Abstract
Objective
This study examined the independent and interactive effects of acculturation and social activity on depressive symptoms.
Method
Using a sample of community-dwelling Korean American older adults (N = 675), hierarchical regression models of depressive symptoms were estimated with an array of predictors: (a) demographic variables, (b) health-related variables, (c) acculturation, (d) social activity, and (e) an interaction between acculturation and social activity.
Results
After controlling for the effects of demographic and health-related variables, both acculturation and social activity were identified as significant predictors. Moreover, their interaction was significant (β = .09, p < .05). Further analysis showed that the beneficial effect of social activity on mental health was particularly strong among those with lower levels of acculturation.
Discussion
Our findings suggest that enhancing opportunities for social engagement may serve to protect and promote the mental health of vulnerable older immigrants, particularly those who are less acculturated.
Keywords: acculturation, social activity, depressive symptoms, Korean American elders
One of the core themes of activity theory (Havighurst, 1956; Lemon, Bengtson, & Peterson, 1972) and successful aging (Rowe & Kahn, 1998) is that active engagement is an integral part of life in later years. Participation in social activities provides social contacts and interactions with others, fulfilling a basic human need for affiliation and building a sense of community (Maier & Klumb, 2005). The reported consequences of participation in social activities include physiologic benefits (e.g., immune function, cardiovascular reactivity, cardiopulmonary fitness), delayed rate of physical health decline, increased self-efficacy, sense of belonging, purpose of life and life satisfaction, reduced depressive symptoms, and even lowered mortality (e.g., Berkman, Glass, Brissette, & Seeman, 2000; Buchman et al., 2009; Glass, Mendes de Leon, Bassuk, & Berkman, 2006; Hong, Hasche, & Bowland, 2009; Isaac, Stewart, Artero, Ancelin, & Ritchie, 2009; Maier & Klumb, 2005; Morrow-Howell, Hinterlong, Rozario, & Tang, 2003; Perkins, Multhaup, Perkins, & Barton, 2008).
Although the benefits of active engagement with life would seem universal (Su & Ferraro, 1997), the value that each individual places in social activities may vary. Depending on personal situations and social contexts, people may assign different values to social activities. In the present study, the focus was on the importance of social activities for older immigrants, conceptualizing acculturation as a conditioning variable. Acculturation, the extent to which those from another culture have learned the language and behaviors expected in the host culture (e.g., Myers & Rodriguez, 2002; Phinney & Flores, 2002; Rogler, Cortes, & Malgady, 1991; Sam & Berry, 2006), has received considerable attention as a means of understanding the varied experiences of immigrants. Research has generally shown that a higher level of acculturation is linked to lowered depressive symptoms (e.g., Chiriboga, Black, Aranda, & Markides, 2002; Myers & Rodriguez, 2002; Sam & Berry, 2006). Moving beyond its direct benefits on mental health, the present study hypothesized that acculturation might determine the magnitudes of benefits from social activities. Elderly immigrant with low acculturation may experience reduced social boundary and opportunity for social engagement. In such circumstances, their circumscribed but active social activity participation may bring greater psychological benefits than would be the case for those who are more acculturated. The combined effect of acculturation and social activity in older immigrant populations has been rarely discussed in the literature and is of interest to the present study.
For a research population, we selected Korean American older adults. Currently ranked as the fourth largest Asian American subgroup, Korean Americans are one of the fastest growing segments of immigrants living in the United States (U.S. Census Bureau, 2009). The majority of Korean Americans immigrated to the United States after the Immigration Reform Act of 1965 (Hurh, 1998). Due to this recent history of immigration, only 7.6% of Korean Americans are aged 65 or older (the corresponding figure for non-Hispanic Whites is 14.5%), but an exponential increase in the Korean American elderly population is projected (U.S. Census Bureau, 2009). In the extant mental health literature, Korean American elders are often profiled as a high-risk group because their rates of probable depression as indexed by standardized depression screening tools are up to four times greater than those of Whites or African Americans (Jang & Chiriboga, 2010; Min, Moon, & Lubben, 2005). Indeed, Korean American elders are reported to have the highest depressive affect scores among five ethnic groups of Asian Americans in the 2007 California Health Interview Survey (Kim et al., 2010). The direct association of depressive symptoms with low levels of acculturation (e.g., Jang & Chiriboga, 2010; Oh, Koeske, & Sales, 2002) or limited social activities (e.g., Choi, Wilbur, Miller, Szalacha, & McAuley, 2008; Yang et al., 2007) has been reported in previous studies with Korean American elders. However, little attention has been paid to the conditioning role of acculturation in determining the impact of social activities on depressive symptoms.
Based on the issues raised in the above review, the present study was designed to explore the independent and interactive effects of acculturation and social activity on depressive symptoms using a sample of community-dwelling Korean American older adults. Along with basic demographic information, chronic conditions and functional disability were controlled for the analyses because physical health status is closely linked to both the levels of social activities and depressive symptoms. We hypothesized that those with lower levels of acculturation would gain more benefits from social activities compared with their counterparts.
Method
Participants
With approval from the institutional review board at the University of South Florida, we conducted a survey of older Korean Americans (≥ 60) from March to August 2008 in Tampa and Orlando, Florida. As immigrant populations are often hard to identify by any single approach, and also because a single-source sampling frame may lead to bias when dealing with such populations, we combined several sampling methods in our recruitment efforts. These methods included contacting local Korean churches, other religious groups, senior centers, senior housing, and elder associations. To recruit individuals who were not affiliated with those groups or organizations, we made requests for referrals from respondents as well as other individuals associated with our primary data collection sites. A copy of the questionnaire and a self-addressed, stamped return envelope were mailed to all individuals with whom onsite contacts were not possible.
We supplemented this convenience sampling procedure with a systematic approach using a telephone directory of Korean residents provided by the Florida Korean American Association. A total of 2,000 Korean residents in Tampa and Orlando were listed in the directory. After excluding those who had already been recruited through our convenience sampling efforts, we called all remaining individuals to ask whether there were age-eligible members in their household. Up to five phone calls were made until the individual was considered unreachable. If there was an eligible person in the household, a mail survey packet was sent. This step was designed to improve comprehensiveness of the sample by including individuals who were not recruited by the convenience sampling efforts and to offset limitations associated with non-representativeness of convenience sampling.
A total of 675 participants were included in our final sample. Of the sample, 73% was recruited through visits and about 27% through mail surveys. We conducted a series of comparative analyses to check whether there was any difference in sample characteristics by recruitment method. No significant difference was found for major demographic characteristics; however, compared with the individuals whose data were collected through mail surveys, participants recruited through visits were less educated (χ2 = 10.3, p < .01). This finding suggests that a sole reliance on mail surveys might have excluded individuals with low levels of education. All respondents were paid US$20 for their participation.
Measures
The survey instrument was a standardized questionnaire designed to be self-administered; however, trained interviewers were available for assistance. A Korean-language questionnaire was developed specifically for this project. Several of the measures had been translated into Korean and evaluated for psychometric qualities in our previous work (e.g., Jang & Chiriboga, 2010; Jang, Kim, Chiriboga, & King-Kallimanis, 2007). For additional scales, back-translation was used to confirm the appropriateness of initial translations into Korean. The final product was reviewed and reconciled by bilingual individuals who did not participate in the initial translation process. The structured questionnaire was pilot tested with 20 Korean American older adults who were representative of the anticipated sample. As no specific difficulties or problems were reported in the pilot testing, no modification was made. For the convenience of the participants, survey questionnaires were printed using a large font. Measures for the present analyses included the following:
Chronic conditions
Individuals were asked to report existing medical conditions using a list of chronic diseases and conditions commonly found among older populations. The list included arthritis, stroke, heart problems, liver problems, problems with digestive systems, kidney problems, hypertension, diabetes, and cancer. Response was coded using a yes/no format. A summated score was used for the analysis.
Functional disability
Functional status was assessed with a composite measure of the physical activities of daily living (PADL; Fillenbaum, 1988), instrumental activities of daily living (IADL; Fillenbaum, 1988), Physical Performance Scale (Nagi, 1976), and Functional Health Scale (Rosow & Breslau, 1966). The 20 items covered a wide range of activities including eating, dressing, traveling, managing money, carrying a bag of groceries, and ability to reach above the head with one’s arms. Participants were asked whether they could perform each activity, and response was coded as 0 = without help, 1 = with some help, or 2 = unable to do. Total scores could range from 0 = no disability to 40 = severe disability. Internal consistency for the measure was high in the present sample (α = .93).
Acculturation
The level of acculturation was assessed with a 12-item inventory adapted from several studies on acculturation (e.g., Hazuda, Stern, & Haffner, 1988; Suinn, Ahuna, & Khoo, 1992; Ying, 1995). The scale contains 12 items on language proficiency, frequency of language use, audiovisual media consumption (e.g., TV, video), printed media consumption (e.g., newspaper, magazine), food consumption at home, food consumption outside the home, ethnicity of friends, social gathering, sense of belonging, getting along, familiarity to culture and custom, and celebration of holidays. Each response was coded from 0 to 3. Total scores could range from 0 to 36, with a higher score indicating a greater level of acculturation to mainstream American culture. Validation of the instrument has been conducted in previous studies with Korean American elders (e.g., Jang et al., 2007). Internal consistency for the scale in the present sample was high (α = .92). In an exploratory factor analysis, the 12 items yielded a single-factor solution that accounts for 53.1% of the variance. Although the two items on language showed the highest loadings, all items fell under one dominant factor.
Social activity
Individuals were asked how often they participated in the following six activities: religious meetings, social gatherings (e.g., elder association, alumni association), senior centers, leisure or sporting activities, volunteer activities, and education/learning activities. Each activity was rated on a 4-point scale, with 0 = never and 3 = everyday or almost everyday. Internal consistency of the scale was low (α = .62), but it was expected because the list represented various activities. Responses on each item were combined to yield a composite score.
Depressive symptoms
A 10-item short form of the Center for Epidemiologic Studies-Depression Scale (CES-D; Andresen, Malmgren, Carter, & Patrick, 1994; see also Radloff, 1977) was employed to assess depressive symptoms. The scale assessed the frequency of depressive symptoms during the past week on a 4-point scale, namely, rarely or none of the time, some of the time, much of the time, and most or all of the time. The scale includes two positively worded items (“I felt hopeful” and “I was happy”) and eight negatively worded items (e.g., “I felt depressed” and “I felt lonely”). The positive items were reverse-coded, and all items were summed into total scores that span from 0 = no depressive symptoms to 30 = severe depressive symptoms. The CES-D has been translated into the Korean language, and its psychometric properties have been validated in previous studies (e.g., Cho, Nam, & Suh, 1998; Noh, Avison, & Kaspar, 1992). Internal consistency in the present sample was good (α = .77).
Other variables
Demographic information included age (in years), gender (0 = male, 1 = female), marital status (0 = married, 1 = not married), and educational attainment (0 = <high school, 1 = ≥high school).
Analytic Strategy
Prior to the main analyses, intercorrelations among study variables were assessed to check for the presence of collinearity. Depressive symptoms served as the outcome criterion, and its predictive model was estimated by entering blocks of variables in the following order: (a) demographic variables (age, gender, marital status, and education), (b) physical health status (chronic conditions and functional disability), (c) acculturation, (d) social activity, and (e) an interaction between acculturation and social activity. In computing the interaction term, centered scores were used to minimize problems associated with collinearity between the main effect and interaction term (Aiken & West, 1991). Analyses were performed using SPSS, version 18 (SPSS Inc., Chicago, IL).
Results
Descriptive Information of the Sample and Study Variables
Table 1 summarizes descriptive information of the sample. The sample consisted of 675 Korean American older adults. The mean age was 70.2 (SD = 6.87), with a range from 60 to 96. More than half (58.8%) of the participants were female, and about 23% of the sample was presently unmarried. Seventy percent of the sample had received a high school education or more. These demographic characteristics were similar to previously reported profiles of Korean American elders in Florida and in other states (e.g., Jang & Chiriboga, 2010; Min et al., 2005).
Table 1.
Descriptive Information of the Sample and Study Variables (N = 675)
| Variable | Value |
|---|---|
| Age, M ± SD (range 60–96) | 70.2 ± 6.87 |
| Female (%) | 58.8 |
| Not married (%) | 23.4 |
| ≥High school (%) | 70.5 |
| Chronic conditions, M ± SD (range 0–9) | 1.35 ± 1.24 |
| Functional disability, M ± SD (range 0–40) | 1.81 ± 4.46 |
| Acculturation, M ± SD (range 0–35) | 15.8 ± 7.56 |
| Social activity, M ± SD (range 0–17) | 4.66 ± 2.74 |
| Depressive symptoms, M ± SD (range 0–27) | 7.24 ± 4.63 |
Participants had an average of 1.35 (SD = 1.24) chronic conditions and their functional status averaged 1.81 (SD = 4.46). The mean scores for acculturation and social activities were 15.8 (SD = 7.56) and 4.66 (SD = 2.74) respectively. The mean CES-D score was 7.24 (SD = 4.63) out of a possible maximum of 30. When the suggested cutoff score (≥ 10) was applied (Andresen et al., 1994), 30.8% of the sample fell within the category of probable depression.
Bivariate Correlations
To check collinearity among study variables, bivariate correlation coefficients were examined, and the absence of collinearity was confirmed (i.e., all rs < .39). As shown in Table 2, individuals who had more depressive symptoms were more likely to be unmarried and to have more numbers of chronic conditions and greater levels of functional disability. As anticipated, those with low levels of acculturation and social activity had higher levels of depressive symptoms. Higher levels of social activities were observed among males, those who were married and more educated, and those who had better physical health status (lower levels of chronic conditions and functional disability) and greater levels of acculturation.
Table 2.
Correlations Among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | — | ||||||||
| 2. Female | −.14*** | — | |||||||
| 3. Not married | .19*** | .33*** | — | ||||||
| 4. ≥High school | −.22*** | −.27*** | −.30*** | — | |||||
| 5. Chronic conditions | .14*** | .08* | .12** | −.10** | — | ||||
| 6. Functional disability | .36*** | .10** | .18*** | −.21*** | .32*** | — | |||
| 7. Acculturation | −.20*** | −.09* | −.12** | .38*** | −.11** | −.28*** | — | ||
| 8. Social activity | −.04 | −.09* | −.09* | .18*** | −.12** | −.17*** | .29*** | — | |
| 9. Depressive symptoms | −.02 | .05 | .16*** | −.07 | .24*** | .27*** | −.25*** | −.20*** | — |
p < .05.
p < .01.
p < .001.
Multivariate Models of Depressive Symptoms
Results from hierarchical regression analyses are summarized in Table 3. In the initial model, the demographic variables explained 3% of the total variance of depressive symptoms. Marital status was the only significant contributor: individuals who were not married were likely to have greater levels of depressive symptoms. In the next model, the addition of variables representing physical health status led to an 11% increase in accounted variance. Those who had more chronic conditions and greater levels of functional disability were more likely to report depressive symptoms. The subsequent model with acculturation accounted for an additional 3% of variance, and lower levels of acculturation was a significant predictor of depressive symptoms. The addition of social activity accrued an additional 1% of the explained variance, and a lower level of participation was shown to predict depressive symptoms. In the final step, the interaction term between acculturation and social activity was found to be significant, adding 1% to the explained variance. The contribution of the interaction term to the overall model was found to be significant (ΔF = 6.27, p < .05). The total variance explained by the estimated model was 19%.
Table 3.
Hierarchical Regression Models of Depressive Symptoms
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| Predictor | β | t | β | t | β | t | β | t | β | t |
| Age | −.06 | −1.58 | −.17 | −4.19*** | −.18 | −4.60*** | −.18 | −4.47*** | −.19 | −4.68*** |
| Female | −.02 | −0.53 | −.06 | −1.58 | −.06 | −1.62 | −.06 | −1.70 | −.06 | −1.67 |
| Not married | .17 | 3.89*** | .14 | 3.45** | .14 | 3.62*** | .14 | 3.29 | .14 | 3.72*** |
| ≥High school | −.05 | −1.10 | −.02 | −0.49 | .05 | 1.26 | .06 | 1.41 | .05 | 1.43 |
| Chronic conditions | .17 | 4.29*** | .16 | 4.23*** | .15 | 4.07*** | .15 | 4.06*** | ||
| Functional disability | .26 | 6.27*** | .22 | 5.38*** | .21 | 5.18*** | .20 | 4.89*** | ||
| Acculturation | −.21 | −5.36*** | −.19 | −4.61*** | −.20 | −4.87*** | ||||
| Social activity | −.10 | −2.61** | −.10 | −2.72** | ||||||
| Acculturation × Social activity | .09 | 2.50* | ||||||||
| R2 | .03 | .14 | .17 | .18 | .19 | |||||
| F | 5.13*** | 16.9*** | 19.3*** | 17.9*** | 16.7*** | |||||
p < .05.
p < .01.
p < .001.
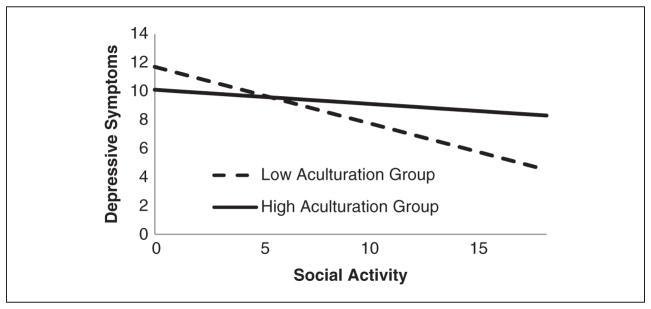
As it is difficult to obtain statistical significance of an interaction (McClelland & Judd, 1993), the observed finding deserves attention. As hypothesized, the interaction suggests that the impact of social activity on depressive symptoms may be conditioned by the level of acculturation. To further examine the interaction effect, we divided the sample into a low-acculturation group (n = 333) and a high-acculturation group (n = 340) based on median split and compared the correlations between social activity and depressive symptoms between the groups. In the high-acculturation group, the inverse association between social activity and depressive symptoms was low and not significant (r = −.06, p > .05). However, the association was significant in the low-acculturation group (r = −.24, p < .001). The group difference in bivariate coefficients was statistically significant (t = 2.39, p < .05).
Figure 1 displays regression lines for low and high acculturation groups where median acculturation score for each group was used. The low acculturation group showed a steeper slope than the high acculturation group, indicating greater benefits of social activity on mental well-being.
Figure 1.
Graph of interaction effect of acculturation and social activity on depressive symptoms
Discussion
Although there seems to be no doubt about the benefits of active engagement with life in the later years, individual variations in the magnitude of such benefits are evident (e.g., Harlow & Cantor, 1996; Jang, Mortimer, Haley, & Borenstein-Graves, 2004). Given the dislocation of social networks and restricted social boundaries that often follow immigration, especially for immigrant elders whose racial/ethnic group is not well represented in the communities in which they settle, the present study assessed how contextual factors affect the role of social activities. We conceptualized that acculturation may serve as a conditioning factor that determines the effect of social activity on depressive symptoms in immigrant older adults and found supportive evidence for the proposed hypothesis.
As observed in numerous studies with immigrant populations (e.g., Chiriboga et al., 2002; Myers & Rodriguez, 2002; Sam & Berry, 2006), a low level of acculturation was found to be a significant contributor to depressive symptoms. Its significance remained after controlling for major demographic and health risks. The benefits of acculturation may be explained in part by the facts that acculturation suggests a greater capacity to engage in activities of the host culture and, not coincidently, is also associated with higher socioeconomic status (Jang & Chiriboga, 2010; Myers & Rodriguez, 2002). With respect to social activity, results were similar to previous studies with Korean Americans (e.g., Choi et al., 2008; Yang et al., 2007) and with other racial/ethnic groups (e.g., Berkman et al., 2000; Glass et al., 2006; Hong et al., 2009; Morrow-Howell et al., 2003; Su & Ferraro, 1997) in that social activity was found to have direct benefits for mental health. Although the present study used a composite score of social activities, a separate analysis, not included in the tables, showed that of all the items, religious activity had the greatest levels of participation and its impact on depressive symptom level was the highest.
The unique feature of the present investigation was its focus on the combined effects of acculturation and social activity. At the bivariate level, the results indicated that greater acculturation was linked to greater engagement in social activities. This association was of particular interest as the social activity measure used in the present study covered a broad range of activities that were not specific to either mainstream or ethnic-oriented cultures. In a supplementary analysis not included in the tables, the group with higher acculturation was found to score significantly higher (p < .05) in four out the six activities assessed by the instrument, including social gatherings (e.g., elder association, alumni association), leisure or sporting activities, volunteer activities, and education/learning activities. Their higher scores in these activities may result from their greater ability to engage in the host culture. However, no group difference was observed in activities related to religious meetings and senior centers, both of which represented engagement with the culture of origin.
It is interesting to note that in predicting depressive symptomatology, acculturation and social activity participation, while both individually linked to fewer symptoms of depression, interacted in a way that accents the importance of social activities for those low in acculturation. In other words, despite their generally low levels of activity participation, the positive impact of social activity on mental health was stronger among those with lower levels of acculturation. This finding is in accordance with findings of the previous studies that older individuals whose social life participation was challenged either by retirement or functional disability—similar to the challenges faced by immigration—were likely to enjoy relatively high psychological benefits from those social activities in which they were able to participate (e.g., Harlow & Cantor, 1996; Jang et al., 2004).
Some limitations to the present study should be noted. Foremost important concern is the use of a sample of convenience. The present sample was not recruited through random sampling procedures and may be somewhat biased toward advantaged individuals. Given the nature of the sample, the findings are only suggestive and await further investigation on the issue with a more representative sample. The cross-sectional design of the study also constrained implications due to potential bidirectionality of social activities and depressive symptoms. In addition, investigation needs to include other ethnic immigrants to see whether the similar findings are observed across groups.
Despite these limitations, the present study contributed to research and practice on mental health of immigrant older adults and highlighted the importance of understanding contextual factors. By investigating the role of acculturation in the widely known link between social activities and depressive symptoms, we were able to explore within-group variations in a group of immigrant older adults and identify subgroups of individuals that might be a target of interventions. Our findings on the particular benefits of social participation among those with low acculturation suggest that enhancing opportunities for social engagement may serve as a way to protect and promote the mental health of these vulnerable older adults. Indeed, interventions that foster the development of meaningful social roles and active engagement in the local community have demonstrated positive changes in quality of life and the health of socially isolated older populations (e.g., Ciechanowski et al., 2004; Greaves & Farbus, 2006). Interventions and social programs may not only help less acculturated elders to become more involved in meaningful social activities but also have psychological benefits.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:
The project was supported by the National Institute of Mental Health Research Grant Program (1R21MH081094; PI—Yuri Jang, PhD).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aiken L, West S. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science and Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Buchman AS, Boyle PA, Wilson RS, Fleischman DA, Leurgans S, Bennett DA. Association between late-life social activity and motor decline in older adults. Archives of Internal Medicine. 2009;169:1139–1146. doi: 10.1001/archinternmed.2009.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiriboga DA, Black SA, Aranda M, Markides K. Stress and depressive symptoms among Mexican American elders. Journal of Gerontology: Psychological Sciences. 2002;57B:P559–P568. doi: 10.1093/geronb/57.6.p559. [DOI] [PubMed] [Google Scholar]
- Cho MJ, Nam JJ, Suh GH. Prevalence of symptoms of depression in a nationwide sample of Korean adults. Psychiatry Research. 1998;81:341–352. doi: 10.1016/s0165-1781(98)00122-x. [DOI] [PubMed] [Google Scholar]
- Choi J, Wilbur J, Miller A, Szalacha L, McAuley E. Correlates of leisure-time physical activity in Korean immigrant women. Western Journal of Nursing Research. 2008;30:620–638. doi: 10.1177/0193945907310645. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, Diehr P, … LoGerfo J. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. Journal of the American Medical Association. 2004;291:1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- Fillenbaum G. Multidimensional functional assessment: The Duke older Americans resources and services procedure. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Glass TA, Mendes de Leon CF, Bassuk SS, Berkman LF. Social engagement and depressive symptoms in late life: Longitudinal findings. Journal of Aging and Health. 2006;18:604–628. doi: 10.1177/0898264306291017. [DOI] [PubMed] [Google Scholar]
- Greaves CJ, Farbus L. Effects of creative and social activity on the health and well-being of socially isolated older people: Outcomes from a multi-method observational study. Journal of the Royal Society for the Promotion of Health. 2006;126(3):134–142. doi: 10.1177/1466424006064303. [DOI] [PubMed] [Google Scholar]
- Harlow RE, Cantor N. Still participating after all these years: A study of life task participation in later life. Journal of Personality and Social Psychology. 1996;71:1235–1249. doi: 10.1037//0022-3514.71.6.1235. [DOI] [PubMed] [Google Scholar]
- Havighurst R. Psychological aspects of aging. Washington, DC: American Psychological Association; 1956. [Google Scholar]
- Hazuda HP, Stern MP, Haffner SM. Acculturation and assimilation among Mexican-Americans: Scales and population-based data. Social Science Quarterly. 1988;69:687–706. [Google Scholar]
- Hong SI, Hasche L, Bowland S. Structural relationships between social activities and longitudinal trajectories of depression among older adults. The Gerontologist. 2009;49(1):1–11. doi: 10.1093/geront/gnp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurh W. The Korean Americans. Westport, CT: Greenwood; 1998. [Google Scholar]
- Isaac V, Stewart R, Artero S, Ancelin ML, Ritchie K. Social activity and improvement in depressive symptoms in older people: A prospective community cohort study. American Journal of Geriatric Psychiatry. 2009;17:688–696. doi: 10.1097/JGP.0b013e3181a88441. [DOI] [PubMed] [Google Scholar]
- Jang Y, Chiriboga DA. Living in a different world: Acculturative stress among Korean American elders. Journal of Gerontology: Psychological Sciences. 2010;65B(1):14–21. doi: 10.1093/geronb/gbp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Y, Kim G, Chiriboga DA, King-Kallimanis B. A bidimensional model of acculturation for Korean American older adults. Journal of Aging Studies. 2007;21:267–275. doi: 10.1016/j.jaging.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Y, Mortimer JA, Haley WE, Borenstein-Graves A. The role of social engagement in life satisfaction: Its significance among older individuals with disease and disability. Journal of Applied Gerontology. 2004;23:266–278. [Google Scholar]
- Kim G, Chiriboga DA, Jang Y, Lee S, Huang CH, Parmelee P. Health status of older Asian Americans in California. Journal of the American Geriatrics Society. 2010;58:2003–2008. doi: 10.1111/j.1532-5415.2010.03034.x. [DOI] [PubMed] [Google Scholar]
- Lemon BW, Bengtson VL, Peterson JA. An exploration of the activity theory of aging: Activity types and life satisfaction among in-movers to a retirement community. Journal of Gerontology. 1972;27:511–523. doi: 10.1093/geronj/27.4.511. [DOI] [PubMed] [Google Scholar]
- Maier H, Klumb PL. Social participation and survival at older ages: Is the effect driven by activity content or context? European Journal of Ageing. 2005;2:31–39. doi: 10.1007/s10433-005-0018-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland G, Judd C. Statistical difficulties for detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Min J, Moon A, Lubben J. Determinants of psychological distress over time among older Korean immigrants and non-Hispanic White elders: Evidence from a two-wave panel study. Aging and Mental Health. 2005;9:210–222. doi: 10.1080/13607860500090011. [DOI] [PubMed] [Google Scholar]
- Morrow-Howell N, Hinterlong J, Rozario P, Tang F. The effects of volunteering on the well-being of older adults. Journals of Gerontology: Social Sciences. 2003;58:S137–S145. doi: 10.1093/geronb/58.3.s137. [DOI] [PubMed] [Google Scholar]
- Myers H, Rodriguez N. Acculturation and physical health in racial and ethnic minorities. In: Chun K, Organista P, Marin G, editors. Acculturation: Advances in theory, measurement, and applied research. Washington, DC: American Psychological Association; 2002. pp. 163–185. [Google Scholar]
- Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Memorial Fund Quarterly-Health and Society. 1976;54:439–467. [PubMed] [Google Scholar]
- Noh S, Avison WR, Kaspar V. Depressive symptoms among Korean immigrants: Assessment of a translation of the Center for Epidemiologic Studies Depression Scale. Psychological Assessment. 1992;4(1):84–91. [Google Scholar]
- Oh YJ, Koeske GF, Sales E. Acculturation, stress, and depressive symptoms among Korean immigrants in the United States. Journal of Social Psychology. 2002;142:511–526. doi: 10.1080/00224540209603915. [DOI] [PubMed] [Google Scholar]
- Perkins JM, Multhaup KS, Perkins HW, Barton C. Self-efficacy and participation in physical and social activity among older adults in Spain and the United States. The Gerontologist. 2008;48(1):51–58. doi: 10.1093/geront/48.1.51. [DOI] [PubMed] [Google Scholar]
- Phinney JS, Flores J. “Unpackaging” acculturation: Aspects of acculturation as predictors of traditional sex role attitudes. Journal of Cross-Cultural Psychology. 2002;33:320–331. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rogler LH, Cortes DE, Malgady RG. Acculturation and mental health status among Hispanics: Convergence and new directions for research. American Psychologist. 1991;46:585–597. doi: 10.1037//0003-066x.46.6.585. [DOI] [PubMed] [Google Scholar]
- Rosow I, Breslau N. A Guttman Health Scale for the aged. Journal of Gerontology. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- Rowe JW, Kahn RL. Successful aging. New York, NY: Pantheon; 1998. [Google Scholar]
- Sam D, Berry J. The Cambridge handbook of acculturation psychology. Cambridge, UK: Cambridge University Press; 2006. [Google Scholar]
- Su YP, Ferraro KF. Social relations and health assessments among older people: Do the effects of integration and social contributions vary cross-culturally? Journal of Gerontology: Social Sciences. 1997;52B(1):S27–S36. doi: 10.1093/geronb/52b.1.s27. [DOI] [PubMed] [Google Scholar]
- Suinn RM, Ahuna C, Khoo G. The Suinn-Lew Asian Self-Identity Acculturation Scale: Concurrent and factorial validation. Educational and Psychological Measurement. 1992;52:1041–1046. [Google Scholar]
- U.S. Census Bureau. Selected characteristics of the native and foreign-born populations: American Community Survey 2008. 2009 Retrieved from http://www.census.gov/prod/2009pubs/10statab/pop.pdf.
- Yang K, Laffrey SC, Stuifbergen A, Im EO, May K, Kouzekanani K. Leisure-time physical activity among midlife Korean immigrant women in the US. Journal of Immigrant Minority Health. 2007;9:291–298. doi: 10.1007/s10903-007-9039-9. [DOI] [PubMed] [Google Scholar]
- Ying YW. Cultural orientation and psychological well-being in Chinese Americans. American Journal of Community Psychology. 1995;23:893–911. doi: 10.1007/BF02507020. [DOI] [PubMed] [Google Scholar]