Abstract
Background Around 5 to 15% of all scaphoid fractures result in nonunion. Treatment of long-lasting scaphoid nonunion remains a challenge for the treating surgeon. Healing of scaphoid nonunion is essential for prevention of scaphoid nonunion advanced collapse and the subsequent predictable pattern of radiocarpal osteoarthritis.
Purpose The purpose of this study was to investigate the feasibility of fixation of the scaphoid nonunion with a volar angular stable miniplate and cancellous bone grafting. We hypothesized that this technique could be successful, even in patients with previous surgery for nonunion and in patients with a long duration of nonunion.
Patients and Methods A total of 21 patients enrolled in a single-center prospective cohort study. Healing of nonunion was assessed on multiplanar computed tomography scan of the wrist at a 3-month interval. Functional outcome was assessed by measuring grip strength, range of motion, and by means of the patient-rated wrist and hand evaluation (PRWHE) questionnaire.
Results During follow-up, 19 out of 21 patients (90%) showed radiological healing of the nonunion. The range of motion did not improve significantly. Postoperative PRWHE scores decreased by 34 points. Healing occurred regardless of the length of time of the nonunion (range: 6–183 months) and regardless of previous surgery (38% of patients).
Conclusion Volar angular stable miniplate fixation with autologous cancellous bone grafting is a successful technique for the treatment of chronic unstable scaphoid nonunion, even in patients with long-lasting nonunion and in patients who underwent previous surgery for a scaphoid fracture. Rotational interfragmentary stability might be an important determining factor for the successful treatment of unstable scaphoid nonunion.
Level of Evidence Level IV.
Keywords: scaphoid nonunion, internal fixation, plating
Fractures of the scaphoid are the most common carpal fractures and account for 60% of all carpal fractures, 10% of all hand fractures, and 2% of all fractures. 1 Most undisplaced fractures will unite after conservative treatment with a plaster for 4 to 8 weeks. 2 Several anatomical aspects of the scaphoid fracture are crucial for the time and likelihood of union; proximal pole fractures have a nonunion rate of up to 30 to 40% with conservative treatment. 3 4 5 Fracture displacement of >1 mm, comminution and humpback deformity increase the nonunion rate significantly. 2 5 6
Healing of scaphoid nonunion is essential for prevention of carpal collapse and subsequent progressive osteoarthritis. The first internal fixation of a scaphoid nonunion was described by McLaughlin in 1954. 7 After the introduction of the double-threaded, twin pitch headless screw by Herbert and Fisher in 1984 the operative treatment gained popularity. 8 Headless screw fixation combined with volar grafting of a cancellous bone wedge achieves union in 82 to 95% of cases of surgery for nonunion. 9 10 Despite its relative success, there are occasions when scaphoid screw fixation is not an ideal treatment option for treatment of nonunion. Examples include cases of persistent nonunion after scaphoid screw fixation or cases of significant bone loss where screw purchase may be compromised. From the mechanical standpoint, in comparison to compression screws, the buttress plate provides an alternative method of internal fixation for a collapsed fracture. It is considered to provide an improved mechanical construct that meets the anatomical and biomechanical requirements of unstable fractures with the tendency of their fragments to collapse axially. The use of plates to treat the nonunion of the scaphoid has been described previously. 11 12 13 14 15
There are numerous factors that can adversely affect the outcome of surgery for scaphoid nonunion. Besides the radiological and anatomical aspects such as a sclerotic nonunion, humpback deformity, and the vascularization of the proximal fragment, certain patient characteristics, such as age, smoking, and occupation adversely affect the outcomes of surgical treatment. 2 3 5 Also, it is believed that previous surgery for scaphoid fracture or nonunion and long duration of the scaphoid nonunion also adversely affect the outcome of surgery for scaphoid nonunion. 16 We believe that rigid fixation and interfragmentary rotational stability is a determining factor for the successful outcome of scaphoid nonunion surgery. We hypothesized that treatment of chronically unstable scaphoid nonunion with a volar angular stable miniplate and cancellous bone grafting is a successful technique, even in patients with long-lasting nonunion. It can be a successful technique in patients who underwent previous surgery for a scaphoid fracture.
Patients and Methods
Between November 2013 and May 2016, 21 patients with a scaphoid nonunion were enrolled in this prospective cohort study. Consecutive patients with a proximal pole fragment large enough to accommodate three angular stable screws were enrolled. The possibility of plate removal was discussed with each patient, before inclusion. Patients were treated using a volar angular-stable miniplate and cancellous bone grafting technique. Patient characteristics are summarized in Table 1 . Patients with and without previous surgery of a scaphoid fracture were included in the study. All nonunions were diagnosed preoperatively on multiplanar reconstruction computed tomography (MRCT) with 1 mm slice thickness and coronal and sagittal reconstructions. In all patients, a preoperative magnetic resonance imaging (MRI) was made for determination of possible avascularity of the proximal pole. In concordance with the study by Fox et al, avascular necrosis of the proximal pole of the scaphoid was diagnosed on the enhanced T1-weighted fat-suppressed sequences when the signal intensity in the proximal pole was qualitatively less than the signal in the distal pole. 17
Table 1. Patient characteristics and preoperative findings of physical examination and MRI and/or CT imaging.
| Characteristics | Findings | |
|---|---|---|
| Number of patients | 21 | |
| Sex | 20/21 male | (95% male) |
| Age (y) | 31 | (18–76) |
| Avascular necrosis on MRI | 5/21 | (24%) |
| Sclerotic nonunion | 10/21 | (47%) |
| Proximal pole fracture | 6/21 | (29%) |
| Humpback deformity | 10/21 | (47%) |
| DISI | 9/21 | (43%) |
| SNAC | 6/21 | (29%) |
| Previous surgery | 8/21 | (38%) |
| Average duration of nonunion (mo) | 41 | (6–183) |
Abbreviations: CT, computed tomography; DISI, dorsal intercalated segment instability; MRI, magnetic resonance imaging; SNAC, scaphoid nonunion advanced collapse.
For functional assessment, the range of motion of the affected wrist and grip strength were evaluated. The range of active extension, flexion, radial, and ulnar deviation was determined using a handheld goniometer, and the sum was expressed as a proportion of that of the opposite, unaffected wrist. Grip strength was measured using a JAMAR dynamometer (Sammons Preston Rolyan, Bolingbrook, IL) and expressed as a proportion of the grip strength on the unaffected side. Also, the patient-rated wrist and hand evaluation (PRWHE) was used to assess the level of fracture related functional deficit and pain level from the patient's perspective. The PRWHE is a 15-item questionnaire that allows patients to rate the level of wrist pain and disability in activities of daily living via a 10-point categorical scale from 0 (no pain/difficulty) to 10 (worst pain ever/unable to do). 18 All patients were required to fill in the PRWHE questionnaire at baseline 3, 6, 9, and 12 months after surgery. Postoperatively nonunion healing was assessed by performing MRCT scans of the wrist using the technique used by Sanders at a 3-month interval until the union was achieved. A set of scans consisted of the 1.0 mm source transverse images and sagittal and coronal multiplanar reconstructions in the central longitudinal axis of the scaphoid. 19 The extent of the union was quantified as described by Singh et al and judged independently by a musculoskeletal radiologist and a trauma surgeon. 20 Since Singh et al demonstrated that even fractures with only 25% union after 12 to 18 weeks would heal within 1 year, we feel it is safe to consider a nonunion healed when at least 50% of the whole width of the scaphoid showed signs of trabecular bridging after 3 months ( Fig. 1 ). Functional outcomes were determined at a 3-month interval postoperatively using the methods mentioned above. The plate was removed only in patients with functional deficits or pain due to the interposition of the plate in the radiocarpal joint. Any deviation from the normal postoperative course without the need for pharmacological or surgical treatment was deemed a minor complication. All other complications were regarded major complications. Plate removal was not considered a complication, as it is regarded mandatory by the manufacturer of the plates.
Fig. 1.
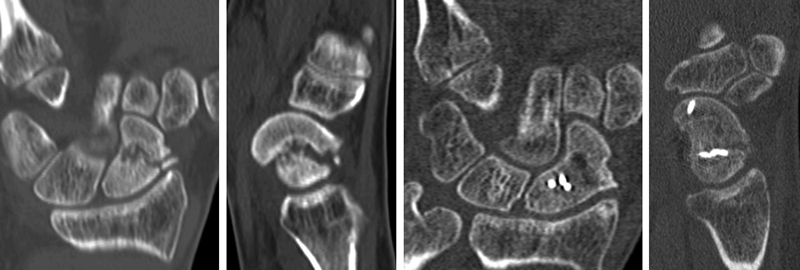
Assessment of union by CT scan at 3 months postoperatively. CT, computed tomography.
Operative Technique
The patient is placed in supine position with the affected hand outstretched on an arm table with a tourniquet inflated to 250 mmHg around the upper arm. A modified Henry approach is used to access the radioscaphocapitate ligament. The ligament is opened, and the volar surface of the scaphoid is exposed. The nonunion is debrided, and carpal alignment is corrected using 1.2 mm Kirschner wires (K-wires) ( Fig. 2 ). In the case of a dorsal intercalated segment instability (DISI) deformity, an extension of the lunate was corrected using a 1.6 mm K-wire. Punctate bleeding of the proximal pole is assessed after the release of the tourniquet, which correlated in all cases with the preoperative MRI. After correction of scaphoid geometry, internal fixation of the scaphoid is performed using a precontoured angular stable 1.5 mm miniplate (Aptus hand; Medartis, Switzerland). We aim to have three variable angled locking screws at either side of the fracture. Following fixation, the autologous cancellous bone graft is added from the ipsilateral iliac crest ( Fig. 3 ). The position of the plate, scaphoid geometry, and carpal alignment are checked by fluoroscopy ( Fig. 4 ). This includes identifying if the plate impinges on the volar rim of the radius, confirming that humpback deformity is corrected and that the screws do not violate the articulations around the scaphoid. The wound is then irrigated. The radioscaphocapitate ligament is restored with a Vicryl 3–0 suture (Ethicon) before closing the skin. A volar wrist splint is applied postoperatively for 7 to 10 days before starting active wrist movement. After 7 to 10 days of surgery, patients visited the outpatient department to check for early complications. Patients are then submitted to a 3-month interval follow-up regime as previously described.
Fig. 2.
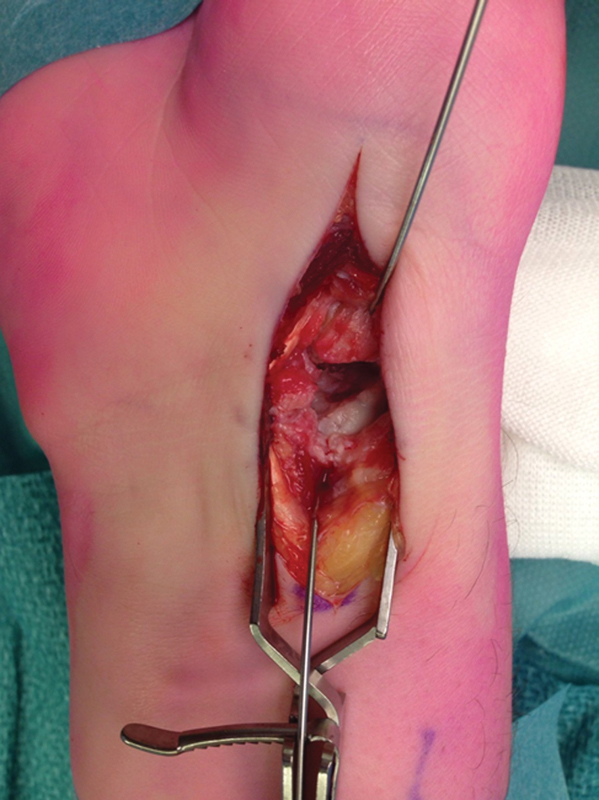
The nonunion is debrided, and carpal alignment is corrected using 1.2 mm K-wires. K-wires, Kirschner wires.
Fig. 3.
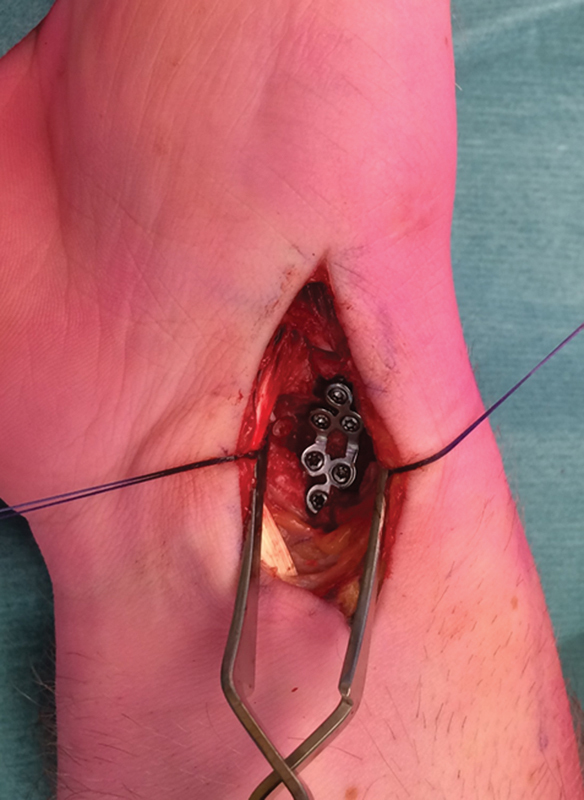
Application and fixation of the 1.5 mm miniplate.
Fig. 4.
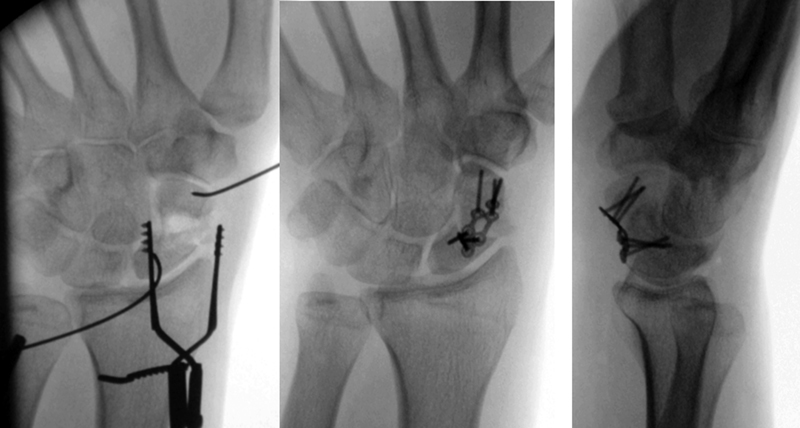
Assessment of scaphoid geometry and plate positioning.
Results
Patient characteristics are summarized in Table 1 . A total of 21 patients (20 males, mean age 31 years) with an unstable scaphoid nonunion were included in our prospective cohort study and completed a minimal follow-up of 3 months postoperatively. The average duration of nonunion was 41 months. Five patients (24%) had signs of avascular necrosis of the proximal pole on preoperative MRI ( Fig. 5 ). Overall, 10 patients (47%) had a sclerotic nonunion, 6 patients (29%) had a proximal pole nonunion, and 10 patients (49%) showed a humpback deformity of the scaphoid. Also, nine patients (43%) had DISI, and six patients (29%) had signs of a stage 1 scaphoid nonunion advanced collapse of the wrist. Eight patients (38%) underwent previous surgery of the scaphoid.
Fig. 5.
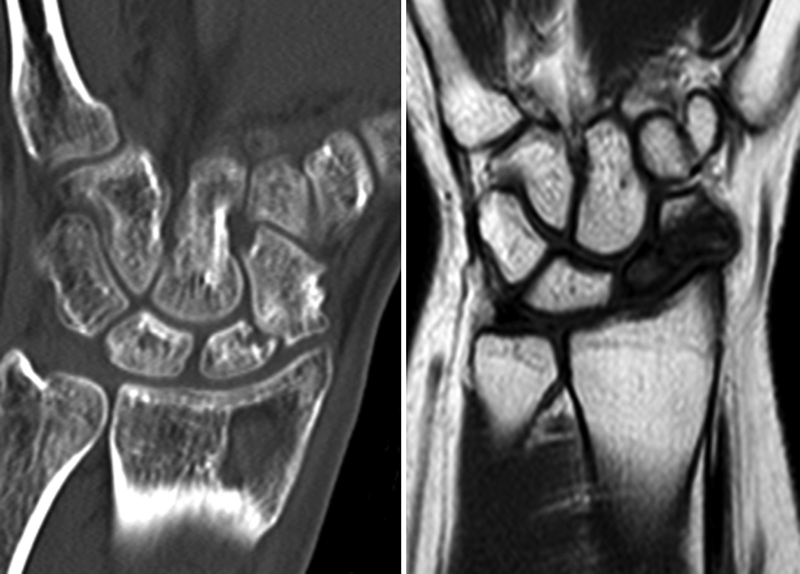
Example of scaphoid nonunion as diagnosed on CT scan and signs of avascular necrosis on the corresponding T1-weighted sequence MRI. CT, computed tomography; MRI, magnetic resonance imaging.
Outcomes are summarized in Table 2 . Median follow-up was 14 months with a range of 4 to 30 months. Out of 21, 19 nonunions were united on follow-up CT scan, correlating with a success rate of 90%. Average time to union was 4.2 months. At 3, 6, 9, and 12 months, union rates were 52, 76, 86, and 90%, respectively.
Table 2. Outcomes of volar angular stable miniplate and cancellous bone grafting.
| Radiological outcomes a | ||
|---|---|---|
| Union on CT-scan | ||
| 3 mo | 11/21 | 52% |
| 6 mo | 16/21 | 76% |
| 9 mo | 18/21 | 86% |
| 12 mo | 19/21 | 90% |
| Functional outcomes b | (Preoperative) | (Postoperative) |
| PRWHE | 59 points | 25 points |
| Grip strength | 68% | 64% |
| Range of motion | 102 degrees | 106 degrees |
| Complications and plate removal | ||
| Major | 0/21 | 0% |
| Minor | 1/21 | 0,05% |
| Plate removal | 6/21 | 29% |
Abbreviations: CT, computed tomography; PRWHE, patient-rated wrist and hand evaluation.
Radiological outcomes as assessed on CT scan at 3, 6, 9, and 12 months after surgery.
Functional outcomes as measured at the time of union as assessed by follow-up CT scan.
Out of the 21 patients, 2 patients did not achieve union after 6 months. The first patient was a 21-year-old male with a 14-month-old proximal pole nonunion, initially treated with a single screw fixation. The preoperative CT scan showed a sclerotic nonunion with a humpback deformation and a DISI. After 6 months, a follow-up CT scan showed no signs of fracture healing and a broken proximal screw. We decided to remove the plate and screws. Subsequently, the scaphoid bone was remodeled using a corticocancellous wedge bone graft harvested from the ipsilateral iliac crest. The nonunion was again fixated this time using a trapezoidal 8-hole locking miniplate (Medartis). The second patient was a 50-year-old male with a 96-month-old proximal pole fracture, initially treated with a single screw fixation. The preoperative CT scan showed a sclerotic nonunion with a humpback deformation and a DISI deformity. The preoperative MRI showed an avascular proximal pole. After 6 months, a follow-up CT scan showed only minimal signs of fracture healing and migration of one of the proximal screws. Again, we decided to remove the plate and screws. The scaphoid bone was remodeled using a corticocancellous wedge bone graft harvested from the ipsilateral iliac crest. The nonunion was again fixated using a six-hole 1.5 mm angular stable miniplate (Medartis). Both patients are currently being followed up.
The mean range of motion did not differ significantly at final follow-up with a preoperative range of motion. Grip strength did not differ significantly as well, with outcomes of 68% of the contralateral hand preoperatively to 64% postoperatively at the time of union. PRWHE scores improved significantly from 59 points preoperatively to 25 points postoperatively at the time of union as demonstrated on CT scan. One patient had hypertrophic scar tissue formation as a minor complication. There were no major complications. In six patients (29%) the plate was removed postoperatively (range: 3–12 months after surgery). In three patients this was because of pain and/or impairment in flexion of the wrist joint. In two patients the plate intervened in the radiocarpal joint on the postoperative CT scan in full flexion of the wrist. In one patient, the plate was removed during a revision surgery for an extensive and complex wrist trauma involving intra-articular radial fracture and a perilunate dislocation.
Discussion
To our knowledge, this is the only prospective series published to describe volar angular stable miniplate in combination with cancellous bone grafting for scaphoid nonunion. With a 90% union rate after an average time of 4.5 months, our technique proved successful for treating chronic unstable scaphoid nonunion. The duration of nonunion did not influence the healing of nonunion and previous surgery was not decisive for the outcome. The functional outcomes improved postoperatively as measured by the PRWHE questionnaire from 58 to 25 points.
The past decades, numerous techniques have been developed to achieve bone healing of the scaphoid nonunion. These techniques aim to improve the vascularization of the nonunion and/or try to improve the stability of the nonunited scaphoid.
Since Matti and Russe described the application of an autologous bone graft for nonunions in 1937 and 1960, respectively, numerous techniques have been developed trying to improve the vascularization of the proximal part of the scaphoid nonunion. 21 22 The Matti–Russe technique uses corticocancellous autografts that are placed in the cleared nonunion site. Autografts from the iliac crest or distal radius are just as successful. 23 Union rates after this procedure vary from 72 to 87%. 24 25 Vascularized bone grafts can be harvested locally (either dorsally or volary at the site of the distal radius) or remotely from the medial femoral condyle. The most commonly used dorsal vascularized bone graft is the 1,2 intercompartmental supraretinacular artery with reported union rates ranging from 60 to 100%. 26 For the volar local vascularized bone graft the pedicle just distal to the pronator quadratus is used with satisfactory rates of union. 27 28
To add stability to the scaphoid nonunion different methods of internal fixation have been suggested throughout the years. Currently, there is a wide diversity of screws available for fixation of scaphoid nonunions. The most widely used screws are the headless compression screw and the AO small fragment screw. Christodoulou et al compared the AO small fragment screw with the Herbert screw and K-wires and found union rates of 85, 77, and 55%, respectively. 29 Small series of double screw fixation have been described. 30 An arthroscopic assist for scaphoid fixation can be useful to assess the quality of the reduction, the stability of fixation, and to assess hardware position. 31 Historically, the use of plate fixation by means of AO plates was first described by Braun et al. 11 The Ender compression hooked blade plate system was suggested by Huene and Stankovic. 12 32 In 2011 Ghoneim retrospectively reviewed the effectiveness of the anterior wedge graft and internal fixation with the use of a volar buttress plate, achieving 93% union in a series of 14 patients with a scaphoid nonunion. 13 Dodds et al described a novel combination of a vascularized volar distal radius autograft in combination with a volar buttress plate for the treatment of chronic scaphoid nonunions. 14 Union was confirmed in eight out of nine (89%) patients. 33 In 2015 Bain et al found that dorsal scaphoid plating provides a more stable construct than the traditional Herbert screw and mitigates the need for vascular or cancellous bone grafting in most cases with a union rate of 90%. 15
We believe plate fixation has several advantages over single screw fixation and vascularized bone grafts. First of all, despite including scaphoid nonunions with an avascular proximal pole, as confirmed by both preoperative MRI scan and intraoperative bleeding, the nonunions united after plate fixation with bone grafting. These results support our notion that interfragmentary stability is a key factor for healing and in line with the recently proposed theoretical framework of reducing strain on bone. 34 Also, a recent biomechanical study by Jurkowitsch et al demonstrated that plate fixation adds more stability than single screw fixation. 35 This might be a reason for the relative higher union rate in our series as compared with series using the traditional Herbert screw fixation. 29 Second, as compared with vascularized grafting, we describe a technique, which is less technically demanding and less invasive with a shorter operation time and with a comparable high union rate. Because of the tendency of the scaphoid to collide to the volar side into a humpback deformity, we feel that volar plating provides a biomechanical more stable construct than dorsal plating.
As described we have seen two persisting nonunions in this series. In both patients, we saw a failure of the proximal screws with one screw breakage and one screw migration. One possible explanation could be that due to the ultraproximal placement of the plate, stability was compromised due to friction created by the interference of the plate against the volar rim of the radius. Another possible explanation might be an insufficient grip of the screws in the proximal fragment. For us, this stresses the necessity of sufficient corticocancellous grip of the screws in the proximal pole, and it underlines the strong preference to place three screws in the proximal fragment. For cases where the insufficient grip of the screws in the proximal fragment can be achieved, or in cases where the proximal fragment is too small to accommodate three screws, volar miniplate fixation might not be an ideal technique for treatment of the scaphoid nonunion. Our study has some caveats. The main limitation of this study is the relatively small sample size, although the current results represent the largest published series so far. Furthermore, due to the short follow-up of these patients, no definitive conclusions can be drawn concerning the long-term outcome of wrist function as well as the effectiveness of this technique in preventing a scaphoid nonunion advanced collapse of the radiocarpal and intercarpal joints. However, since significant functional improvement is observed postoperatively in this series with relatively short follow-up, long-term results are expected to be promising.
Conclusion
We conclude that volar angular stable miniplate fixation with autologous cancellous bone grafting is a successful technique for the treatment of chronic unstable scaphoid nonunion, even in patients with a long lasting nonunion. It can be a successful technique in patients who underwent previous surgery for a scaphoid fracture. We believe that rotational interfragmentary stability is an important determining factor for the successful treatment of unstable scaphoid nonunion.
Ethical Review Committee Statement
This study was conducted according to the revised version of the Declaration of Helsinki (October 2013).
Footnotes
Conflict of Interest None.
References
- 1.Hove L M. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999;33(04):423–426. doi: 10.1080/02844319950159145. [DOI] [PubMed] [Google Scholar]
- 2.Clementson M, Jørgsholm P, Besjakov J, Björkman A, Thomsen N. Union of scaphoid waist fractures assessed by CT scan. J Wrist Surg. 2015;4(01):49–55. doi: 10.1055/s-0034-1398472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leslie I J, Dickson R A. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg Br. 1981;63-B(02):225–230. doi: 10.1302/0301-620X.63B2.7217146. [DOI] [PubMed] [Google Scholar]
- 4.Eastley N, Singh H, Dias J J, Taub N. Union rates after proximal scaphoid fractures; meta-analyses and review of available evidence. J Hand Surg Eur Vol. 2013;38(08):888–897. doi: 10.1177/1753193412451424. [DOI] [PubMed] [Google Scholar]
- 5.Singh H P, Taub N, Dias J J. Management of displaced fractures of the waist of the scaphoid: meta-analyses of comparative studies. Injury. 2012;43(06):933–939. doi: 10.1016/j.injury.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Grewal R, Suh N, Macdermid J C. Use of computed tomography to predict union and time to union in acute scaphoid fractures treated nonoperatively. J Hand Surg Am. 2013;38(05):872–877. doi: 10.1016/j.jhsa.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 7.McLaughlin H L. Fracture of the carpal navicular (scaphoid) bone; some observations based on treatment by open reduction and internal fixation. J Bone Joint Surg Am. 1954;36-A(04):765–774. [PubMed] [Google Scholar]
- 8.Herbert T J, Fisher W E. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66(01):114–123. doi: 10.1302/0301-620X.66B1.6693468. [DOI] [PubMed] [Google Scholar]
- 9.Daly K, Gill P, Magnussen P A, Simonis R B. Established nonunion of the scaphoid treated by volar wedge grafting and Herbert screw fixation. J Bone Joint Surg Br. 1996;78(04):530–534. [PubMed] [Google Scholar]
- 10.Filan S L, Herbert T J. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Br. 1996;78(04):519–529. [PubMed] [Google Scholar]
- 11.Braun C, Gross G, Bühren V. Osteosynthesis using a buttress plate--a new principle for stabilizing scaphoid pseudarthroses [in German] Unfallchirurg. 1993;96(01):9–11. [PubMed] [Google Scholar]
- 12.Huene D R, Huene D S. Treatment of nonunions of the scaphoid with the Ender compression blade plate system. J Hand Surg Am. 1991;16(05):913–922. doi: 10.1016/s0363-5023(10)80160-1. [DOI] [PubMed] [Google Scholar]
- 13.Ghoneim A. The unstable nonunited scaphoid waist fracture: results of treatment by open reduction, anterior wedge grafting, and internal fixation by volar buttress plate. J Hand Surg Am. 2011;36(01):17–24. doi: 10.1016/j.jhsa.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Dodds S D, Patterson J T, Halim A. Volar plate fixation of recalcitrant scaphoid nonunions with volar carpal artery vascularized bone graft. Tech Hand Up Extrem Surg. 2014;18(01):2–7. doi: 10.1097/BTH.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 15.Bain G I, Turow A, Phadnis J. Dorsal Plating of Unstable Scaphoid Fractures and Nonunions. Tech Hand Up Extrem Surg. 2015;19(03):95–100. doi: 10.1097/BTH.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 16.Tambe A D, Cutler L, Stilwell J, Murali S R, Trail I A, Stanley J K. Scaphoid non-union: the role of vascularized grafting in recalcitrant non-unions of the scaphoid. J Hand Surg [Br] 2006;31(02):185–190. doi: 10.1016/j.jhsb.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 17.Fox M G, Wang D T, Chhabra A B. Accuracy of enhanced and unenhanced MRI in diagnosing scaphoid proximal pole avascular necrosis and predicting surgical outcome. Skeletal Radiol. 2015;44(11):1671–1678. doi: 10.1007/s00256-015-2221-6. [DOI] [PubMed] [Google Scholar]
- 18.Hoang-Kim A, Pegreffi F, Moroni A, Ladd A. Measuring wrist and hand function: common scales and checklists. Injury. 2011;42(03):253–258. doi: 10.1016/j.injury.2010.11.050. [DOI] [PubMed] [Google Scholar]
- 19.Sanders W E. Evaluation of the humpback scaphoid by computed tomography in the longitudinal axial plane of the scaphoid. J Hand Surg Am. 1988;13(02):182–187. doi: 10.1016/s0363-5023(88)80045-5. [DOI] [PubMed] [Google Scholar]
- 20.Singh H P, Forward D, Davis T R, Dawson J S, Oni J A, Downing N D. Partial union of acute scaphoid fractures. J Hand Surg [Br] 2005;30(05):440–445. doi: 10.1016/j.jhsb.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Matti H. Uber die behandlung der navicularfracture und der refractura patellae durch Plombierung mit Spongiosa [in German] Zentralbl Chir. 1937;64:2353–2359. [Google Scholar]
- 22.Russe O. Fracture of the carpal navicular. Diagnosis, non-operative treatment, and operative treatment. J Bone Joint Surg Am. 1960;42-A:759–768. [PubMed] [Google Scholar]
- 23.Tambe A DCL, Cutler L, Murali S R, Trail I A, Stanley J K. In scaphoid non-union, does the source of graft affect outcome? Iliac crest versus distal end of radius bone graft. J Hand Surg [Br] 2006;31(01):47–51. doi: 10.1016/j.jhsb.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Zarezadeh A, Moezi M, Rastegar S, Motififard M, Foladi A, Daneshpajouhnejad P.Scaphoid nonunion fracture and results of the modified Matti-Russe technique Adv Biomed Res 2015439. Doi: 10.4103/2277-9175.151248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kołodziej R KBJ, Blacha J, Bogacz A, Mazurkiewicz T. Long-term outcome of scaphoid nonunion treated by the Matti-Russe operation. Ortop Traumatol Rehabil. 2006;8(05):507–512. [PubMed] [Google Scholar]
- 26.Payatakes A, Sotereanos D G. Pedicled vascularized bone grafts for scaphoid and lunate reconstruction. J Am Acad Orthop Surg. 2009;17(12):744–755. doi: 10.5435/00124635-200912000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Kawai H, Yamamoto K. Pronator quadratus pedicled bone graft for old scaphoid fractures. J Bone Joint Surg Br. 1988;70(05):829–831. doi: 10.1302/0301-620X.70B5.3192587. [DOI] [PubMed] [Google Scholar]
- 28.Mathoulin C, Haerle M. Vascularized bone graft from the palmar carpal artery for treatment of scaphoid nonunion. J Hand Surg [Br] 1998;23(03):318–323. doi: 10.1016/s0266-7681(98)80049-1. [DOI] [PubMed] [Google Scholar]
- 29.Christodoulou L S, Kitsis C K, Chamberlain S T. Internal fixation of scaphoid non-union: a comparative study of three methods. Injury. 2001;32(08):625–630. doi: 10.1016/s0020-1383(01)00018-3. [DOI] [PubMed] [Google Scholar]
- 30.Croutzet P, Ferreira B, Gaston-Nouvel A et al. Benefits of a double antirotation screw fixation performed with arthroscopy for scaphoid fractures: A prospective series of 9 cases. J Hand Surg [Br] 2014;39(09):41–42. [Google Scholar]
- 31.Slutsky D J, Trevare J. Use of arthroscopy for the treatment of scaphoid fractures. Hand Clin. 2014;30(01):91–103. doi: 10.1016/j.hcl.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Stanković P, Burchhardt H. [Experience with the Ender hooked plate in the management of 42 scaphoid pseudarthroses] Handchir Mikrochir Plast Chir. 1993;25(04):217–222. [PubMed] [Google Scholar]
- 33.Dodds S D, Halim A. Scaphoid plate fixation and volar carpal artery vascularized bone graft for recalcitrant scaphoid nonunions. J Hand Surg Am. 2016;41(07):e191–e198. doi: 10.1016/j.jhsa.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Elliott D S, Newman K J, Forward D P et al. A unified theory of bone healing and nonunion: BHN theory. Bone Joint J. 2016;98-B(07):884–891. doi: 10.1302/0301-620X.98B7.36061. [DOI] [PubMed] [Google Scholar]
- 35.Jurkowitsch J, Dall'Ara E, Quadlbauer S et al. Rotational stability in screw-fixed scaphoid fractures compared to plate-fixed scaphoid fractures. Arch Orthop Trauma Surg. 2016;136(11):1623–1628. doi: 10.1007/s00402-016-2556-z. [DOI] [PubMed] [Google Scholar]


