Abstract
Background Displaced scaphoid fractures have a relatively high rate of nonunion. Detection of displacement is vital in limiting the risk of nonunion when treating scaphoid fractures.
Questions/Purpose We evaluated the ability to diagnose displacement on radiographs and computed tomography (CT), hypothesizing that displacement is underestimated in assessing scaphoid fracture by radiograph compared with CT.
Materials and Methods Thirty-five preoperative radiographs and CT scans of acute scaphoid fractures were evaluated by two blinded observers. Displacement and angular deformity were measured, and the fracture was judged as displaced or nondisplaced. Scapholunate, radiolunate, and intrascaphoid angles were measured. Radiograph and CT measurements between nondisplaced and displaced fractures were compared. Intraobserver reliability was measured.
Results Reader 1 identified 12 fractures as nondisplaced on radiograph, but displaced on CT (34%). Reader 2 identified 9 fractures as nondisplaced on radiograph, but displaced on CT (26%). For displaced fractures, the mean intrascaphoid angle was over three times greater when measured on CT than on radiograph (56 vs. 16 degrees). Scapholunate angle >65 degrees and radiolunate angle >16 degrees were significantly associated with displacement on CT. Interobserver reliability for diagnosing displacement was perfect on CT but less reliable on radiograph.
Conclusion Scaphoid fracture displacement on CT was identified in 26 to 34% of fractures that were nondisplaced on radiograph, confirming that radiographic evaluation alone underestimates displacement. These results underscore the importance of CT scan in determining displacement and angular deformity when evaluating scaphoid fractures, as it may alter the decision on treatment and surgical approach to the fracture. We recommend considering CT scan to evaluate all scaphoid fractures.
Level of Evidence Level III.
Keywords: scaphoid, fracture, displacement, computed tomography
Displaced scaphoid fractures have a relatively high rate of nonunion. Both adequate vascularity and stable immobilization are required for scaphoid fractures to heal reliably. Nonunion rates have ranged from 5 to 15% for all scaphoid fractures, with an increased risk among displaced fractures. 1 2 Singh et al showed that 18% of displaced scaphoid fractures treated nonoperatively result in nonunion and that the odds of nonunion in displaced scaphoid fractures treated with cast immobilization was 17 times greater compared with those treated with surgical fixation. 3
Although there is variability in interpretation of what constitutes displacement of scaphoid fractures, Cooney et al 4 defined displacement and instability as a fracture with greater than 1 mm of fracture displacement and 15 degrees of lunate tilt. It was suggested that, using this criteria, displacement and instability increases the risk of nonunion and the progression of degenerative changes of the radiocarpal joint. 5 Angulation of a displaced scaphoid fracture can predictably lead to flexion of the scaphoid into a “humpback deformity.” This can, in turn, result in dorsal intercalated segment instability. 6 In the treatment of scaphoid waist and proximal pole fractures, detection of displacement is vital in limiting the risk of nonunion and humpback deformity.
We measured acute scaphoid fracture displacement on radiographs and computed tomography (CT), testing the hypothesis that displacement is underestimated in assessing scaphoid fracture on radiographs compared with CT scan.
Materials and Methods
Patient Selection
After approval by the institutional Review Board, we retrospectively reviewed patient charts between 2011 and 2014 of operatively treated scaphoid waist or proximal pole acute fractures by two senior hand surgeons (M.G.C. and A.J.W.). Forty-five patients with preoperative radiographs and CT scans were identified. Ten patients who lacked preoperative radiographs loaded in the institutional PACS (picture archiving and communication system) system were excluded. A total of 35 patients were included with standardized preoperative radiographs (posteroanterior [PA], lateral, oblique, and scaphoid views) obtained at our institution and CT scans with fine-cut reconstructions in the sagittal long-axis plane of the scaphoid and coronal plane. The long axis of the scaphoid was identified in the coronal plane of the CT scan. Sagittal cuts were reformatted in the long axis of the scaphoid. This gives the “true” lateral of the scaphoid versus standard sagittal cuts in line with the long axis of the radius. Of these 35 patients, 32 were classified as waist fractures and 3 as proximal pole fractures.
Image Review
Two blinded orthopaedic hand fellow observers evaluated the radiographs and CT scans, randomly ordered, in two separate sessions. First, the radiographs were assessed for fracture displacement (cortical step-off or translation) and angular displacement (measured by sagittal intrascaphoid angle). Scapholunate, radiolunate, and capitolunate angles were measured. CT scans were evaluated for dorsal and volar gapping and angular displacement (intrascaphoid angle) using a series of coronal and sagittal cuts in the plane of the long axis of the scaphoid. The lateral intrascaphoid angles were measured by creating a perpendicular line to both the proximal and distal articular surfaces and measuring the resulting angle between these two lines as described by Amadio et al. 6 7 Finally, the observers were asked to make an overall judgment of the fracture as either displaced or nondisplaced based on cortical displacement, translation, or gapping of >1 mm on the PA or scaphoid radiographic views, as defined by Cooney et al, 4 and coronal and sagittal CT reconstructions in long-axis of the scaphoid.
Statistical Analysis
Mann–Whitney U -tests were used to assess radiographic measures of fractures that were read nondisplaced on radiographs but displaced on CT compared with fractures reported nondisplaced on both imaging modalities. Kappa statistics were calculated to evaluate the reliability of diagnosing displacement between raters. Intraclass correlation coefficient (ICC) was calculated to determine the reliability of the intrascaphoid angle measured on radiograph and CT.
Results
Determining Displacement
Reader 1 identified 10 fractures (29%) as displaced on radiographs and 22 (63%) as displaced on CT scan ( Fig. 1 ). Twelve fractures were recorded as nondisplaced on radiograph, but displaced on CT scan (34%) ( Fig. 2 ). Reader 2 identified 13 fractures (37%) as displaced on radiograph and 22 (63%) displaced on CT scan. Nine fractures were reported by reader 2 as nondisplaced on radiograph, but displaced on CT scan (26%). All fractures that were reported displaced on radiograph were also reported displaced on CT scan. Interobserver reliability for diagnosing displacement on CT was perfect (kappa = 1.00; p < 0.001), but interobserver reliability for diagnosing displacement on radiograph was good (kappa = 0.68; p < 0.001).
Fig. 1.
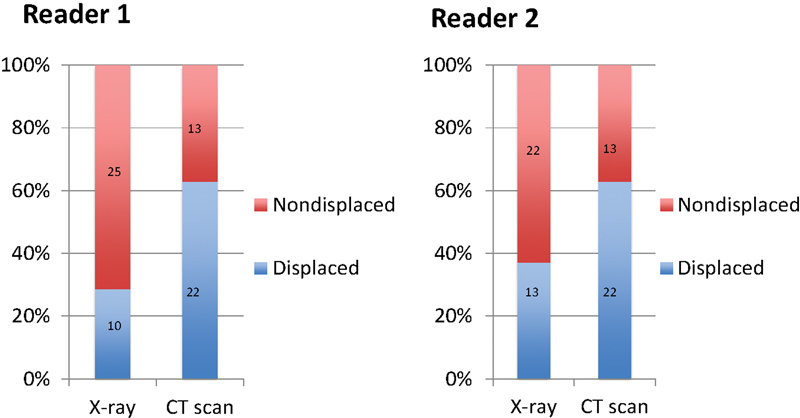
Overall judgment of scaphoid fracture displacement on X-ray and computed tomography scan for reader 1 and reader 2.
Fig. 2.

( A ) Scaphoid fracture rated as nondisplaced on plain radiograph. ( B ) Computed tomography scan of the same patient showing displacement and increased intrascaphoid angle not recognized on initial radiographs.
Measurements of Carpal Instability
Comparative analysis was calculated for two groups: group 1 represented the patients in which radiographs and CT scans were read as nondisplaced, and group 2 had radiographs read as nondisplaced but CT scans were recorded as displaced. There was no significant difference in capitolunate angle between group 1 (8.5 ± 6.7 degrees) and group 2 (10.2 ± 10.1 degrees; p > 0.05), or in intrascaphoid angle between group 1 (16.1 ± 9.4 degrees) and group 2 (8.5 ± 7.9 degrees; p > 0.05). There was no significant difference in scapholunate angle between group 1 (mean: 52.8 ± 10.3 degrees) and group 2 (57.8 ± 11.8 degrees; p > 0.05), or in radiolunate angle between group 1 (mean: 1.4 ± 8.7 degrees) and group 2 (5.6 ± 15.6 degrees; p > 0.05). However, when scapholunate angle was analyzed in a bimodal distribution of ≤65 or >65 degrees and radiolunate angle was analyzed as ≤16 and >16 degrees, there was an association of scaphoid displacement on CT scan with scapholunate angle >65 degrees ( p < 0.05) and radiolunate angle >16 degrees ( p < 0.05). In predicting displacement on CT scan, both scapholunate angle >65 degrees and radiolunate angle >16 degrees had a specificity of 100% and positive predictive value of 1.0 for both readers. Sensitivity, however, was low for both scapholunate angle >65 degrees (45% for both readers) and for radiolunate angle >16 degrees (30% for Reader 1 and 42% for Reader 2) ( Table 1 ). Eleven of 22 scaphoid fractures with normal scapholunate angles were displaced on CT scan.
Table 1. Sensitivity and specificity contingency table for scapholunate angle >65 degrees predicting scaphoid displacement on CT scan.
| Displaced on CT | Nondisplaced on CT | Total | |
|---|---|---|---|
| Scapholunate angle ≤ 65 degrees | 11 | 11 | 22 |
| Scapholunate angle > 65 degrees | 9 | 0 | 9 |
| Total | 20 | 11 | 31 |
Abbreviation: CT, computed tomography.
Flexion Deformity
In addition, there was no reliability between intrascaphoid angle (humpback deformity) measured on radiograph and CT scan (ICC = –0.52; p > 0.05). For the patients determined nondisplaced on radiograph and displaced on CT scan, the intrascaphoid angle was an average of 9 degrees on X-ray and 54 degrees on CT scan.
Discussion
In this study, the two readers identified scaphoid fracture displacement on CT in 26 and 34% of fractures that were initially designated nondisplaced by radiograph. Our hypothesis that radiographic evaluation alone underestimates displacement was confirmed. Although interobserver reliability between readers on radiographs was acceptable (68%), the reliability of diagnosing displacement between readers on CT was perfect (100%), demonstrating that among different readers, CT can provide a more reliable diagnosis of displacement. These results underscore the importance of CT scan in determining displacement and angular deformity. In accurately identifying displacement or step-off and scaphoid flexion deformity, the risk of nonunion and humpback deformity may be diminished.
The poor reliability in measuring the intrascaphoid angle on radiograph and CT highlights the difficulty in recognizing the flexion or humpback deformity using plain radiography alone. Increased dorsal tilt and evidence of carpal malalignment as measured by scapholunate angle >65 degrees and radiolunate angle >16 degrees were associated with displacement on CT, showing very high specificities, and can serve as indicators of scaphoid displacement when not otherwise detected on the plain films. 8 However, these measures had low sensitivity (55% of displaced fractures had normal scapholunate angles, and 58–70% of displaced fractures had normal radiolunate angles), indicating that many displaced fractures would be missed using these criteria on plain radiograph alone.
Limitations of this study include the retrospective nature and the effect of selection bias. All patients included in this study were treated operatively. After radiographs were reviewed, this study reported 34% of the fractures displaced among the operatively treated acute scaphoid fractures, which may be an increased incidence compared with other studies (10–30% displaced). 3 9 10 11 12 Both senior hand surgeons (M.G.C. and A.J.W.) in this study routinely recommend and offer operative fixation to nearly all healthy, active patients with scaphoid waist and proximal pole fracture regardless of displacement. However, including only operatively managed patients in this series may have artificially increased the incidence of displacement or number of patients who were offered surgical treatment after a CT scan was obtained or by excluding patient that elected for nonoperative treatment. The increased incidence of displacement may also be skewed, however, due to the inclusion of scaphoid nonunions in this study.
A lack of standardization in defining a displaced scaphoid fracture also limits our ability to make direct correlations between displacement and clinical outcomes. We applied the 1 mm of displacement threshold that Cooney et al put forth, defining a displaced or unstable fracture that portends a higher rate of nonunion. 4 13 The literature regarding the incidence of nonunion has been based on radiographic diagnoses. The 5 to 15% of radiographically diagnosed nondisplaced scaphoid fractures that progress to nonunion cited in other series may represent a subgroup of fractures that were actually displaced or unstable but underappreciated on conventional radiography. In addition, we currently do not have a standard for defining displacement on CT. We have extrapolated the 1-mm threshold of displacement on plain films to represent displacement or instability on CT, but the clinical significance of this threshold on CT is unclear.
Even using a standardizing definition of displacement, our ability to detect 1 mm of step-off or translation is difficult on plain radiograph alone and has been questioned. 14 15 Bernard et al 16 evaluated the ability to detect 1 mm of displacement on conventional radiographs predetermined by cadaveric osteotomy. Their results demonstrated an accuracy of 72% and poor-to-moderate interobserver reliability in determining displacement, concluding that plain radiography is not reliable in determining 1 mm of scaphoid waist fracture displacement. Temple et al 14 examined the sensitivity and specificity of plain radiography and CT in detecting >1 mm of displacement in cadaveric scaphoid fracture models among different specialties. Low sensitivity of 52% for plain film and 49% for CT implied that the diagnosis of displacement was inaccurate half of the time. They noted, consistently, that plain radiographs poorly detected sagittal plane displacement and that CT poorly identified coronal displacement, although they only evaluated sagittal plane CT series.
Our results are comparable to two other clinical studies that have sought to evaluate the sensitivity and specificity of radiographs versus CT in diagnosing displacement. Lozano-Calderón et al 15 found the interobserver reliability of CT alone, and the combination of CT and plain radiograph evaluation improved when compared with plain radiograph estimation alone (kappa values 0.43, 0.48, and 0.27). We agree that CT scan adds benefit between readers in diagnosing displacement, however, to a much greater degree with perfect correlation between our readers when making an overall determination of displacement on CT. This difference may be due to the technological advances in CT acquisition and reformatting in the long axis of the scaphoid. In a follow-up study, Buijze et al evaluated the performance of radiographs and CT in detecting displacement that correlated with instability on arthroscopic examination. 17 They raised the question as to whether displacement on CT accurately correlated with instability upon probing arthroscopically. However, it is not clear if this instability seen arthroscopically has clinical significance, especially in light of the traction placed across the wrist during the arthroscopic examination. Ultimately, it was concluded that CT and arthroscopy more clearly identify displacement and instability compared with radiographs alone.
Improved recognition of the displacement and flexion deformity of scaphoid fractures may have important implications in the treatment offered and surgical approach taken. Certainly, a CT scan should be obtained of any fracture diagnosed as nondisplaced on radiographs prior to electing nonoperative treatment to avoid misdiagnosis and the potential of an increased risk of nonunion. Proper restoration of anatomical carpal alignment and scaphoid morphology has been demonstrated to correlate with improved clinical outcomes in terms of grip strength, range of motion, and functional outcome scores. 18 19 Displacement and alignment can best be evaluated preoperatively with sagittal CT series in the long-axis plane of the scaphoid. A more accurate estimation of the flexion deformity may have significant implications such as potentially changing the surgeon's operative plan from a dorsal approach to a volar approach in an effort to correct the humpback deformity. For these reasons, we recommend a protocol of obtaining a CT scan to evaluate all scaphoid fractures prior to definitive treatment.
Conflict of Interest None.
Ethical Board Approval
Institutional ethical board review approval was obtained from the Hospital for Special Surgery's Institutional Review Board.
Note
This work was performed at the Hospital for Special Surgery, New York.
References
- 1.Osterman A L, Mikulics M. Scaphoid nonunion. Hand Clin. 1988;4(03):437–455. [PubMed] [Google Scholar]
- 2.Kuschner S H, Lane C S, Brien W W, Gellman H. Scaphoid fractures and scaphoid nonunion. Diagnosis and treatment. Orthop Rev. 1994;23(11):861–871. [PubMed] [Google Scholar]
- 3.Singh H P, Taub N, Dias J J. Management of displaced fractures of the waist of the scaphoid: meta-analyses of comparative studies. Injury. 2012;43(06):933–939. doi: 10.1016/j.injury.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Cooney W P, Dobyns J H, Linscheid R L. Fractures of the scaphoid: a rational approach to management. Clin Orthop Relat Res. 1980;(149):90–97. [PubMed] [Google Scholar]
- 5.Amadio P, Moran S. Philadelphia, PA: Elsevier; 2005. Fractures of the carpal bones; pp. 711–768. [Google Scholar]
- 6.Amadio P C, Berquist T H, Smith D K, Ilstrup D M, Cooney W P, III, Linscheid R L. Scaphoid malunion. J Hand Surg Am. 1989;14(04):679–687. doi: 10.1016/0363-5023(89)90191-3. [DOI] [PubMed] [Google Scholar]
- 7.Bain G I, Bennett J D, MacDermid J C, Slethaug G P, Richards R S, Roth J H. Measurement of the scaphoid humpback deformity using longitudinal computed tomography: intra- and interobserver variability using various measurement techniques. J Hand Surg Am. 1998;23(01):76–81. doi: 10.1016/S0363-5023(98)80093-2. [DOI] [PubMed] [Google Scholar]
- 8.Roh Y H, Noh J H, Lee B K et al. Reliability and validity of carpal alignment measurements in evaluating deformities of scaphoid fractures. Arch Orthop Trauma Surg. 2014;134(06):887–893. doi: 10.1007/s00402-014-1998-4. [DOI] [PubMed] [Google Scholar]
- 9.Szabo R M, Manske D. Displaced fractures of the scaphoid. Clin Orthop Relat Res. 1988;(230):30–38. [PubMed] [Google Scholar]
- 10.Dabezies E J, Mathews R, Faust D C. Injuries to the carpus. Orthopedics. 1982;5(11):1510–1521. doi: 10.3928/0147-7447-19821101-13. [DOI] [PubMed] [Google Scholar]
- 11.Bhat M, McCarthy M, Davis T R, Oni J A, Dawson S. MRI and plain radiography in the assessment of displaced fractures of the waist of the carpal scaphoid. J Bone Joint Surg Br. 2004;86(05):705–713. doi: 10.1302/0301-620x.86b5.14374. [DOI] [PubMed] [Google Scholar]
- 12.Thorleifsson R, Karlsson J, Sigurjonsson K. Fractures of the scaphoid bone. A follow-up study. Arch Orthop Trauma Surg. 1984;103(02):96–99. doi: 10.1007/BF00389579. [DOI] [PubMed] [Google Scholar]
- 13.Cooney W P, Linscheid R L, Dobyns J H, Wood M B. Scaphoid nonunion: role of anterior interpositional bone grafts. J Hand Surg Am. 1988;13(05):635–650. doi: 10.1016/s0363-5023(88)80116-3. [DOI] [PubMed] [Google Scholar]
- 14.Temple C L, Ross D C, Bennett J D, Garvin G J, King G J, Faber K J. Comparison of sagittal computed tomography and plain film radiography in a scaphoid fracture model. J Hand Surg Am. 2005;30(03):534–542. doi: 10.1016/j.jhsa.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Lozano-Calderón S, Blazar P, Zurakowski D, Lee S G, Ring D. Diagnosis of scaphoid fracture displacement with radiography and computed tomography. J Bone Joint Surg Am. 2006;88(12):2695–2703. doi: 10.2106/JBJS.E.01211. [DOI] [PubMed] [Google Scholar]
- 16.Bernard S A, Murray P M, Heckman M G. Validity of conventional radiography in determining scaphoid waist fracture displacement. J Orthop Trauma. 2010;24(07):448–451. doi: 10.1097/BOT.0b013e3181c3e865. [DOI] [PubMed] [Google Scholar]
- 17.Buijze G A, Jørgsholm P, Thomsen N O, Bjorkman A, Besjakov J, Ring D. Diagnostic performance of radiographs and computed tomography for displacement and instability of acute scaphoid waist fractures. J Bone Joint Surg Am. 2012;94(21):1967–1974. doi: 10.2106/JBJS.K.00993. [DOI] [PubMed] [Google Scholar]
- 18.Megerle K, Harenberg P S, Germann G, Hellmich S. Scaphoid morphology and clinical outcomes in scaphoid reconstructions. Injury. 2012;43(03):306–310. doi: 10.1016/j.injury.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 19.Lynch N M, Linscheid R L. Corrective osteotomy for scaphoid malunion: technique and long-term follow-up evaluation. J Hand Surg Am. 1997;22(01):35–43. doi: 10.1016/S0363-5023(05)80177-7. [DOI] [PubMed] [Google Scholar]


