Abstract
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by a progressive joint damage due to largely unknown environmental factors acting in concert with risk alleles conferring genetic susceptibility. A major role has been attributed to viral infections that include past contacts with Epstein-Barr virus (EBV) and, more recently, to non-protein coding sequences of human endogenous retrovirus K (HERV-K) integrated in the human genome. Molecular mimicry between viral and self proteins is supposed to cause the loss of immune tolerance in predisposed hosts. There are evidences that anti-IL-2 antibodies (Abs) are present in subjects affected by autoimmune diseases and may be responsible for alterations in regulatory T cell responses. In this study, we evaluated the levels of Abs against IL-2, viral epitopes and interferon regulatory factor 5 (IRF5) in 140 RA patients and 137 healthy controls (HCs). Ab reactivity reached the highest levels for IRF5, EBV and IL-2 (56%, 44% and 39%, respectively) in RA with significantly lower values among HCs (7–9%, p < 0.0001), which suggests a possible cross-reaction between IRF5/EBV homologous antigens and shifts in T cell balance disrupted by anti-IL-2 Abs.
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disease of complex pathogenesis that leads to a progressive disability and major systemic complications with resulting socioeconomic concerns and premature death. Common manifestations involve synovial tissue inflammation and hyperplasia, autoantibody production, cartilage and bone destruction along with systemic features including pulmonary and cardiovascular complications1. RA is caused by largely unknown environmental factors acting in concert with risk alleles conferring genetic susceptibility2; among the former ones, a major role is attributed to viral infections putatively associated with numerous autoimmune diseases. The contribution of past contacts with Epstein-Barr virus (EBV) to RA pathogenesis has been postulated for over 30 years3. Although EBV resides stably at low levels during the lifetime in about 95% of the adult population worldwide4, molecular mimicry between viral and self proteins is supposed to cause the loss of immune tolerance in predisposed hosts5–9. More recently, human endogenous retrovirus K (HERV-K) has been called into question10–14. Remnants of previous HERV-K infections are present in the human genome as non-protein coding sequences integrated into germline cells15. Transcription of these elements may be activated or stimulated by exogenous viruses such as EBV resulting in the production of antigenic peptides16.
We have previously reported increased humoral responses to EBV and HERV-K peptides in Sardinian RA patients17,18 that mirrored elevated antibody (Abs) titers directed against an epitope derived from Mycobacterium avium subsp. paratuberculosis (MAP) homologous to EBV inner tegument protein BOLF1 and human interferon regulatory factor 5 (IRF5)19. IRF5 is known to mediate virus-induced immune responses including expression of proinflammatory cytokines and its pro-apoptotic effect is activated by EBV in transformed cells20,21. In systemic lupus erythematosus (SLE), IRF5 was found to negatively regulate the expression of interleukin-2 (IL-2)22. IL-2 is crucial for function, expansion and survival of regulatory T cells (Treg) and balance within this pathway is disrupted in Th1-mediated autoimmune diseases such as RA, SLE or type 1 diabetes (T1D)23–25. Recently, the loss of self-tolerance to IL-2 has been described in T1D subjects whose peripheral blood mononuclear cells yielded high quantities of INF-γ upon stimulation with IL-2-derived peptides26. Similarly, RA patients displayed raised levels of anti-IL-2 Abs supposed to affect IL-2 bioavailability necessary for Treg homeostasis.
In the present study, we evaluated humoral responses to synthetic IL-2 peptides in a larger cohort of Sardinian RA patients. A correlation analysis with seroreactivity to HERV-K and homologous EBV, MAP and IRF5 epitopes permitted to assess a possible cross-reactivity of the antigens supposedly involved in RA pathogenesis. Human autoantigens along with EBV elicited the highest responses, while the strongest correlation was found between IL-2 and HERV-K pointing at a potential pathway that links EBV-induced transactivation of retroviral proteins and the subsequent cytokine secretion mediated by IRF5.
Results
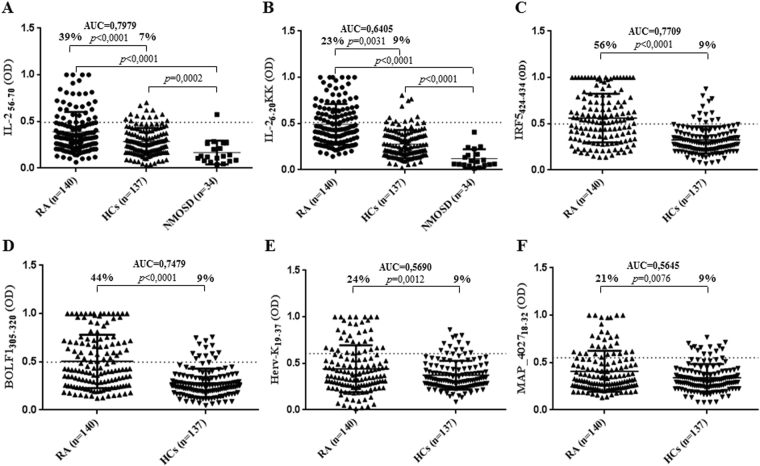
The potential to raise Ab responses differed between the two analyzed Il-2 peptides. IL-26–20KK elicited a higher Ab seroreactivity accounting for 39% (n = 55) among RA patients and 7% (n = 10) in HCs (p < 0.0001, Fig. 1A), while Abs against IL-256–70 were detected in 23% (n = 32) of RA subjects and 8% (n = 13) of HCs (p = 0.0031, Fig. 1B). However, the highest levels of autoreactive Abs were directed against IRF5424–434 observed in 56% (n = 79) of RA patients and only 9% (n = 13) of HCs (p < 0.0001, Fig. 1C). Slightly lower prevalence was observed for anti-BOLF1305–320 Abs found in 44% (n = 61) of RA subjects and 9% of HCs (p < 0.0001, Fig. 1D). Responses against Herv-Kenv19–37 and MAP_402718–32 were maintained at the same levels (9%) among HCs, while seroreactivity of RA patients equaled 24% (n = 34, p = 0.0012, Fig. 1E) and 21% (n = 30, p = 0.0076, Fig. 1F), respectively. Despite antigen-related differences in single-type Abs prevalence, all results attained statistical significance with the highest AUC values for IL-26–20KK and IRF5424–434.
Figure 1.
ELISA-based analysis of Abs reactivity against human, viral and MAP-derived peptides in RA, NMOSD and HCs. The sera were tested against plate-coated IL-26–20KK (B), IL-256–70 (A), IRF5424–434 (C), BOLF1305–320 (D), Herv-Kenv19–37 (E) and MAP_402718–32 (F) peptides. Bars represent the median ± interquartile range. Thresholds for Abs positivity are indicated by dashed lines. Percentages of Abs prevalence respective to each group, AUC and P-values are indicated above the distributions.
The prevalence of Abs against both IL-2 epitopes was additionally assessed in 34 samples of patients affected by neuromyelitis optica spectrum disorder (NMOSD). Only one patients displayed values above the established cut-off for IL-256–70 (2.9%, Fig. 1A) whereas lower means obtained for IL-26–20KK were mirrored by the absence of positive cases (Fig. 1B). Moreover, the responses of NMOSD patients were markedly lower compared not only to RA subjects, but also to HCs. The immunone response against the other peptides of this study in NMOSD patients has been evaluated in another study (manuscript submitted).
To test the specificity of humoral responses mounted against the selected peptides, 22 HCs and 22 RA patients were randomly selected from the study population and tested for seroreactivity against J0I929_HELPX1–11 control peptide derived from Helicobacter pylori homologous to human ZnT827. In both groups, half number of samples tested positive to at least one (HCs) or all (RA) of the previously assessed peptides. The observed mean values were slighty higher for HCs and corresponded to the absence of positive subjects compared to 9% (n = 2) among RA patients, however statistical significance was not attained (p = 0.07). Interestingly, RA individuals with multiple Abs positivity presented lower mean values compared to HCs with single-peptide positivity (Fig. 2).
Figure 2.
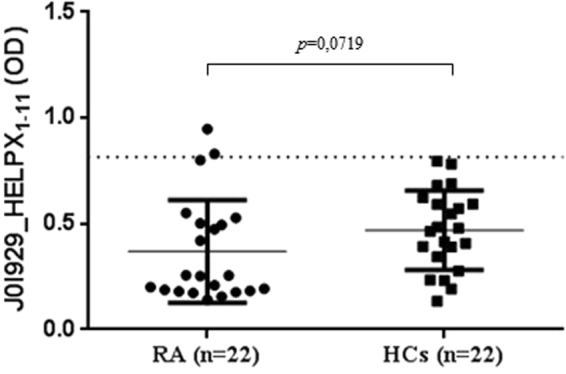
Abs reactivity against the antigenic peptide derived from H. pylori in RA patients and HCs. Bars represent mean value ± interquartile range, while dashed lines indicate the positivity threshold. Despite sequence homology to human ZnT8 protein fragment, no significant differences in Abs levels were detected.
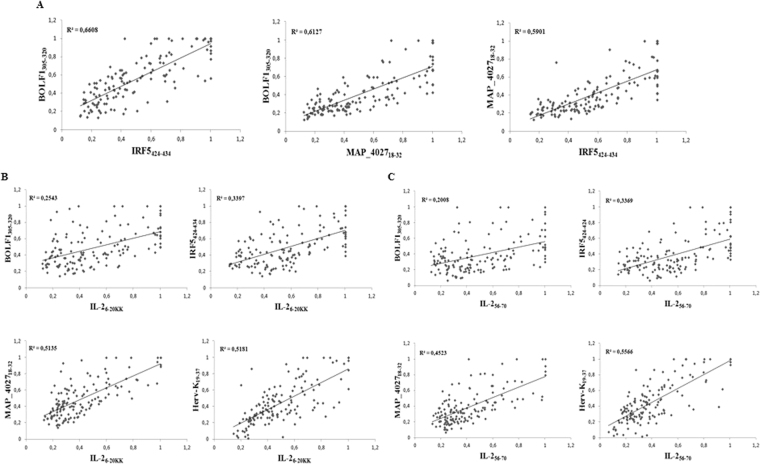
To define associations between the antigenicity of the assessed peptides we performed correlation analyses of Abs positivity values among RA patients (Fig. 3). The highest coefficients were obtained for the homologous epitopes BOLF1305–320, MAP_402718–32 and IRF5424–434 in pairwise plots (Fig. 3A) pointing at cross-reactivity due to shared amino acid sequence. Correlation trends of both IL-2 peptides were similar with respect to the other antigens (Fig. 3B,C): Herv-Kenv19–37 and MAP_402718–32 correlated moderately with either IL-26–20KK or IL-256–70, however IL-256–70/Herv-Kenv19–37 distribution corresponded to a slightly higher R2 value (Fig. 3B). Unexpectedly, weak to modest correlations were found between IL-2, IRF5424–434 and BOLF1305–320 (Fig. 3C).
Figure 3.
Scatter plots showing correlations between Abs titers in RA patients. Pairwise distributions are classified for homologous peptides (A), IL-26–20KK (B) and IL-256–70 (C). Each dot correspond to OD values obtained for a single patient.
We further evaluated multiple positivity to the assessed peptides in order to verify whether correlations between Ab titers find correspondence with the overlap in seroreactivity against IL-2 (Table 1). In contrast to mild correlations of both IL-2 epitopes plotted against IRF5424–434 or BOLF1305–320, double or triple humoral responses to these antigens were detected in a major number of subjects with distinctly higher percentages for IL-2/IRF5 reflecting single-peptide Abs prevalence. On the other hand, responsiveness to Herv-Kenv19–37 overlapped well with the presence of anti-IL-256–70 Abs as expected from the correlation analysis and stood out also in triple positivity with positivity to IRF5424–434. Even though multiple responses among HCs are low in general, they visibly tend to diminish for Abs against at least three antigens.
Table 1.
Multiple Abs prevalence in RA patients and HCs. Seroreactivity against IL-2 antigens was compared with humoral responses to MAP, EBV, HERV-K and human IRF5 peptides.
| IL-256–70 | IL-26–20 KK | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| HCs | RA | HCs | RA | IL-2 | BOLF1305–320 | IRF5424–434 | MAP_402718–32 | Herv-K19–37 | |
| b | 5 (3.65) | 24 (17.14) | 5 (3.65) | 36 (25.17) |
|
||||
| 2 (1.46) | 27 (19.28) | 4 (2.92) | 43 (30.71) |
|
|
||||
| b | 3 (2.19) | 20 (14.28) | 4 (2.92) | 28 (20.00) |
|
|
|||
| a | 5 (3.65) | 25 (17.86) | 0 | 29 (20.71) |
|
|
|||
| 2 (1.46) | 20 (14.28) | 0 | 24 (17.14) |
|
|
||||
| 1 (0.73) | 20 (14.28) | 2 (1.46) | 27 (19.28) |
|
|
||||
| 1(0.73) | 24 (17.14) | 3 (2.19) | 33 (23.57) |
|
|||||
| 0 | 19 (13.57) | 2 (1.46) | 27 (19.28) |
|
|
||||
| 1 (0.73) | 17 (12.14) | 0 | 19 (13.57) |
|
|
||||
| 1 (0.73) | 23 (16.43) | 0 | 27 (19.28) |
|
|
|
|||
| 0 | 19 (13.57) | 1 (0.73) | 26 (18.57) |
|
|||||
| 0 | 19 (13.57) | 0 | 23 (16.43) |
|
|
||||
| 1 (0.73) | 17 (12.14) | 0 | 20 (14.28) |
|
|
||||
| 0 | 19 (13.57) | 0 | 19 (13.57) |
|
|
||||
| 0 | 16 (11.43) | 0 | 19 (13.57) |
|
|||||
The numbers of subjects positive for anti-IL-26–20KK and/or anti-IL-256–70 Abs are reported with relative percentages in brackets. Horizontal bars indicate Abs against at least two antigens identified in the samples with IL-2 referred to as both IL-26–20KK and IL-256–70. p < 0.0001 for all values except aIL-256–70 (p < 0.0002) and bIL-256–70 (p < 0.0003).
Upon sex-related screening of RA samples, females showed higher mean Abs values and positivity prevalence for all peptides compared to males, however statistical significance was reached only for IRF5424–434 (p = 0.034). After classification of RA patients and HCs in three age groups (≤49, 50–59 and ≥60), the highest responsiveness was observed for BOLF1, IRF5 and IL-26–20KK (Table 2). This trend was clearly visible in the youngest RA group regardless of sex, however females maintained it more stably until the age of 59. In contrast to men, humoral responses of RA and HC women were not significant in the oldest group but this could be affected by a small number of elderly HCs in our study population. A general decrease in Ab positivity proportional to age was common to either male or female patients. Importantly, seroreactivity to IRF5 exceeded 93% in the youngest females and reached a 100% in ≤49 year-old males (one patient).
Table 2.
Age- and sex-related Abs prevalence in RA patients and HCs.
| Gender | Age (y) | N | Subjects | BOLF1 | P | IRF5 | P | MAP_4027 | P | IL-2 56–70 | P | IL-2 6–20KK | P | Herv-K19–37 | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Females | ≤49 | 16 | RA | 12 (75%) | <0,0001 | 15 (93,75%) | <0,0001 | 5 (31,25%) | 0,0063 | 5 (31,25%) | 0,088 | 8 (50%) | <0,0001 | 5 (31,25%) | 0,38 |
| 65 | HCs | 8 (12,30%) | 6 (9,2%) | 5 (7,6%) | 9 (13,8%) | 6 (9,2%) | 9 (13,8%) | ||||||||
| 50–59 | 41 | RA | 21 (51,21%) | <0,0001 | 23 (56,09%) | <0,0001 | 8 (19,51%) | 0,51 | 10 (24,39%) | 0,045 | 20 (48,78%) | <0,0001 | 9 (21,95%) | 0,13 | |
| 19 | HCs | 2 (10,52%) | 1 (5,2%) | 3 (15,78%) | 1 (5,2%) | 1 (5,2%) | 1 (5,2%) | ||||||||
| ≥60 | 49 | RA | 17 (34,69%) | 0,17 | 25 (51,02%) | 0,024 | 11 (22,44%) | 0,92 | 12 (22,44%) | 0,61 | 17 (34,69%) | 0,081 | 15 (30,61%) | 0,17 | |
| 6 | HCs | 1 (16,66%) | 1 (16,66%) | 0 | 1 (16,66%) | 1 (16,66%) | 0 | ||||||||
| Males | ≤49 | 6 | RA | 4 (66,66%) | 0,0046 | 6 (100%) | 0,0001 | 3 (50%) | 0,094 | 3 (50%) | 0,302 | 4 (66,66%) | 0,0449 | 2 (33,33%) | 0,34 |
| 15 | HCs | 2 (13,33%) | 1 (6,6%) | 4 (13,3%) | 1 (6,6%) | 2 (13,33%) | 1 (6,6%) | ||||||||
| 50–59 | 11 | RA | 2 (18,18%) | 0,0023 | 3 (27,27%) | 0,535 | 1 (9%) | 0,43 | 2 (9%) | 0,015 | 1 (18,18%) | 0,0006 | 2 (18,18%) | 0,198 | |
| 23 | HCs | 0 | 3 (13,04%) | 1 (4,3%) | 1 (4,3%) | 0 | 1 (4,3%) | ||||||||
| ≥60 | 17 | RA | 5 (29,41%) | 0,0035 | 7 (41,17%) | 0,104 | 3 (17,64%) | 0,0246 | 1 (5,8%) | 0,0211 | 4 (23,52%) | 0,0005 | 1 (5,8%) | 0,652 | |
| 9 | HCs | 0 | 1 (11,1%) | 0 | 0 | 0 | 1 (11,1%) |
The numbers of individuals responsive to single antigens are provided with relative percentages. Statistically significant values are highlighted in bold.
PCA analysis permitted to identify relationships between clinical variables and the selected epitopes with 79.17% of cumulative variation describing four principal components (Table 3). Correlation between Ab values and two inflammatory parameters was low but attained a statistical significance that differed based on the analyzed measure: ESR correlated to Ab values towards IL-2 and HERV-K, while CRP yielded higher coefficients in plots with the homologous MAP, EBV and IRF5 antigens. No correlation with other clinical data was found.
Table 3.
Correlation coefficients between inflammation measures, demographic data and seroreactivity relative to the selected antigens. All correlations are expressed as squared cosines of the variables.
| PC1 | PC2 | PC3 | PC4 | |
|---|---|---|---|---|
| BOLF1 | 0,629 | 0,017 | 0,063 | 0,003 |
| IRF5 | 0,732 | 0,014 | 0,037 | 0,004 |
| MAP_4027 | 0,820 | 0,000 | 0,000 | 0,005 |
| IL-256–70 | 0,685 | 0,042 | 0,012 | 0,008 |
| IL-26–20KK | 0,726 | 0,047 | 0,028 | 0,001 |
| Herv-K | 0,596 | 0,099 | 0,037 | 0,000 |
| ESR | 0,044 | 0,281 | 0,475 | 0,007 |
| CRP | 0,023 | 0,660 | 0,002 | 0,120 |
| Age | 0,041 | 0,065 | 0,590 | 0,015 |
| Sex | 0,054 | 0,206 | 0,004 | 0,727 |
Discussion
Recent reports on the loss of self-tolerance to IL-2 in autoimmune diseases encouraged us to evaluate the presence of anti-IL-2 Abs in Sardinian RA patients in association to antigens most frequently described as possible contributors to RA progression. Our results confirm the involvement of IL-2 in RA at higher rates compared to a French cohort (39% vs.15%, respectively)26 and is mirrored by a concomitant positivity to peptide antigens derived from EBV, HERV-K, MAP or human IRF5. The latter has been linked to acute inflammation as a factor promoting polarization of macrophages towards an inflammatory phenotype in antigen-induced RA mouse models and driving Th1/Th17 responses28–30.
In the present study, IRF5, together with the EBV surface tegument protein BOLF1 and IL-2, triggered the greatest response even though devoid of a good correlation with IL-2. This suggests that the association between the two human autoantigens may not be proportionally dependent on Ab titers but favour autoimmunity when a tolerance threshold is surmounted. In contrast, IRF5 correlated well with homologous BOLF1 and MAP epitopes pointing at molecular mimicry that leads to a probable cross-reactivity with the assessed environmental agents to which humans are constantly exposed. This was recently confirmed by the competitive inhibition assay in our previous study31. For IL-2, the best correlation was obtained in the plot with HERV-K. While reactivation of endogenous retroviral protein expression may elicit serological and cell-mediated responses, an uncontrolled expansion of Treg cells in subjects who lost self-tolerance to IL-2 or IRF5 may explain the development of autoimmunity. Interestingly, over 30% of our RA cohort displayed anti-IL-2/IRF5 Abs in a highly significant double positivity (p < 0.0001) and a more frequent multiple seroreactivity was observed in RA patients compared to healthy controls (Table 1).
Major prevalence of Abs directed against all single peptides and higher mean Abs values obtained for RA females in a sex-related analysis point at a more grave disease course proper to women and highlight the involvement of IRF5. This was mirrored by a strikingly high prevalence of Abs against IRF5 in the ≤49 year-old group independently of patients’ sex. An elevated general seroreactivity observed in the youngest group that decreases with age points at strong immune responses accompanying early disease onset.
A significant correlation between levels of anti-IL-2 Abs and measures of systemic inflammation (Table 3) is supportive of the hypothesis that anti-IL-2-driven impairment of Treg activity may alter autoimmune processes and inflammatory burden. Other than expected, we did not find significant correlations between disease severity, immunosuppressive treatment, RF and ACPA status with levels and positivity of anti-IL-2 Abs. It should be acknowledged that all patients were under different immunosuppressive drugs at the moment of sample collection. The heterogeneity of treatment across subjects may have biased interpretation and significance of associations between humoral responses and inflammatory measures. Further analysis of IL-2 levels, quantification of INF-γ upon stimulation with the analyzed peptides and Treg activity are needed to complete our observations. More numerous groups of the youngest patients at RA onset and elderly HCs would additionally permit to associate the efficacy of therapy in modulating serological and cell responses.
Materials and Methods
Subjects
Blood samples of 140 RA patients (34 males, 106 females; median age 58.95) and 137 healthy controls (HCs; 47 males, 90 females; median age 46.30) were collected in Vacutainer tubes for the separation of serum and further screening for Abs against IL-2, IRF5, MAP_4027, BOLF1 and HERV-K by indirect enzyme-linked immunosorbent assay (ELISA). RA patients who met the criteria of the American College of Rheumatology32,33 were enrolled from the outpatient clinic of the Rheumatology Unit, Department of Clinical and Experimental Medicine, University Hospital of Sassari, Italy. Clinical data collected during control medical visits included information relative to the duration of RA, therapy (steroids, Tocilizumab, Rituximab, Abatacept, DMARDs, Etanercept, Adalimumab, Golimumab, Infliximab and Certolizumab anti-TNF-α), levels of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) levels, positivity to rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP), Disease Activity Score-28 (DAS-28) and grade of disability defined through the health assessment questionnaire (HAQ). 34 NMOSD patients (5 males, 29 females; median age 51.32) were enrolled at the Neurology Clinic of the University Hospital of Sassari and at the Department of Neurosciences, Biomedicine and Motion, University of Verona, Italy. HCs were recruited at the Blood Transfusion Center of Sassari, Italy. Demographic, clinical and laboratory characteristics of the participants are summarized in Table 4. Ethical clearance for the study protocols was achieved from the local health authority (Azienda Ospedaliero-Universitaria, protocols 1134/L-16/04/2013 and 1192/L-04/02/2014) and all methods were performed in accordance with national and regional regulations. All participants were resident in Sardinia and signed written informed consent.
Table 4.
Demographics, clinical history and laboratory data of RA patients and HCs.
| RA n = 140 | HCs n = 137 | p value | |
|---|---|---|---|
| Age, yrs | 59 ± 10 | 46 (13) | <0.001 |
| Female sex, n (%) | 106 (79.3) | 90 (65.7) | 0.02 |
| Early disease, n (%) | 10 (7.2) | ||
| ACPA positivity, % | 74.1 | ||
| RF positivity | 74.4 | ||
| HAQ (0–3) | 0.83 (0.73) | ||
| DAS-28 | 3.59 ± 1.33 | ||
| CRP, mg/dL | 0.8 ± 1.1 | ||
| ESR, mm/h | 29 ± 24 | ||
| Steroids therapy, % | 41 | ||
| DMARDs therapy, % | 63.3 | ||
| Anti-TNF therapy, % | 25.9 | ||
| Tocilizumab therapy, % | 12.9 | ||
| Abatacept therapy, % | 4.3 |
Data are expressed as median ± 1 standard deviation. RA duration <12 months is reported as early disease. ACPA: anti-cyclic citrullinated peptide antibodies. RF: rheumatoid factor. HAQ: health assessment questionnaire. DAS-28: Disease Activity Score-28. CRP: C-reactive protein. ESR: erythrocyte sedimentation rate. DMARDs: disease modifying anti-rheumatic drugs. Anti-TNF: anti-tumor necrosis factor alpha.
Antigens
The following peptides synthesized commercially at >90% purity (LifeTein, South Plainfield, USA) were included in the study: IL-26–20KK (KK-LLSCIALSLALVTNS-KK) and IL-256–70 (LTEMLTFKFYMPKKA) based on Pérol et al. with modifications26, IRF5424–434 (VVPV–AARL-LLE), MAP_402718–32 (AVVPVLAYAAARL-LL), BOLF1305–320 (AAVPVLAFDAARLRLLE) and Herv-Kenv19–37 (VWVPGPTDDRCPAKPEEEG). In addition, J0I929_HELPX1–11 (MIIGGGVSGCA) derived from H. pylori quinone oxidoreductase, homologous to human ZnT827 was used as a control peptide. Moreover, wells containing no peptides adsorbed were included as negative control.
Enzyme-linked immunosorbent assays (ELISA) and statistical analysis
Indirect ELISA to detect specific Abs against the selected antigens was performed as described previously34. The optical density (OD) was read at a wavelength of 405 nm using SpectraMax Plus 384 microplate reader (Molecular Devices, Sunnyvale, CA 94089, USA). For data normalization, a highly responsive serum with Ab reactivity fixed at 1.0 arbitrary unit (AU)/ml was included in all experiments. The results were expressed as a mean of three separate experiments and the statistical analyses were performed using Graphpad Prism 6.0 software (GraphPad Software Inc., La Jolla, CA 92037, USA). Upon determination of sample distribution through D’Agostino-Pearson normality test, values between RA patients and HCs were compared using a two-tailed Mann-Whitney U test with p < 0.05 considered statistically significant. The cut-off for positivity was established in the interval 0.49–0.60 (AU)/ml based on the receiver operating characteristic (ROC) curve (Fig. 1) with ≥90% specificity and 95% confidence interval. Fisher’s exact test was employed to compare the percentages of positive subjects in the two groups. Correlations between variables were analyzed through principal component analysis (PCA) using XLSTAT software ver. 17 (Addinsoft, New York).
Acknowledgements
The authors declare that the work was done thanks to the spare funds collected from different sources but not Italian or funds from the Sardinian Region.
Author Contributions
M.B. was involved in the experimental design, carried out the samples analysis, analyzed the results and drafted the manuscript. M.N. carried out the samples analysis and analyzed the results. G.P. and G.E. analyzed the results, M.M., P.M., M.P. and M.G.L. contributed to materials and sample collection. L.A.S. conceived the study and its experimental design, analyzed the results and helped to draft the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Firestein GS. Evolving concepts of rheumatoid arthritis. Nature. 2003;423:356–361. doi: 10.1038/nature01661. [DOI] [PubMed] [Google Scholar]
- 2.McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365:2205–2219. doi: 10.1056/NEJMra1004965. [DOI] [PubMed] [Google Scholar]
- 3.Ollier W. Rheumatoid arthritis and Epstein-Barr virus: a case of living with the enemy? Ann Rheum Dis. 2000;59:497–499. doi: 10.1136/ard.59.7.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hadinoto V, et al. The dynamics of EBV shedding implicate a central role for epithelial cells in amplifying viral output. PloS Pathog. 2009;5(7):e1000496. doi: 10.1371/journal.ppat.1000496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adtani P, Malathi N. Epstein-Barr virus and its association with rheumatoid arthritis and oral lichen planus. J Oral Maxillofac Pathol. 2015;19(3):282–5. doi: 10.4103/0973-029X.174643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ball RJ, Avenell A, Aucott L, Hanlon P, Vickers MA. Systematic review and meta-analysis of the sero-epidemiological association between Epstein-Barr virus and rheumatoid arthritis. Arthritis Res. 2015;29(17):274. doi: 10.1186/s13075-015-0755-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westergaard MW, Draborg AH, Troelsen L, Jacobsen S, Houen G. Isotypes of Epstein-Barr virus antibodies in rheumatoid arthritis: association with rheumatoid factors and citrulline-dependent antibodies. Biomed Res Int. 2015;2015:472174. doi: 10.1155/2015/472174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahabadi M, Faghihiloo E, Alishiri GH, Ataee MH, Ataee RA. Detection of Epstein-Barr virus in synovial fluid of rheumatoid arthritis patients. Electron Physician. 2016;25(8(3)):2181–6. doi: 10.19082/2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balandraud, N. & Roudier J. Epstein-Barr virus and rheumatoid arthritis. Joint Bone Spine. pii: S1297-319X(17)30093-3 [Epub ahead of print] (2017). [DOI] [PubMed]
- 10.Manghera M, Douville RN. Endogenous retrovirus-K promoter: a landing strip for inflammatory transcription factors? Retrovirology. 2013;10:16. doi: 10.1186/1742-4690-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reynier F, et al. Increase in human endogenous retrovirus HERV-K (HML-2) viral load in active rheumatoid arthritis. Scand J Immunol. 2009;70:295–9. doi: 10.1111/j.1365-3083.2009.02271.x. [DOI] [PubMed] [Google Scholar]
- 12.Reimanis G, et al. A role for human endogenous retrovirus-K (HML-2) in rheumatoid arthritis: investigating mechanisms of pathogenesis. Clin Exp Immunol. 2010;160:340–7. doi: 10.1111/j.1365-2249.2010.04110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson PN, et al. Rheumatoid arthritis is associated with IgG antibodies to human endogenous retrovirus gag matrix: a potential pathogenic mechanism of disease? J Rheumatol. 2014;41:1952–60. doi: 10.3899/jrheum.130502. [DOI] [PubMed] [Google Scholar]
- 14.Tugnet N, Rylance P, Roden D, Trela M, Nelson P. Human endogenous retroviruses (HERVs) and autoimmune rheumatic disease: is there a link? Open Rheumatol J. 2103;7:13–21. doi: 10.2174/1874312901307010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lander ES, et al. Initial sequencing and analysis of the human genome. Nature. 2001;15(409(6822)):860–921. doi: 10.1038/35057062. [DOI] [PubMed] [Google Scholar]
- 16.Nelson PN, et al. Demystified. Human endogenous retroviruses. Mol Pathol. 2003;56(1):11–8. doi: 10.1136/mp.56.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erre GL, et al. Increased Epstein-Barr Virus DNA Load and Antibodies Against EBNA1 and EA in Sardinian Patients with Rheumatoid Arthritis. Viral Immunol. 2015;28(7):385–90. doi: 10.1089/vim.2015.0035. [DOI] [PubMed] [Google Scholar]
- 18.Mameli G, et al. Identification of HERV-K env surface peptide highly recognized in Rheumatoid Arthritis (RA) patients: a cross-sectional case-control study. Clin Exp Immunol. 2017;189(1):127–131. doi: 10.1111/cei.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erre GL, et al. Mycobacterium tuberculosis lipoarabinomannan antibodies are associated to rheumatoid arthritis in Sardinian patients. Clin Rheumatol. 2014;33:1725–9. doi: 10.1007/s10067-014-2678-z. [DOI] [PubMed] [Google Scholar]
- 20.Xu D, Meyer F, Ehlers E, Blasnitz L, Zhang L. Interferon Regulatory Factor 4 (IRF-4) Targets IRF-5 to Regulate Epstein-Barr Virus Transformation. J Biol Chem. 2011;20(286(20)):18261–7. doi: 10.1074/jbc.M110.210542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cham CM, Ko K, Niewold TB. Interferon regulatory factor 5 in the pathogenesis of systemic lupus erythematosus. Clin Dev Immunol. 2012;2012:780436. doi: 10.1155/2012/780436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo Q, Chen XY, Su Y. Interleukin-2 Signaling Pathway Regulating Molecules in Systemic Lupus Erythematosus. Beijing Da Xue Xue Bao. 2016;48(6):1100–1104. [PubMed] [Google Scholar]
- 23.Bayer AL, Yu A, Adeegbe D, Malek TR. Essential role for interleukin-2 for CD4+CD25+ T regulatory cell development during the neonatal period. J Exp Med. 2005;201:769–777. doi: 10.1084/jem.20041179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thornton AM, Piccirillo CA, Shevach EM. Activation requirements for the induction of CD4+CD25+ T cell suppressor function. Eur. J. Immunol. 2004;34:366–376. doi: 10.1002/eji.200324455. [DOI] [PubMed] [Google Scholar]
- 25.Niu Q, Cai B, Huang ZC, Shi YY, Wang LL. Disturbed Th17/Treg balance in patients with rheumatoid arthritis. Rheumatol Int. 2012;32(9):2731–6. doi: 10.1007/s00296-011-1984-x. [DOI] [PubMed] [Google Scholar]
- 26.Pérol L, et al. Loss of immune tolerance to IL-2 in type 1 diabetes. Nat Commun. 2016;6(7):13027. doi: 10.1038/ncomms13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Masala S, et al. Lack of humoral response against Helicobacter pylori peptides homologous to human ZnT8 in Hashimoto’s thyroiditis patients. J Infect Dev Ctries. 2015;9(6):631–4. doi: 10.3855/jidc.6284. [DOI] [PubMed] [Google Scholar]
- 28.Krausgruber T, et al. IRF5 promotes inflammatory macrophage polarization and TH1–TH17 responses. Nature Immunology. 2011;12:231–238. doi: 10.1038/ni.1990. [DOI] [PubMed] [Google Scholar]
- 29.Weiss M, et al. IRF5 controls both acute and chronic inflammation. Proc Natl Acad Sci USA. 2015;112:11001–11006. doi: 10.1073/pnas.1506254112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss M, Blazek K, Byrne AJ, Perocheau DP, Udalova IA. IRF5 is a specific marker of inflammatory macrophages in vivo. Mediators Inflamm. 2013;2013:245804. doi: 10.1155/2013/245804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bo, M. et al. Mycobacterium avium subspecies paratuberculosis and myelin basic protein specific epitopes are highly recognized by sera from patients with Neuromyelitis Optica Spectrum Disorder. J of Neuroimmunol. Submitted (2018). [DOI] [PubMed]
- 32.Arnett FC, et al. The American Rheumatism Association1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 33.Aletaha D, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69(9):1580–8. doi: 10.1136/ard.2010.138461. [DOI] [PubMed] [Google Scholar]
- 34.Mameli G, et al. Epstein–Barr virus and Mycobacterium avium subsp. paratuberculosis peptides are cross recognized by anti-myelin basic protein antibodies in multiple sclerosis patients. Journal of Neuroimmunology. 2014;270(1-2):51–5. doi: 10.1016/j.jneuroim.2014.02.013. [DOI] [PubMed] [Google Scholar]