Abstract
Background: Hand spasticity after a stroke greatly increases the difficulties of the daily living activities and limits the effectiveness of rehabilitation. Radial extracorporeal shock wave therapy (RESWT) has been suggested as an alternative treatment for spasticity reduction. We demonstrate the effectiveness of RESWT regarding hand spasticity in a stroke patient.
Case description: We describe the case of a 42-year-old woman with right hemiparesis after ischaemic stroke. Her right arm was plegic with increased spasticity. The patient received a total of six RESWT treatments. Clinical evaluation was performed using the Modified Ashworth Scale, passive dorsal flexion of the wrist and the Disability Assessment Scale (DAS). The measurements were made before initiation, immediately after the sixth treatment, one and three months after the RESWT. Immediately after the RESWT there was a reduction of the spasticity of the hand and fingers and increased passive range of motion of the affected wrist, as well as decreased DAS score. These effects lasted for four weeks. With time, the therapeutic effect regarding spasticity decreased, but three months following termination of treatment there was a better clinical result than before initiation of treatment.
Conclusion: RESWT is a safe alternative treatment for hand and fingers spasticity reduction after stroke. Hippokratia 2016, 20(4): 309-312
Keywords: Stroke, spasticity, radial extracorporeal shock wave therapy, rehabilitation
Introduction
According to the most quoted definition by Lance dated in 1980, spasticity is “a motor disorder characterized by the velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, which results from hyperexcitability of the stretch reflex, as one component of the upper motoneuron syndrome disorder”1.
Watkins et al reported the incidence of spasticity at 39 % in the first year after a stroke2. Spasticity of the upper extremity was observed in 43 % of patients as a consequence of ischemic stroke. Fifteen percent of the patients with ischemic stroke have at least one joint affected with a Modified Ashworth scale (MAS) score of three. The upper extremity is more often affected (19 %) by a more severe degree of spasticity than the lower extremity (5-6 %)3.
The pathophysiology of spasticity is very complex and still not completely understood. The changes in the muscle tone result from the alterations in the balance of the incoming impulses from the reticulospinal and the other descending pathways of the motor and interneuron circuits in the spinal cord, and the absence of an intact corticospinal system4,5. The pathophysiological mechanisms of spasticity resulting from an abnormal descending control that can be detected at the spinal level are: alpha motoneuron hyperexcitability, increased polysynaptic Ia excitation, reduced presynaptic inhibition, reduced reciprocal inhibition, reduced autogenic Ib inhibition, and increased sensitivity of the muscle spindles due to gamma hyperactivity1,4.
The resistance to passive stretching of the muscle is not always accompanied by an increased stretching reflex, but it is also due to changes in the biomechanical properties of the muscle. There are changes of degenerative nature (atrophy, fibrosis), as well as changes in its contractile properties. The underlying reasons for the increased stiffness of the muscles are the persisting links between the myofilaments and the reduction of the active motor units in the affected muscles6.
Radial extracorporeal shock wave therapy (RESWT) involves an application of high-intensity acoustic radiation (high-energy acoustic waves-shock waves). Shock waves are defined as the sequence of single sound pulses which are characterized by high point of pressure that can reach up to 100 MPa (most often 50-80 MPa), fast reach of this pressure in a short period (less than 10 ns), short duration (10 μs), followed by a variable negative pressure that can affect cavitation and a frequency of 16-20 Hz7,8.
Over time, it was proved that RESWT is an efficient and non-invasive method for the treatment of localized musculoskeletal pathology including epicondylitis, calcar calcanei, plantar fasciitis, disorders of the rotator cuff, treatment of trigger points, chronic tendinopathy, pseudoarthrosis, and others7-10.
Recently, attempts have been made to extend the therapeutic range of RESWT, thus proving its effectiveness in reducing spasticity11-16.
The purpose of this report is to demonstrate the effectiveness of RESWT regarding hand spasticity in a stroke patient.
Case report
A 42-year-old housewife woman with no previous medical history presented two years after an ischemic stroke in the area of the left middle cerebral artery which resulted in right hemiplegia and dysarthria. During the acute phase, she was hospitalized and treated in a clinical setting under the supervision of a neurologist. Two months after the stroke, she was hospitalized and rehabilitated in a clinical setting in a specialized institution for physical medicine and rehabilitation. She was rehabilitated on two occasions, with an interruption of five weeks. The rehabilitation program included manual massage, occupational therapy, and kinesitherapy. Due to severe pain in her right shoulder, the patient also received sonotherapy and transcutaneous electrical nerve stimulation on the affected shoulder. After her second hospital admission, the patient was able to walk independently with an ankle-foot orthosis for the right leg and a forearm crutch. The right arm remained plegic, dysfunctional, and with increased spasticity.
Two years after the stroke, she came to our Institute for Physical Medicine and Rehabilitation due to pain involving her right hand and fingers. As a result of the increased spasticity, the pain was particularly pronounced during passive movements of the wrist and fingers. The patient did not take any antispastic drug therapy neither used a passive forearm orthosis for the right hand.
During the physical examination, it was observed that the right arm had an adducted shoulder, semiflexed elbow, semipronated forearm, hand and fingers in volar flexion with the thumb closed into a fist. The musculature was slightly hypotrophic with an increased tone, and the tendon reflexes were also increased. Active movements in the shoulder were limited under a horizontal line, but there were no active movements in the other joints. Passive movements were possible in all joints: in the shoulder and elbow they were possible up to the normal range and in the wrist and fingers they were limited and accompanied by severe pain. The superficial and deep sensibility were normal. She did not use her right hand in the activities of daily living.
The MAS was used to evaluate the wrist and fingers spasticity. This is a scale that measures the degree of spasticity from 0 to 41,5. A manual goniometer was utilized to measure the passive range of motion in the wrist. The Disability Assessment Scale (DAS) was used to evaluate the functional disability of the upper extremity. This scale assesses the upper extremity functional disability in patients with spasticity following a stroke. The patient is interviewed to determine the extent of the functional impairment for the following four areas: hygiene, dressing, limb position, and pain. Each item is evaluated on a scale from 0-3, where: 0: no disability, 1: mild disability (noticeable but does not interfere significantly with the normal activities), 2: moderate disability (normal activities require increased effort and/or assistance), 3: severe disability (normal activities are limited)17.
The measurements were made before initiation of treatment, immediately after the sixth application of RESWT, and one and three months after the treatment. Having met the basic criteria for RESWT application (no anticoagulant therapy, no infection or inflammation at the site of application, no contracture of the wrist and fingers) she was offered this therapy. BTL-5000 SWT Power device (BTL Industries Ltd., UK) with 15 mm radial probe was used for the application of RESWT.
Therapy was applied per the recommendations of the manufacturer: 1,500 shocks on the ulnar side of the forearm with a “painting” technique over the muscles flexor carpi ulnaris and flexor carpi radialis and 3,500 shocks over the interosseous muscles on the volar side of the hand. The shocks were applied with a pressure of two Bar and a frequency of 10 Hz. A low energy was used; thus the application was painless and required no anesthesia or analgesics. As per manufacturer’s recommendation a total of six sessions were applied at a time distance of two-three days. During the same period when the patient was treated with RESWT, a rehabilitation program was implemented which included passive exercises on the right hand, occupational therapy, and manual massage.
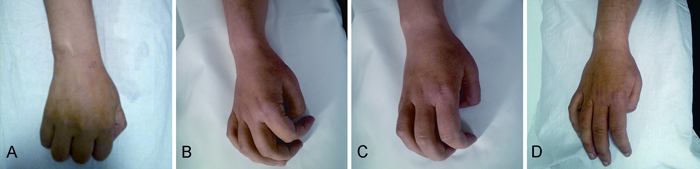
According to the MAS score, a significant reduction of spasticity of the hand and fingers was achieved immediately after the application. From a score of three before the beginning of the treatment, the spasticity was reduced to a score of one immediately after the treatment. The reduction of spasticity remained for one month after the treatment. Over time, the therapeutic effect decreased and after three months the MAS score of the hand and fingers was 1+.
The passive dorsal flexion of the wrist before treatment was 50º, and immediately after treatment was 65º. This result was maintained one and three months after the treatment.
The total score of the DAS before the initiation of RESWT was 7 (moderate disability), and immediately after treatment was reduced to 4 (mild disability). This score was maintained one and three months after the treatment (Figure 1). After completion of treatment, the patient did not complain of pain while making passive movements in the wrist and fingers.
Figure 1. Images showing the results of the radial extracorporeal shock wave therapy (RESWT) in the passive dorsal flexion of the affected wrist of a 42-year-old with hand spasticity two years after a stroke. A) spastic hand at baseline (before treatment initiation), B) immediately after the sixth RESWT session, C) and D) one and three months (respectively) after completion of RESWT treatment.
Discussion
Spasticity of the upper extremity leads to reduced quality of life. It is one of the most significant obstacles we confront in the rehabilitation of patients with stroke consequences. It is usually accompanied by muscle weakness, decreased range of motion often with painful spasms and contractures. Hand spasticity after stroke significantly increases the difficulties of daily living activities and limits the effectiveness of rehabilitation. Hence is reasonable assumption that the reduction of spasticity will in many cases contribute to improvement of the residual extremity function.
Today, there are numerous possibilities for spasticity treatment including physical therapy and rehabilitation, drug treatment, intrathecal baclofen, phenol, and ethanol injections, administration of botulinum toxin and surgery. However, sometimes, even when one utilizes combinations of the above methods, regardless their possible side effects, spasticity reduction cannot be achieved1,4,5. Therefore, it is necessary to consider developing a new non-invasive treatment for dealing with this condition.
The results of this case report confirm the benefits of RESWT in the treatment of spasticity after a stroke. Immediately after the treatment, there was a reduction in the spasticity of the hand and fingers and increased passive dorsal flexion of the affected wrist, as well as decreased DAS score. Except for the spasticity score, other results lasted for three months after the therapy. With time, the therapeutic effect regarding spasticity decreased, but even three months following termination of treatment there was a better clinical result than before initiation of treatment. During and after completion of treatment, there were no observed adverse effects.
The results of this clinical assessment support the effectiveness of RESWT therapy in reducing spasticity. They are consistent with previous studies dealing with this issue even though each study followed a different protocol for application of the treatment11-16. There is still no unified protocol for RESWT application in the treatment of spasticity after a stroke.
The mechanism of action of RESWT on the spastic muscles is not yet sufficiently known. Various mechanisms of action were proposed such as synthesis of nitrogen monoxide, reduction of spinal excitability, and induction of mechanical vibrations. However, the effect of RESWT on the spinal excitability can be excluded as there are no significant changes in the minimum latency of the F wave, in the latency of the H reflex or the H-M ratio11-16. Furthermore, it is assumed that the reduction of the spasticity is due to its direct effect on the connective tissue fibrosis in chronic spastic muscles, as no change in the amplitude of the F wave has been detected11-16.
Conclusion
The RESWT reduced the spasticity of the wrist and fingers flexors after stroke for a sufficient period of time. No side effects of its application were noted. RESWT is a safe alternative, non-invasive treatment in reducing spasticity after a stroke. This therapy opens a new field of research in the non-invasive treatment of spasticity. Further future studies are needed with large cohort of patients.
Conflict of interest
Authors have no potential conflicts of interest to disclose.
References
- 1.Thibaut A, Chatelle C, Ziegler E, Bruno MA, Laureys S, Gosseries O. Spasticity after stroke: physiology, assessment and treatment. Brain Inj. 2013;27:1093–1105. doi: 10.3109/02699052.2013.804202. [DOI] [PubMed] [Google Scholar]
- 2.Wissel J, Schelosky LD, Scott J, Christe W, Faiss JH, Mueller J. Early development of spasticity following stroke: a prospective, observational trial. J Neurol. 2010;257:1067–1072. doi: 10.1007/s00415-010-5463-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Urban PP, Wolf T, Uebele M, Marx JJ, Vogt T, Stoeter P, et al. Occurrence and clinical predictors of spasticity after ischemic stroke. Stroke. 2010;41:2016–2020. doi: 10.1161/STROKEAHA.110.581991. [DOI] [PubMed] [Google Scholar]
- 4.Brown P. Pathophysiology of spasticity. J Neurol Neurosurg Psychiatry. 1994;57:773–777. doi: 10.1136/jnnp.57.7.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marciniak C. Poststroke hypertonicity: upper limb assessment and treatment. Top Stroke Rehabil. 2011;18:179–194. doi: 10.1310/tsr1803-179. [DOI] [PubMed] [Google Scholar]
- 6.Carey JR, Burghardt TP. Movement dysfunction following central nervous system lesions: a problem of neurologic or muscular impairment? . Phys Ther. 1993;73:538–547. doi: 10.1093/ptj/73.8.538. [DOI] [PubMed] [Google Scholar]
- 7.Schmitz C, Császár BM N, Rompe JD, Chaves H, Furia JP. Treatment of chronic plantar fasciopathy with extracorporeal shock waves (review) J Orthop Surg Res. 2013;8:31. doi: 10.1186/1749-799X-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Notarnicola A, Moretti B. The biological effects of extracorporeal shock wave therapy (eswt) on tendon tissue. Muscles Ligaments Tendons J. 2012;2:33–37. [PMC free article] [PubMed] [Google Scholar]
- 9.Engebretsen K, Grotle M, Bautz-Holter E, Sandvik L, Juel NG, Ekeberg OM, et al. Radial extracorporeal shockwave treatment compared with supervised exercises in patients with subacromial pain syndrome: single blind randomised study. BMJ. 2009;339:b3360. doi: 10.1136/bmj.b3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vahdatpour B, Taheri P, Zade ZA, Moradian S. Efficacy of extracorporeal shockwave therapy in frozen shoulder. Int J Prev Med. 2014;5:875–881. [PMC free article] [PubMed] [Google Scholar]
- 11.Manganotti P, Amelio E. Long-term effect of shock wave therapy on upper limb hypertonia in patients affected by stroke. Stroke. 2005;36:1967–1971. doi: 10.1161/01.STR.0000177880.06663.5c. [DOI] [PubMed] [Google Scholar]
- 12.Amelio E, Manganotti P. Effect of shock wave stimulation on hypertonic plantar flexor muscles in patients with cerebral palsy: a placebo-controlled study. J Rehabil Med. 2010;42:339–343. doi: 10.2340/16501977-0522. [DOI] [PubMed] [Google Scholar]
- 13.Lee JY, Kim SN, Lee IS, Jung H, Lee KS, Koh SE. Effects of Extracorporeal Shock Wave Therapy on Spasticity in Patients after Brain Injury: A Meta-analysis. J Phys Ther Sci. 2014;26:1641–1647. doi: 10.1589/jpts.26.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li TY, Chang CY, Chou YC, Chen LC, Chu HY, Chiang SL, et al. Effect of Radial Shock Wave Therapy onSpasticityof the Upper Limb in Patients With Chronic Stroke: A Prospective, Randomized, Single Blind, Controlled Trial. Medicine (Baltimore) 2016;95:e3544. doi: 10.1097/MD.0000000000003544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim YW, Shin JC, Yoon JG, Kim YK, Lee SC. Usefulness of radial extracorporeal shock wave therapy for thespasticityof the subscapularis in patients with stroke: a pilot study. Chin Med J (Engl) 2013;126:4638–4643. [PubMed] [Google Scholar]
- 16.Sohn MK, Cho KH, Kim YJ, Hwang SL. Spasticity and electrophysiologic changes after extracorporeal shock wave therapy on gastrocnemius. Ann Rehabil Med. 2011;35:599–604. doi: 10.5535/arm.2011.35.5.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brashear A, Zafonte R, Corcoran M, Galvez-Jimenez N, Gracies JM, Gordon MF, et al. Inter- and intrarater reliability of the Ashworth Scale and the Disability Assessment Scale in patients with upper-limb poststroke spasticity. Arch Phys Med Rehabil. 2002;83:1349–1354. doi: 10.1053/apmr.2002.35474. [DOI] [PubMed] [Google Scholar]


