Abstract
A growing body of research suggests that impulsive responses to emotion more robustly predict suicidality than do other forms of impulsivity. This issue has not yet been examined within bipolar disorder, however. Participants diagnosed with bipolar I disorder (n = 133) and control participants (n = 110) diagnosed with no mood or psychotic disorder completed self-report measures of emotion-triggered impulsivity (Negative and Positive Urgency Scales) and interviews concerning lifetime suicidality. Analyses examined the effects of emotion-triggered impulsivity alone and in combination with gender, age of onset, depression severity, comorbid anxiety, comorbid substance use, and medication. A history of suicide ideation and attempts, as well as self-harm, were significantly more common in the bipolar disorder group compared with the control group. Impulsive responses to positive emotions related to suicide ideation, attempts, and self-harm within the bipolar group. Findings extend research on the importance of emotion-triggered impulsivity to a broad range of key outcomes within bipolar disorder. The discussion focuses on limitations and potential clinical implications.
A large body of literature establishes that suicide rates are highly elevated in bipolar I disorder. Across studies, suicide deaths in bipolar disorder have been estimated to occur at 20 to 30 times the rate observed in the general population (Pompili et al., 2013; Schaffer, Isometsa, Tondo, Moreno, Sinyor et al., 2015; Schaffer, Isometsa, Tondo, Moreno, Turecki et al., 2015). In two prospective studies, one involving 3,291,891 Veterans Administration patients (Ilgen et al., 2010) and the other a national cohort of individuals who were followed for 36 years after a first psychiatric contact (Nordentoft, Mortensen, & Pedersen, 2011), bipolar disorder was found to be the psychiatric condition with the highest rate of suicide. In the national cohort study, 8% of men and 5% of women diagnosed with bipolar disorder died from suicide (Nordentoft et al., 2011). In the representative sample of the World Mental Health Survey, one in four persons diagnosed with bipolar I disorder reported a suicide attempt and more than half reported suicide ideation within the past 12 months (Merikangas et al., 2011). Similar rates of ideation and attempts were reported in a community representative sample of those with bipolar I disorder in the Netherlands (ten Have, Vollebergh, & Nolen, 2002).
In the general population, impulsivity has been found to predict suicide attempts (Brezo, Paris, & Turecki, 2006), using both self-report personality measures and performance-based measures of impulsivity (Jollant et al., 2007; Swann, 2005), although effects were found to be modest in a recent systematic meta-analysis of 70 studies (Anestis, Soberay, Gutierrez, Hernandez, & Joiner, 2014). It has long been suggested that suicide attempts within bipolar disorder are also related to the high rates of impulsivity in that disorder. Impulsive traits are elevated among those with remitted bipolar disorder (Muhtadie, 2013; Strakowski Johnson, Carver, Gotlib, & Ketter, 2010; Swann, Pazzaglia, Nicholls, Dougherty, and Moeller, 2003) and predict the onset of bipolar spectrum disorders (Alloy et al., 2009; Kwapil, Miller, Zinser, Chapman, Chapman, & Eckblad, 2000).
As with research in general community and patient samples, research on impulsivity and suicide attempts in bipolar disorder has produced mixed findings. One study found no significant relationship of a self-report measure of trait-like impulsivity with suicide attempts in a sample of 652 persons diagnosed with bipolar I or II disorder (Parmentier et al., 2012). Watkins and Meyer (2013) identified 16 studies of impulsivity and suicide attempts within bipolar disorder. Across 12 studies using the Barrett Impulsivity Scale, no consistent link emerged with suicide attempts. With respect to behavioral indicators of impulsivity, persons with bipolar disorder who displayed impulsive responses on the Iowa Gambling Task (Malloy-Diniz, Neves, Abrantes, Fuentes, & Correa, 2009; MALLOY-DINIZ et al., 2011) and on the Immediate Memory Task (Swann, Dougherty, Pazzaglia, Pham, Steinberg, & Moeller, 2005; Swann et al., 2003) had elevations in suicide attempts. On the whole, however, findings have not provided the strong support for impulsivity as an indicator that one might expect.
One possible explanation for the limited effect sizes could be the need to focus on specific facets of impulsivity. A growing body of research suggests that impulsivity is an umbrella concept that has quite diverse facets. Multiple separable dimensions of trait-like impulsivity have been identified, including urgency in response to negative emotions, sensation seeking, and (lack of) perseverance (Whiteside & Lynam, 2001). These dimensions have only modest intercorrelations and differential effects on other outcomes (Sharma, Markon, & Clark, 2014). The vast majority of the studies of impulsivity and suicide attempts within bipolar disorder have relied on the self-report Barratt Impulsiveness Scale (BIS; Barratt, 1965). This measure might not capture the forms of impulsivity that are most relevant for suicidal behavior.
One form of impulsivity that appears particularly relevant to suicidal ideation and behavior in the general population is negative urgency. As operationalized in the Negative Urgency Scale of the multiscale UPPS (Whiteside & Lynam, 2001), urgency is the tendency to respond to states of negative emotion with rash or regrettable behavior. Negative Urgency correlates with syndromes (and associated symptoms) directly related to risk for suicidal ideation and behavior, including depressive symptoms (Gallardo-Pujol, Andres-Pueyo, & Maydeu-Olivares, 2013), borderline personality disorder symptoms and diagnoses (Whiteside & Lynam, 2003; Whiteside, Lynam, Miller, & Reynolds, 2005), impulse-control disorders (Nock, Prinstein, & Sterba, 2009), and nonsuicidal self-injury (Black & Mildred, 2014; Glenn & Klonsky, 2010; Mullins-Sweatt, Lengel, & Grant, 2009; Peterson, Davis-Becker, & Fischer, 2014; Peterson & Fischer, 2012; Rawlings, Shevlin, Corcoran, Morriss, & Taylor, 2015). Negative Urgency has also been found to be related to composite measures of nonsuicidal self-injury and to suicidal ideation and behavior (Lynam, Miller, Miller, Bornovalova, & Lejeuz, 2011). In a recent meta-analysis of 115 studies (40,432 participants) using the UPPS (Whiteside & Lynam, 2001), the Negative Urgency Scale was significantly related to a composite of suicidal ideation and behavior and nonsuicidal self-injury, with an effect size, r = .25, that was larger than effects observed for other forms of impulsivity such as lack of premeditation, lack of perseverance, and sensation seeking, rs = .16–.18 (Berg, Latzman, Bliwise, & Lilienfeld, 2015).
Negative Urgency has also been found to correlate with indices of suicidality severity (Dvorak, Lamis, & Malone, 2013), with suicide ideation in a sample of 2,011 military recruits, 1,296 college students, and 399 high school students (Klonsky & May, 2010), with suicide attempts among inpatients with substance use disorders (Anestis, Tull, Lavender, & Gratz, 2014; Lynam, Gaughan, Miller, Mullins-Sweatt, & Widiger, 2011), and in a 7-year longitudinal study, with faster time to suicide attempts among patients diagnosed with depression or personality disorders (Yen et al., 2009). Taken together, findings suggest that Negative Urgency may be a particularly relevant form of impulsivity for understanding suicidal ideation and behavior. One possibility is that for those with this form of impulsivity, negative emotions more quickly spiral into globally negative thoughts as well as reflexive, regrettable behaviors expressive of the emotion state due to a lack of constraint over emotions (Carver, Johnson, & Joormann, 2008).
The Negative Urgency Scale focuses on impulsivity in the context of negative emotions. Given that focus, research linking Negative Urgency with suicidal ideation or behavior could be criticized as confounding negative emotionality with impulsivity. Partly because of this limitation of the Negative Urgency Scale, Cyders, Smith, Spillane, Fischer, Annus, and Peterson (2007) developed the Positive Urgency Measure (PUM), which measures tendencies to respond to positive emotion states with rash thought and behavior. By examining Positive Urgency as a correlate of suicidal ideation or behavior, one could differentiate between the tendency toward heightened negative emotionality and the tendency to become impulsive during states of heightened emotion more generally. Findings suggest that Positive Urgency Scores are related to higher scores on a composite measure of suicidal ideation and behavior severity in a general university population (Johnson, Carver, & Joormann, 2013). To date, however, researchers have not examined either Negative or Positive Urgency in relation to suicidal thought or behavior within bipolar disorder.
Positive Urgency scores have been found to correlate with risk for bipolar disorder, as indexed by subsyndromal lifetime mania symptoms (Giovanelli, Hoerger, Johnson, & Gruber 2013; Johnson, Carver, Mule, & Joormann, 2013). In one study, Positive Urgency and Negative Urgency were both found to be more elevated among persons with bipolar I disorder in remission than were other forms of impulsivity (Muhtadie et al., 2013). These scales have also been found to predict lower quality of life and functioning among persons with bipolar disorder (Victor, Johnson, & Gotlib, 2011).
In the current study, we assessed how Positive and Negative Urgency relate to suicidal ideation and behavior among persons with bipolar disorder. In doing so, we also took into account well-established demographic and clinical correlates of suicide ideation and attempts. A recent meta-regression of 34 reports encompassing 50,004 participants with bipolar disorder identified a set of demographic and clinical risk variables consistently tied to suicide attempts, including female gender, younger age of onset, greater depressive severity, comorbid anxiety disorders, and comorbid substance or alcohol use disorder (Schaffer, Isometsa, Tondo, Moreno, Sinyor et al., 2015; Schaffer, Isometsa, Tondo, Moreno, Turecki et al., 2015). Other research has indicated that childhood abuse may intensify risks for suicide ideation and attempts among those diagnosed with bipolar disorder (Daruy-Filho, Brietzke, Lafer, & Grassi-Oliveira 2011). We hypothesized that impulsivity is a correlate of self-harm, suicide ideation, and suicide attempts; we also considered its role in combination with these variables.
METHOD
Data for these analyses were drawn from two previous studies (Edge, Lwi, & Johnson, 2014; Johnson, Carver, & Gotlib, 2012; Muhtadie & Johnson, 2015). Previous reports from one of the data sets described group differences in impulsivity levels (Muhtadie & Johnson, 2015) and the correlations of impulsivity with functional outcomes (Victor et al., 2011). Procedures for both studies were approved by the relevant university institutional review boards.
Participants
For both samples, persons were eligible to participate if they met criteria for bipolar I disorder or, for the control group, if they had no history of major depression or any bipolar spectrum disorder as assessed with the Structured Clinical Interview for DSM–IV (First, Spitzer, Gibbon, & Williams, 1995). Sample 1 included 58 individuals with remitted bipolar I disorder and 53 control participants. Sample 2 included 75 persons with remitted bipolar I disorder and 47 control participants. Here, we focus on the participants diagnosed with bipolar I disorder.
Both bipolar samples were recruited using online advertisements, flyers at local clinics and public transportation sites, and referrals through local providers and bipolar disorder support groups. To identify matched control participants, flyers were distributed in unemployment centers. In sample 2, to target common comorbid anxiety and substance-related disorders, additional internet and community advertisements specific to these disorders were made. All participants completed written informed consent procedures and were paid for their participation.
All participants were at least age 18 and fluent English speakers. Exclusion criteria included a diagnosis of alcohol or substance abuse or dependence in the past year, primary psychotic disorder during the lifetime, general medical diseases of the central nervous system (e.g., Alzheimer’s or Parkinson’s disease), vascular disease, degenerative disorder, severe head trauma, or developmental, cognitive, language, or learning disabilities that could interfere with the ability to complete informed consent or study measures. Exclusion criteria for sample 1 included age above 60 and, for sample 2, age above 65 years. Two participants in sample 1 were excluded for incorrectly responding to more than half of 10 “catch” items included in the battery (e.g., “please answer this question with ‘3’.”).
As has been reported previously (Johnson, Tharp, Peckham, Sanchez, & Carver, 2016; Muhtadie & Johnson, 2015; Ng & Johnson, 2013), persons with bipolar disorder did not differ from controls in years of age, gender, years of education, or current employment in either sample. In both samples, diagnoses of lifetime substance or alcohol use disorders were significantly elevated in the bipolar group as compared to the control group.
Measures
All participants completed interviews to assess diagnosis, medication status, symptom severity, and suicidality indices. Positive Urgency was assessed by self-report. Participants in sample 1 were interviewed concerning trauma exposure. Participants in sample 2 completed a fuller set of impulsivity measures, including self-rated Negative Urgency and the Barrett Impulsivity Scale.
Diagnostic Interview
The Structured Clinical Interview for DSM–IV (SCID) is a widely used and well-validated semi-structured diagnostic interview (First et al., 1995). The SCID was used to assess lifetime diagnoses of bipolar disorder, major depressive disorder, anxiety disorders, or alcohol or substance use disorder, as well as course parameters across the lifetime. In both samples, SCID interviews were conducted by clinical psychology graduate students and postdoctoral fellows who had completed extensive didactic and interactive training and had achieved interrater reliability in evaluating gold standard diagnostic interviews. Reliability meetings were held intermittently throughout both studies to protect against rater drift. Interrater agreement was strong in both studies for current and lifetime manic and depressive episodes, intraclass rs = .89–1.0 (Johnson et al., 2012; Muhtadie & Johnson, 2015).
For the seven participants with an onset after age 35, scores were winsorized (set to 35 to reduce skew). On average, participants diagnosed with bipolar disorder reported an age of disorder onset of 21.85 (SD = 8.09), a mean of 8.29 previous manic episodes (SD = 8.97), and 50% had been hospitalized for mania at least once. They also reported an average of 12.84 previous major depressive episodes (MDD; SD = 11.54), and 17.2% had been hospitalized for depression at least once. Because the number of lifetime MDD episodes was highly skewed, this variable was collapsed into never (19 persons), 1–3 episodes (25 persons), 4–6 episodes (19 persons), and 6 or more episodes (69 persons); depressive history was missing for one person.
Self-Harm, Suicide Ideation, and Suicidal Behavior
Participants were interviewed to assess whether they had experienced self-harm, suicide ideation, and suicide-directed behavior during their lifetime (see Table 1 for rates of endorsement). As expected, self-harm, suicide ideation, and suicide attempts were significantly higher for those in the bipolar group than for those in the control group across both samples, all ps < .001. Indeed, across both samples, rates of suicide ideation or action were too low to examine correlates of suicidality within the control participants. Thus, subsequent analyses of those variables are limited to the bipolar group.
TABLE 1.
Clinical and Demographic Characteristics of the Combined Bipolar Sample (N = 133, except where otherwise noted)
| Mean (SD) or Percent | |
|---|---|
| Age (in years) | 36.81 (11.67) |
| Female | 58.6% |
| Years education | 15.01 (1.92) |
| Employed | 44.3% |
| Anxiety disorder | 54.9% |
| Past substance use | 55.6% |
| Manic symptom level—BRMSb | 2.52 (2.74) |
| Manic symptom level—YMRSa | 1.72 (1.60) |
| Depressive symptom level (MHRSD) | 7.42 (8.06) |
| Childhood traumaa | 20.6% |
| Positive Urgency | 33.84 (9.55) |
| Negative Urgencyb | 3.65 (0.66) |
| BIS Attentionb | 11.49 (3.02) |
| BIS Motor Impulsivenessb | 16.48 (4.06) |
| BIS Nonplanningb | 24.90 (5.22) |
| History of self-harm | 40.7% |
| History of suicidal ideation | 82.7% |
| History of suicide attempts | 35.2% |
Note. BIS, Barrett Impulsiveness Scale; BRMS, Bech-Rafaelsen Mania Scale; MHRSD, Modified Hamilton Rating Scale for Depression; YMRS, Young Mania Rating Scale.
MHRSD data were not recorded for 12 in the bipolar group, and one person reported being unable to recall the number of episodes of depression.
Only for sample 1, n = 58 (except YMRS where n = 56).
Only for sample 2, n = 75 (except BRMS where n = 61).
Medication Coding
Current medication regimens and adherence within the bipolar group were assessed using a structured interview. Thirty-four of the persons diagnosed with bipolar disorder were taking lithium. Lithium dose was adjusted for non-adherence levels. Three high scores on lithium dose (e.g., 1800–2100 mg) were reset to the next highest score (1200 mg) to reduce leptokursis and skew. Those who were not taking a medication were coded as “0” for analyses, yielding a mean lithium dose (in mg) among the bipolar group of 225.30 (SD = 418.67). The presence of other mood-stabilizing medications was coded as yes/no. Across the two samples, 75 of the bipolar participants were taking some other form of mood-stabilizing medications, and many were taking multiple medications (39 taking atypical antipsychotics, 35 taking lamotrigine, 34 taking antidepressants, and 20 anticonvulsant medications).
Modified Hamilton Rating Scale for Depression
The Modified Hamilton Rating Scale for Depression (MHRSD) is a 17-item semistructured interview designed to assess severity of current depression (Miller, Bishop, Norman, & Maddever, 1985). Scores range from 0 to 52. The MHRSD correlates well with other measures of depression in unipolar and bipolar disorder (Gonzalez-Pinto, Ballesteros, Aldama, Perez de Heredia, Gutierrez, & Mosquera, 2003; Johnson et al., 2008). Interrater agreement was high (ICC = .99 for 4 randomly selected tapes in sample 1 and .93 for 14 randomly selected tapes in sample 2). Internal consistency for the current sample was adequate (α = .84 in sample 1 and .92 in sample 2). Training for the MHRSD mirrored procedures employed for the SCID interview. Depression remission has been defined as scores of 6 or lower on the MHRSD (Miller et al., 1985).
Young Mania Rating Scale
The Young Mania Rating Scale (YMRS; Young, Biggs, Ziegler, & Meyer, 1978) is an 11-item interview measure that was used to assess cognitive, affective, and behavioral symptoms of mania in sample 1. Scores range from 0 to 60, with scores of 6 or lower indicating remission. Scores are correlated with other mania rating scales, clinician ratings, and treatment (Young et al., 1978). Training for the YMRS followed the same procedures as the SCID interview. Interrater agreement was excellent for this sample (ICC = .99 for four randomly selected tapes).
Bech-Rafaelsen Mania Scale
The Bech-Rafaelsen Mania Scale (BRMS; Bech, Bolwig, Kramp, & Rafaelsen, 1979) was used to assess the severity of manic symptoms in sample 2. Each of the 11 items is scored on a 5-point rating scale, and items are summed to yield a total. The scale has been shown to be sensitive to changes in clinical status and has been widely used to assess treatment outcomes (Bech, 2002). Scores of 5 or below have been defined as remission, and scores of 15 or above indicate definite mania (Bech, 1988). We used a set of standardized probes and obtained high interrater reliability (ICC = .93 in a sample of 14 randomly selected audiotapes) and internal consistency (α = .94). The scale distinguishes between persons with and without current mania, and is highly correlated with other measures of current mania (Bech, 2002).
Positive Urgency Measure
The PUM (Cyders et al., 2007) was designed to capture the tendency to act impulsively in response to positive emotion (e.g., “Others would say I make bad choices when I am extremely happy about something”). The scale consists of 14 items that were rated on a 4-point scale ranging from 1 = agree strongly to 4 = disagree strongly. The PUM has factor-analytic support and good internal consistency (Cyders et al., 2007), and has been associated with risky behavior, gambling behavior, problematic drinking behavior (Cyders & Smith, 2007), and measures of mania risk and bipolar diagnosis (Johnson, Carver, Mulé, et al., 2013; Muhtadie & Johnson, 2015). The scale had good internal consistency here (αs = .97 in both samples).
Negative Urgency
The Negative Urgency Scale assesses the tendency to act impulsively when experiencing strong negative emotion (Whiteside & Lynam, 2001). Respondents were asked to indicate the extent to which they agree with each of 13 statements using a 4-point scale ranging from 1 = agree strongly to 4 = disagree strongly. Negative Urgency has strong factor-analytic support and has been linked to outcomes such as aggression, alcohol abuse, disordered eating, and bipolar disorder, and a particularly strong link with borderline personality disorder (Berg et al., 2015; Lynam & Miller, 2004; Lynam, Gaughan et al., 2011; Muhtadie & Johnson, 2015). Only participants in sample 2 completed the Negative Urgency Scale (α = .93).
Barratt Impulsiveness Scale-11
The Barratt Impulsiveness Scale (BIS) is a widely used and well-validated measure of impulsivity (Patton, Stanford, & Barratt, 1995). The scale is composed of three factor-analytically based subscales: Attentional Impulsiveness, Motor Impulsiveness, and Nonplanning Impulsiveness. Participants responded to each of the 30 items on a 4-point scale, ranging from 1 = rarely/never to 4 = almost always/always. The BIS was administered only in sample 2. Internal consistencies for sample 2 were αs = .77, .76, and .73, respectively.
Trauma History Screen
The Trauma History Screen was given in sample 1 to provide a brief screener for lifetime history of exposure to high magnitude stressors, including physical abuse, sexual abuse, attacked with a weapon, military events, parental abandonment, accidents, and natural disasters (Carlson et al., 2011). For each type of stressor endorsed, participants are asked to clarify whether the trauma was serious enough that they were worried that they or someone else would be killed. The scale has been found to have adequate test–retest stability and convergent validity with trauma and PTSD across community, homeless, and inpatient samples (Carlson et al., 2011). Here, we focus on traumatic events occurring during childhood, as those have been found to be predictive of suicidal ideation and attempts (BrodskyOquendo, Ellis, Haas, Malone, & Mann, 2001; Sarchiapone et al., 2006, 2009).
Procedure
Preliminary screening of potential participants in both samples was conducted via phone interviews. Participants who appeared to be potentially eligible were invited to individual appointments to complete written informed consent procedures and a SCID interview, as well as interviews concerning medication status, self-harm, and suicidal thoughts and behaviors. Because personality difficulties may be exacerbated during symptomatic periods (George, Miklowitz, Richards, Simoneau, & Taylor, 2003), participants with bipolar disorder were assessed on these traits after remission. To do so, participants diagnosed with bipolar I disorder were interviewed monthly by telephone until they achieved symptom remission, as defined by cutoffs that have been validated in previous research on the MHRSD and the YMRS or BRMS (Chengappa et al., 2003; Thompson et al., 2005). Telephone assessments have been shown to be reliable and valid for evaluating symptom severity (Potts, Daniels, Burnam, & Wells, 2000; Simon, Revicki, & VonKroff, 1993). Symptom severity scores within a remitted range were confirmed by a phone interview within 48 hours before the in-person sessions for those with bipolar disorder. Participants who met study criteria and symptom remission were scheduled for inperson sessions to complete the measures of impulsivity and other risk factors, along with other measures not discussed here.
RESULTS
Analyses were completed using SPSS, version 23 (Armonk, NY: IBM Corp., 2014). Preliminary analyses indicated that variables did not violate assumptions regarding skew or kurtosis.
Preliminary Analyses
To test whether study sample should be considered as a predictor in analyses, four regression models were conducted to assess whether study sample moderated the effects of bipolar diagnostic status on PUM, self-harm, suicide ideation, or suicide attempts. No interaction term was significant, all r2 changes < .07, all ps > .30, nor did mean levels of these four variables differ by sample, ts < 1.62, all ps > .10. Subsequent analyses collapsed across the two study samples.
The characteristics of the bipolar participants are displayed in Table 1. Symptom severity was within the remitted range within both groups. As has been published previously for sample 2, the bipolar group had significantly higher impulsivity scores on the Positive and Negative Urgency scales and the BIS-11 Nonplanning Impulsivity scales than the controls (Muhtadie et al., 2013). Sample 1 provides a replication of the diagnostic group effect on Positive Urgency, in that PUM scores were significantly elevated in the bipolar group, M = 33.84 (SD = 9.55) as compared to the control group, M = 19.34 (SD = 6.01), t(231) = −13.32, p < .001.
Preliminary analyses were conducted to examine whether lithium dosages or the presence of other mood-stabilizing medication were confounded with impulsivity scores. Neither medication variable was significantly related to PUM, rs < |.05|, or Negative Urgency, rs < |.23|. Because medication scores were not available across the life course (and self-harm, suicide ideation, and suicidal behavior scores were based on lifetime severity), medication was not considered further.
Intercorrelations of the predictor variables (gender, clinical, childhood trauma, and impulsivity) within the bipolar group are shown in Table 2. As shown there, number of MDD recurrences was significantly related to higher rates of substance/alcohol use diagnoses and anxiety disorder diagnoses. Substance use diagnoses were also related to higher rates of anxiety disorder diagnoses, as well as childhood trauma. The measures of impulsivity were modestly correlated, rs = .21–.48. Positive Urgency scores were related to more recurrences of MDD and higher rates of substance use. Negative Urgency scores were related to higher rates of substance/alcohol use diagnoses and anxiety disorders.
TABLE 2.
Correlations of Clinical, Trauma, Impulsivity, and Suicidality Variables (Bipolar Participants, N = 133 except where noted)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Number of MDD episodes | – | |||||||||||
| 2. Lifetime substance diagnoses | .24** | – | ||||||||||
| 3. Lifetime anxiety diagnoses | .29** | .28** | – | |||||||||
| 4. Gender | −.02 | −.01 | .16 | – | ||||||||
| 5. Positive Urgency | .21* | .22* | .14 | .07 | – | |||||||
| 6. Negative Urgencyb | .14 | .27* | .37** | .18 | .39** | – | ||||||
| 7. BIS Attentionb | .08 | .21 | .12 | .13 | .44*** | .44*** | – | |||||
| 8. BIS Motor Impulsivenessb | −.04 | .23 | .06 | −.09 | .20 | .29* | .42*** | – | ||||
| 9. BIS Nonplanningb | .07 | .12 | .05 | −.17 | .32** | .40*** | .45*** | .48*** | – | |||
| 10. Childhood traumaa | .21 | .34* | .15 | .20 | .22 | n/a | n/a | n/a | n/a | – | ||
| 11. Self-harm | .18* | .13 | .14 | .33*** | .20* | .18 | .13 | .22 | .15 | .27* | – | |
| 12. Suicide ideation | .23** | .31*** | .38*** | −.12 | .20* | .52*** | .26* | .24* | .37** | .12 | .24** | – |
| 13. Suicide attempt | .16 | .25** | .12 | .09 | .20* | .20 | .10 | .15 | .09 | .15 | .31*** | .29** |
Note. BIS, Barrett Impulsiveness Scale; MDD, major depressive disorder. One person reported being unable to recall the number of episodes of depression.
Only for sample 1, n = 58.
Only for sample 2, n = 75.
p < .05;
p < .01;
p < .001.
Correlates of Suicide Ideation, Suicide Attempts, and Self-Harm
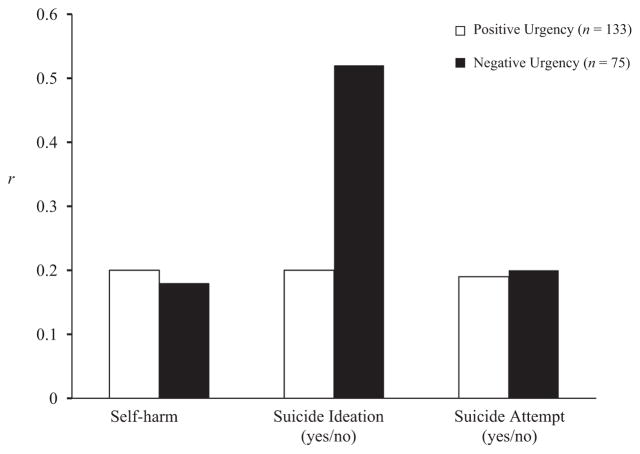
Also shown in Table 2, suicide ideation, attempts, and self-harm were only modestly associated with one another. Thus, each was treated as a separate outcome. Suicide ideation was associated with more MDD recurrences, substance/alcohol use diagnoses, anxiety diagnoses, higher Positive and Negative Urgency scores, and higher scores on all three subscales of the BIS-11. Suicide attempts were significantly correlated only with substance/alcohol use and Positive Urgency. Self-harm was significantly related to number of depressive episodes, being female, and higher Positive Urgency. The size of the associations of Positive and Negative Urgency with self-harm, suicide ideation, and suicide attempts is shown in Figure 1. As can be seen there, the contributions made by these measures were roughly equivalent for all outcomes except suicide ideation, where the effect of Negative Urgency was substantially greater than that of Positive Urgency (Fisher’s Z comparing the two correlations = −2.77, p < .01).
Figure 1.
Positive and Negative Urgency predicting self-harm, suicide ideation, and suicide attempts (Fisher’s Z = −2.77).
Three simultaneous-entry multiple regression models were used to test the unique contributions of the significant correlates of suicide ideation, attempts, and self-harm. As above, these analyses were within the bipolar disorder group. These regressions included only the variables that were measured across both samples (i.e., omitting trauma, BIS-11, and Negative Urgency scores). Before conducting analyses, statistical assumptions concerning outliers, heteroscedasticity, and colinearity were checked; no violations were noted.
The model for self-harm accounted for 15.9% of the variance, F(3, 121) = 7.43, p < .001. After accounting for gender (β = .32, t = 3.49, p < .001, semipartial r = .32) and number of MDD recurrences (β = .17, t = 1.93, p = .06, semipartial r = .16), PUM (β = .14, t = 1.62, p = .11, semipartial r = .14) did not relate significantly to self-harm.
For suicide ideation, the model accounted for 19.7% of the variance, F(4, 130) = 7.75, p < .001. After accounting for substance use disorders (β = .20, t = 2.34, p = .02, semipartial r = .19), anxiety disorders (β = .28, t = 3.33, p = .001, semipartial r = .27), number of MDD recurrences (β = .06, t = 0.73, p = .47, semipartial r = .06), and PUM (β = .10, t = 1.16, p = .25, semipartial r = .09) did not relate significantly to suicide ideation. When Negative Urgency was added to this model in a second block, Negative Urgency remained significantly related to suicide ideation (β = .41, t = 3.52, p = .001, semipartial r = .39), even though the N was reduced to 73, F(5, 73) = 6.98, p < .001, r2 total = .34.
For suicide attempts, the model accounted for 8.3% of the variance, F(2, 131) = 5.86, p = .004. After accounting for substance use diagnoses(β = .22, t = 2.54, p = .01, semipartial r = .21), PUM scores were not significantly related to suicide attempts(β = .15, t = 1.68, p = .10, semipartial r = .14).
DISCUSSION
In this study, most (82.7%) of the persons diagnosed with bipolar I disorder reported having experienced suicide ideation during their lifetime, nearly 41% reported having engaged in self-harm, and 35% reported engaging in at least one suicide attempt, echoing previous results. Our findings also replicate a previous report that Positive Urgency is elevated among those diagnosed with bipolar disorder (Muhtadie & Johnson, 2015). Taken together, current findings suggest the need to develop better models for understanding and addressing self-harm, suicide ideation, and suicide attempts within bipolar disorder and, more particularly, the need to understand the implications of emotion-triggered impulsivity.
Findings provide novel evidence that impulsive responses to emotions uniquely and significantly related to self-harm, suicide ideation, and suicide attempts among persons with bipolar disorder. As in previous research (Watkins & Meyer, 2013), the BIS-11 subscales did not significantly relate to self-harm or suicidal behavior among persons with bipolar disorder. The differential associations of these impulsivity scales suggest the advantage of taking a more nuanced approach to impulsivity in bipolar suicidality. The profile obtained here is similar to that observed in a meta-analysis of general community and student samples (rather than persons with bipolar disorder), in which Negative Urgency is more robustly tied to severity of suicide ideation than are other forms of impulsivity (Berg et al., 2015). Although fewer individuals completed the Negative Urgency Scale than the other scales, it is interesting to note that effect sizes were quite comparable for the effects of Negative and Positive Urgency on self-harm and suicidal action; this suggests that a more general tendency to respond to emotion states of either valence with impulsivity may guide these behavioral patterns. In contrast, the effect size for Negative Urgency was more than double the effect size for Positive Urgency or BIS-11 subscales on suicide ideation, and Negative Urgency contributed significant variance to suicide ideation after accounting for clinical variables, suggesting that impulsive responses to negative emotion may have particular importance for understanding the development of thoughts about suicide.
In addition to emotion-triggered impulsivity, clinical variables were important correlates of self-harm and suicidal thought and behavior. The severity of depression, comorbid anxiety, and comorbid substance problems were related to suicide variables. Lifetime substance use disorders were related to a history of suicide attempt. The number of depression recurrences was tied to ideation and self-harm history, and comorbid lifetime anxiety disorders related to ideation history. These findings largely replicate the previous literature (Schaffer, Isometsa, Tondo, Moreno, Sinyor et al., 2015; Schaffer, Isometsa, Tondo, Moreno, Turecki et al., 2015).
Findings regarding whether impulsive responses to emotion could explain suicidality above and beyond the role of clinical variables were mixed. It should be noted that depression and substance covariates themselves were related to Positive Urgency, consistent with previous research (Cyders & Smith, 2008). We did not find that impulsive responses to positive emotion predicted additional variance in suicidality after accounting for comorbidity. This is in parallel with previous work on self-harm (Rawlings et al., 2015). We did find that Negative Urgency contributed significant variance to suicide ideation after controlling for clinical variables, which is consistent with previous work indicating that the effects of Negative Urgency on suicide ideation and attempts withstood control for depression (Anestis et al., 2012; Anestis, Soberay et al., 2014; Anestis, Tull et al., 2014), for depression and alcohol use (Dvorak et al., 2013), and for borderline personality disorder diagnoses (Lynam, Gaughan et al., 2011; Lynam, Miller et al., 2011). Across our own and previous studies, though, researchers have focused on statistical control over conceptually related variables, an approach that has been criticized (Miller & Chapman, 2001); in considering whether urgency matters above and beyond variables like depression, a better approach would be to examine the predictive power of emotion-related impulsivity within a depressed sample.
Before considering implications, it is worth noting several limitations. First, and most obvious, the cross-sectional design precludes making any statements about causality. Those who have made suicide attempts, for example, may be reflecting on that behavior when asked to complete items evaluating their ability to control their responses to emotion. Second, other aspects of suicidal action and risk may be important to measure. In future studies, it would be desirable to assess the severity and violence of suicide attempts (Witte et al., 2008), as well as the planfulness of attempts (Anestis, Soberay et al., 2014; Anestis, Tull et al., 2014). Third, we did not consider the full range of variables relevant to self-harm, suicide thoughts, or suicide attempts. Recent meta-analyses suggest a major role for borderline personality traits and family history of suicidal behavior in bipolar disorder (Schaffer, Isometsa, Tondo, Moreno, Sinyor et al., 2015; Schaffer, Isometsa, Tondo, Moreno, Turecki et al., 2015). Future research should integrate these other risk factors for suicidal behavior in models of emotion-triggered impulsivity and bipolar disorder.
In future work, we also recommend inclusion of behavioral measures of impulsivity. It is important to note that relatively small correlations have been observed between self-report and performance-based measures of impulsivity (Sharma et al., 2014). There is some evidence that at least one performance-based measure of impulsivity, the Immediate Memory Task, is correlated with the severity of suicide attempts (Swann et al., 2005). Another issue concerns pathways. Negative Urgency has been found to be related to more robust links of the well-established transdiagnostic risk factors of lack of belongingness and perceived burden with suicidality in a community sample (Anestis & Joiner, 2011; Van Orden, Lynam, Hollar, & Joiner, 2006). It has been argued that one reason Negative Urgency relates to suicidal behavior may be indirect, in that persons who are impulsive may thereby have greater exposure to painful experiences, which then increases their acquired capacity for suicidal behavior (Anestis, Soberay et al., 2014; Anestis, Tull et al., 2014). Three studies provide correlational evidence in support of this idea in the general population (Anestis, Soberay et al., 2014; Anestis, Tull et al., 2014; Bender, Anestis, Anestis, Gordon, & Joiner, 2012; Bender, Gordon, Bresin, & Joiner, 2011).
Notwithstanding limitations, current findings extend a growing body of research to suggest that impulsivity in the context of emotion states may be highly relevant to understanding bipolar disorder. Across two samples (Muhtadie et al., 2013), people with remitted bipolar disorder describe experiencing difficulties with impulsive responses to emotion. Joining with previous findings that Positive Urgency is related to aggression, poor functioning, and low quality of life within bipolar disorder (Johnson & Carver, 2016; Muhtadie et al., 2013; Victor et al., 2011), our findings provide another example of a key outcome tied to emotion-triggered impulsivity. It is of particular interest that significant effects emerged for a measure of impulsive responses during positively valenced states.
Self-harm, suicide ideation, and suicide attempts are important issues for those with bipolar disorder and their families, with rates of suicide attempts and death that far exceed the general population. Current findings are encouraging, in that a brief self-report measure might be useful for understanding self-harm, suicidal thoughts, and suicidal behaviors. It is hoped that future research can use a longitudinal design with a larger sample to build a model integrating the effects of emotion-triggered impulsivity with other risk factors for suicidality in the prediction of self-harm, suicidal ideation, and suicidal action in bipolar disorder. If the effects of emotion-related impulsivity on self-harm, suicide ideation, and suicide behaviors are replicated, this would suggest the need to consider treatment interventions that have been shown to directly address impulsive behavior, such as the formation and use of implementation intentions (Webb & Sheeran, 2006).
Contributor Information
Sheri L. Johnson, Department of Psychology, University of California, Berkeley, Berkeley, CA, USA.
Charles S. Carver, Department of Psychology, University of Miami, Coral Gables, FL, USA.
Jordan A. Tharp, Department of Psychology, University of California, Berkeley, Berkeley, CA, USA.
References
- Alloy LB, Bender RE, Wagner CA, White House Wagner WG, Abramson LY, Hogan ME, et al. Bipolar spectrum-substance use co-occurrence: Behavioral approach system (BAS) sensitivity and impulsiveness as shared personality vulnerabilities. Journal of Personality and Social Psychology. 2009;97:549–565. doi: 10.1037/a0016061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Fink EL, Bender TW, Selby EA, Smith AR, Witte TK, et al. Re-considering the association between negative urgency and suicidality. Personality and Mental Health. 2012;6:138–142. [Google Scholar]
- Anestis MD, Joiner TE. Examining the role of emotion in suicidality: Negative urgency as an amplifier of the relationship between components of the interpersonal-psychological theory of suicidal behavior and lifetime number of suicide attempts. Journal of Affective Disorders. 2011;129:261–269. doi: 10.1016/j.jad.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Soberay KA, Gutierrez PM, Hernandez TD, Joiner TE. Reconsidering the link between impulsivity and suicidal behavior. Personality and Social Psychology Review. 2014;4:366–386. doi: 10.1177/1088868314535988. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Tull MT, Lavender JM, Gratz KL. The mediating role of non-suicidal self-injury in the relationship between impulsivity and suicidal behavior among inpatients receiving treatment for substance use disorders. Psychiatry Research. 2014;218:166–173. doi: 10.1016/j.psychres.2014.03.031. [DOI] [PubMed] [Google Scholar]
- Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychological Reports. 1965;16:547–554. doi: 10.2466/pr0.1965.16.2.547. [DOI] [PubMed] [Google Scholar]
- Bech P. Rating scales for mood disorders: Applicability, consistency and construct validity. Acta Psychiatrica Scandinavica. Supplementum. 1988;345:45–55. doi: 10.1111/j.1600-0447.1988.tb08567.x. [DOI] [PubMed] [Google Scholar]
- Bech P. The Bech-Rafaelsen Mania Scale in clinical trials of therapies for bipolar disorder: A 20-year review of its use as an outcome measure. CNS Drugs. 2002;16:47–63. doi: 10.2165/00023210-200216010-00004. [DOI] [PubMed] [Google Scholar]
- Bech P, Bolwig TG, Kramp P, Rafaelsen OJ. The Bech-Rafaelsen Mania Scale and the Hamilton Depression Scale. Acta Psychiatrica Scandinavica. 1979;59:420–430. doi: 10.1111/j.1600-0447.1979.tb04484.x. [DOI] [PubMed] [Google Scholar]
- Bender TW, Anestis MD, Anestis JC, Gordon KH, Joiner TE. Affective and behavioral paths toward the acquired capacity for suicide. Journal of Social and Clinical Psychology. 2012;31:81–100. [Google Scholar]
- Bender TW, Gordon KH, Bresin K, Joiner TE. Impulsivity and suicidality: The mediating role of painful and provocative experiences. Journal of Affective Disorders. 2011;129:301–307. doi: 10.1016/j.jad.2010.07.023. [DOI] [PubMed] [Google Scholar]
- Berg JM, Latzman RD, Bliwise NG, Lilienfeld S. Parsing the heterogeneity of impulsivity: A meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychological Assessment. 2015;27:1129–46. doi: 10.1037/pas0000111. [DOI] [PubMed] [Google Scholar]
- Black EB, Mildred H. A cross-sectional examination of non-suicidal self-injury, disordered eating, impulsivity, and compulsivity in a sample of adult women. Eating Behaviors. 2014;15:578–581. doi: 10.1016/j.eatbeh.2014.08.011. [DOI] [PubMed] [Google Scholar]
- Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: A systematic review. Acta Psychiatrica Scandinavica. 2006;113:180–206. doi: 10.1111/j.1600-0447.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- Brodsky BS, Oquendo M, Ellis SP, Haas GL, Malone KM, Mann JJ. The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. American Journal of Psychiatry. 2001;158:1871–1877. doi: 10.1176/appi.ajp.158.11.1871. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, et al. Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment. 2011;23:463–477. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, Joormann J. Serotonergic function, two-mode models of self-regulation, and vulnerability to depression: What depression has in common with impulsive aggression. Psychological Bulletin. 2008;134:912–943. doi: 10.1037/a0013740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chengappa KNR, Kupfer DJ, Frank E, Houck PR, Grochocinski VJ, Cluss PA, et al. Relationship of birth cohort and early age at onset of illness in a bipolar disorder case registry. The American Journal of Psychiatry. 2003;160:1636–1642. doi: 10.1176/appi.ajp.160.9.1636. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Mood-based rash action and its components: Positive and negative urgency and their relations with other impulsivity-like constructs. Personality and Individual Differences. 2007;43:839–850. [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin. 2008;134:807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Daruy-Filho L, Brietzke E, Lafer B, Grassi-Oliveira R. Childhood maltreatment and clinical outcomes of bipolar disorder. Acta Psychiatrica Scandinavica. 2011;124:427–434. doi: 10.1111/j.1600-0447.2011.01756.x. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Lamis DA, Malone PS. Alcohol use, depressive symptoms, and impulsivity as risk factors for suicide proneness among college students. Journal of Affective Disorders. 2013;149:326–334. doi: 10.1016/j.jad.2013.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edge MD, Lwi S, Johnson SL. An assessment of emotional reactivity to frustration of goal pursuit in euthymic bipolar I disorder. Clinical Psychological Science. 2014 Epub ahead of print. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV disorders patient edition (SCID version 2.0) New York: Biomedics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Gallardo-Pujol D, Andres-Pueyo A, Maydeu-Olivares A. MAOA genotype, social exclusion and aggression: An experimental test of a gene-environment interaction. Genes, Brain, and Behavior. 2013;12:140–145. doi: 10.1111/j.1601-183X.2012.00868.x. [DOI] [PubMed] [Google Scholar]
- George EL, Miklowitz DJ, Richards JA, Simoneau TL, Taylor DO. The comorbidity of bipolar disorder and axis II personality disorders: Prevalence and clinical correlates. Bipolar Disorders. 2003;5:115–122. doi: 10.1034/j.1399-5618.2003.00028.x. [DOI] [PubMed] [Google Scholar]
- Giovanelli A, Hoerger M, Johnson SL, Gruber J. Impulsive responses to positive mood and reward are related to mania risk. Cognition & Emotion. 2013;27:1091–1104. doi: 10.1080/02699931.2013.772048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. A multimethod analysis of impulsivity in nonsuicidal self-injury. Personality Disorders. 2010;1:67–75. doi: 10.1037/a0017427. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Pinto A, Ballesteros J, Aldama A, Perez de Heredia JL, Gutierrez M, Mosquera F. Principal components of mania. Journal of Affective Disorders. 2003;76:95–102. doi: 10.1016/s0165-0327(02)00070-8. [DOI] [PubMed] [Google Scholar]
- ten Have M, Vollebergh W, Nolen WA. Bipolar disorder in the general population in The Netherlands (prevalence, consequences and care utilisation): Results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Journal of Affective Disorders. 2002;68:203–213. doi: 10.1016/s0165-0327(00)00310-4. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Bohnert AS, Ignacio RV, McCarthy JF, Valenstein MM, Kim HM, et al. Psychiatric diagnoses and risk of suicide in veterans. Archives of General Psychiatry. 2010;67:1152–1158. doi: 10.1001/archgenpsychiatry.2010.129. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Carver CS. Emotion-relevant impulsivity predicts sustained anger and aggression after remission in bipolar I disorder. Journal of Affective Disorders. 2016;189:169–175. doi: 10.1016/j.jad.2015.07.050. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Carver CS, Gotlib IH. Elevated ambitions for fame among persons diagnosed with bipolar I disorder. Journal of Abnormal Psychology. 2012;121:602–609. doi: 10.1037/a0026370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Carver CS, Joormann J. Impulsive responses to emotion as a transdiagnostic vulnerability to internalizing and externalizing symptoms. Journal of Affective Disorders. 2013;150:872–878. doi: 10.1016/j.jad.2013.05.004. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Carver CS, Mule S, Joormann J. Impulsivity and risk for mania: Towards greater specificity. Psychology and Psychotherapy. 2013;86:401–412. doi: 10.1111/j.2044-8341.2012.02078.x. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Cuellar AK, Ruggero C, Winett-Perlman C, Goodnick P, White R, Miller I. Life events as predictors of mania and depression in bipolar I disorder. Journal of Abnormal Psychology. 2008;117:268–277. doi: 10.1037/0021-843X.117.2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Tharp JA, Peckham AD, Sanchez AH, Carver CS. Emotion in bipolar I disorder: Implications for functional and symptom outcomes. Journal of Abnormal Psychology. 2016;125:40–52. doi: 10.1037/abn0000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jollant F, Guillaume S, Jaussent I, Bellivier F, Leboyer M, Castelnau D, et al. Psychiatric diagnoses and personality traits associated with disadvantageous decision-making. European Psychiatry. 2007;22:455–461. doi: 10.1016/j.eurpsy.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide and Life-Threatening Behavior. 2010;40:612–619. doi: 10.1521/suli.2010.40.6.612. [DOI] [PubMed] [Google Scholar]
- Kwapil TR, Miller MB, Zinser MC, Chapman LJ, Chapman J, Eckblad M. A longitudinal study of high scorers on the hypomanic personality scale. Journal of Abnormal Psychology. 2000;109:222–226. [PubMed] [Google Scholar]
- Lynam DR, Gaughan ET, Miller JD, Miller DJ, Mullins-Sweatt S, Widiger TA. Assessing the basic traits associated with psychopathy: Development and validation of the Elemental Psychopathy Assessment. Psychological Assessment. 2011;23:108–124. doi: 10.1037/a0021146. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Miller JD. Personality pathways to impulsive behavior and their relations to deviance: Results from three samples. Journal of Quantitative Criminology. 2004;20:319–341. [Google Scholar]
- Lynam DR, Miller JD, Miller DJ, Bornovalova MA, Lejeuz CW. Testing the relations between impulsivity-related traits, suicidality, and nonsuicidal self-injury: A test of the incremental validity of the UPPS model. Personality Disorders. 2011;2:151–160. doi: 10.1037/a0019978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malloy-Diniz LF, Neves FS, Abrantes SS, Fuentes D, Correa H. Suicide behavior and neuropsychological assessment of type I bipolar patients. Journal of Affective Disorders. 2009;112:231–236. doi: 10.1016/j.jad.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Malloy-Diniz LF, Neves FS, de Moraes PH, De Marco LA, Romano-Silva MA, Krebs MO, Correa H. The 5-HTTLPR polymorphism, impulsivity and suicide behavior in euthymic bipolar patients. Journal of Affective Disorders. 2011;133:221–226. doi: 10.1016/j.jad.2011.03.051. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Jin R, He JP, Kessler R, Lee S, Sampson N, et al. Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey Initiative. Archives of General Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GA, Chapman JP. Misunderstanding analysis of covariance. Journal of Abnormal Psychology. 2001;110:40–48. doi: 10.1037//0021-843x.110.1.40. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop S, Norman WH, Maddever H. The Modified Hamilton Rating Scale for Depression: Reliability and validity. Psychiatry Research. 1985;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Muhtadie L, Johnson SL. Threat sensitivity in bipolar disorder. Journal of Abnormal Psychology. 2015;124:93–101. doi: 10.1037/a0038065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhtadie L, Johnson SL, Carver CS, Gotlib IH, Ketter TA. A profile approach to impulsivity in bipolar disorder: The key role of strong emotions. Acta Psychiatrica Scandinavica. 2013;129:100–108. doi: 10.1111/acps.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullins-Sweatt SN, Lengel GJ, Grant DM. Non-suicidal self-injury: The contribution of general personality functioning. Personality and Mental Health. 2009;7:56–68. doi: 10.1002/pmh.1211. [DOI] [PubMed] [Google Scholar]
- Ng TH, Johnson SL. Rejection sensitivity is associated with quality of life, psychosocial outcome, and the course of depression in euthymic patients with bipolar I disorder. Cognitive Therapy and Research. 2013;37:1169–1178. doi: 10.1007/s10608-013-9552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, Sterba SK. Revealing the form and functions of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology. 2009;118:816–827. doi: 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Archives of General Psychiatry. 2011;68:1058–1064. doi: 10.1001/archgenpsychiatry.2011.113. [DOI] [PubMed] [Google Scholar]
- Parmentier C, Etain B, Yon L, Misson H, Mathieu F, Lajnef M, et al. Clinical and dimensional characteristics of euthymic bipolar patients with or without suicidal behavior. European Psychiatry. 2012;27:570–576. doi: 10.1016/j.eurpsy.2011.05.005. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Peterson CM, Davis-Becker K, Fischer S. Interactive role of depression, distress tolerance and negative urgency on nonsuicidal self-injury. Personality and Mental Health. 2014;8:151–160. doi: 10.1002/pmh.1256. [DOI] [PubMed] [Google Scholar]
- Peterson CM, Fischer S. A prospective study of the influence of the UPPS model of impulsivity on the co-occurrence of bulimic symptoms and non-suicidal self-injury. Eating Behaviors. 2012;13:335–341. doi: 10.1016/j.eatbeh.2012.05.007. [DOI] [PubMed] [Google Scholar]
- Pompili M, Gonda X, Serafini G, Innamorati M, Sher L, Amore M, et al. Epidemiology of suicide in bipolar disorders: A systematic review of the literature. Bipolar Disorders. 2013;15:457–490. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- Potts MK, Daniels M, Burnam MA, Wells KB. A structured interview version of the Hamilton Depression Rating Scale: Evidence of reliability and versatility of administration. Journal of Psychiatric Research. 2000;24:335–350. doi: 10.1016/0022-3956(90)90005-b. [DOI] [PubMed] [Google Scholar]
- Rawlings J, Shevlin M, Corcoran R, Morriss R, Taylor PJ. Out of the blue: Untangling the association between impulsivity and planning in self-harm. Journal of Affective Disorders. 2015;184:29–35. doi: 10.1016/j.jad.2015.05.042. [DOI] [PubMed] [Google Scholar]
- Sarchiapone M, Carli V, Camardese G, Cuomo C, Di Giuda D, Calcagni ML, et al. Dopamine transporter binding in depressed patients with anhedonia. Psychiatry Research. 2006;147:243–248. doi: 10.1016/j.pscychresns.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Sarchiapone M, Jaussent I, Roy A, Carli V, Guillaume S, Jollant F, et al. Childhood trauma as a correlative factor of suicidal behavior via aggression traits: Similar results in an Italian and in a French sample. European Psychiatry. 2009;24:57–62. doi: 10.1016/j.eurpsy.2008.07.005. [DOI] [PubMed] [Google Scholar]
- Schaffer A, Isometsa ET, Tondo L, Moreno DH, Sinyor M, et al. Epidemiology, neurobiology and pharmacological interventions related to suicide deaths and suicide attempts in bipolar disorder: Part I of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. The Australian and New Zealand Journal of Psychiatry. 2015;49:785–802. doi: 10.1177/0004867415594427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaffer A, Isometsa ET, Tondo L, Moreno DH, Turecki G, et al. International Society for Bipolar Disorders Task Force on Suicide: Meta-analyses and meta-regression of correlates of suicide attempts and suicide deaths in bipolar disorder. Bipolar Disorders. 2015;17:1–16. doi: 10.1111/bdi.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma L, Markon KE, Clark LA. Toward a theory of distinct types of “impulsive” behaviors: A meta-analysis of self-report and behavioral measures. Psychological Bulletin. 2014;140:374–408. doi: 10.1037/a0034418. [DOI] [PubMed] [Google Scholar]
- Simon GE, Revicki D, VonKroff M. Telephone assessment of depression severity. Journal of Psychiatric Research. 1993;27:247–252. doi: 10.1016/0022-3956(93)90035-z. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, Fleck DE, DelBello MP, Adler CM, Shear PK, Kotwal R, Arndt S. Impulsivity across the course of bipolar disorder. Bipolar Disorders. 2010;12:285–297. doi: 10.1111/j.1399-5618.2010.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann AC. Long-term treatment in bipolar disorder. Journal of Clinical Psychiatry. 2005;66(Suppl 1):7–12. [PubMed] [Google Scholar]
- Swann AC, Dougherty DM, Pazzaglia PJ, Pham M, Steinberg JL, Moeller FG. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. American Journal of Psychiatry. 2005;162:1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- Swann AC, Pazzaglia P, Nicholls A, Dougherty DM, Moeller FG. Impulsivity and phase of illness in bipolar disorder. Journal of Affective Disorders. 2003;73:105–111. doi: 10.1016/s0165-0327(02)00328-2. [DOI] [PubMed] [Google Scholar]
- Thompson JM, Gallagher P, Hughes JH, Watson S, Gray JM, Ferrier IN, Young AH. Neurocognitive impairment in euthymic patients with bipolar affective disorder. British Journal of Psychiatry. 2005;186:32–40. doi: 10.1192/bjp.186.1.32. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Lynam ME, Hollar D, Joiner TE. Perceived burdensomeness as an indicator of suicidal symptoms. Cognitive Therapy and Research. 2006;30:457–467. [Google Scholar]
- Victor SE, Johnson SL, Gotlib IH. Quality of life and impulsivity in bipolar disorder. Bipolar Disorders. 2011;13:303–309. doi: 10.1111/j.1399-5618.2011.00919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins HB, Meyer TD. Is there an empirical link between impulsivity and suicidality in bipolar disorders? A review of the current literature and the potential psychological implications of the relationship. Bipolar Disorders. 2013;15:542–558. doi: 10.1111/bdi.12090. [DOI] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin. 2006;132:249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Whiteside SP, Lynam DR. Understanding the role of impulsivity and externalizing psychopathology in alcohol abuse: Application of the UPPS impulsive behavior scale. Experimental and Clinical Psychopharmacology. 2003;10:210–217. doi: 10.1037/1064-1297.11.3.210. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behavior scale: A four-factor model of impulsivity. European Journal of Personality. 2005;19:559–574. [Google Scholar]
- Witte TK, Merrill KA, Stellrecht NE, Bernert RA, Hollar DL, Schatschneider C, Joiner TE., Jr “Impulsive” youth suicide attempters are not necessarily all that impulsive. Journal of Affective Disorders. 2008;107:107–116. doi: 10.1016/j.jad.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Skodol AE, Grilo CM, Edelen MO, et al. Personality traits as prospective predictors of suicide attempts. Acta Psychiatrica Scandinavica. 2009;120:222–229. doi: 10.1111/j.1600-0447.2009.01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]