Abstract
Objective:
Although evidence suggests that treatment seeking for mental illness has increased over time, little is known about how the health system is meeting the increasing demand for services. We examined trends in physician-based mental health service use across multiple sectors.
Method:
In this population-based study, we used linked health-administrative databases to measure annual rates of mental health–related outpatient physician visits to family physicians and psychiatrists, emergency department visits, and hospitalizations in adults aged 16+ from 2006 to 2014. We examined absolute and relative changes in visit rates, number of patients, and frequency of visits per patient, and assessed temporal trends using linear regressions.
Results:
Among approximately 11 million Ontario adults, age- and sex-standardized rates of mental health–related outpatient physician visits declined from 604.8 to 565.5 per 1000 population over the study period (P trend = 0.04). Over time, the rate of visits to family physicians/general practitioners remained stable (P trend = 0.12); the number of individuals served decreased, but the number of visits per patient increased. The rate of visits to psychiatrists declined (P trend < 0.001); the number of individuals served increased, but the number of visits per patient decreased. Concurrently, visit rates to emergency departments and hospitals increased (16.1 to 19.7, P trend < 0.001 and 5.6 to 6.0, P trend = 0.01, per 1000 population, respectively). Increases in acute care service use were greatest for anxiety and addictions.
Conclusions:
The increasing acute care service use coupled with the reduction in outpatient visits suggest, overall, an increase in demand for mental health care that is not being met in ambulatory care settings.
Keywords: time trends, mental health services, epidemiology
Abstract
Objectif :
Bien que les données probantes suggèrent que la demande de traitement pour la maladie mentale a augmenté avec le temps, nous en savons très peu sur la façon dont le système de santé répond à la demande croissante de services. Nous avons examiné les tendances de l’utilisation des services de santé mentale fournis par les médecins dans de multiples secteurs.
Méthode :
Dans cette étude dans la population, nous avons relié les bases de données administratives de la santé pour mesurer les taux annuels des visites ambulatoires pour santé mentale à des médecins de famille et des psychiatres, aux services d’urgence, et des hospitalisations chez des adultes de plus de 16 ans, de 2006 à 2014. Nous avons examiné les changements absolus et relatifs des taux de visite, du nombre de patients, et de la fréquence des visites par patient, et évalué les tendances temporelles à l’aide de régressions linéaires.
Résultats :
Chez quelque 11 millions d’adultes ontariens, les taux normalisés selon l’âge et le sexe des visites ambulatoires à un médecin pour santé mentale ont chuté de 604,8 à 565,5 par 1 000 de population sur la période de l’étude (ptendance = 0,04). Avec le temps, le taux des visites aux médecins de famille/omnipraticiens est demeuré stable (ptendance = 0,12); le nombre de personnes servies a diminué, mais le nombre de visites par patient a augmenté. Le taux des visites aux psychiatres a diminué (ptendance < 0,001); le nombre de personnes servies a augmenté, mais le nombre de visites par patient a diminué. Parallèlement, les taux de visite aux services d’urgence et dans les hôpitaux ont augmenté (16,1 à 19,7, ptendance < 0,001 et 5,6 à 6,0, ptendance = 0,01 par 1 000 de population, respectivement). Les accroissements de l’utilisation des services de soins actifs étaient surtout pour l’anxiété et les dépendances.
Conclusions :
L’accroissement de l’utilisation des services de soins actifs jumelé à la réduction des visites ambulatoires suggère, généralement, une augmentation de la demande de soins de santé mentale à laquelle les milieux de soins ambulatoires ne peuvent répondre.
Mental illnesses and addiction are common and are associated with substantial disability and reduced quality of life, especially among those who do not receive timely and effective early intervention.1,2 The prevalence of these conditions has remained relatively stable throughout the past decade,3,4 but treatment seeking has increased.3,5,6 This may be attributed to active efforts to raise awareness and reduce stigma for mental illness.7 Unfortunately, many high-income countries are reporting unmet needs for care.5,8,9 Timely access is crucial,10 and there is some concern that emergency departments are becoming the only guaranteed entry point to mental health care.11 Little is known, however, about whether the health system is meeting the increasing demand for mental health services.
Evaluation of trends over time in how mental health services are used can help guide decisions about resource allocation and inform development of new models of care. Internationally, use of mental health services has increased over the past few decades.6 There has been an increase in the number of individuals receiving outpatient services,5,12–14 but there may be a decline in the number of visits per service user.15 In the acute care sector, the literature is mixed. Some studies have reported an increased use of emergency department11,16 and inpatient services,17 while others have reported a decreasing number of psychiatric beds and resultant decline in admission rates.18 Most previous studies have relied on self-report to ascertain service use, but these data are subject to recall and social desirability biases.19 Furthermore, published studies often did not differentiate between service sectors or types of professionals who were delivering mental health care,6,12 or focused on a single outcome in an isolated setting, such as emergency departments or hospitals only.11,16,18
Population-based linked health administrative data provide a unique opportunity to examine trends in mental health service utilization in multiple sectors simultaneously without relying on patient recall. The province of Ontario, the most populous province in Canada, is an ideal setting for such an undertaking, owing to a universal health care system that insures almost 14 million residents.20 Our aim, therefore, was to generate a comprehensive picture of the extent and nature of mental health service utilization in the outpatient and acute care sectors by examining trends in outpatient physician visits, including primary care providers and psychiatrists, as well as visits to the emergency department and hospitalizations.
Method
Setting, Design, and Study Population
In this population-based, repeated cross-sectional study, we examined the physician-based mental health service utilization of all Ontario residents aged 16 to 105 years between January 1, 2006, and December 31, 2014, a timeframe corresponding to the most recent health-administrative data available across all mental health service sectors. The Registered Person’s Database, the central population registry file that enables linkage across population-based health administrative data sets, was used to identify all Ontario residents who are insured under Ontario’s universal health coverage. Health administrative data sets were linked using unique encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences.
Mental Health Services: Data Sources and Definitions
Outpatient physician visits
Mental health–related visits to primary care providers (i.e., family physicians or general practitioners) and psychiatrists were identified from the Ontario Health Insurance Plan database, which contains patient diagnostic codes for physician billings, visits, and consultations. We included all outpatient (office, home, and long-term care) billings made by family physicians or general practitioners with a mental health diagnostic code21 and all outpatient billings made by psychiatrists (for more detail, see Suppl. Table S1). Outpatient mental health–related visits were examined overall and by type of physician provider. Visits to psychologists, social workers, and other community mental health supports were not available in our data, as these services are not typically covered under the Ontario Health Insurance Plan.
Acute care emergency department visits and hospitalizations
Psychiatric emergency department visits were identified from the National Ambulatory Care Reporting System using the International Classification of Diseases, Tenth Revision, with Canadian enhancements (ICD-10-CA). Hospitalizations were identified from the Canadian Institute for Health Information’s Discharge Abstract Database, which uses ICD-10-CA coding for the primary diagnosis field, and the Ontario Mental Health Reporting System, which uses the multiaxial Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). We included any mental health–related diagnoses in the underlying problem field or deliberate self-harm diagnoses in secondary problem fields when there was no primary mental health diagnosis. We further categorized emergency department visits and hospitalizations by the following diagnostic groups: substance-related disorders, schizophrenia, mood disorders, anxiety disorders, and deliberate self-harm (see Suppl. Table S1). Acute care visits were not constructed as mutually exclusive categories; a subset of emergency department visits may have resulted in a hospitalization.
Statistical Analyses
The annual rate of outpatient and acute care service use was defined as the number of visits per 1000 persons in the Ontario population aged 16 to 105 years in a calendar year. We calculated crude and age- and sex-standardized rates using the direct method,22 with 5 age categories (16-24, 25-44, 45-64, 65-84, 85-105 years) and the 2006 Ontario census population as the standard population. Outpatient and acute care visit rates were calculated for the overall population and for males and females separately, and acute care visit rates were further stratified by diagnosis. Nonoverlapping 95% confidence intervals (CIs) for rates indicated a statistically significant difference between strata.
To investigate whether observed changes in visit rates over time were due to changes in the number of unique patients accessing services or the frequency with which services were accessed, or both, we calculated the number of unique patients using services annually and the number of visits per patient. We also calculated the percentage of the adult population accessing each service, defined as unique patients divided by the annual population.
We compared the rates of visits and unique patients in 2006 and 2014 by calculating absolute differences and relative change, expressed as a percentage of the 2006 rate, and tested for statistical significance of trends throughout the study period using P trends derived from unadjusted linear regression models, with year as the independent variable.
Statistical analyses were conducted using SAS statistical software (version 9.4; SAS Institute, Cary, NC). Ethics approval for this study was obtained from the Research Ethics Board at Sunnybrook Health Sciences Centre.
Results
Characteristics of Mental Health–Related Service Use
Among the 11.4 million adults living in Ontario in 2014, there were 1.6 million individuals who accounted for 6.4 million outpatient physician visits for mental health care. Most of these visits were to primary care providers, with a substantial rate of visits to psychiatrists as well (378.4 visits and 180.6 visits per 1000 population, respectively, in 2014). Women had higher rates of outpatient visits to either physician specialty than men (619.5 [95% CI, 618.9-620.2] and 495.0 [95% CI, 494.4-495.6], per 1000 persons, respectively in 2014; see Suppl. Table S2 for more detail). In 2014, there were 217,512 emergency department visits and 67,446 psychiatric hospitalizations observed among 138,723 and 50,919 individuals, respectively. Men had higher rates than women with regards to emergency department visits (20.4 [95% CI, 20.2-20.5] vs. 18.0 [95% CI, 17.9-18.1] per 1000 population) and hospitalizations (6.2 [95% CI, 6.1-6.3] vs. 5.7 [95% CI, 5.6-5.8]). The most common reasons for mental health–related emergency department visits and hospitalizations in 2014 were anxiety disorders (5.9 visits per 1000 population) and mood disorders (1.8 visits per 1000 population), respectively (Suppl. Table S2).
Trends over Time in Mental Health–Related Service Use
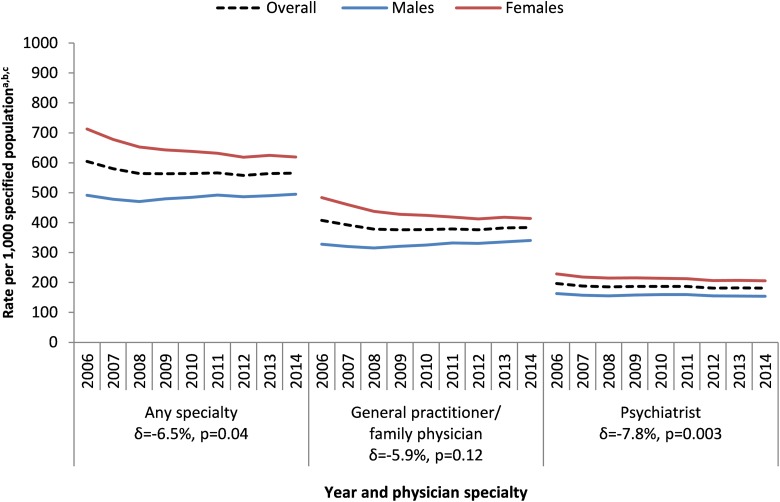
Age- and sex-standardized rates of outpatient physician visits decreased over time, with a 6.5% relative decline between 2006 and 2014 and a significant (P trend = 0.04) declining linear trend throughout the study period (Figure 1). When stratified by physician specialty, standardized visit rates to primary care providers remained stable (P trend = 0.12) while standardized visit rates to psychiatrists declined by 7.8% (P trend = 0.003). Psychiatrists saw 75,912 more unique patients in 2014 than in 2006 (Table 1), a significant increase from 2.9% to 3.3% of the population served by these specialists (P trend < 0.001), but the average number of psychiatrist visits per patient decreased from 6.7 to 5.4 (P trend < 0.001). Conversely, primary care physicians saw 88,439 fewer patients in 2014 than in 2006, a decrease from 14.8% to 12.7% of the population served (P trend < 0.001), while the average number of visits per patient increased from 2.8 to 3.0 (P trend < 0.001). Although crude rates of visits to psychiatrists significantly decreased among both males and females over time (P trend < 0.05), crude rates of visits to primary care providers increased among males by 12.6 visits per 1000 persons but decreased among females by 70.2 visits per 1000 persons (Suppl. Table S2).
Figure 1.
Annual (2006-2014) rates of mental health–related outpatient physician visits, by physician specialty, per 1000 Ontario population aged 16 to 105 years. aOverall rates were age and sex standardized to the 2006 Ontario population using the direct method; rates for males and females are crude (for 95% confidence intervals, see Suppl. Table S2). bDelta (δ) represents the relative change between the 2006 and 2014 overall rates, expressed as a percentage of the 2006 rate. c P values for trend were obtained using unadjusted linear regressions.
Table 1.
Annual Numbers of Mental Health–Related and Addictions-Related Outpatient Physician Visits, Unique Patients Seen, and Percentiles of Visits per Patient among the Ontario Population Aged 16 to 105 Years.
| Year | Population Aged 16-105 | No. of Unique Patients | Percent Patients per Population | No. of visits | Visits per Patient | |||
|---|---|---|---|---|---|---|---|---|
| Mean | 25% Q1 | 50% Median | 75% Q3 | |||||
| Any physician specialty | ||||||||
| 2006 | 10,323,237 | 1,672,068 | 16.2 | 6,243,748 | 3.7 | 1 | 2 | 4 |
| 2007 | 10,437,173 | 1,645,708 | 15.8 | 6,061,141 | 3.7 | 1 | 2 | 3 |
| 2008 | 10,580,179 | 1,626,412 | 15.4 | 5,970,398 | 3.7 | 1 | 2 | 3 |
| 2009 | 10,745,957 | 1,618,031 | 15.1 | 6,054,420 | 3.7 | 1 | 2 | 3 |
| 2010 | 10,876,759 | 1,614,095 | 14.8 | 6,128,057 | 3.8 | 1 | 2 | 4 |
| 2011 | 11,026,486 | 1,617,971 | 14.7 | 6,219,927 | 3.8 | 1 | 2 | 4 |
| 2012 | 11,164,909 | 1,609,264 | 14.4 | 6,190,574 | 3.9 | 1 | 2 | 4 |
| 2013 | 11,293,711 | 1,639,893 | 14.5 | 6,319,587 | 3.9 | 1 | 2 | 4 |
| 2014 | 11,368,477 | 1,632,268 | 14.4 | 6,354,848 | 3.9 | 1 | 2 | 4 |
| Absolute changea | –1.8 | +0.2 | ||||||
| Relative change (δ)b | –11.4% | +4.3% | ||||||
| P trendc | <0.001 | <0.001 | ||||||
| General practitioner/family physician | ||||||||
| 2006 | 10,323,237 | 1,531,977 | 14.8 | 4,212,144 | 2.8 | 1 | 1 | 3 |
| 2007 | 10,437,173 | 1,500,182 | 14.4 | 4,090,756 | 2.7 | 1 | 1 | 3 |
| 2008 | 10,580,179 | 1,473,486 | 13.9 | 4,001,378 | 2.7 | 1 | 1 | 3 |
| 2009 | 10,745,957 | 1,457,658 | 13.6 | 4,037,306 | 2.8 | 1 | 1 | 3 |
| 2010 | 10,876,759 | 1,447,418 | 13.3 | 4,089,538 | 2.8 | 1 | 1 | 3 |
| 2011 | 11,026,486 | 1,442,818 | 13.1 | 4,156,520 | 2.9 | 1 | 1 | 3 |
| 2012 | 11,164,909 | 1,425,100 | 12.8 | 4,164,760 | 2.9 | 1 | 1 | 3 |
| 2013 | 11,293,711 | 1,453,541 | 12.9 | 4,269,373 | 2.9 | 1 | 1 | 3 |
| 2014 | 11,368,477 | 1,443,538 | 12.7 | 4,301,392 | 3.0 | 1 | 1 | 3 |
| Absolute changea | –2.1 | +0.2 | ||||||
| Relative change (δ)b | –14.4% | +8.4% | ||||||
| P trendc | <.001 | <.001 | ||||||
| Psychiatrist | ||||||||
| 2006 | 10,323,237 | 303,485 | 2.9 | 2,031,604 | 6.7 | 1 | 3 | 8 |
| 2007 | 10,437,173 | 306,973 | 2.9 | 1,970,385 | 6.4 | 1 | 3 | 7 |
| 2008 | 10,580,179 | 315,391 | 3.0 | 1,969,020 | 6.2 | 1 | 3 | 7 |
| 2009 | 10,745,957 | 327,314 | 3.0 | 2,017,114 | 6.2 | 1 | 3 | 7 |
| 2010 | 10,876,759 | 339,383 | 3.1 | 2,038,519 | 6.0 | 1 | 3 | 7 |
| 2011 | 11,026,486 | 351,268 | 3.2 | 2,063,407 | 5.9 | 1 | 3 | 7 |
| 2012 | 11,164,909 | 364,070 | 3.3 | 2,025,814 | 5.6 | 1 | 3 | 6 |
| 2013 | 11,293,711 | 374,342 | 3.3 | 2,050,214 | 5.5 | 1 | 3 | 6 |
| 2014 | 11,368,477 | 379,397 | 3.3 | 2,053,456 | 5.4 | 1 | 3 | 6 |
| Absolute changea | +0.4 | –1.3 | ||||||
| Relative change (δ)b | +13.5% | –19.1% | ||||||
| P trendc | <.001 | <.001 | ||||||
aAbsolute change = 2006 estimate – 2014 estimate.
bDelta (δ) represents the relative change between the 2006 and 2014 estimate, expressed as a percentage of the 2006 estimate.
c P values for trend were obtained using unadjusted linear regression, with time as the independent variable.
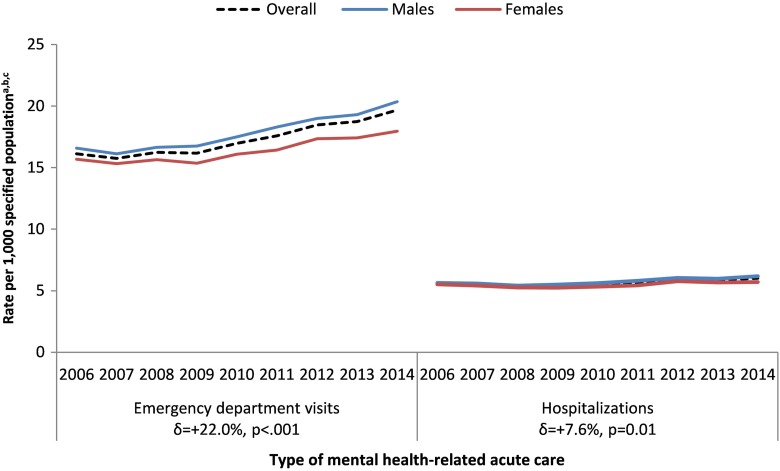
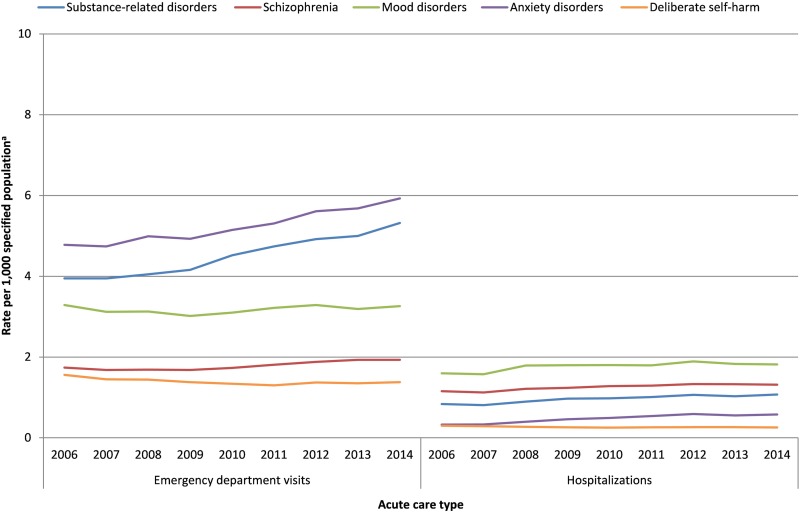
Mental health–related service use in acute care settings increased between 2006 and 2014 (Figure 2). Age- and sex-standardized rates of emergency department visits significantly increased by 22% (P trend < 0.001), from 16.1 to 19.7 per 1000 persons. Similarly, during the same period, the standardized rate of psychiatric hospitalizations increased by 8% from 5.6 to 6.0 per 1000 (P trend = 0.01). The crude rate of emergency department visits increased over time for most mental health conditions (Figure 3; see Suppl. Table S3 for more detail), with the greatest relative increases occurring for substance-related disorders (35%) and anxiety disorders (24%). Between 2006 and 2014, the number of unique patients accessing mental health care in the emergency department and being hospitalized increased by 28,335 and 7,670, respectively. During the same period, the average annual number of emergency department visits per person increased from 1.5 to 1.6 (P trend = 0.002), while the average number of hospitalizations per person remained stable at 1.3 hospitalizations annually, per person (P trend = 0.48; see Table 2).
Figure 2.
Annual (2006-2014) rates of mental health–related acute care visits to the emergency department and hospitalizations, per 1000 Ontario population aged 16 to 105 years. aOverall rates were age and sex standardized to the 2006 Ontario population using the direct method; rates for males and females are crude (for 95% confidence intervals, see Suppl. Table S2). bDelta (δ) represents the relative change between the 2006 and 2014 overall rates, expressed as a percentage of the 2006 rate. c P values for trend were obtained using unadjusted linear regressions.
Figure 3.
Annual (2006-2014) rates of mental health–related acute care visits to the emergency department and hospitalizations, per 1000 Ontario population aged 16 to 105 years, by diagnostic category. aFor 95% confidence intervals around the crude rates by diagnostic category, see Suppl. Table S3.
Table 2.
Annual Numbers of Mental Health–Related and Addictions-Related Emergency Department Visits and Hospitalizations, Unique Patients Seen, and Percentiles of Visits per Patient among the Ontario Population Aged 16 to 105 Years.
| Year | Population Aged 16-105 | No. of Unique Patients | Percent Patients per Population | No. of Visits or Hospitalizations | Visits or Hospitalizations per Patient | |||
|---|---|---|---|---|---|---|---|---|
| Mean | 25% Q1 | 50% Median | 75% Q3 | |||||
| Mental health–related emergency department visits | ||||||||
| 2006 | 10,323,237 | 110,388 | 1.07 | 166,469 | 1.51 | 1 | 1 | 1 |
| 2007 | 10,437,173 | 109,476 | 1.05 | 164,052 | 1.50 | 1 | 1 | 1 |
| 2008 | 10,580,179 | 114,437 | 1.08 | 170,791 | 1.49 | 1 | 1 | 1 |
| 2009 | 10,745,957 | 115,166 | 1.07 | 172,424 | 1.50 | 1 | 1 | 1 |
| 2010 | 10,876,759 | 120,709 | 1.11 | 182,514 | 1.51 | 1 | 1 | 1 |
| 2011 | 11,026,486 | 125,658 | 1.14 | 191,251 | 1.52 | 1 | 1 | 1 |
| 2012 | 11,164,909 | 132,622 | 1.19 | 202,790 | 1.53 | 1 | 1 | 1 |
| 2013 | 11,293,711 | 133,524 | 1.18 | 207,068 | 1.55 | 1 | 1 | 1 |
| 2014 | 11,368,477 | 138,723 | 1.22 | 217,512 | 1.57 | 1 | 1 | 1 |
| Absolute changea | +1.51 | +0.06 | ||||||
| Relative change (δ)b | +14.11% | +3.97% | ||||||
| P trendc | <.001 | .002 | ||||||
| Mental health–related hospitalizations | ||||||||
| 2006 | 10,323,237 | 43,249 | 0.42 | 57,608 | 1.33 | 1 | 1 | 1 |
| 2007 | 10,437,173 | 43,229 | 0.41 | 57,334 | 1.33 | 1 | 1 | 1 |
| 2008 | 10,580,179 | 43,031 | 0.41 | 56,468 | 1.31 | 1 | 1 | 1 |
| 2009 | 10,745,957 | 43,888 | 0.41 | 57,707 | 1.31 | 1 | 1 | 1 |
| 2010 | 10,876,759 | 45,316 | 0.42 | 59,524 | 1.31 | 1 | 1 | 1 |
| 2011 | 11,026,486 | 47,234 | 0.43 | 61,877 | 1.31 | 1 | 1 | 1 |
| 2012 | 11,164,909 | 49,807 | 0.45 | 65,961 | 1.32 | 1 | 1 | 1 |
| 2013 | 11,293,711 | 50,033 | 0.44 | 65,767 | 1.31 | 1 | 1 | 1 |
| 2014 | 11,368,477 | 50,919 | 0.45 | 67,446 | 1.32 | 1 | 1 | 1 |
| Absolute changea | +0.29 | –0.01 | ||||||
| Relative change (δ)b | +6.91% | –0.56% | ||||||
| P trendc | .005 | .48 | ||||||
aAbsolute change = 2006 estimate – 2014 estimate.
bDelta (δ) represents the relative change between the 2006 and 2014 estimate, expressed as a percentage of the 2006 estimate.
c P values for trend were obtained using unadjusted linear regression, with time as the independent variable.
Discussion
Summary of Findings
In this population-based study conducted in a publicly funded health care system, we observed an overall decline over time in outpatient physician visit rates for mental illness and addiction, along with an increased rate of acute care service use. Primary care doctors provided the majority of physician-based outpatient mental health care in Ontario, but the service use trends differed by physician specialty and by patients’ sex. The number of patients seen by primary care providers declined and the number of visits per patient increased over time. Conversely, psychiatrists saw an increased number of patients over time but fewer visits per patient. Most emergency department visits and the greatest increases in rates over time were observed for conditions that could be treated in an ambulatory care setting, including anxiety and addiction.
Interpretation
Previous research in this area, relying predominantly on patient self-report, found an increase in the use of outpatient services, but most studies were conducted in the early 2000s, prior to our study timeframe.12,13 Similar to our findings, however, a study among individuals diagnosed with depression found a decline in the number of psychiatric treatments per patient over time.15 A more recent study also found that self-reported mental health treatment seeking in general has increased between 2002 and 2012.6 However, this study used a composite outcome of any form of treatment, including both inpatient and outpatient settings, which did not allow for a thorough examination of these sectors separately. Consistent with our findings, an increase in acute care service use has been reported in the United States11,16,23 and internationally,17,24 with the acute care burden concentrated among individuals diagnosed with anxiety, mood, and substance-related disorders,11,16,24 suggesting that our findings may be relevant to other jurisdictions outside of Ontario that are seeing similar trends in increasing acute care use.
In light of the dramatic reduction in psychiatric hospital beds per capita in Ontario and in other regions in the world over the past several decades,18,25 the rise in acute care service use amidst declining outpatient visit rates is an important finding. Given previous evidence of stable illness prevalence,3,4 coupled with increasing help seeking,3,5,6 we would expect all aspects of service delivery to increase in order to meet the growing demand. In particular, outpatient physician service utilisation was expected to rise due to increased awareness, reduced stigma, and a public health focus on prevention strategies.7 This has been observed among a population of children and youth in Ontario26 and may reflect government efforts to improve mental health service delivery in this population in the province.27 However, among a population of adults in this study, we observed a decline in the use of outpatient physician services for mental health care, in particular fewer patients being seen by primary care providers over time.
In practice, mental health care is provided along a continuum of inpatient and outpatient services. The latter, which was not fully explored in this study given the lack of available administrative data, includes care provided by social workers, counsellors, psychologists, mental health nurses, community organizations, and nontraditional service providers (e.g., spiritual healers).28 In addition, multidisciplinary teams that include allied health professionals are becoming increasingly popular models of ambulatory care in Ontario.29 Studies from the United States and Canada showed that the proportion of individuals treated by nonphysicians or seeking informal support for mental health–related concerns is relatively small28 but increasing.12,30,31 Another Canadian study found an increase in consultations with social workers, counsellors, or psychotherapists among individuals with major depressive disorder between 2002 and 2012.32 In Ontario specifically, although administrative data on nonphysician mental health care utilization are currently not available, there is evidence that the number of practicing psychologists and social workers has increased throughout the 2000s.33 Nonetheless, the overarching findings of rising acute care service utilization concurrent with a reduction in physician-based outpatient mental health service use suggest that even if ambulatory care seeking has shifted to nonphysician providers, this shift has not been able to keep up with demand observed in the study as rising use of acute care services.
Strengths and Limitations
A major strength of this study was our ability to examine large population-based data over a recent 9-year observation period to monitor mental health service use. This allowed for robust, generalizable estimates that can be used to inform policy. We examined trends across multiple health sectors simultaneously, which is important for both a thorough assessment of the burden of mental illness on the health care system and for allocation of resources and development of targeted interventions. Our analysis of visits, unique individuals, and the number of visits per person further allowed for a more complete picture of health care utilization that informs issues around access and need.
However, some limitations are worth noting. First, this is an ecological study, and the service encounters we identified across multiple sectors were not necessarily made by the same individuals. As such, speculation that individuals avoid care seeking in one setting and turn to another should be taken with caution. Second, the diagnostic codes for outpatient physician billings did not provide a level of granularity that could enable analysis within diagnostic categories, which limited the interpretation for this service sector. Third, we were unable to measure severity or type of treatment at the time of health care visits and were thus unable to infer the appropriateness or quality of each health care encounter. However, our analysis by diagnostic category showed considerable variation in service use in the acute care sector, with care being sought in the emergency department primarily for conditions that can be managed in primary care settings, which suggests potential targets for intervention. Finally, data on community-based mental health services, including services provided by psychologists and social workers that are not covered through Ontario’s universal health care system, were not available in our data. Although literature suggests that the largest proportion of mental health services is carried out by physicians and specialists, rather than by psychotherapists,5,15 future analysis including a broader range of social and mental health services in the community is warranted.
Conclusion
The decreasing use of physician-based outpatient mental health services coupled with the increasing utilization of acute care services that we observed in a publicly funded health care system is an important finding. As most mental illness and addiction is treatable with ambulatory care intervention, attention needs to be paid to issues around access to timely and effective mental health care, as well as the number and type of available resources. Future studies should examine the generalizability of these findings to other health system settings and provide a more in-depth analysis of patients with unmet needs in order that they may be better served.
Acknowledgments
We thank the Ontario Ministry of Health and Long-Term Care (MOHLTC) for their data. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of CIHI.
Footnotes
Author Contributions: MC was the principal investigator and was responsible for the conception of the study. MC and EG were responsible for the design of this study. ZY and PP analyzed the data and all authors interpreted the data (MC, EG, SV, AA, NS, ZY, PP, PK). MC and EG drafted the manuscript, and all authors critically revised it and approved the final manuscript. All authors had full access to the study results and assume full responsibility for the accuracy and completeness of the ideas presented. ZY and PP had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the MOHLTC. It was also supported by the Mental Health and Addictions Scorecard and Evaluation Framework grant from the MOHLTC (04601A14-19). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Dr. Vigod is supported by Women’s College Hospital, the Department of Psychiatry at the University of Toronto, and a New Investigator Award from the Canadian Institutes for Health Research. Dr. Kurdyak received operational grant funding from the MOHLTC Health Services Research Fund Capacity Award and is supported in part by the Medical Psychiatry Alliance, a collaborative health partnership of the University of Toronto, the Centre for Addiction and Mental Health, the Hospital for Sick Children, Trillium Health Partners, the MOHLTC, and an anonymous donor.
Supplemental Material: Supplementary material for this article is available online
References
- 1. Mathers C. The global burden of disease: 2004 update. Geneva (Switzerland): World Health Organization; 2008. [Google Scholar]
- 2. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. [DOI] [PubMed] [Google Scholar]
- 3. Patten SB, Williams JVA, Lavorato DH, et al. Descriptive epidemiology of major depressive disorder in Canada in 2012. Can J Psychiatry. 2015;60(1):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Graaf R, ten Have M, van Gool C, et al. Prevalence of mental disorders and trends from 1996 to 2009: results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–213. [DOI] [PubMed] [Google Scholar]
- 5. Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mojtabai R, Jorm AF. Trends in psychological distress, depressive episodes and mental health treatment-seeking in the United States: 2001-2012. J Affect Disord. 2015;174(Supplement C):556–561. [DOI] [PubMed] [Google Scholar]
- 7. Ontario Ministry of Health and Long-Term Care. Open minds, healthy minds: Ontario’s comprehensive mental health and addictions strategy. Toronto (ON): Ontario Ministry of Health and Long-Term Care; 2011. [Google Scholar]
- 8. Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–2590. [DOI] [PubMed] [Google Scholar]
- 9. Patten SB, Williams JV, Lavorato DH, et al. Major depression in Canada: what has changed over the past 10 years? Can J Psychiatry. 2016;61(2):80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pandya A, Larkin GL, Randles R, et al. Epidemiological trends in psychosis-related emergency department visits in the United States, 1992-2001. Schizophr Res. 2009;110(1-3):28–32. [DOI] [PubMed] [Google Scholar]
- 11. Smith RP, Larkin GL, Southwick SM. Trends in U.S. emergency department visits for anxiety-related mental health conditions, 1992-2001. J Clin Psychiatry. 2008;69(2):286–294. [DOI] [PubMed] [Google Scholar]
- 12. Mojtabai R. Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States: 1997-2002. Am J Public Health. 2005;95(11):2009–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brugha TS, Bebbington PE, Singleton N, et al. Trends in service use and treatment for mental disorders in adults throughout Great Britain. Br J Psychiatry. 2004;185(5):378–384. [DOI] [PubMed] [Google Scholar]
- 14. Olfson M, Blanco C, Wang S, et al. National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry. 2014;71(1):81–90. [DOI] [PubMed] [Google Scholar]
- 15. Olfson M, Marcus SC, Druss B, et al. National trends in the outpatient treatment of depression. JAMA. 2002;287(2):203–209. [DOI] [PubMed] [Google Scholar]
- 16. Larkin GL, Claassen CA, Emond JA, et al. Trends in U.S. emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv. 2005;56(6):671–677. [DOI] [PubMed] [Google Scholar]
- 17. Oldehinkel AJ. Time trends in mental health care utilization in a Dutch area, 1976-1990. Soc Psychiatry Psychiatr Epidemiol. 1998;33(4):181–185. [DOI] [PubMed] [Google Scholar]
- 18. Sogaard HJ, Godt HH, Blinkenberg S. Trends in psychiatric hospitalization and changes in admission patterns in two counties in Denmark from 1977 to 1989. Soc Psychiatry Psychiatr Epidemiol. 1992;27(6):263–269. [DOI] [PubMed] [Google Scholar]
- 19. Drapeau A, Boyer R, Diallo FB. Discrepancies between survey and administrative data on the use of mental health services in the general population: findings from a study conducted in Quebec. BMC Public Health. 2011;11(1):837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Statistics Canada. Canada year book: population and demography (Catalogue No. 11-402-X). 2010. [Cited 2017 July]. Available from: http://www.statcan.gc.ca/pub/11-402-x/2010000/pdf/population-eng.pdf.
- 21. Steele LS, Glazier RH, Lin E, et al. Using administrative data to measure ambulatory mental health service provision in primary care. Med Care. 2004;42(10):960–965. [DOI] [PubMed] [Google Scholar]
- 22. Ahmad OB, Boschi-Pinto C, Lopez AD, et al. Age standardization of rates: a new WHO standard. Geneva (Switzerland): World Health Organization; 2001. [Google Scholar]
- 23. Hazlett SB, McCarthy ML, Londner MS, et al. Epidemiology of adult psychiatric visits to U.S. emergency departments. Acad Emerg Med. 2004;11(2):193–195. [PubMed] [Google Scholar]
- 24. Kosidou K, Magnusson C, Mittendorfer-Rutz E, et al. Recent time trends in levels of self-reported anxiety, mental health service use and suicidal behaviour in Stockholm. Acta Psychiatr Scand. 2010;122(1):47–55. [DOI] [PubMed] [Google Scholar]
- 25. Hartford K, Schrecker T, Wiktorowicz M, et al. Report: four decades of mental health policy in Ontario, Canada. Adm Policy Ment Health. 2003;31(1):65–73. [DOI] [PubMed] [Google Scholar]
- 26. Gandhi S, Chiu M, Lam K, et al. Mental health service use among children and youth in Ontario: population-based trends over time. Can J Psychiatry. 2016;61(2):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ontario Ministry of Children and Youth Services. Moving On Mental Health: A system that makes sense for children and youth 2012. [Cited 2017 July]. Available from: http://www.children.gov.on.ca/htdocs/English/professionals/specialneeds/momh/momh.aspx.
- 28. Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the united states: results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):629–640. [DOI] [PubMed] [Google Scholar]
- 29. Rosser WW, Colwill JM, Kasperski J, et al. Progress of Ontario’s family health team model: a patient-centered medical home. Ann Fam Med. 2011;9(2):165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Urbanoski K, Inglis D, Veldhuizen S. Service use and unmet needs for substance use and mental disorders in Canada. Can J Psychiatry. 2017;62(8):551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Urbanoski KA, Rush BR, Wild TC, et al. Use of mental health care services by Canadians with co-occurring substance dependence and mental disorders. Psychiatr Serv. 2007;58(7):962–969. [DOI] [PubMed] [Google Scholar]
- 32. Patten SB, Williams JV, Lavorato DH, et al. The prevalence of major depression is not changing. Can J Psychiatry. 2015;60(1):31–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Canadian Institute for Health Information. Canada’s health care providers, 2000 to 2009: a reference guide. Ottawa (ON): CHI; 2011. [Google Scholar]