Abstract
Background Ideal internal fixation of the scaphoid relies on adequate bone stock for screw purchase; so, knowledge of regional bone density of the scaphoid is crucial.
Questions/Purpose The purpose of this study was to evaluate regional variations in scaphoid bone density.
Materials and Methods Three-dimensional CT models of fractured scaphoids were created and sectioned into proximal/distal segments and then into quadrants (volar/dorsal/radial/ulnar). Concentric shells in the proximal and distal pole were constructed in 2-mm increments moving from exterior to interior. Bone density was measured in Hounsfield units (HU).
Results Bone density of the distal scaphoid (453.2 ± 70.8 HU) was less than the proximal scaphoid (619.8 ± 124.2 HU). There was no difference in bone density between the four quadrants in either pole. In both the poles, the first subchondral shell was the densest. In both the proximal and distal poles, bone density decreased significantly in all three deeper shells.
Conclusion The proximal scaphoid had a greater density than the distal scaphoid. Within the poles, there was no difference in bone density between the quadrants. The subchondral 2-mm shell had the greatest density. Bone density dropped off significantly between the first and second shell in both the proximal and distal scaphoids.
Clinical Relevance In scaphoid fracture ORIF, optimal screw placement engages the subchondral 2-mm shell, especially in the distal pole, which has an overall lower bone density, and the second shell has only two-third the density of the first shell.
Keywords: scaphoid, bone density, subchondral, Hounsfield units
Internal fixation of the scaphoid has become increasingly popular as the first-line treatment for scaphoid fractures and is encouraged for the treatment of nonunions. 1 2 3 Ideal internal fixation relies on adequate bone stock for screw purchase; so, knowledge of regional bone density of the scaphoid is crucial.
Increased subchondral bone density has been described due to increased local forces, and for this reason, subchondral screws have been cited as superior. 4 5 These cadaver wrist studies have demonstrated increased bone density at the scaphoid and lunate fossa of the radius and corresponding increase in bone density in the scaphoid. Actual density of the subchondral bone, though, has never been formally measured. Increased bone density in the proximal pole of the scaphoid has also been described, likely due to increases in loading. 6 In a study by Cheung et al, in 2006, 6 wrist CT scans were reviewed, and proximal pole scaphoid marrow density was compared with distal pole marrow density. Proximal pole marrow density was found to be significantly higher than the distal pole density but differences in subchondral bone were not addressed. In 2012, Lee et al 5 looked at the osseous microarchitecture of the scaphoid. They performed micro CT scans of cadaver scaphoids and mapped out subchondral bone thickness and bone mineral density in eight different regions of the scaphoid. They found differences in subchondral bone thickness throughout the scaphoid; however, the density of the subchondral bone compared with the interior scaphoid was not reported.
We hypothesized that the bone density of the scaphoid was variable. We measured scaphoid bone density in concentric rings beginning at the most superficial subchondral bone and progressing internally into the core of the scaphoid. We also compared the proximal and distal poles of the scaphoid and evaluated the four quadrants of the proximal and distal poles (radial/ulnar/dorsal/volar).
Materials and Methods
Twelve acute scaphoid waist fractures were evaluated. All twelve fractures were nondisplaced. The average patient age was 34.3 years old (range, 18–62). Nine fractures were reported in male patients and three in female patients. Six patients were left hand dominant and six were right hand dominant. Average time from injury to CT scan was 11 days (range, 2–41 days). Three-dimensional models of fractured scaphoids were created using preoperative CT scans. Mimics (Materialise, Leuven, Belgium) software was used to indicate the proximal and distal poles on the in-line scaphoid reformatted images. After the proximal and distal poles were located, the scaphoid was sectioned in thirds to create proximal and distal sections ( Fig. 1 ). The proximal and distal poles were evaluated in the following two ways: (1) Two-millimeter concentric shells were created from the outer scaphoid segments to inner scaphoid of the proximal and distal poles ( Fig. 2 ) and (2) the proximal and distal poles of the scaphoid were divided into quadrants in radial-ulnar and volar-dorsal directions for comparison between these regions as well ( Fig. 3 ). Hounsfield units (HUs) were then measured in each region of the scaphoid to evaluate bone density using the method previously described by Schreiber et al. 7 8 Bone density of the scaphoid proximal and distal poles, the distal radius, and the capitate was measured by averaging three axial sections proximal to the physeal scar in the distal radius and three cross sections in the carpal bones as described by Schreiber et al. 7 8 Cortical regions were included in these measurements.
Fig. 1.
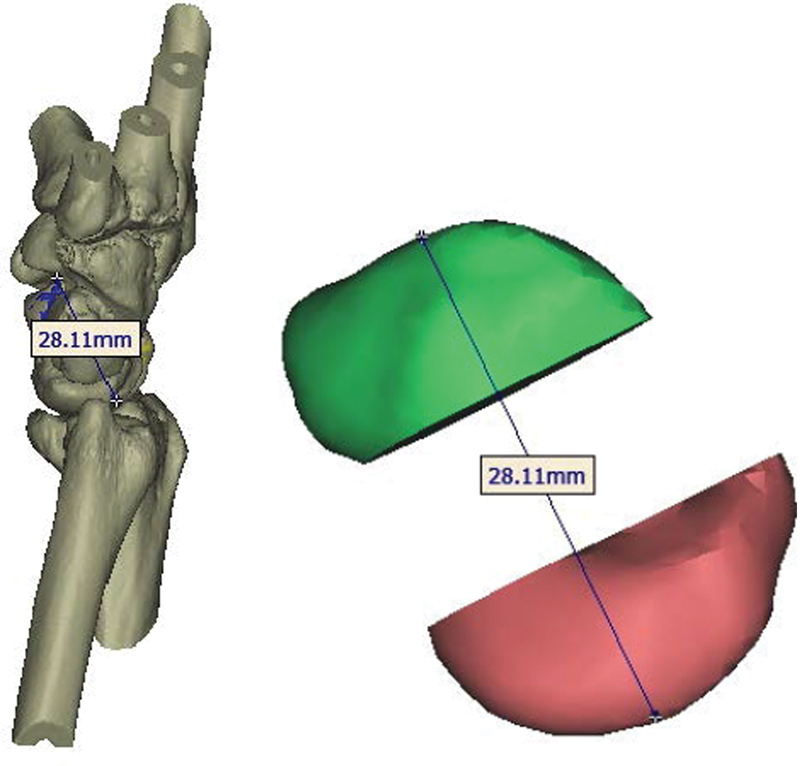
Sectioning of the scaphoid into proximal and distal poles.
Fig. 2.
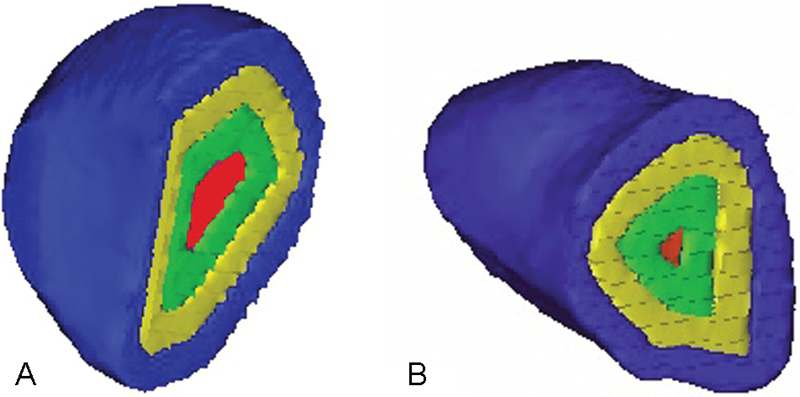
Two-mm concentric shells measuring scaphoid bone density from exterior (blue) to interior (red). ( A ) Proximal pole. ( B ) Distal pole.
Fig. 3.
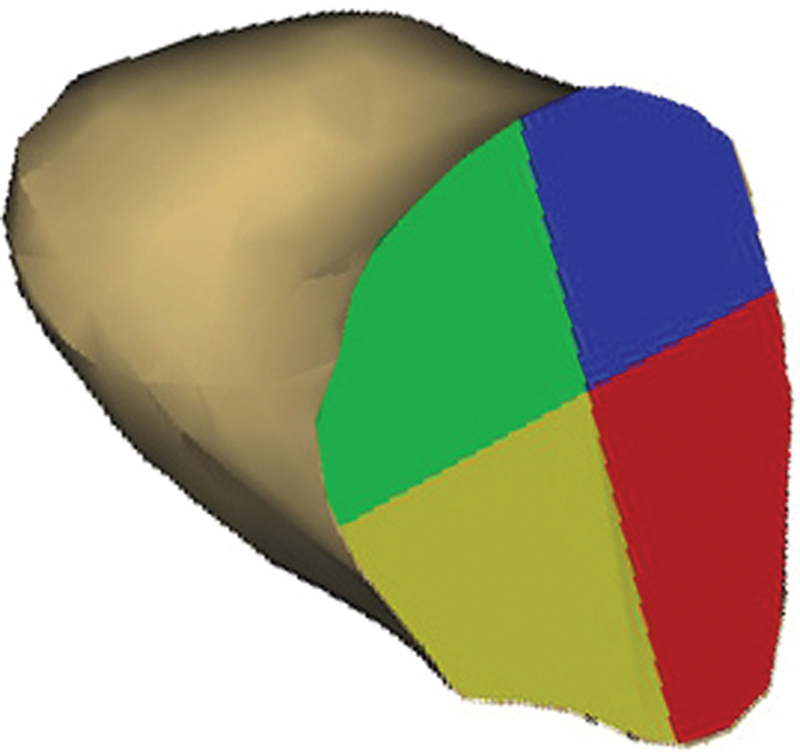
Division of the scaphoid into radial volar (red), radial dorsal (blue), ulnar volar (yellow), and ulnar dorsal (green) quadrants.
One-way ANOVAs were utilized to analyze the differences in bone density between the proximal pole, distal pole, and radius with multiple comparisons, and the p -values were adjusted using the Bonferroni technique. A similar statistical technique was used to compare bone density between the quadrants created. The incremental change in bone density of the 2-mm shells was analyzed using a general linear model to account for the clustered nature of the data with the Bonferroni technique used for p -value adjustments in the multiple comparison analyses. All data were reported as mean ± standard error. The p -values less than 0.05 were considered significant.
Results
Average bone density of the concentric shells and quadrants of scaphoid and of the distal radius and the capitate is listed in Table 1 .
Table 1. Mean and standard deviation of bone density in HU of four concentric shells and four quadrants of the proximal and distal poles of the scaphoid, and of the distal radius, and capitate.
| Proximal pole | Distal pole | |
|---|---|---|
| Scaphoid concentric shells | ||
| First shell | 710.5 ± 129.1 | 623.2 ± 107.8 |
| Second shell | 567.5 ± 126.9 | 395.4 ± 89.9 |
| Third shell | 512.7 ± 94.4 | 333.8 ± 72.6 |
| Fourth shell | 486.0 ± 77.4 | 295.1 ± 81.3 |
| Scaphoid quadrants | ||
| Radial volar quadrant | 605.6 ± 100.5 | 472.2 ± 92.0 |
| Radial dorsal quadrant | 649.2 ± 118.3 | 514.7 ± 74.2 |
| Ulnar volar quadrant | 638.4 ± 145.0 | 550.6 ± 115.4 |
| Ulnar dorsal quadrant | 673.3 ± 139.7 | 553.5 ± 114.2 |
| Distal radius | 272.9 ± 85.5 | |
| Capitate | 447.0 ± 66.1 | |
Proximal versus Distal Pole
There was a significant difference in bone density between the radius, proximal pole, and distal pole ( p < 0.01). The bone density of the distal pole was less than the proximal pole (453.2 ± 70.8 vs. 619.8 ± 124.2 HU, p < 0.01). The bone density of both the distal (453.2 ± 70.8 HU) and proximal (619.8 ± 124.2 HU) poles of the scaphoid were significantly greater than the bone density of the distal radius (272.9 ± 85.5 HU, p < 0.01 for both comparisons).
Quadrants
There was no significant difference in the bone density between the four quadrants in the proximal ( p > 0.05) or distal poles of the scaphoid ( p > 0.05; Fig. 4 ; Table 1 ).
Fig. 4.
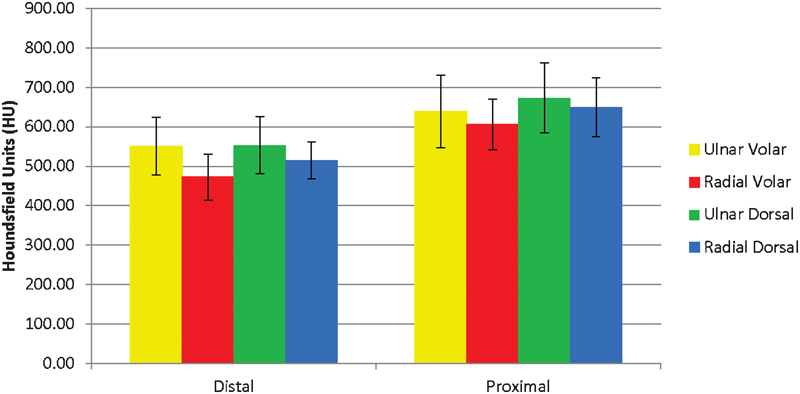
Average bone density of ulnar volar (yellow), radial volar (red), ulnar dorsal (green), and radial dorsal (blue) quadrants in the distal and proximal poles of the scaphoid.
Concentric Shells
In both poles, the first subchondral 2-mm shell had a greater bone density than the remaining deeper shells ( Fig. 5 , Table 1 ).
Fig. 5.
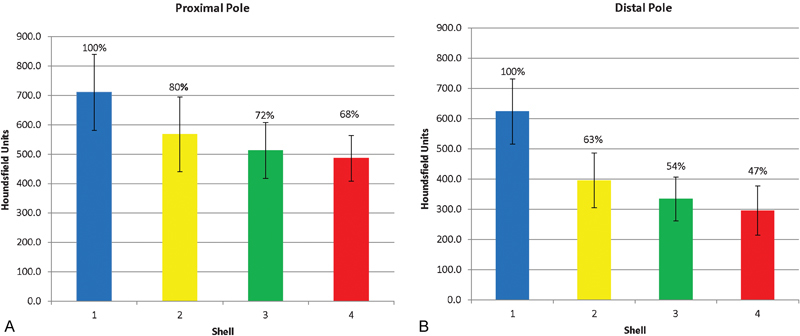
Bone density of 2-mm incremental shells of ( A ) proximal pole and ( B ) distal pole of the scaphoid. Shell 1 (blue) is the subchondral shell and shell 4 (red) is the innermost shell. Bone density as a percentage of shell 1 is indicated above the corresponding bar of each shell.
Proximal Pole
The outermost shells in the proximal scaphoid had a greater bone density than the innermost shells, and the bone density decreased from the subchondral to the innermost shell ( Fig. 5A ). When the bone density was compared with the subchondral densest shell, it dropped to 80% in the second shell, 72% in the third shell, and 68% in the interior most, fourth shell. The bone density of the subchondral shell (710.5 ± 129.1 HU) was significantly greater than the bone density of the second (567.5 ± 126.9 HU, p < 0.05), third (512.7 ± 94.4 HU, p = 0.001), and fourth (486.0 ± 77.4 HU, p < 0.001) inner shells.
Distal Pole
In the distal pole of the scaphoid, the bone density also decreased from the outermost shells to the innermost shells ( Fig. 5B ). Bone density of the second shell was 63% of the bone density of the subchondral shell and this decreased to 54 and 47% of the subchondral shell in the third and fourth shells, respectively. The bone density of the subchondral shell (623.2 ± 107.8 HU) was significantly greater than the bone density of the second (395.4 ± 89.9 HU, p < 0.001), third (333.8 ± 72.6, p < 0.001), and fourth (295.1 ± 81.3 HU, p < 0.001) inner shells.
Discussion
The correlation of bone density to compression and pull-out screw strength has been shown at multiple sites in the body. 9 10 11 12 13 For this reason, a clear understanding of the relative bone density of different regions of the scaphoid is essential to allow for screw placement that will yield maximum compression and strength.
Proximal versus Distal Pole
The proximal pole of the scaphoid had a greater bone density than the distal pole. This corroborates the work done by Cheung et al in 2006, 6 who showed an increase in proximal pole density in intact and fractured scaphoids. Loading patterns across the wrist and the changes from the fracture may explain this difference. It has been hypothesized that the proximal pole of the scaphoid had increased bone density because the radioscaphoid joint sustained the majority of force transmission from the carpus to the forearm. 4 14 15 Madelay et al in 2006 16 hypothesized that this difference might be due to a relative decrease in distal pole bone density following scaphoid fracture. They showed a disproportionate reduction in bone density in the distal pole as compared with the proximal pole as time from fracture increased, thereby producing an overall denser proximal pole after fracture. Clinically, with decreased distal pole density, it is important to maximize length of fixation in the distal pole. With volar retrograde screws, this is already accomplished because the head is sunk right below the articular surface. With antegrade dorsal screws, the decreased bone density in the distal pole makes it important to have as long a screw as possible in the distal pole to engage as much of the less dense distal pole as possible.
Quadrants
Within the proximal and distal scaphoid, we found no differences in bone density between dorsal, volar, radial, or ulnar quadrants. This contrasts the work done in 2012 by Lee et al 5 in which they reported the radial side of the body of the scaphoid to have the highest bone density followed by the midcarpal body (articulating with distal radius and capitate). The lowest bone mineral density was the radial side of the distal tuberosity articulating with the trapezium. This study was performed in an elderly population (average age, 61.2 years) of nonfractured scaphoids, which may be the reason for this difference as the population of scaphoid fractures were typically younger and more active. Clinically, the lack of difference in bone density of the quadrants means that the location of the starting or endpoint of the screw will not affect the compression strength of the screw based on bone density. For example, a dorsal screw is not better than a volar one, and a radial screw is not better than an ulnar one. Although the volar radial bone was the least dense, this was not significant.
Concentric Shells
The subchondral 2-mm shell of the scaphoid had the greatest bone density. Bone density in the scaphoid decreased from the subchondral shell to its core, with significant differences between the subchondral shell and all the other shells. In the distal pole, the second shell had only two-third the density of the subchondral shell. In the proximal pole, the third shell had only three-fourth the density of the subchondral shell. This demonstrates the importance of subchondral screw placement, especially in the distal pole. Because of the overall decreased density of the distal pole and the significant drop in density deep to the subchondral shell, it is especially important that the leading tip of the screw be subchondral for maximal screw purchase.
Biomechanical studies have shown that centrally placed longer screws, 2 mm from the cortex, resulted in greater stability across varying forearm–wrist positions compared with shorter screws. 17 18 This correlates with our finding that the greatest bone density was in the subchondral shell.
This computational model of actual scaphoid fractures has many strengths. We were able to evaluate scaphoids that represented normal age and gender of patients who traditionally sustained scaphoid fractures. This is in contrast to typical cadaver studies. We also used fractured scaphoids, with the inherent changes that occurred after fracture and would have affected bone density in this population.
We used a method of determining bone density using CT scans rather than dual-energy X-ray absorptiometry (DEXA), which some may consider a limitation. However, this method of correlating HU with DEXA scores has been shown to be reliable. 7 8 Our distal radius and capitate bone density findings are comparable to those of Schreiber et al. 8 Additionally, Todisco et al in 2005 19 showed that bone mineral density on CT scan directly correlated to bone volume on histomorphometry. Norton in 2001 20 showed that HU correlated with bone quality, and Ahlo in 1998 21 showed a significant correlation between HU and trabecular bone mineral density.
In conclusion, for scaphoid fracture fixation, maximal screw purchase engages the subchondral 2-mm shell of both poles. It is especially important for scaphoid screws to engage the 2-mm subchondral bone in the distal pole due to the overall lower bone density in the distal pole and because the subchondral shell has 157% of the bone density of the next deeper shell. While it is advantageous to have ideal screw purchase for fracture-implant construct stability, it is unacceptable to leave a screw prominent in the joint, and ideal screw placement should be within subchondral bone.
Ethical Board Approval
Institutional ethical board review approval was obtained from the Institutional Review Board (IRB) of the Hospital for Special Surgery.
Conflict of Interest None.
Note
This work was performed at the Hospital for Special Surgery, New York.
References
- 1.Buijze G A, Ochtman L, Ring D. Management of scaphoid nonunion. J Hand Surg Am. 2012;37(05):1095–1100. doi: 10.1016/j.jhsa.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Symes T H, Stothard J. A systematic review of the treatment of acute fractures of the scaphoid. J Hand Surg Eur Vol. 2011;36(09):802–810. doi: 10.1177/1753193411412151. [DOI] [PubMed] [Google Scholar]
- 3.Buijze G A, Doornberg J N, Ham J S, Ring D, Bhandari M, Poolman R W. Surgical compared with conservative treatment for acute nondisplaced or minimally displaced scaphoid fractures: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2010;92(06):1534–1544. doi: 10.2106/JBJS.I.01214. [DOI] [PubMed] [Google Scholar]
- 4.Hoogbergen M M, Niessen W J, Schuurman A H, Spauwen P H, Kauer J M. Subchondral bone mineral density patterns representing the loading history of the wrist joint. J Hand Surg Br. 2002;27(02):150–154. doi: 10.1054/jhsb.2001.0714. [DOI] [PubMed] [Google Scholar]
- 5.Lee S B, Kim H J, Chun J M et al. Osseous microarchitecture of the scaphoid: Cadaveric study of regional variations and clinical implications. Clin Anat. 2012;25(02):203–211. doi: 10.1002/ca.21198. [DOI] [PubMed] [Google Scholar]
- 6.Cheung Y Y, Naspinsky S R, Goodwin D W, Murphy J M, Nutting J T. Increased radiodensity of the proximal pole of the scaphoid: a common finding in computed tomography imaging of the wrist. J Comput Assist Tomogr. 2006;30(05):850–857. doi: 10.1097/01.rct.0000214249.59593.8e. [DOI] [PubMed] [Google Scholar]
- 7.Schreiber J J, Anderson P A, Rosas H G, Buchholz A L, Au A G. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93(11):1057–1063. doi: 10.2106/JBJS.J.00160. [DOI] [PubMed] [Google Scholar]
- 8.Schreiber J J, Gausden E B, Anderson P A, Carlson M G, Weiland A J. Opportunistic osteoporosis screening - gleaning additional information from diagnostic wrist CT scans. J Bone Joint Surg Am. 2015;97(13):1095–1100. doi: 10.2106/JBJS.N.01230. [DOI] [PubMed] [Google Scholar]
- 9.Faran K J, Ichioka N, Trzeciak M A, Han S, Medige J, Moy O J. Effect of bone quality on the forces generated by compression screws. J Biomech. 1999;32(08):861–864. doi: 10.1016/s0021-9290(99)00076-7. [DOI] [PubMed] [Google Scholar]
- 10.Gruszka D S, Burkhart K J, Nowak T E, Achenbach T, Rommens P M, Müller L P. The durability of the intrascaphoid compression of headless compression screws: in vitro study. J Hand Surg Am. 2012;37(06):1142–1150. doi: 10.1016/j.jhsa.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Ab-Lazid R, Perilli E, Ryan M K, Costi J J, Reynolds K J. Pullout strength of cancellous screws in human femoral heads depends on applied insertion torque, trabecular bone microarchitecture and areal bone mineral density. J Mech Behav Biomed Mater. 2014;40:354–361. doi: 10.1016/j.jmbbm.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Reynolds K J, Cleek T M, Mohtar A A, Hearn T C. Predicting cancellous bone failure during screw insertion. J Biomech. 2013;46(06):1207–1210. doi: 10.1016/j.jbiomech.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 13.Lehman R A, Jr, Kang D G, Wagner S C. Management of osteoporosis in spine surgery. J Am Acad Orthop Surg. 2015;23(04):253–263. doi: 10.5435/JAAOS-D-14-00042. [DOI] [PubMed] [Google Scholar]
- 14.Schuind F, Cooney W P, Linscheid R L, An K N, Chao E Y. Force and pressure transmission through the normal wrist. A theoretical two-dimensional study in the posteroanterior plane. J Biomech. 1995;28(05):587–601. doi: 10.1016/0021-9290(94)00093-j. [DOI] [PubMed] [Google Scholar]
- 15.Iwasaki N, Minami A, Miyazawa T, Kaneda K. Force distribution through the wrist joint in patients with different stages of Kienböck's disease: using computed tomography osteoabsorptiometry. J Hand Surg Am. 2000;25(05):870–876. doi: 10.1053/jhsu.2000.16353. [DOI] [PubMed] [Google Scholar]
- 16.Madeley N J, Stephen A B, Downing N D, Davis T R. Changes in scaphoid bone density after acute fracture. J Hand Surg Br. 2006;31(04):368–370. doi: 10.1016/j.jhsb.2006.03.164. [DOI] [PubMed] [Google Scholar]
- 17.Dodds S D, Panjabi M M, Slade J F., III Screw fixation of scaphoid fractures: a biomechanical assessment of screw length and screw augmentation. J Hand Surg Am. 2006;31(03):405–413. doi: 10.1016/j.jhsa.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 18.McCallister W V, Knight J, Kaliappan R, Trumble T E. Central placement of the screw in simulated fractures of the scaphoid waist: a biomechanical study. J Bone Joint Surg Am. 2003;85-A(01):72–77. doi: 10.2106/00004623-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Todisco M, Trisi P. Bone mineral density and bone histomorphometry are statistically related. Int J Oral Maxillofac Implants. 2005;20(06):898–904. [PubMed] [Google Scholar]
- 20.Norton M R, Gamble C. Bone classification: an objective scale of bone density using the computerized tomography scan. Clin Oral Implants Res. 2001;12(01):79–84. doi: 10.1034/j.1600-0501.2001.012001079.x. [DOI] [PubMed] [Google Scholar]
- 21.Alho A, Husby T, Høiseth A. Bone mineral content and mechanical strength. An ex vivo study on human femora at autopsy. Clin Orthop Relat Res. 1988;227(227):292–297. [PubMed] [Google Scholar]


