Abstract
Purpose
Zika virus infection is associated with vision-threatening ocular complications including uveitis and outer retinopathy. The aim of this report is to describe a case of an adult patient with serologically confirmed Zika infection who presented with retinal vascular abnormalities that coincided with systemic post-viral neurological manifestations of the disease.
Observations
A 34-year-old white female presented with symptoms of peripheral neuropathy following serologically confirmed Zika virus infection that was acquired in Puerto Rico four months prior to presentation. Ocular evaluation revealed perifoveal microaneurysms which were not associated with visual symptoms.
Conclusions and importance
These data potentially expand the phenotypic spectrum of Zika virus retinopathy. In addition to outer retinal abnormalities which are well-described in infants and adults, inner retinal vascular abnormalities may also occur and may be temporally associated with post-viral neurological sequelae of Zika virus infection. Clinicians should be aware of potential retinal involvement in affected patients who present with neurological symptoms after recovery from acute Zika virus infection.
Keywords: Zika virus, Retina, Vision, Vasculopathy, Angiography, Multimodal imaging
1. Introduction
Zika virus infection is known to cause vision-threatening ocular disease in infants and adults. Outer retinal and retinal pigment epithelium (RPE) lesions include macular pigment mottling and chorioretinal atrophy in approximately two-thirds of affected eyes in infants.1 Data in older patients have also implicated the outer retina as the locus of disease in ZIKV retinopathy.2, 3, 4, 5, 6, 7 Here we report a patient who presented with abnormalities in the inner retinal vasculature, concurrent with the onset of systemic neurological symptoms in the post-viral period.
2. Case report
A 38-year-old nondiabetic white female complained of intermittent numbness and tingling in all extremities. Four months prior, she had developed Zika virus infection in Puerto Rico (IgM ELISA and PRNT positive, RT-PCR negative) with a generalized maculopapular rash, fever, headache, conjunctivitis, arthralgia and myalgia. Tests for Dengue and Chikungunya viruses were negative, and there was evidence of previous West Nile virus infection (IgG elevated and IgM negative). She described a prior episode, years earlier, of painful genital and oral ulceration of unknown etiology (herpes, syphilis, HIV, tuberculosis and toxoplasmosis tests were negative).
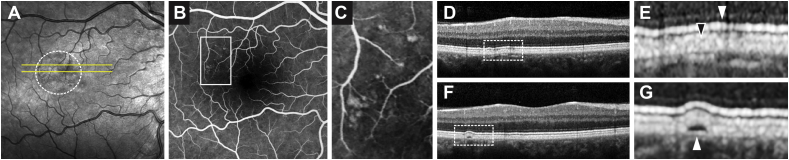
The patient did not have visual symptoms and her uncorrected visual acuity was 20/20 in the right eye and 20/25 in the left. The confrontation visual field, pupil reflex, anterior segment and intraocular pressure were normal in both eyes. Slit-lamp ophthalmoscopy revealed microaneurysms in the right macula. Infrared reflectance imaging (Spectralis HRA, Heidelberg Engineering, Germany) showed a hyporeflective macular lesion (Fig. 1A). Fundus fluorescein angiography revealed perifoveal microaneurysms in the inner retinal circulation (Fig. 1B and C). Optical coherence tomography (OCT) imaging showed an RPE detachment adjacent to a zone of outer retinal and RPE irregularity (Fig. 1D–G), underlying the region of inner retinal change, without macular edema. Fundus-controlled microperimetry (MP1 Retinal Microperimeter, Nidek Technologies, Italy) did not reveal any loss of retinal sensitivity. The findings remained stable over 6 subsequent weeks and routine monitoring is now scheduled.
Fig. 1.
Abnormalities in the inner retina, revealed by multimodal retinal imaging. (A) Infrared reflectance map of the right macula showing areas of reduced reflectance (dotted circle) outside of the foveal center. The horizontal lines indicate the position of the cross-sectional scans shown in D–E (top line) and F–G (bottom line). (B) Fundus fluorescein angiogram of the right retina showing microaneurysms located superotemporal to the foveal center. (C) Enlarged section showing the number and distribution of microaneurysms from the box in (B). (D) Optical coherence tomography section of the macula showing abnormalities in the outer retina with the dotted box enlarged in (E). (E) Irregularity of the bright horizontal lines corresponding to the photoreceptor ellipsoid zone (white arrowhead) and photoreceptor-retina pigment epithelium (RPE) interdigitating zone (black arrowhead). (F) Another section across the macula demonstrating a small detachment of the RPE, dotted box enlarged in (G, arrowhead) to show greater detail.
3. Discussion
To our knowledge, this is the first report of inner retinal abnormalities that are temporally associated with ZIKV disease. The human retina has inner and outer zones that are supplied by the distinct retinal and choroidal circulations, respectively. The inner retinal vasculature, supplied by the central retinal artery, is distinct from the choroidal system and is often involved in other viral retinopathies. Based on available information, we could not exclude prior retinal involvement in West Nile virus or Behçet diseases. We considered macular telangiectasia as a differential diagnosis; however, there were no supporting features such as reduced retinal transparency, right-angled venules, cystic spaces, retinal crystals, or loss of macular pigment in either eye. There were no features in the history, biomicroscopy or imaging findings to support branch retinal vein occlusion affecting the central macula. The unilateral presentation in this case may reflect interocular asymmetry in vascular anatomy or flow.
The spectrum of ZIKV retinal disease in adults is not yet fully known. The retinal findings here add to our understanding of retinal involvement in ZIKV disease by indicating a possible new cellular locus for ZIKV disease in the human retina. Interestingly, the retinopathy in this case occurred simultaneously with post-viral peripheral neuropathy, and so the two conditions could share common pathophysiological features.
4. Conclusions
Clinicians should be aware that patients with recent ZIKV infection, including those who present with post-infection neurological symptoms, may harbor retinal changes involving the inner retinal vasculature. These changes have the potential to impact vision and should be monitored closely. These data expand the known spectrum of ocular manifestations that could be associated with Zika virus infection, adding the inner retinal vasculature as a possible locus of disease manifestation in addition to the well-described outer retinal effects of this condition.
Acknowledgements and disclosures
Funding
No funding or grant support.
Conflict of interest
The following authors have no financial disclosures: MSS, MCM, RO, AR, RBJ, WNM.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.De Paula Freitas B., De Oliveira Dias J.R., Prazeres J. Ocular findings in infants with microcephaly associated with presumed zika virus congenital infection in Salvador. Brazil JAMA Ophthalmol. 2016;134(5):529–535. doi: 10.1001/jamaophthalmol.2016.0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Furtado J.M., Espósito D.L., Klein T.M., Teixeira-Pinto T., Da Fonseca B.A. Uveitis associated with zika virus infection. N Engl J Med. 2016;375(4):394–396. doi: 10.1056/NEJMc1603618. [DOI] [PubMed] [Google Scholar]
- 3.Parke D.W., 3rd, Almeida D.R., Albini T.A., Ventura C.V., Berrocal A.M., Mittra R.A. Serologically confirmed Zika-related unilateral acute maculopathy in an adult. Ophthalmology. 2016 Nov;123(11):2432–2433. doi: 10.1016/j.ophtha.2016.06.039. [DOI] [PubMed] [Google Scholar]
- 4.Fontes B.M. Zika virus-related hypertensive iridocyclitis. Arq Bras Oftalmol. 2016;79(1):63. doi: 10.5935/0004-2749.20160020. [DOI] [PubMed] [Google Scholar]
- 5.Kodati S., Palmore T.N., Spellman F.A., Cunningham D., Weistrop B., Sen H.N. Bilateral posterior uveitis associated with Zika virus infection. Lancet. 2017 Jan 7;389(10064):125–126. doi: 10.1016/S0140-6736(16)32518-1. [DOI] [PubMed] [Google Scholar]
- 6.Wong C.W., Ng S.R., Cheung C.M., Wong T.Y., Mathur R. Zika-related maculopathy. Retin Cases Brief Rep. 2017 Feb 17 doi: 10.1097/ICB.0000000000000552. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Henry C.R., Al-Attar L., Cruz-Chacon A.M., Davis J.L. Chorioretinal lesions presumed secondary to Zika virus infection in an immunocompromised adult. JAMA Ophthalmol. 2017;135(4):386–389. doi: 10.1001/jamaophthalmol.2017.0098. [DOI] [PubMed] [Google Scholar]