Abstract
Background
Urinary incontinence (UI) is highly prevalent in the aging population. UI is one of the most common geriatric syndromes and affects overall health, quality of life, and economical burden in patients. The aims of this study were to investigate the characteristics of patients with UI and to assess its association with other geriatric health problems.
Methods
We used data from the Korean Longitudinal Study of Ageing obtained in 2006. Among the 10,254 individuals aged 45 years and older, we analyzed data from 2,418 women aged 65 years and older. Data were obtained using questionnaires for UI, comorbidities, and lifestyle factors.
Results
Among the 2,418 women aged 65 years and older, 506 (20.9%) had UI. Cerebrovascular disease (odds ratio [OR], 2.02; 95% confidence interval [CI], 1.26 to 3.23), arthritis (OR, 1.44; 95% CI, 1.18 to 1.77), and fear of falling (OR, 1.62; 95% CI, 1.18 to 2.22) were significantly associated with UI, while chronic lung disease, psychiatric disease, difficulty in daily living due to visual and hearing problems, and experiencing a fall in the last 2 years were not associated with UI.
Conclusion
Cerebrovascular disease, arthritis, and especially fear of falls were significantly associated with UI in elderly Korean women.
Keywords: Accidental Falls, Geriatrics, Urinary Incontinence, Aged
INTRODUCTION
Urinary incontinence (UI) is a complaint of any involuntary leakage of urine. The International Continence Society has defined UI as “the complaint of any involuntary loss of urine that is a hygienic or social problem.”1,2) The most common type of UI in women is stress UI (SUI), which occurs when abdominal pressure rises (49%). This is followed by urge UI (UUI) (21%), which is caused by involuntary detrusor muscle contractions during the filling phase, which may be spontaneous or triggered. There is also mixed UI (29%), which consists of a combination of the symptoms of SUI and UUI.3,4) UI causes psychological and physical problems, which in turn affect life quality and economic burden in patients.5,6,7)
UI is prevalent in women, especially in the elderly population. The prevalence of UI is reported to be between 20% and 30% in women and increases with age.7) It is reported that approximately 50% of institutionalized elderly persons and 15% of community-dwelling elderly individuals have UI.1) Oh et al.8) report that the prevalence of UI is approximately 41.2% among Korean women aged 30 to 79 years9) and Shin et al.10) report that approximately 48% of individuals in a sanatorium in Busan have UI.9)
UI is an important component of geriatric syndromes.1,11) Geriatric syndromes are defined as “multifactorial health states that arise when accumulated effects of disorders in multiple systems make an older person vulnerable to situational challenges”, and consist of falls, delirium, malnutrition, memory impairment, and UI.12,13) Geriatric syndromes are also prevalent in older adults and affect quality of life, leading to disability.13,14) Among the geriatric syndromes, voiding symptoms, such as urgency, frequency, and UI, are very common.6) Geriatric syndromes such as UI, falls, and delirium share risk factors such as age, functional impairment, and cognitive impairment. These shared risk factors may support the presence of common pathophysiology amenable to the same prevention strategies.13) Recently, several studies have investigated the prevalence and pathophysiology of UI and its association with other geriatric syndromes. Kwon et al.6) have reported on the prevalence, risk factors, and quality of life of Korean women with UI. In addition, Silay et al.1) have reported on the prevalence of occult UI and its association with other geriatric conditions.
The purposes of this study were to investigate the prevalence of UI in older women in Korea and to evaluate its association with other geriatric health problems.
METHODS
1. Study Subjects
Our study was based on data from the Korean Longitudinal Study of Ageing (KLoSA), which was designed to investigate labor market participation, health status, social security system efficacy, and the wealth and income levels of individuals. Baseline surveys were performed every two years beginning in 2006. The study included 10,254 individuals aged 45 years and older who resided within the country, but excluded those living on Jeju Island. The survey was conducted using the computer-assisted personal interviewing method. We analyzed 2,418 women aged 65 years and older. The study protocol of KLoSA was reviewed and approved by the institutional review board of the Samsung Medical Center (SMC 2016-02-114).
2. Definition of Urinary Incontinence
UI was defined as having experience of urine leakage in the past 12 months. To assess experience of urine leakage, participants were asked to answer “yes” or “no” to a question concerning UI.
3. Covariates
The subjects were divided into three age groups: 65–75, 75–85, and 85 years or older. Body mass index (BMI) was calculated using self-reported height and weight. Education level was categorized as “uneducated” or “higher than elementary school”. Marital status was categorized as “married” or “single” (separated, divorced, bereaved, and unmarried). Smoking was assessed based on responses to the question: “Do you currently smoke?” Alcohol intake was assessed using the question: “Do you occasionally or often drink alcohol?” Social activity was assessed by asking whether the subject has contact with people close to them. Chronic diseases, such as hypertension, diabetes mellitus, chronic lung disease (bronchitis or pulmonary emphysema), cerebrovascular disease (stroke, cerebral hemorrhage, or cerebral infarction), arthritis, and psychiatric disease (anxiety, insomnia, excessive stress, or difficulties in interpersonal relationships), were assessed by asking the participants whether they were diagnosed with any of the conditions by a doctor. We also asked the participants whether hearing or visual problems caused difficulties in their daily living. Depression was assessed using the Center for Epidemiologic Studies Short Depression Scale-Revised 10. Falls were assessed by asking the questions: “Have you experienced falls in the past 2 years?” and “Do you have a fear of falls?”
4. Statistical Analysis
The numbers and percentages of clinical characteristics were compared between the group with UI and the group without UI. Continuous data were described using means and standard deviations, and Student t-tests were used to compare the differences. Categorical data were reported as proportions, and a chi-square test or a Fisher's exact test was used for analysis. Univariate and multivariate logistic regressions were performed for the analyses of the associations. Finally, associations between UI and other geriatric syndromes were analyzed after adjusting for age and education. Statistical analysis was performed using IBM SPSS for Windows ver. 21.0 (IBM Corp., Armonk, NY, USA). Values of P<0.05 were considered statistically significant.
RESULTS
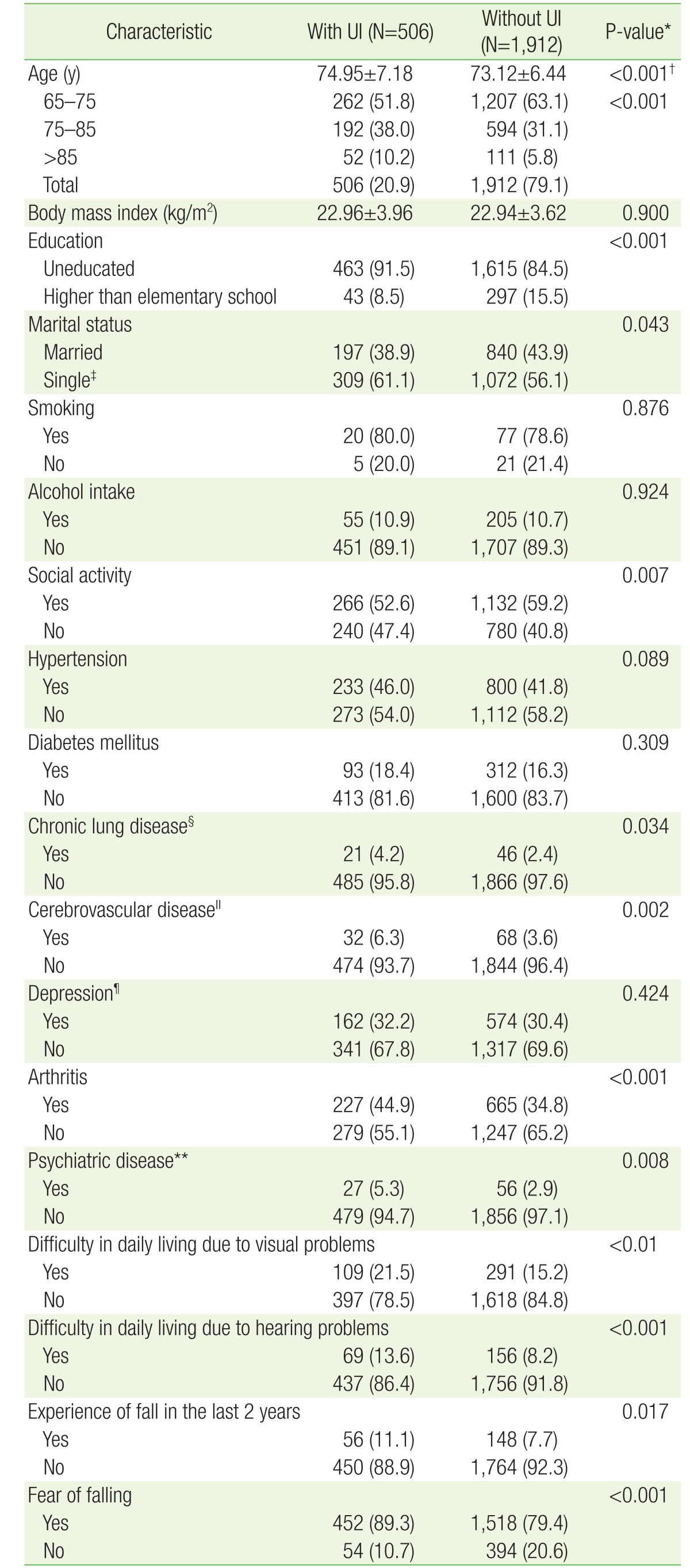
Table 1 shows the baseline characteristics of the participants in this study. Among the 2,418 participants, 506 (20.9%) had UI. The mean age of the participants with UI was 74.95±7.18 years and that of participants without UI was 73.12±6.44 years (P<0.001). Compared to the group without UI, subjects with UI had significantly higher proportions of low education level, single marital state, and absence of social activity. Participants with UI were more likely to have chronic lung disease (P=0.034), cerebrovascular disease (P=0.002), arthritis (P<0.001), psychiatric disease (P=0.008), and difficulty in daily living due to visual (P<0.01) and hearing problems (P<0.001) compared to subjects without UI. There was a significant difference in the proportion of subjects experiencing falls in the last 2 years between the two groups. Fifty-six (11.1%) of the subjects in the UI group and 148 (7.7%) of the subjects without UI (P=0.017) had experienced falls in the past two years. In addition, there was a significant difference in fear of falling between the two groups. Four-hundred and fifty-two (89.3%) of subjects in the UI group and 1,518 (79.4%) of those without UI (P<0.001) had a fear of falling. However, BMI, smoking, alcohol intake, hypertension, diabetes mellitus, and depression were not significantly different between the two groups.
Table 1. Baseline characteristics of study participants with or without urinary incontinence.
Values are presented as mean±standard deviation or number (%).
UI, urinary incontinence.
*Assessed using a chi-square test. †Assessed using a t-test. ‡Separated, divorced, bereaved, and unmarried. §Bronchitis or pulmonary emphysema. ∥Stroke, cerebral hemorrhage, or cerebral infarction. ¶Using the Center for Epidemiologic Studies Short Depression Scale-Revised 10. **Includes anxiety, insomnia, excessive stress, or difficulties in interpersonal relationships diagnosed by doctors.
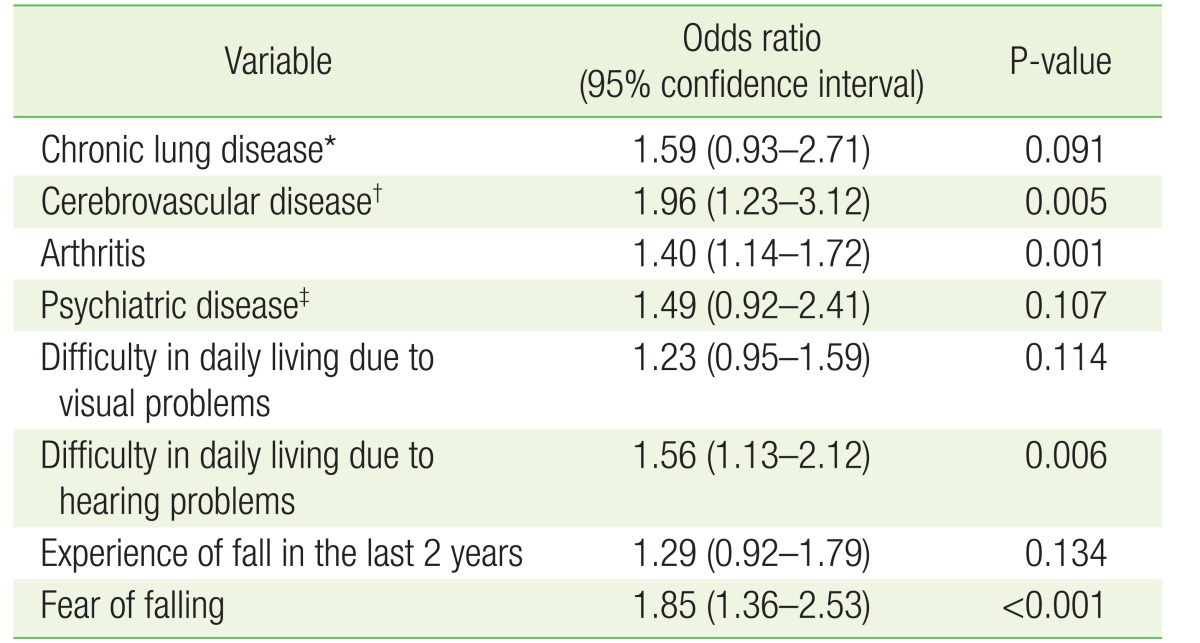
Table 2 shows the univariate logistic regression analysis of the association factors for UI. Cerebrovascular disease (odds ratio [OR], 1.96; 95% confidence interval [CI], 1.23 to 3.12), arthritis (OR, 1.40; 95% CI, 1.14 to 1.72), difficulty in daily living due to hearing problems (OR, 1.56; 95% CI, 1.13 to 2.12), and fear of falling (OR, 1.85; 95% CI, 1.36 to 2.53) were associated with a risk of UI.
Table 2. Univariate logistic regression analysis of factors associated with urinary incontinence.
*Bronchitis or pulmonary emphysema. †Stroke, cerebral hemorrhage, or cerebral infarction. ‡Includes anxiety, insomnia, excessive stress, or difficulties in interpersonal relationships diagnosed by doctors.
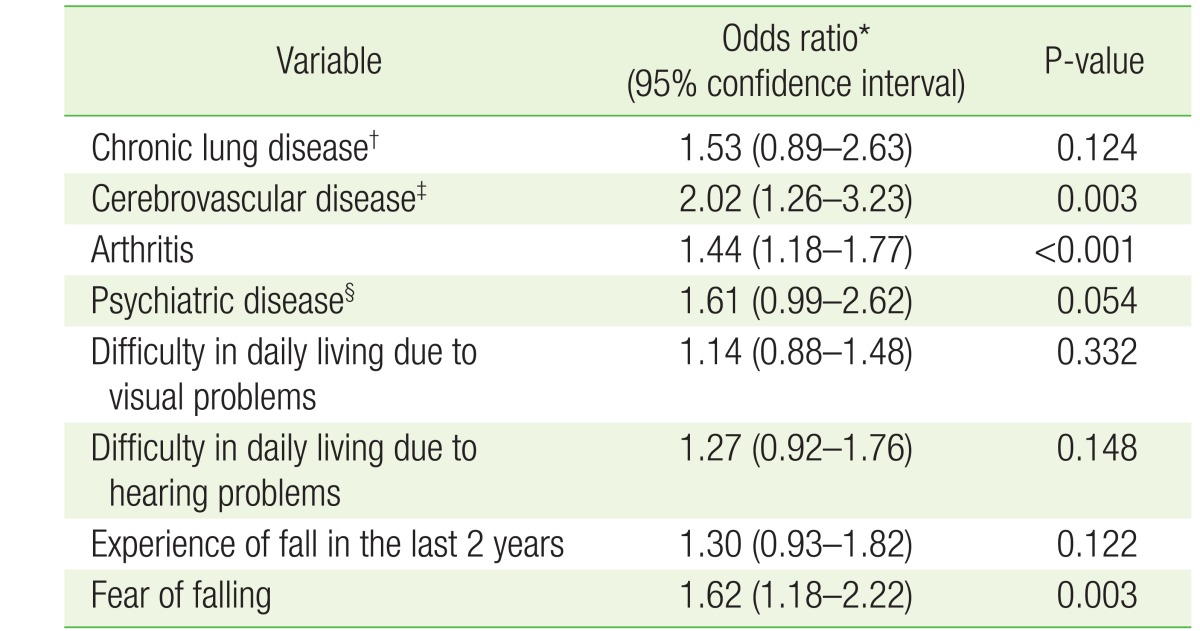
Table 3 shows the multivariate logistic regression analysis used to determine associations between UI and geriatric health problems after adjusting for covariates, such as age and education. Cerebrovascular disease (OR, 2.02; 95% CI, 1.26 to 3.23), arthritis (OR, 1.44; 95% CI, 1.18 to 1.77), and fear of falling (OR, 1.62; 95% CI, 1.18 to 2.22) were associated with a risk for UI. However, chronic lung disease, psychiatric disease, difficulty in daily living due to visual and hearing problems, and experience of a fall in the last 2 years were not significantly associated with UI in multivariate logistic regression analysis.
Table 3. Multivariate logistic regression analysis of factors associated with urinary incontinence.
*Adjusted for age and education. †Bronchitis or pulmonary emphysema. ‡Stroke, cerebral hemorrhage, or cerebral infarction. §Defined as anxiety, insomnia, excessive stress, or difficulties in interpersonal relationships diagnosed by doctors.
DISCUSSION
We found that UI is associated with geriatric health problems, especially with cerebrovascular disease, arthritis, and fear of falls, in older Korean women. In our study, advanced age was associated with UI. Another study showed age, parity, and obesity were associated with UI.6) Aging changes the bladder and the pelvic structure, which causes UI.1) In addition, atrophic changes in the urogenital tract that occur with aging cause urinary tract infections and UI.4) Women with diabetes are more likely to have UI. Hyperglycemia causes microvascular damage to bladder innervation and the urethral sphincter, which leads to diabetic cystopathy.15) Several studies have reported an increased prevalence of UI among women with diabetes. However, the impact of glycemic control on UI risk remains unclear.16) Our study indicates that there is no association between UI and diabetes. This may be explained by a lack of data distinguishing the different types of UI. Many studies have only used a self-reported history of diabetes in their analyses of associations between UI and diabetes.16) Further studies are required to explain the relationships between different types of UI and diabetes.
We found no association between UI and depression. One study of UI and depression showed no association between the two in multiethnic older women.17) However, another study indicated a threefold increase in depression in a group younger than 45 years compared to a group older than 45 years.18) In our study, cerebrovascular disease was identified as a significant factor associated with UI. In healthy adults, the normal micturition process is initiated by the medial frontal micturition centers, which activate the detrusor reflex, which is mediated by spinal cord circuits regulated by the pons. Urinary flow is sustained by detrusor contraction and sphincter relaxation.19) Brain damage causes detrusor overactivity and UI by interrupting suprapontine inhibition.20)
In our study, fear of falls was identified as a significant factor associated with UI, while falls had no association with UI. First, respondents who experienced falls might have not have remembered previous falling events during the survey. Second, women with UI frequently use the toilet with care, which may have reduced the occurrence of falling events. UI and falls are common problems for the elderly and are related to significant morbidity, mortality, and poor quality of life.7) It is reported that the prevalence of UI and falls gradually increase with age.21) In individuals aged 65 years and older, the prevalence of UI is approximately 8%–22% and the prevalence of falls is 19%–50%.22) Falls are associated with several risk factors.23,24) Old age, visual disturbances, cognitive disorders, and urge incontinence are identified as risk factors for falls.25,26,27) UI is one of the identified risk factors for falling. Chiarelli et al.28) reported an increased odds of falling of 1.45 (95% CI, 1.36 to 1.54) in the presence of any type of UI.29) In another epidemiological study, UI of urge type, but not UI of stress type, was reported as risk factor for falls.7) Individuals with UI who have experienced falls have a fear of falling. This limits the activities of these individuals and leads to poor health.25) In other words, UI is an important geriatric syndrome, not only as a disease in itself, but also for the individual's quality of life. Despite the association between UI and falls, there are limited intervention studies targeting a reduction of UI-related falls. It has been reported that incontinence interventions can successfully reduce the incidence of falls among cognitively normal older women.30) Therefore, intervention studies targeting UI as a component with falls as a primary outcome are needed.29)
Our study has several limitations. First, the cross-sectional design of our study prevented us from drawing conclusions regarding causality between UI and other variables. Second, we could not assess the type of UI, such as stress or urge types, as the data we had were insufficient for this purpose. It is important to know the type of UI as each type has a different treatment modality. Finally, our study was carried out based on a self-reporting survey for UI and chronic health problems. This may have resulted in the underreporting of incidences of UI.
Despite these limitations, we believe that our study contributes to a better understanding of UI and its associated factors. Based on our findings, we suggest that physicians consider other health problems, especially arthritis, fear of falling, and a history of cerebrovascular diseases, when they encounter old patients with UI. In addition, physicians should always consider and screen for UI when managing elderly women with geriatric syndromes. It is necessary to design effective UI interventions to promote healthy aging in the geriatric population. Further longitudinal studies are required to understand the causality between UI and other geriatric syndromes.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Silay K, Akinci S, Ulas A, Yalcin A, Silay YS, Akinci MB, et al. Occult urinary incontinence in elderly women and its association with geriatric condition. Eur Rev Med Pharmacol Sci. 2016;20:447–451. [PubMed] [Google Scholar]
- 2.Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29:213–240. doi: 10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- 3.Buckley BS, Lapitan MC Epidemiology Committee of the Fourth International Consultation on Incontinence, Paris, 2008. Prevalence of urinary incontinence in men, women, and children--current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76:265–270. doi: 10.1016/j.urology.2009.11.078. [DOI] [PubMed] [Google Scholar]
- 4.Aniuliene R, Aniulis P, Steibliene V. Risk factors and types of urinary incontinence among middle-aged and older male and female primary care patients in Kaunas Region of Lithuania: cross sectional study. Urol J. 2016;13:2552–2561. [PubMed] [Google Scholar]
- 5.Jung HB, Kim HJ, Cho ST. A current perspective on geriatric lower urinary tract dysfunction. Korean J Urol. 2015;56:266–275. doi: 10.4111/kju.2015.56.4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon CS, Lee JH. Prevalence, risk factors, quality of life, and health-care seeking behaviors of female urinary incontinence: results from the 4th Korean National Health and Nutrition Examination Survey VI (2007-2009) Int Neurourol J. 2014;18:31–36. doi: 10.5213/inj.2014.18.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards R, Hunter K, Wagg A. Lower urinary tract symptoms and falls in older women: a case control study. Maturitas. 2015;80:308–311. doi: 10.1016/j.maturitas.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Oh SJ, Park WH, Park CH, Paick JS, Seo JT, Lee YS, et al. Prevalence of urinary incontinence and incontinence-related quality of life in Korean women: a population-based study. J Korean Continence Soc. 2003;7:73–80. [Google Scholar]
- 9.Lee SH, Kang JS, Kim JW, Lee SJ. Incontinence pad usage in medical welfare facilities in Korea. Int Neurourol J. 2013;17:186–190. doi: 10.5213/inj.2013.17.4.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean J Urol. 2009;50:450–456. [Google Scholar]
- 11.Lee PG, Cigolle C, Blaum C. The co-occurrence of chronic diseases and geriatric syndromes: the health and retirement study. J Am Geriatr Soc. 2009;57:511–516. doi: 10.1111/j.1532-5415.2008.02150.x. [DOI] [PubMed] [Google Scholar]
- 12.Vetrano DL, Foebel AD, Marengoni A, Brandi V, Collamati A, Heckman GA, et al. Chronic diseases and geriatric syndromes: the different weight of comorbidity. Eur J Intern Med. 2016;27:62–67. doi: 10.1016/j.ejim.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 13.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55:780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allain TJ, Mwambelo M, Mdolo T, Mfune P. Falls and other geriatric syndromes in Blantyre, Malawi: a community survey of older adults. Malawi Med J. 2014;26:105–108. [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson SL, Scholes D, Boyko EJ, Abraham L, Fihn SD. Urinary incontinence and diabetes in postmenopausal women. Diabetes Care. 2005;28:1730–1738. doi: 10.2337/diacare.28.7.1730. [DOI] [PubMed] [Google Scholar]
- 16.Weinberg AE, Leppert JT, Elliott CS. Biochemical measures of diabetes are not independent predictors of urinary incontinence in women. J Urol. 2015;194:1668–1674. doi: 10.1016/j.juro.2015.06.074. [DOI] [PubMed] [Google Scholar]
- 17.Lagana L, Bloom DW, Ainsworth A. Urinary incontinence: its assessment and relationship to depression among community-dwelling multiethnic older women. ScientificWorldJournal. 2014;2014:708564. doi: 10.1155/2014/708564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vigod SN, Stewart DE. Major depression in female urinary incontinence. Psychosomatics. 2006;47:147–151. doi: 10.1176/appi.psy.47.2.147. [DOI] [PubMed] [Google Scholar]
- 19.Woessner H, Vibhute P, Barrett K. Acute loss of bladder control in a stroke of the frontal cortex. Neurohospitalist. 2012;2:129–131. doi: 10.1177/1941874412450715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pehrson R, Stenman E, Andersson KE. Effects of tramadol on rat detrusor overactivity induced by experimental cerebral infarction. Eur Urol. 2003;44:495–499. doi: 10.1016/s0302-2838(03)00353-1. [DOI] [PubMed] [Google Scholar]
- 21.Morris V, Wagg A. Lower urinary tract symptoms, incontinence and falls in elderly people: time for an intervention study. Int J Clin Pract. 2007;61:320–323. doi: 10.1111/j.1742-1241.2006.01174.x. [DOI] [PubMed] [Google Scholar]
- 22.Foley AL, Loharuka S, Barrett JA, Mathews R, Williams K, McGrother CW, et al. Association between the geriatric giants of urinary incontinence and falls in older people using data from the Leicestershire MRC Incontinence Study. Age Ageing. 2012;41:35–40. doi: 10.1093/ageing/afr125. [DOI] [PubMed] [Google Scholar]
- 23.Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R. Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol A Biol Sci Med Sci. 2002;57:M722–M726. doi: 10.1093/gerona/57.11.m722. [DOI] [PubMed] [Google Scholar]
- 24.Choi EJ, Kim SA, Kim NR, Rhee JA, Yun YW, Shin MH. Risk factors for falls in older Korean adults: the 2011 Community Health Survey. J Korean Med Sci. 2014;29:1482–1487. doi: 10.3346/jkms.2014.29.11.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moon SJ, Kim YT, Lee TY, Moon H, Kim MJ, Kim SA, et al. The influence of an overactive bladder on falling: a study of females aged 40 and older in the community. Int Neurourol J. 2011;15:41–47. doi: 10.5213/inj.2011.15.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coutinho ES, Fletcher A, Bloch KV, Rodrigues LC. Risk factors for falls with severe fracture in elderly people living in a middle-income country: a case control study. BMC Geriatr. 2008;8:21. doi: 10.1186/1471-2318-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown JS, Vittinghoff E, Wyman JF, Stone KL, Nevitt MC, Ensrud KE, et al. Urinary incontinence: does it increase risk for falls and fractures?: study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48:721–725. doi: 10.1111/j.1532-5415.2000.tb04744.x. [DOI] [PubMed] [Google Scholar]
- 28.Chiarelli PE, Mackenzie LA, Osmotherly PG. Urinary incontinence is associated with an increase in falls: a systematic review. Aust J Physiother. 2009;55:89–95. doi: 10.1016/s0004-9514(09)70038-8. [DOI] [PubMed] [Google Scholar]
- 29.Batchelor FA, Dow B, Low MA. Do continence management strategies reduce falls?: a systematic review. Australas J Ageing. 2013;32:211–216. doi: 10.1111/ajag.12047. [DOI] [PubMed] [Google Scholar]
- 30.Lee CY, Chen LK, Lo YK, Liang CK, Chou MY, Lo CC, et al. Urinary incontinence: an under-recognized risk factor for falls among elderly dementia patients. Neurourol Urodyn. 2011;30:1286–1290. doi: 10.1002/nau.21044. [DOI] [PubMed] [Google Scholar]