubMed] [Google Scholar]
- 48. Perreault M, Pawliuk N, Veilleux R, et al. Qualitative assessment of mental health services satisfaction: strengths and limitations of a self-administered procedure. Commun Mental Health J. 2006;42(3):233–242. [DOI] [PubMed] [Google Scholar]
- 49. Ruggeri M, Dall’’Agnola R. The development and use of the Verona Expectations for Care Scale (VECS) and the Verona Service Satisfaction Scale (VSSS) for measuring expectations and satisfaction with community-based psychiatric services in patients, relatives and professionals. Psychol Med. 1993;23(2):511–523. [DOI] [PubMed] [Google Scholar]
- 50. Ruggeri M, Dall’Agnola R, Agostini C, et al. Acceptability, sensitivity and content validity of the VECS and VSSS in measuring expectations and satisfaction in psychiatric patients and their relatives. Soc Psychiatry Psychiatr Epidemiol. 1994;29(6):265–276. [DOI] [PubMed] [Google Scholar]
- 51. Ruggeri M, Lasalvia A, Dall’Agnola R, et al. Development, internal consistency and reliability of the Verona Service Satisfaction Scale--European version. EPSILON study 7. european psychiatric services: inputs linked to outcome domains and needs. Br J Psychiatry Suppl. 2000;(39):s41–s48. [DOI] [PubMed] [Google Scholar]
- 52. Greenfield TK, Attkisson CC. Steps toward a multifactorial satisfaction scale for primary care and mental health services. Eval Program Plann. 1989;12:271–278. [Google Scholar]
- 53. Greenfield TK, Attkisson CC, The UCSF. Client Satisfaction Scales: II. The Service Satisfaction Scale-30 In: Maruish M, editor. The use of psychological testing for treatment planning and outcome assessment, 3rd ed. Mahwah (NJ; ): Lawrence Erlbaum Associates; 2004. [Google Scholar]
- 54. Larsen DL, Attkisson CC, Hargreaves WA, et al. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. [DOI] [PubMed] [Google Scholar]
- 55. Paludetto M, Camuccio CA, Cutrone F, et al. Can we have routine measurement of patient satisfaction in acute psychiatric settings? A cross sectional study. Arch Psychiatr Nurs. 2015;29(6):447–453. [DOI] [PubMed] [Google Scholar]
- 56. Barrett B, Young MS, Teague GB, et al. Recovery orientation of treatment, consumer empowerment, and satisfaction with services: a mediational model. Psychiatr Rehabil J. 2010;34(2):153–156. [DOI] [PubMed] [Google Scholar]
- 57. Gigantesco A, Picardi A, Chiaia E, et al. Patients’ and relatives’ satisfaction with psychiatric services in a large catchment area in Rome. Eur Psychiatry. 2002;17(3):139–147. [DOI] [PubMed] [Google Scholar]
- 58. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 59. Fleury MJ, Grenier G, Vallée C, et al. Implementation of the Quebec mental health reform (2005-2015). BMC Health Serv Res. 2016;16:586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fleury MJ, Grenier G, Vallée C, et al. Implementation of integrated service networks under the Quebec Mental Health Reform: facilitators and barriers associated with different territorial profiles. Int J Integr Care. 2017;17(1):1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Roux P, Passerieux C, Fleury MJ. Mediation analysis of severity of needs, service performance and outcomes for patients with mental disorders. Br J Psychiatry. 2016;209(6):511–516. [DOI] [PubMed] [Google Scholar]
- 62. Kessler RC, Calabrese JR, Farley PA, et al. Composite International Diagnostic Interview screening scales for DSM-IV anxiety and mood disorders. Psychol Med. 2013;43(8):1625–1637. [DOI] [PubMed] [Google Scholar]
- 63. O’Connell M, Tondora J, Croog G, et al. From rhetoric to routine: Assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatr Rehabil J. 2005;28(4):378–386. [DOI] [PubMed] [Google Scholar]
- 64. Giffort D, Schmook A, Woody C, et al. Construction of a scale to measure consumer recovery. Springfield (IL: ): Illinois Office of Mental Health; 1995. [Google Scholar]
- 65. Oliver JPJ, Huxley PJ, Priebe S, et al. Measuring the quality of life of severely mentally ill people using the Lancashire Quality of Life Profile. Soc Psychiatry Psychiatr Epidemiol. 1997;32(2):76–83. [DOI] [PubMed] [Google Scholar]
- 66. Caron J, Mercier C, Diaz P, et al. Socio-demographic and clinical predictors of quality of life in patients with schizophrenia or schizo-affective disorder. Psychiatry Res. 2005;137(3):203–213. [DOI] [PubMed] [Google Scholar]
- 67. Durbin J, Goering P, Streiner DL, et al. Continuity of care: Validation of a new self-report measure for individuals using mental health services. J Behav Health Serv Res. 2004;31(3):279–296. [DOI] [PubMed] [Google Scholar]
- 68. Tremblay J, Bamvita JM, Grenier G, et al. Utility of the Montreal assessment of need questionnaire for community mental health planning. J Nerv Mental Dis. 2014;202(9):677–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Slade M, Thornicroft G, Loftus L, et al. CAN camberwell assessment of need. London (GB: ): Gaskell; 1999. [Google Scholar]
- 70. Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56(4):423–432. [DOI] [PubMed] [Google Scholar]
- 71. Cocco KM, Carey KB. Psychometric properties of the drug abuse screening test in psychiatric outpatients. Psychol Assess. 1998;10(4):408–414. [Google Scholar]
- 72. IBM Corp. IBM SPSS Statistics for Windows, Version 24.0 Armonk (NY; ): IBM Corp; 2015. [Google Scholar]
- 73. Fleury MJ, Grenier G, Bamvita JM, et al. Determinants of the utilization of diversified types of professionals for mental health reasons in a Montreal (Canadian) catchment area. Glob J Health Sci. 2012;4(3):13–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Fleury MJ, Grenier G, Bamvita JM, et al. Comprehensive determinants of health service utilization for mental health reasons in a Canadian catchment area. Int J Equity Health. 2012;11(20):2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Fleury MJ, Grenier G, Bamvita JM, et al. Variables Associated With Perceived Unmet Need for Mental Health Care in a Canadian Epidemiologic Catchment Area. Psychiatr Serv. 2015. doi:10.1176/appi.ps.201400363. [DOI] [PubMed] [Google Scholar]
- 76. Joyced A, Wild T, Adair C, et al. Continuity of care in mental health services: toward clarifying the construct. Can J Psychiatry. 2004;49(8):539–550. [DOI] [PubMed] [Google Scholar]
- 77. Bachrach L. Continuity of care and approaches to case management for long-term mentally ill patients. Hosp Community Psychiatry. 1993;44(5):465–468. [DOI] [PubMed] [Google Scholar]
- 78. Poremski D, Wise Harris D, Kahan D, et al. Improving continuity of care for frequent users of emergency departments: service user and provider. Gen Hosp Psychiatry. 2016;40:55–59. Published online 2016 Jan 18. doi:10.1016/j.genhosppsych.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 79. Adair CE, McDougall GM, Mitton CR, et al. Continuity of care and health outcomes among persons with severe mental illness. Psychiatr Serv. 2005;56(9):1061–1069. [DOI] [PubMed] [Google Scholar]
- 80. Burn T, Catty J, White S, et al. Continuity of care in mental health: understanding and measuring a complex phenomenon. Psychol Med. 2009;39:313–323. Published online 2008 Jun 23. doi:10.1017/S0033291708003747. [DOI] [PubMed] [Google Scholar]
- 81. Alonso Suàrez M, Bravo-Ortiz MF, Fernàndez-Liria A, et al. Effectiveness of Continuity-of-Care programs to reduce time in hospital in persons with schizophrenia. Epidemiol Psychiatr Sci. 2011;20(1):65–72. [DOI] [PubMed] [Google Scholar]
- 82. Fleury MJ, Grenier G. Needs and appropriateness of help according to types of professionals and their users. Int J Psychosoc Rehabil. 2007;12:5–22. [Google Scholar]
- 83. The American Psychiatry Association (APA). Practice guideline for the treatment of patients with major depressive disorder 2010. 3rd ed. http://www.psychiatryonline.com/pracGuide/pracGuideTopic_7.aspx. Cited 15 August 2017.
- 84. Lesage A, Vasiliadis H-M, Gagné M-A, et al. Prévalence de la maladie mentale et utilisation des services connexes au Canada: Une analyse des données de l’Enquête sur la santé dans les collectivités canadiennes. Ottawa (Canada: ): Initiative canadienne de collaboration en santé mentale; 2006. [Google Scholar]