Abstract
It has long been accepted that mitochondrial function and morphology is affected in Parkinson’s disease, and that mitochondrial function can be directly related to its morphology. So far, mitochondrial morphological alterations studies, in the context of this neurodegenerative disease, have been performed through microscopic methodologies. The goal of the present work is to address if the modifications in the mitochondrial-shaping proteins occurring in this disorder have implications in other cellular pathways, which might constitute important pathways for the disease progression. To do so, we conducted a novel approach through a thorough exploration of the available proteomics-based studies in the context of Parkinson’s disease. The analysis provided insight into the altered biological pathways affected by changes in the expression of mitochondrial-shaping proteins via different bioinformatic tools. Unexpectedly, we observed that the mitochondrial-shaping proteins altered in the context of Parkinson’s disease are, in the vast majority, related to the organization of the mitochondrial cristae. Conversely, in the studies that have resorted to microscopy-based techniques, the most widely reported alteration in the context of this disorder is mitochondria fragmentation. Cristae membrane organization is pivotal for mitochondrial ATP production, and changes in their morphology have a direct impact on the organization and function of the oxidative phosphorylation (OXPHOS) complexes. To understand which biological processes are affected by the alteration of these proteins we analyzed the binding partners of the mitochondrial-shaping proteins that were found altered in Parkinson’s disease. We showed that the binding partners fall into seven different cellular components, which include mitochondria, proteasome, and endoplasmic reticulum (ER), amongst others. It is noteworthy that, by evaluating the biological process in which these modified proteins are involved, we showed that they are related to the production and metabolism of ATP, immune response, cytoskeleton alteration, and oxidative stress, amongst others. In summary, with our bioinformatics approach using the data on the modified proteins in Parkinson’s disease patients, we were able to relate the alteration of mitochondrial-shaping proteins to modifications of crucial cellular pathways affected in this disease.
Keywords: Parkinson’s disease, proteomics, bioinformatics, biological processes, mitochondria
1. Introduction
Mitochondria are pivotal organelles for several cellular functions, namely, the production of ATP through oxidative phosphorylation, the regulation of the Krebs cycle, fatty acid metabolism, gluconeogenesis, heme-synthesis, calcium and redox homeostasis, cell signaling, and the amplification of apoptosis [1]. They are highly dynamic organelles, as they can change their shape in response to cellular stimuli by fusion and fission processes and by their movement along the cellular cytoskeleton [2]. Alterations of mitochondria morphology can significantly influence several functions of the cellular metabolism, not only related to energy production but also in communication with the cytosol and the import and export of proteins, lipids, solutes, and metabolites or even the cytosol protection from possible harmful effects of certain mitochondrial components [3]. Mitochondria dynamic processes are of utmost importance for the mitochondrial growth rate, their redistribution within the cell, and for the maintenance of healthy mitochondria and proper functioning hence their alterations are frequently associated with different pathological conditions [4].
Parkinson’s disease is a highly debilitating condition, being a common neurodegenerative disease, and more than 10 million people worldwide are affected by this disease [5]. Currently, its etiology is not fully unraveled; however, evidences point to the importance of mitochondria in its pathobiology. Clinical features include mainly motor-based dysfunctions such as bradykinesia, resting tremor, or cogwheel rigidity [6]. Those features are a consequence of the loss of dopaminergic (DA) neurons in the substantia nigra (SN). The association between mitochondrial dysfunction and the pathobiology of Parkinson’s disease was first described in 1989. By using post mortem tissue from human patients, a functional deficiency was found on the mitochondrial Complex I from the respiratory chain [7,8]. Accumulating evidence shows the occurrence of mitochondria fragmentation in the context of different models of the pathology. Furthermore, alteration of the expression levels of different proteins linked to Parkinson´s disease (e.g., PINK1, Parkin, or DJ-1) are known to induce mitochondria fragmentation in DA neurons [9,10]. Recently, it was observed that alterations of the mitochondrial morphology can be related to their functional state and new tools were consequently designed to analyze mitochondrial shape and predict mitochondrial function [11].
Interestingly, several hypotheses for the specific loss of the DA neurons from the SN are also related to the vulnerability associated with the mitochondria of these neurons [12]. It has been suggested that DA neurons from the SN are more susceptible to oxidative stress due to the production of reactive oxygen species (ROS) during dopamine degradation, and these neurons present fewer amounts of antioxidants than other DA neurons within the brain [12]. They have very long axons in which mitochondria travel and also fragment to be able to accommodate within the synaptic terminals. Besides, it is known that DA neurons from the SN present lower mitochondria mass in the soma than in the dendrites, indicating that alterations of either fragmentation or movement along the cytoskeleton might have a bigger impact on these neurons [12]. Additionally, most of the substances that are used to model the disease directly target the mitochondria and induce the specific degeneration of the DA neurons.
In this study we made a thorough literature search to identify the mitochondrial proteins involved in controlling mitochondrial morphology that are differentially expressed in Parkinson’s disease. The altered biological pathways that might be affected by changes in the expression of these mitochondrial-shaping proteins in Parkinson’s disease were identified and analyzed. Considerations were made to better understand the biological mechanisms involved in this debilitating disease.
2. Methods
Literature Search
For the compilation of the mitochondrial proteins involved in controlling mitochondrial morphology (Table 1), two independent users performed a search on PubMed, Science Direct, and Google up to 7 July 2017 using the following keywords in separate queries: “mitochondrial morphology”, “mitochondrial shape”, “mitochondrial organization”, “mitochondrial fusion”, “mitochondrial fission”, and “mitochondrial dynamics”. Only Homo sapiens proteins were gathered. The corresponding gene name and synonyms were collected in Table 1 by searching at the Universal Protein Resource (UniProt) databases [13].
Table 1.
List of mitochondrial-shaping proteins.
| Gene Name (with Synonyms) | Protein Name | Function | Localization | Shaping Function | References |
|---|---|---|---|---|---|
| APOO, FAM121B, MIC23, MIC26, My025, UNQ1866/PRO4302 | MICOS Complex subunit MIC26 (Apolipoprotein O) (MICOS Complex subunit MIC23) (Protein FAM121B) | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | IMM | Cristae shape | [14,15,16] |
| APOOL, CXorf33, FAM121A, MIC27, UNQ8193/PRO23204 | MICOS Complex subunit MIC27 (Apolipoprotein O-like) (Protein FAM121A) | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | IMM | Cristae shape | [14,15,17,18] |
| ATP5A1, ATP5B, ATP5C1, ATP5D, ATP5E, ATP5F1, ATP5G1, ATP5G2, ATP5G3, ATP5H, ATP5I, ATP5J, ATP5J2, ATP5L, ATP5O, MT-ATP6, MT-ATP8 | ATP synthase | ATP production | IMM | Cristae shape | [3,15,19] |
| ATPIF1, ATPI | ATPase inhibitor, mitochondrial (Inhibitor of F(1)F(o)-ATPase) (IF(1)) (IF1) | ATP production regulation | Matrix | Cristae shape | [3,20] |
| BAK1, BAK, BCL2L7, CDN1 | Bcl-2 homologous antagonist/killer (Apoptosis regulator BAK) | Promotes apoptosis | OMM | OMM permeabilization | [3,21] |
| BAX, BCL2L4 | Apoptosis regulator BAX | Accelerates apoptosis | OMM | OMM permeabilization | [3,19,21,22] |
| BCL2 | Apoptosis regulator Bcl-2 | Promotes cell survival | OMM | OMM permeabilization | [3,22] |
| BCL2A1, BCL2L5, BFL1, GRS, HBPA1 | Bcl-2-related protein A1 (A1-A) (Hemopoietic-specific early response protein) (Protein BFL-1) | Promotes cell survival | OMM | Not clear function | [23,24] |
| BCL2L11, BIM | Bcl-2-like protein 11 (Bcl2-L-11) (Bcl2-interacting mediator of cell death) | Induces apoptosis and anoikis | IMM | Cristae remodeling | [25,26] |
| BID | BH3-interacting domain death agonist | The major proteolytic product p15 BID allows the release of cytochrome c | IMM | Cristae remodeling | [25,27] |
| BIK, NBK | Bcl-2-interacting killer (Apoptosis inducer NBK) (BIP1) (BP4) | Promotes apoptosis | IMM | Cristae remodeling | [25,28] |
| CHCHD3, MIC19, MINOS3 | MICOS Complex subunit MIC19 (Coiled-coil-helix-coiled-coil-helix domain-containing protein 3) | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | IMM | Cristae shape | [14,16,18] |
| COA3, CCDC56, MITRAC12, HSPC009 | Cytochrome c oxidase assembly factor 3 homolog, mitochondrial (Coiled-coil domain-containing protein 56) (Mitochondrial translation regulation assembly intermediate of cytochrome c oxidase protein of 12 kDa) | Core component of the MITRAC (mitochondrial translation regulation assembly intermediate of cytochrome c oxidase) Complex, which regulates cytochrome c oxidase assembly. | IMM | Cytochrome c oxidase | [29,30] |
| COX4I1, COX4I2, COX5A, COX5B, COX6A1, COX6A2, COX6B1, COX6B2, COX6C, COX7A1, COX7A2, COX7B, COX7B2, COX7C, COX8A, COX8C, MT-CO1, MT-CO2, MT-CO3 | Mitochondrial Complex IV: cytochrome c oxidase subunits | ATP production | IMM | Cristae shape | [18] |
| CYC1, MT-CYB, UQCR10, UQCR11, UQCRB, UQCRC1, UQCRC2, UQCRFS1, UQCRH, UQCRQ | Mitochondrial Complex III: ubiquinol-cytochrome c reductase Complex subunits (UQCR) | ATP production | IMM | Cristae shape | [18] |
| DNAJC19, TIM14, TIMM14 | Mitochondrial import inner membrane translocase subunit TIM14 (DnaJ homolog subfamily C member 19) | Probable component of the PAM Complex, a Complex required for the translocation of transit peptide-containing proteins from the inner membrane into the mitochondrial matrix in an ATP-dependent manner | IMM | Crista shape | [15,31,32] |
| DNM1L, DLP1, DRP1 | Dynamin-1-like protein (EC 3.6.5.5) (Dnm1p/Vps1p-like protein) (DVLP) (Dynamin family member proline-rich carboxyl-terminal domain less) (Dymple) (Dynamin-like protein) (Dynamin-like protein 4) (Dynamin-like protein IV) (HdynIV) (Dynamin-related protein 1) | Mitochondrial and peroxisome division | OMM and cytosol | Fission | [3,18,22] |
| DNM2, DYN2 | Dynamin-2 (EC 3.6.5.5) | Microtubule-associated force-producing protein involved in producing microtubule bundles and able to bind and hydrolyze GTP | Cytosol | Fission | [4,33] |
| FIS1, TTC11, CGI-135 | Mitochondrial fission 1 protein (FIS1 homolog) (hFis1) (Tetratricopeptide repeat protein 11) (TPR repeat protein 11) | Mitochondrial fragmentation | OMM | Fission | [3,19,22] |
| FUNDC1 | FUN14 domain-containing protein 1FUN14 domain-containing protein 1 | Mitophagy | OMM | Fission | [29,34,35,36] |
| GDAP1 | Ganglioside-induced differentiation-associated protein 1 | Mitochondrial fission | OMM | Fission | [1,19,22] |
| hfzo1 | Mitochondrial transmembrane GTPase Fzo-1 | FUNDC1 mediates highly selective mitochondrial clearance under hypoxic conditions without impacting general autophagy | OMM | Fusion | [19] |
| IMMT, HMP, MIC60, MINOS2, PIG4, PIG52 | MICOS Complex subunit MIC60(Cell proliferation-inducing gene 4/52 protein) (Inner mitochondrial membrane protein) (Mitofilin) (p87/89) | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | IMM | Cristae shape | [15,16,18,19,37] |
| INF2, C14orf151, C14orf173 | Inverted formin-2 (HBEBP2-binding protein C) | Severs actin filaments and accelerates their polymerization and depolymerization | Cytosol | Mitochondrial constriction | [29,38] |
| LETM1 | Mitochondrial proton/calcium exchanger protein (Leucine zipper-EF-hand-containing transmembrane protein 1) | Mitochondrial proton/calcium antiporter that mediates proton-dependent calcium efflux from mitochondria | IMM | Fission | [1,22,39] |
| MARCH5, RNF153 | E3 ubiquitin-protein ligase MARCH5 (EC 2.3.2.27) (Membrane-associated RING finger protein 5) (Membrane-associated RING-CH protein V) (MARCH-V) (Mitochondrial ubiquitin ligase) (MITOL) (RING finger protein 153) (RING-type E3 ubiquitin transferase MARCH5) | Membrane-bound E3 ligase for mitochondrial morphology control | OMM | Fission | [1,19] |
| MAVS, IPS1, KIAA1271, VISA | Mitochondrial antiviral-signaling protein (MAVS) (CARD adapter inducing interferon beta) (Cardif) (Interferon beta promoter stimulator protein 1) (IPS-1) (Putative NF-kappa-B-activating protein 031N) (Virus-induced-signaling adapter) (VISA) | Required for innate immune response against viruses | OMM | Fusion | [22,40] |
| MCL1, BCL2L3 | Induced myeloid leukemia cell differentiation protein Mcl-1 (Bcl-2-like protein 3) (Bcl2-L-3) (Bcl-2-related protein EAT/mcl1) (mcl1/EAT) | Regulation of apoptosis | IMM and OMM | Cristae shape (IMM isoform) | [18,29,41,42] |
| MFF, C2orf33, AD030, AD033, GL004 | Mitochondrial Fission Factor | Mitochondrial and peroxisome division | OMM | Fission | [3,19] |
| MFN1 | Mitofusin-1 (EC 3.6.5.-) (Fzo homolog) (Transmembrane GTPase MFN1) | Mitochondrial fusion | OMM | Fusion | [18,22,43] |
| MFN2, CPRP1, KIAA0214 | Mitofusin-2 (EC 3.6.5.-) (Transmembrane GTPase MFN2) | Regulates mitochondrial clustering and fusion | OMM | Fusion | [18,22,43] |
| MIC13, C19orf70, QIL1 | MICOS Complex subunit MIC13 (Protein P117) | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | IMM | Cristae shape | [15,18] |
| MIEF1, MID51, SMCR7L | Mid51/Mief, mitochondrial dynamics proteins of 51 | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | OMM | Fission | [3,19] |
| MIEF2, MID49, SMCR7 | Mitochondrial dynamics protein MID49 (Mitochondrial dynamics protein of 49 kDa) (Mitochondrial elongation factor 2) (Smith-Magenis syndrome chromosomal region candidate gene 7 protein) | Component of the MICOS Complex, a large protein Complex of the inner mitochondrial membrane that plays crucial roles in the maintenance of crista junctions, inner membrane architecture, and formation of contact sites to the outer membrane | OMM | Fission | [3,19] |
| MIGA1, FAM73A | Mitoguardin 1 (Protein FAM73A) | Regulator of mitochondrial fusion | OMM | Fusion | [4,44] |
| MIGA2, C9orf54, FAM73B, PSEC0112 | Mitoguardin 2 (Protein FAM73B) | Regulator of mitochondrial fusion | OMM | Fusion | [4,44] |
| MINOS1, C1orf151, MIC10 | MICOS Complex subunit MIC10 (Inner mitochondrial membrane organizing system protein 1) | Maintenance of cristae junctions, inner membrane architecture, and formation of contact sites to the outer membrane | IMM | Cristae shape | [15,18] |
| MTFP1, MTP18, HSPC242, My022 | Mitochondrial fission process protein 1(Mitochondrial 18 kDa protein) (MTP18) | Involved in the mitochondrial division probably by regulating membrane fission | IMM | Fission | [1,22,45] |
| MUL1, C1orf166, GIDE, MAPL, MULAN, RNF218 | Mitochondrial ubiquitin ligase activator of NFKB 1 (EC 2.3.2.27) (E3 SUMO-protein ligase MUL1) (E3 ubiquitin-protein ligase MUL1) (Growth inhibition and death E3 ligase) (Mitochondrial-anchored protein ligase) (MAPL) (Putative NF-kappa-B-activating protein 266) (RING finger protein 218) (RING-type E3 ubiquitin transferase NFKB 1) | Ubiquitin ligase activity | OMM | Fusion | [19,29] |
| NFE2L2, NRF2 | Nuclear factor erythroid 2-related factor 2 (NF-E2-related factor 2) (NFE2-related factor 2) (HEBP1) (Nuclear factor, erythroid derived 2, like 2) | Transcription activator that binds to antioxidant response (ARE) elements in the promoter regions of target genes | Cytosol | Fusion | [29,46,47] |
| NRF1 | Nuclear respiratory factor 1 (NRF-1) (Alpha palindromic-binding protein) (Alpha-pal) | Transcription factor implicated in the control of nuclear genes required for respiration, heme biosynthesis, and mitochondrial DNA transcription and replication | Cytosol | Fission | [29,46,48,49] |
| OMA1, MPRP1 | Metalloendopeptidase OMA1, mitochondrial (EC 3.4.24.-) (Metalloprotease-related protein 1) (MPRP-1) (Overlapping with the m-AAA protease 1 homolog) | Metalloprotease that is part of the quality control system in the inner membrane of mitochondria | IMM | Fusion | [1,19] |
| OPA1, KIAA0567 | Dynamin-like 120 kDa protein, mitochondrial (EC 3.6.5.5) (Optic atrophy protein 1) (Cleaved into: Dynamin-like 120 kDa protein, form S1) | Opa1 mediates dynamics changes in cristae morphology that correlate with the metabolic state of the organelle | IMM | Cristae shape, fusion | [1,3,15,18,22,50] |
| PARL, PSARL, PRO2207 | Presenilins-associated rhomboid-like protein, mitochondrial (EC 3.4.21.105) (Mitochondrial intramembrane cleaving protease PARL) (Cleaved into: P-beta (Pbeta)) | Required for the control of apoptosis | IMM | Mitochondrial morphology | [1,51] |
| PGAM5 | Serine/threonine-protein phosphatase PGAM5, mitochondrial (EC 3.1.3.16) (Bcl-XL-binding protein v68) (Phosphoglycerate mutase family member 5) | Displays phosphatase activity for serine/threonine residues, as well as dephosphorylates and activates MAP3K5 kinase | OMM | Fission | [1,29,52] |
| PHB | Prohibitin | Prohibitin inhibits DNA synthesis; it has a role in regulating proliferation | IMM | Cristae shape | [1,15,18,31,53] |
| PHB2, BAP, REA | Prohibitin-2 (B-cell receptor-associated protein BAP37) (D-prohibitin) (Repressor of estrogen receptor activity) | Acts as a mediator of transcriptional repression by nuclear hormone receptors via the recruitment of histone deacetylases (by similarity); functions as an estrogen receptor (ER)-selective coregulator that potentiates the inhibitory activities of antiestrogens and represses the activity of estrogens | IMM | Cristae shape | [1,15,18] |
| PINK1 | Serine/threonine-protein kinase PINK1, mitochondrial (EC 2.7.11.1) (BRPK) (PTEN-induced putative kinase protein 1) | Protects against mitochondrial dysfunction during cellular stress by phosphorylating mitochondrial proteins | OMM | Fission | [1,54] |
| PLD6 | Mitochondrial cardiolipin hydrolase (EC 3.1.-.-) (Choline phosphatase 6) (Mitochondrial phospholipase) (MitoPLD) (Phosphatidylcholine-hydrolyzing phospholipase D6) (Phospholipase D6) (PLD 6) (Protein zucchini homolog) | Proposed to act as a cardiolipin hydrolase to generate phosphatidic acid at the mitochondrial surface | OMM | Fusion | [4,19,22,45] |
| PPARGC1A, LEM6, PGC1, PGC1A, PPARGC1 | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1-alpha) (PPAR-gamma coactivator 1-alpha) (PPARGC-1-alpha) (Ligand effect modulator 6) | Transcriptional coactivator for steroid receptors and nuclear receptors | Cytoplasm and nucleus | Fusion | [29,49,55] |
| PPARGC1B, PERC, PGC1, PGC1B, PPARGC1 | Peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC-1-beta) (PPAR-gamma coactivator 1-beta) (PPARGC-1-beta) (PGC-1-related estrogen receptor alpha coactivator) | Plays the role of stimulator of transcription factors and nuclear receptors activities | Nucleus | Fusion | [29,55,56] |
| PRELID1, PRELI, CGI-106, SBBI12 | PRELI domain-containing protein 1, mitochondrial (25 kDa protein of relevant evolutionary and lymphoid interest) (Px19-like protein) | Involved in the modulation of the mitochondrial apoptotic pathway by ensuring the accumulation of cardiolipin (CL) in mitochondrial membranes | Intermembrane space | Fission | [57,58] |
| PRKN, PARK2 | E3 ubiquitin-protein ligase parkin (Parkin) (EC 2.3.2.-) (Parkin RBR E3 ubiquitin-protein ligase) (Parkinson juvenile disease protein 2) (Parkinson disease protein 2) | Functions within a multiprotein E3 ubiquitin ligase Complex, catalyzing the covalent attachment of ubiquitin moieties onto substrate proteins | Cytosol and mitochondria | Fission | [1,54,59,60] |
| ROMO1, C20orf52 | Reactive oxygen species modulator 1(ROS modulator 1) (Epididymis tissue protein Li 175) (Glyrichin) (Mitochondrial targeting GxxxG motif protein) (MTGM) (Protein MGR2 homolog) | Induces the production of reactive oxygen species (ROS), which are necessary for cell proliferation | IMM | Fusion | [29,61] |
| SAMM50, SAM50, CGI-51, TRG3 | Sorting and assembly machinery component 50 homolog (Transformation-related gene 3 protein) (TRG-3) | Plays a crucial role in the maintenance of the structure of mitochondrial cristae and the proper assembly of the mitochondrial respiratory chain Complexes | OMM | Cristae shape | [18] |
| SH3GLB1, KIAA0491, CGI-61 | Endophilin-B1 (Bax-interacting factor 1) (Bif-1) (SH3 domain-containing GRB2-like protein B1) | Outer mitochondrial dynamics | OMM | OMM permeability | [1,22,62] |
| SH3GLB2, KIAA1848, PP578 | Endophilin-B2 (SH3 domain-containing GRB2-like protein B2) | Mitophagy | Cytosol | Fission | [63] |
| SLC25A10, DIC | Mitochondrial dicarboxylate carrier (Solute carrier family 25 member 10) | Involved in the translocation of malonate, malate, and succinate in exchange for phosphate, sulfate, sulfite, or thiosulfate across the inner mitochondrial membrane | IMM | Cristae shape | [18,50] |
| SLC25A11, SLC20A4 | Mitochondrial 2-oxoglutarate/malate carrier protein (OGCP) (Solute carrier family 25 member 11) | Catalyzes the transport of 2-oxoglutarate across the inner mitochondrial membrane in an electroneutral exchange for malate or other dicarboxylic acids, and plays an important role in several metabolic processes, including the malate-aspartate shuttle, the oxoglutarate/isocitrate shuttle, in gluconeogenesis from lactate, and in nitrogen metabolism | IMM | Cristae shape | [18,50] |
| SLC25A12, ARALAR1 | Calcium-binding mitochondrial carrier protein Aralar1 (Mitochondrial aspartate glutamate carrier 1) (Solute carrier family 25 member 12) | Catalyzes the calcium-dependent exchange of cytoplasmic glutamate with mitochondrial aspartate across the inner mitochondrial membrane; may have a function in the urea cycle | IMM | Cristae shape | [18,50] |
| SLC25A13, ARALAR2 | Calcium-binding mitochondrial carrier protein Aralar2 (Citrin) (Mitochondrial aspartate glutamate carrier 2) (Solute carrier family 25 member 13) | Catalyzes the calcium-dependent exchange of cytoplasmic glutamate with mitochondrial aspartate across the inner mitochondrial membrane; may have a function in the urea cycle | IMM | Cristae shape | [18,50] |
| SLC25A38 | Solute carrier family 25 member 38, Appoptosin | Mitochondrial import machinery | IMM | Fusion | [29,64] |
| SMAD2, MADH2, MADR2 | Mothers against decapentaplegic homolog 2 (MAD homolog 2) (Mothers against DPP homolog 2) (JV18-1) (Mad-related protein 2) (hMAD-2) (SMAD family member 2) (SMAD 2) (Smad2) (hSMAD2) | Receptor-regulated SMAD (R-SMAD) that is an intracellular signal transducer and transcriptional modulator activated by TGF-beta (transforming growth factor) and activin type 1 receptor kinases | Cytosol | Fusion | [29,65] |
| SPG7, CAR, CMAR, PGN | Paraplegin (EC 3.4.24.-) (Cell matrix adhesion regulator) (Spastic paraplegia 7 protein) | ATP-dependent zinc metalloprotease | IMM | Cristae shape | [18] |
| SPG7, CAR, CMAR, PGN | Paraplegin (EC 3.4.24.-) (Cell matrix adhesion regulator) (Spastic paraplegia 7 protein) | ATP-dependent zinc metalloprotease | IMM | Fusion | [1,22,51] |
| STOML2, SLP2, HSPC108 | Stomatin-like protein 2, mitochondrial(SLP-2) (EPB72-like protein 2) (Paraprotein target 7) (Paratarg-7) | Mitochondrial protein that probably regulates the biogenesis and the activity of mitochondria; stimulates cardiolipin biosynthesis, binds cardiolipin-enriched membranes where it recruits and stabilizes some proteins including prohibitin, and may therefore act in the organization of functional microdomains in mitochondrial membranes | IMM | Cristae shape/Stabilize IM structure | [15,18] |
| SYNJ2, KIAA0348 | Synaptojanin-2(EC 3.1.3.36) (Synaptic inositol 1,4,5-trisphosphate 5-phosphatase 2) | Membrane trafficking and signaling transduction | Cytosol | Mitochondrial aggregation | [66] |
| TAZ, EFE2, G4.5 | Tafazzin (Protein G4.5) | Some isoforms may be involved in cardiolipin (CL) metabolism | OMM | Cristae shape | [15,16,67,68] |
| TFAM, TCF6, TCF6L2 | Transcription factor A, mitochondrial (mtTFA) (Mitochondrial transcription factor 1) (MtTF1) (Transcription factor 6) (TCF-6) (Transcription factor 6-like 2) | Binds to the mitochondrial light strand promoter and functions in mitochondrial transcription regulation | Matrix | Mitochondrial biogenesis | [29,46] |
| TRAK1, KIAA1042, OIP106 | Trafficking kinesin-binding protein 1 (106 kDa O-GlcNAc transferase-interacting protein) | Organelle trafficking | OMM and cytosol | Fusion | [1,4,19] |
| TRAK2, ALS2CR3, KIAA0549 | Trafficking kinesin-binding protein 2 (Amyotrophic lateral sclerosis 2 chromosomal region candidate gene 3 protein) | Organelle trafficking | OMM and cytosol | Fusion | [1,4,19] |
| UQCC3, C11orf83, UNQ655/PRO1286 | Ubiquinol-cytochrome-c reductase Complex assembly factor 3 | Required for the assembly of the ubiquinol-cytochrome c reductase Complex (mitochondrial respiratory chain Complex III or cytochrome b-c1 Complex), mediating cytochrome b recruitment and probably stabilization within the Complex | IMM | Cristae shape | [18,69] |
| VAT1 | Synaptic vesicle membrane protein VAT-1 homolog (EC 1.-.-.-) (Mitofusin-binding protein) (Protein MIB) | Negatively regulates mitochondrial fusion | OMM | Fusion | [1,19,22,70] |
| YME1L1, FTSH1, YME1L, UNQ1868/PRO4304 | ATP-dependent zinc metalloprotease YME1L1 (EC 3.4.24.-) (ATP-dependent metalloprotease FtsH1) (Meg-4) (Presenilin-associated metalloprotease) (PAMP) (YME1-like protein 1) | Putative ATP-dependent protease; plays a role in mitochondrial organization and mitochondrial protein metabolism, including the degradation of PRELID1 and OPA1 | IMM | Cristae shape | [19,58] |
To collect the information from proteomic-based studies of the differentially expressed proteins in the context of Parkinson’s disease, a search on PubMed and Web of Science (version v5.24) (up to 28 July 2017) was performed using the following keywords: “Parkinson’s disease mass spectrometry”, “Parkinson’s disease proteomics”. Studies working with samples from human patients and cellular models (from cell lines of human origin) were used to build the Supplementary Table S1. Three experienced reviewers selected the list of articles relevant for data extraction, taking into consideration only the studies that match the following criteria: proteomics studies, with information on differentially expressed proteins related to control conditions, employing samples either from human patients or cellular models (using cell lines of human origin).
Mitochondrial-shaping proteins were crossed with the proteins that have been found to be altered in Parkinson’s disease using the respective gene names in Venny web tool (v.2.1.0) [71]. The gene name of the common proteins (proteins that are involved in mitochondrial shape and are modified in Parkinson’s disease) were further used to determine the binding partners in HIPPIE web tool [72].
Network analysis was performed using the Cytoscape software (version v3.5.1) (Cytoscape Consortium, San Diego, CA, US)) with the plugins ClueGo (version v2.3.2) and Cluepedia (version v1.3.2). We used ClueGO’s default settings: merge redundant groups with >50.0% overlap; the minimum GO level used was 3 and the maximum GO level was 8; statistical test used was “Enrichment/Depletion (Two-sided hypergeometric test)”; Kappa Score Threshold was 0.4; and number of genes was set at 2 with a minimum percentage at 4.0.
3. Results
3.1. Differentially Expressed Mitochondrial Proteins Associated with Parkinson’s Disease
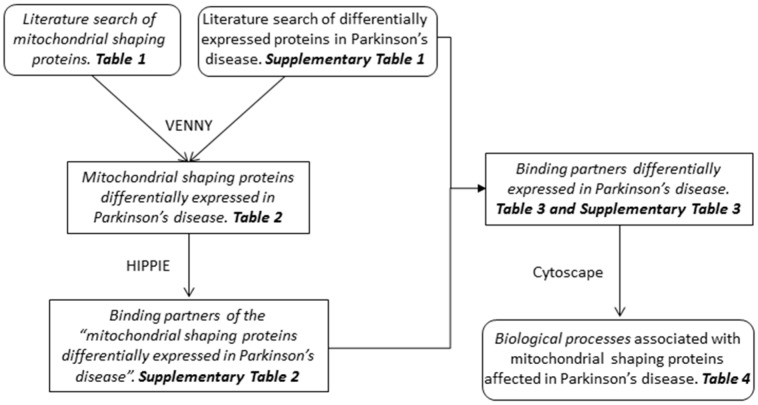
The interplay between mitochondria function and Parkinson’s disease was first described as a deficiency of the mitochondrial respiratory chain Complex I [7,8]. Alterations of the mitochondrial shape have been related to their functional state [11] and, in the past few years, an increasing number of reports have shown alterations of mitochondrial morphology in the context of Parkinson’s disease [73,74,75,76]. Mitochondrial morphology is tightly regulated by the combined action of proteins involved in fusion, fission, and movement along the cytoskeleton [3]. In this study we aimed to integrate the proteins related to mitochondria morphology with Parkinson’s disease pathology. The flowchart followed in the present work is represented in Figure 1. The complete list of mitochondrial proteins that have been described to play a role in the control and regulation of mitochondrial morphology is depicted in Table 1. To integrate the alterations of the mitochondrial dynamics in the context of the pathobiology of Parkinson’s disease, a literature search for proteomics-based studies in this disorder, that used samples from patients or cellular models (cell lines of human origin) (Supplementary Table S1), was performed. These proteins were then cross-referenced with the mitochondrial-shaping proteins listed in Table 1 (Figure 1).
Figure 1.
Flowchart showing the main steps used to identify the biological processes related to the mitochondrial-shaping proteins affected in Parkinson’s disease.
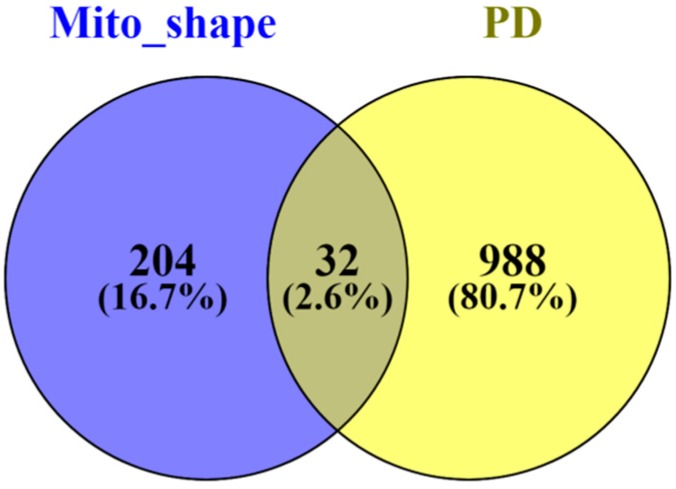
From this analysis, 32 different gene names (Figure 2), related to mitochondrial morphology, were found to be modified in the context of Parkinson’s disease, which correspond to 22 different proteins (Table 2). The vast majority of these mitochondrial proteins are related to the cristae morphology (82%), whereas only 9% are reported to be involved in the fusion and fission processes.
Figure 2.
Venn diagram displaying the comparison of the number of the proteins found differentially expressed in the context of Parkinson’s disease (Supplementary Table S1) and the mitochondrial-shaping proteins described in the literature (Table 1). The Venn diagram was constructed using the Venny 2.1 software [71]. PD—Parkinson’s disease.
Table 2.
List of mitochondrial-shaping proteins found to be modified in Parkinson’s disease.
| Gene Symbol (bioDBnet) | Name | Mito_Shaping |
|---|---|---|
| APOO, FAM121B, MIC23, MIC26, My025, UNQ1866/PRO4302 | MICOS Complex subunit MIC26 (Apolipoprotein O) (MICOS Complex subunit MIC23) (Protein FAM121B) | Cristae shape |
| ATP5A1, ATP5A, ATP5AL2, ATPM | ATP synthase subunit alpha, mitochondrial | Cristae shape |
| ATP5B, ATPMB, ATPSB | ATP synthase subunit beta, mitochondrial | Cristae shape |
| ATP5H | ATP synthase subunit d | Cristae shape |
| ATP5I | ATP synthase subunit e, mitochondrial | Cristae shape |
| SAMM50, SAM50, CGI-51, TRG3 | Sorting and assembly machinery component 50 homolog (Transformation-related gene 3 protein) (TRG-3) | Cristae shape |
| COX4I1, COX4 | Cytochrome c oxidase subunit 4 isoform 1, mitochondrial (Cytochrome c oxidase polypeptide IV) (Cytochrome c oxidase subunit IV isoform 1) (COX IV-1) | Cristae shape |
| COX5A | Cytochrome c oxidase subunit 5A, mitochondrial (Cytochrome c oxidase polypeptide Va) | Cristae shape |
| COX6C | Cytochrome c oxidase subunit 6C (Cytochrome c oxidase polypeptide VIc) | Cristae shape |
| COX7C | Cytochrome c oxidase subunit 7C, mitochondrial (Cytochrome c oxidase polypeptide VIIc) | Cristae shape |
| MFN2, CPRP1, KIAA0214 | Mitofusin-2 (EC 3.6.5.-) (Transmembrane GTPase MFN2) | Fusion |
| DNM1L | Dynamin-like protein | Fission |
| IMMT | Mitofilin | Cristae shape |
| MT-CO1 | Cytochrome c oxidase polypeptide I | Cristae shape |
| PHB | Prohibitin | Cristae shape |
| PHB2 | Prohibitin-2 | Cristae shape |
| SH3GLB2 | SH3-containing protein SH3GLB2 | Fission |
| SLC25A13 | Calcium-binding mitochondrial carrier protein Aralar2 | Cristae shape |
| UQCRB, UQBP | Cytochrome b-c1 Complex subunit 7 (Complex III subunit 7) (Complex III subunit VII) (QP-C) (Ubiquinol-cytochrome c reductase Complex 14 kDa protein) | Cristae shape |
| UQCRFS1 | Ubiquinol cytochrome c reductase iron–sulfur subunit | Cristae shape |
| UQCRH | Cytochrome b-c1 Complex subunit 6, mitochondrial | Cristae shape |
| VAT1 | Synaptic vesicle membrane protein VAT-1 homolog | Fusion |
Curiously, in Parkinson’s disease the most reported mitochondrial morphology alterations are associated with mitochondrial fragmentation and movement impairment [74,77]. Mechanisms proposed for these alterations include: the alteration of the interaction between mitochondria and the motor complexes, and mitophagy impairment [78,79,80,81,82,83].
In our analysis, the fusion- and fission-related proteins found to be altered were Mitofusin-2 and the synaptic vesicle membrane protein VAT-1 homolog, as well as the dynamin-like protein (Drp1) and the SH3-containing protein SH3GLB2, respectively.
Although commonly accepted as a protein involved in mitochondrial fusion, the Mitofusin-2 protein also plays a key role in Ca2+ signaling. This function is facilitated by the physical interaction between the ER and the mitochondria for the delivery of Ca2+ to the mitochondrial matrix, enabling mitochondrial signaling. Hence, Mitofusin-2 is involved in both mitochondrial morphology and crosstalk between the ER and the mitochondria [84]. In the process of mitochondrial fusion both Mitofusin-1 and -2 have been reported to contribute, and although they share a common function in this process; deficiency in Mitofusion-2, but not Mitofusin-1, has been linked to neurodegenerative diseases [85]. Interestingly, the synaptic vesicle membrane protein VAT-1 homolog was found to be negatively regulate mitochondrial fusion in cooperation with Mitofusin-2 [70].
Regarding the mitochondrial fission process, in the context of Parkinson’s disease, the role of Drp1 has been extensively recognized in mitochondrial fragmentation in different animal and cellular models preceding neuronal death [73,86,87]. This large GTPase is a cytosolic protein that, following mitochondrial fragmentation stimuli, translocates to the outer mitochondrial membrane where it assembles into large complexes in a spiral form, enabling the constriction of the mitochondria [19]. Endophilins might be involved in membrane shaping, e.g., Endophilin B2, although they have also been described to play a role in mitophagy by promoting the degradation of the inner mitochondrial membrane [63].
Nevertheless, as reported above, most of the proteins related to mitochondrial morphology that we found to be altered in the context of Parkinson’s disease are associated with the regulation of the mitochondrial cristae morphology. Interestingly, accumulating evidence shows an association between the morphology of the mitochondrial cristae and the OXPHOS complexes. This fact brings forward the idea that the formation of the supercomplexes of the respiratory chain is related to the organization of the inner mitochondrial membrane [18]. The involvement of the mitochondria in Parkinson’s disease is clear, and several indications also reveal that alterations in the balance of fission and fusion processes increase the occurrence of fragmented mitochondria. However, the data collected in the present work points to a major contribution of the modification of the mitochondrial cristae. The major drawback when studying mitochondrial morphology is the fact that many studies have employed immunofluorescence using antibodies against mitochondrial membrane proteins and subsequent observation in optical microscopes. This methodology exhibits a lack of resolution needed to visualize the morphological subtleties in the mitochondrial cristae [88]. Therefore, for the study of mitochondrial dynamics, super-resolution and immunoelectron microscopy are better options since it is then possible to visualize the inner mitochondrial compartment [88,89].
The mitochondrial contact site and the cristae-organizing system (MICOS) have been described as a multiprotein complex relevant to inner membrane architecture [1,90]. In fact, it was described that some of the MICOS subunits control the morphology of the cristae in coordination with the mitochondrial Complexes III and IV from the respiratory chain [18]. In the absence of MICOS, cristae morphology is aberrant and these respiratory chain complexes are not functional [14]. Interestingly, in our study we found that two of the MICOS core subunits were altered in the context of Parkinson’s disease (Table 2): Mitofilin [18] and Mic26 [14]. The MICOS Complex interacts with proteins of the outer mitochondrial membrane, specifically with the sorting and assembly machinery component 50 (SAM50). Its depletion has been found to affect the mitochondria ultrastructure and the loss of cristae, thus affecting the assembly of the complexes of the mitochondrial respiratory chain [91]. Curiously, the SAM50 protein expression was also found to be altered in our analysis (Table 2).
Other modified proteins retrieved in our study included proteins from the mitochondrial respiratory chain such as members of the Complex III (the cytochrome b-c1 Complex subunit, the ubiquinol cytochrome c reductase iron–sulphur subunit, and the cytochrome b-c1 Complex subunit 6) and Complex IV (the cytochrome c oxidase subunit 4, the cytochrome c oxidase subunit 5A, the cytochrome c oxidase subunit 6C, the cytochrome c oxidase subunit 7C, and the cytochrome c oxidase polypeptide I).
Pivotal for the proper architecture of the mitochondrial cristae is the protein OPA1 [3]. Alterations were found to occur in the expression of the calcium-binding mitochondrial carrier protein Aralar2 (Slc25A), which acts in conjunction with OPA1 to sense modifications of the substrate levels for energy production. Following this interaction, the cristae are narrowed and the dimerization of the ATP synthase is stimulated [18].
The mitochondrial cristae structure is not solely maintained by proteins, but also by cardiolipin lipids [18], and several cardiolipin binding proteins have been described to be present at the mitochondrial membrane, amongst them the Prohibitin protein family. Prohibitin and Prohibitin-2 appeared to be altered in the context of Parkinson’s disease in our analysis (Table 2). These proteins are known to be organized in complexes within the inner mitochondrial membrane and are important for the proper organization of the cristae morphology and mitochondrial respiration [53,92]. Moreover, these proteins are involved in the turnover of the subunits of the mitochondrial respiratory chain and participate in the assembly of the Complex IV from the respiratory chain [93,94].
There is evidence that aberrant cristae morphology affects the proper assembly of the OXPHOS complexes, but also that the lack of ATP synthase subunits impacts the morphology of the cristae [95,96]. The latter has been supported by studies showing that ATP synthase dimerization forces membrane curvature [97]. Interestingly, mitochondrial morphology also relies on the cellular energetic state since, by compromising mitochondrial membrane potential, mitochondrial fragmentation is induced [98]. In addition, dimer formation of the F1F0-ATP synthase affects mitochondrial cristae structure [95].
3.2. Binding Partners of Mitochondrial Proteins Differentially Expressed in Parkinson’s Disease
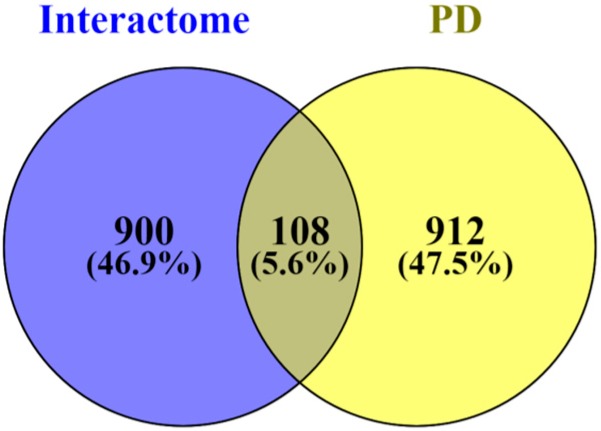
Mitochondria are organelles with important roles in many cellular processes, hence we next explored the binding partners described for the mitochondrial proteins differentially expressed in Parkinson’s disease (Table 2). Using the HIPPIE tool [72,99,100,101], we determined the complete list of binding partners, which is depicted in Supplementary Table S2 (Figure 1). This software provides information on human protein-protein interactions with high confidence scores that are due to the amount of supporting data available as well as derived from annotated information [72,99]. In total, for the 22 mitochondrial-shaping proteins altered in Parkinson’s disease, we found 1683 hints of interacting proteins. Since some of the mitochondrial-shaping proteins have interacting proteins in common, these hints correspond to 1008 different proteins. When we cross-referenced these binding partners with the list of proteins found to be modified in the context of Parkinson’s disease (Supplementary Table S1), 108 common hints were identified (Figure 3, Table 3, and Supplementary Table S3). In Supplementary Table S3, the different hints of the proteins listed in Table 3 within the different proteomics-based studies used in the present work are described.
Figure 3.
Venn diagram displaying the comparison of the number of the binding partners of the mitochondrial-shaping proteins affected in Parkinson’s disease (Table 2) and the proteins found to be differentially expressed in the context of Parkinson’s disease (Supplementary Table S1). The Venn diagram was constructed using the Venny 2.1 software [71]. PD—Parkinson’s disease.
Table 3.
List of binding partners of the mitochondrial-shaping proteins altered in Parkinson’s disease (Table 2) that are found in the list of proteins modified in the context of Parkinson’s disease (Supplementary Table S1).
| Gene Names | Protein Names |
|---|---|
| ACAD9 | Acyl-CoA dehydrogenase family member 9, mitochondrial (ACAD-9) (EC 1.3.99.-) |
| ACP2 | Lysosomal acid phosphatase (LAP) (EC 3.1.3.2) |
| ACTB | Actin, cytoplasmic 1 (Beta-actin) (Cleaved into: Actin, cytoplasmic 1, N-terminally processed) |
| ACTBL2 | Beta-actin-like protein 2 (Kappa-actin) |
| ACTN1 | Alpha-actinin-1 (Alpha-actinin cytoskeletal isoform) (F-actin cross-linking protein) (Non-muscle alpha-actinin-1) |
| ALB, GIG20, GIG42, PRO0903, PRO1708, PRO2044, PRO2619, PRO2675, UNQ696/PRO1341 | Serum albumin |
| ALDH1B1, ALDH5, ALDHX | Aldehyde dehydrogenase X, mitochondrial (EC 1.2.1.3) (Aldehyde dehydrogenase 5) (Aldehyde dehydrogenase family 1 member B1) |
| ALDOA, ALDA | Fructose-bisphosphate aldolase A (EC 4.1.2.13) (Lung cancer antigen NY-LU-1) (Muscle-type aldolase) |
| ANXA2, ANX2, ANX2L4, CAL1H LPC2D | Annexin A2 (Annexin II) (Annexin-2) (Calpactin I heavy chain) (Calpactin-1 heavy chain) (Chromobindin-8) (Lipocortin II) (Placental anticoagulant protein IV) (PAP-IV) (Protein I) (p36) |
| APOA1 | Apolipoprotein A-I (Apo-AI) (ApoA-I) (Apolipoprotein A1) (Cleaved into: Proapolipoprotein A-I (Proapo A-I); Truncated apolipoprotein A-I (Apolipoprotein A-I(1-242))) |
| ATP5A1, ATP5A, ATP5AL2, ATPM | ATP synthase subunit alpha, mitochondrial |
| ATP5B, ATPMB, ATPSB, | ATP synthase subunit beta, mitochondrial (EC 3.6.3.14) |
| ATP5H, My032 | ATP synthase subunit d, mitochondrial (ATPase subunit d) |
| ATP5I, ATP5K | ATP synthase subunit e, mitochondrial (ATPase subunit e) (Cleaved into: ATP synthase subunit e, mitochondrial, N-terminally processed) |
| BCAP31, BAP31, DXS1357E | B-cell receptor-associated protein 31 (BCR-associated protein 31) (Bap31) (6C6-AG tumor-associated antigen) (Protein CDM) (p28) |
| C1QBP, GC1QBP, HABP1, SF2P32 | Complement component 1 Q subcomponent-binding protein, mitochondrial (ASF/SF2-associated protein p32) (Glycoprotein gC1qBP) (C1qBP) (Hyaluronan-binding protein 1) (Mitochondrial matrix protein p32) (gC1q-R protein) (p33) |
| CALR, CRTC | Calreticulin (CRP55) (Calregulin) (Endoplasmic reticulum resident protein 60) (ERp60) (HACBP) (grp60) |
| CCT5, CCTE, KIAA0098 | T-complex protein 1 subunit epsilon (TCP-1-epsilon) (CCT-epsilon) |
| COX4I1, COX4 | Cytochrome c oxidase subunit 4 isoform 1, mitochondrial (Cytochrome c oxidase polypeptide IV) (Cytochrome c oxidase subunit IV isoform 1) (COX IV-1) |
| COX5A | Cytochrome c oxidase subunit 5A, mitochondrial (Cytochrome c oxidase polypeptide Va) |
| COX6C | Cytochrome c oxidase subunit 6C (Cytochrome c oxidase polypeptide VIc) |
| DDAH1, DDAH | N(G),N(G)-dimethylarginine dimethylaminohydrolase 1 (DDAH-1) (Dimethylarginine dimethylaminohydrolase 1) (EC 3.5.3.18) (DDAHI) (Dimethylargininase-1) |
| DDOST, KIAA0115, OST48 OK/SW-cl.45 | Dolichyl-diphosphooligosaccharide—protein glycosyltransferase 48 kDa subunit (DDOST 48 kDa subunit) (Oligosaccharyl transferase 48 kDa subunit) |
| DNM1L, DLP1, DRP1 | Dynamin-1-like protein (EC 3.6.5.5) (Dnm1p/Vps1p-like protein) (DVLP) (Dynamin family member proline-rich carboxyl-terminal domain less) (Dymple) (Dynamin-like protein) (Dynamin-like protein 4) (Dynamin-like protein IV) (HdynIV) (Dynamin-related protein 1) |
| DYNC1H1, DHC1, DNCH1, DNCL, DNECL, DYHC, KIAA0325 | Cytoplasmic dynein 1 heavy chain 1 (Cytoplasmic dynein heavy chain 1) (Dynein heavy chain, cytosolic) |
| EEF1A1, EEF1A, EF1A, LENG7 | Elongation factor 1-alpha 1 (EF-1-alpha-1) (Elongation factor Tu) (EF-Tu) (Eukaryotic elongation factor 1 A-1) (eEF1A-1) (Leukocyte receptor cluster member 7) |
| EEF1B2, EEF1B, EF1B | Elongation factor 1-beta (EF-1-beta) |
| EIF5A | Eukaryotic translation initiation factor 5A-1 (eIF-5A-1) (eIF-5A1) (Eukaryotic initiation factor 5A isoform 1) (eIF-5A) (Rev-binding factor) (eIF-4D) |
| FKBP4, FKBP52 | Peptidyl-prolyl cis-trans isomerase FKBP4 (PPIase FKBP4) (EC 5.2.1.8) (51 kDa FK506-binding protein) (FKBP51) (52 kDa FK506-binding protein) (52 kDa FKBP) (FKBP-52) (59 kDa immunophilin) (p59) (FK506-binding protein 4) (FKBP-4) (FKBP59) (HSP-binding immunophilin) (HBI) (Immunophilin FKBP52) (Rotamase) (Cleaved into: Peptidyl-prolyl cis-trans isomerase FKBP4, N-terminally processed) |
| FLNC, ABPL, FLN2 | Filamin-C (FLN-C) (FLNc) (ABP-280-like protein) (ABP-L) (Actin-binding-like protein) (Filamin-2) (Gamma-filamin) |
| FLOT1 | Flotillin-1 |
| FUBP1 | Far upstream element-binding protein 1 (FBP) (FUSE-binding protein 1) (DNA helicase V) (hDH V) |
| GARS | Glycine-tRNA ligase (EC 3.6.1.17) (EC 6.1.1.14) (Diadenosine tetraphosphate synthetase) (AP-4-A synthetase) (Glycyl-tRNA synthetase) (GlyRS) |
| GSTK1, HDCMD47P | Glutathione S-transferase kappa 1 (EC 2.5.1.18) (GST 13-13) (GST class-kappa) (GSTK1-1) (hGSTK1) (Glutathione S-transferase subunit 13) |
| GSTO1, GSTTLP28 | Glutathione S-transferase omega-1 (GSTO-1) (EC 2.5.1.18) (Glutathione S-transferase omega 1-1) (GSTO 1-1) (Glutathione-dependent dehydroascorbate reductase) (EC 1.8.5.1) (Monomethylarsonic acid reductase) (MMA(V) reductase) (EC 1.20.4.2) (S-(Phenacyl)glutathione reductase) (SPG-R) |
| HSP90AB1, HSP90B HSPC2, HSPCB | Heat shock protein HSP 90-beta (HSP 90) (Heat shock 84 kDa) (HSP 84) (HSP84) |
| HSPA1L | Heat shock 70 kDa protein 1-like (Heat shock 70 kDa protein 1L) (Heat shock 70 kDa protein 1-Hom) (HSP70-Hom) |
| HSPA5, GRP78 | 78 kDa glucose-regulated protein (GRP-78) (Endoplasmic reticulum lumenal Ca(2+)-binding protein grp78) (Heat shock 70 kDa protein 5) (Immunoglobulin heavy chain-binding protein) (BiP) |
| HSPA8, HSC70, HSP73, HSPA10 | Heat shock cognate 71 kDa protein (Heat shock 70 kDa protein 8) (Lipopolysaccharide-associated protein 1) (LAP-1) (LPS-associated protein 1) |
| HSPA9, GRP75, HSPA9B, mt-HSP70 | Stress-70 protein, mitochondrial (75 kDa glucose-regulated protein) (GRP-75) (Heat shock 70 kDa protein 9) (Mortalin) (MOT) (Peptide-binding protein 74) (PBP74) |
| HSPB1, HSP27, HSP28 | Heat shock protein beta-1 (HspB1) (28 kDa heat shock protein) (Estrogen-regulated 24 kDa protein) (Heat shock 27 kDa protein) (HSP 27) (Stress-responsive protein 27) (SRP27) |
| HSPD1, HSP60 | 60 kDa heat shock protein, mitochondrial (EC 3.6.4.9) (60 kDa chaperonin) (Chaperonin 60) (CPN60) (Heat shock protein 60) (HSP-60) (Hsp60) (HuCHA60) (Mitochondrial matrix protein P1) (P60 lymphocyte protein) |
| ILVBL, AHAS | Acetolactate synthase-like protein (EC 2.2.1.-) (IlvB-like protein) |
| IMMT, HMP, MIC60, MINOS2, PIG4, PIG52 | MICOS Complex subunit MIC60 (Cell proliferation-inducing gene 4/52 protein) (Inner mitochondrial membrane protein) (Mitofilin) (p87/89) |
| LDHB | L-lactate dehydrogenase B chain (LDH-B) (EC 1.1.1.27) (LDH heart subunit) (LDH-H) (Renal carcinoma antigen NY-REN-46) |
| LGALS1 | Galectin-1 (Gal-1) (14 kDa laminin-binding protein) (HLBP14) (14 kDa lectin) (Beta-galactoside-binding lectin L-14-I) (Galaptin) (HBL) (HPL) (Lactose-binding lectin 1) (Lectin galactoside-binding soluble 1) (Putative MAPK-activating protein PM12) (S-Lac lectin 1) |
| LMNA, LMN1 | Prelamin-A/C (Cleaved into: Lamin-A/C (70 kDa lamin) (Renal carcinoma antigen NY-REN-32)) |
| MDH2 | Malate dehydrogenase, mitochondrial (EC 1.1.1.37) |
| MFN2, CPRP1, KIAA0214 | Mitofusin-2 (EC 3.6.5.-) (Transmembrane GTPase MFN2) |
| MYL6 | Myosin light polypeptide 6 (17 kDa myosin light chain) (LC17) (Myosin light chain 3) (MLC-3) (Myosin light chain alkali 3) (Myosin light chain A3) (Smooth muscle and non-muscle myosin light chain alkali 6) |
| NDUFA10 | NADH dehydrogenase (ubiquinone) 1 alpha subcomplex subunit 10, mitochondrial (Complex I-42kD) (CI-42kD) (NADH-ubiquinone oxidoreductase 42 kDa subunit) |
| NDUFA11 | NADH dehydrogenase [ubiquinone] 1 alpha subcomplex subunit 11 (Complex I-B14.7) (CI-B14.7) (NADH-ubiquinone oxidoreductase subunit B14.7) |
| NDUFA4 | Cytochrome c oxidase subunit NDUFA4 (Complex I-MLRQ) (CI-MLRQ) (NADH-ubiquinone oxidoreductase MLRQ subunit) |
| NDUFS1 | NADH-ubiquinone oxidoreductase 75 kDa subunit, mitochondrial (EC 1.6.5.3) (EC 1.6.99.3) (Complex I-75kD) (CI-75kD) |
| NDUFS3 | NADH dehydrogenase (ubiquinone) iron-sulfur protein 3, mitochondrial (EC 1.6.5.3) (EC 1.6.99.3) (Complex I-30kD) (CI-30kD) (NADH-ubiquinone oxidoreductase 30 kDa subunit) |
| NEDD8 | NEDD8 (Neddylin) (Neural precursor cell expressed developmentally downregulated protein 8) (NEDD-8) (Ubiquitin-like protein Nedd8) |
| NPM1, NPM | Nucleophosmin (NPM) (Nucleolar phosphoprotein B23) (Nucleolar protein NO38) (Numatrin) |
| OAT | Ornithine aminotransferase, mitochondrial (EC 2.6.1.13) (Ornithine delta-aminotransferase) (Ornithine—oxo-acid aminotransferase) (Cleaved into: Ornithine aminotransferase, hepatic form; Ornithine aminotransferase, renal form) |
| OGDH | 2-oxoglutarate dehydrogenase, mitochondrial (EC 1.2.4.2) (2-oxoglutarate dehydrogenase complex component E1) (OGDC-E1) (Alpha-ketoglutarate dehydrogenase) |
| OTUB1, OTB1, OTU1, HSPC263 | Ubiquitin thioesterase OTUB1 (EC 3.4.19.12) (Deubiquitinating enzyme OTUB1) (OTU domain-containing ubiquitin aldehyde-binding protein 1) (Otubain-1) (hOTU1) (Ubiquitin-specific-processing protease OTUB1) |
| PDIA3, ERP57, ERP60, GRP58 | Protein disulfide-isomerase A3 (EC 5.3.4.1) (58 kDa glucose-regulated protein) (58 kDa microsomal protein) (p58) (Disulfide isomerase ER-60) (Endoplasmic reticulum resident protein 57) (ER protein 57) (ERp57) (Endoplasmic reticulum resident protein 60) (ER protein 60) (ERp60) |
| PGK1, PGKA, MIG10, OK/SW-cl.110 | Phosphoglycerate kinase 1 (EC 2.7.2.3) (Cell migration-inducing gene 10 protein) (Primer recognition protein 2) (PRP 2) |
| PHB | Prohibitin |
| PHB2, BAP, REA | Prohibitin-2 (B-cell receptor-associated protein BAP37) (D-prohibitin) (Repressor of estrogen receptor activity) |
| PIN1 | Peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (EC 5.2.1.8) (Peptidyl-prolyl cis-trans isomerase Pin1) (PPIase Pin1) (Rotamase Pin1) |
| PPIA, CYPA | Peptidyl-prolyl cis-trans isomerase A (PPIase A) (EC 5.2.1.8) (Cyclophilin A) (Cyclosporin A-binding protein) (Rotamase A) (Cleaved into: Peptidyl-prolyl cis-trans isomerase A, N-terminally processed) |
| PRDX4 | Peroxiredoxin-4 (EC 1.11.1.15) (Antioxidant enzyme AOE372) (AOE37-2) (Peroxiredoxin IV) (Prx-IV) (Thioredoxin peroxidase AO372) (Thioredoxin-dependent peroxide reductase A0372) |
| PSMA3, HC8, PSC8 | Proteasome subunit alpha type-3 (EC 3.4.25.1) (Macropain subunit C8) (Multi-catalytic endopeptidase complex subunit C8) (Proteasome component C8) |
| PTPN5 | Tyrosine-protein phosphatase non-receptor type 5 (EC 3.1.3.48) (Neural-specific protein-tyrosine phosphatase) (Striatum-enriched protein-tyrosine phosphatase) (STEP) |
| RAB14 | Ras-related protein Rab-14 |
| RAB2A, RAB2 | Ras-related protein Rab-2A |
| RAC1, TC25, MIG5 | Ras-related C3 botulinum toxin substrate 1 (Cell migration-inducing gene 5 protein) (Ras-like protein TC25) (p21-Rac1) |
| RAPGEF2, KIAA0313, NRAPGEP, PDZGEF1 | Rap guanine nucleotide exchange factor 2 (Cyclic nucleotide ras GEF) (CNrasGEF) (Neural RAP guanine nucleotide exchange protein) (nRap GEP) (PDZ domain-containing guanine nucleotide exchange factor 1) (PDZ-GEF1) (RA-GEF-1) (Ras/Rap1-associating GEF-1) |
| RHOA, ARH12, ARHA, RHO12 | Transforming protein RhoA (Rho cDNA clone 12) (h12) |
| RNH1, PRI, RNH | Ribonuclease inhibitor (Placental ribonuclease inhibitor) (Placental RNase inhibitor) (Ribonuclease/angiogenin inhibitor 1) (RAI) |
| RPN1 | Dolichyl-diphosphooligosaccharide—protein glycosyltransferase subunit 1 (Dolichyl-diphosphooligosaccharide—protein glycosyltransferase 67 kDa subunit) (Ribophorin I) (RPN-I) (Ribophorin-1) |
| RPN2 | Dolichyl-diphosphooligosaccharide—protein glycosyltransferase subunit 2 (Dolichyl-diphosphooligosaccharide—protein glycosyltransferase 63 kDa subunit) (RIBIIR) (Ribophorin II) (RPN-II) (Ribophorin-2) |
| RPS15A, OK/SW-cl.82 | 40S ribosomal protein S15a (Small ribosomal subunit protein uS8) |
| RPS3, OK/SW-cl.26 | 40S ribosomal protein S3 (EC 4.2.99.18) (Small ribosomal subunit protein uS3) |
| S100A10, ANX2LG CAL1L CLP11 | Protein S100-A10 (Calpactin I light chain) (Calpactin-1 light chain) (Cellular ligand of annexin II) (S100 calcium-binding protein A10) (p10 protein) (p11) |
| SAMM50, SAM50 CGI-51 TRG3 | Sorting and assembly machinery component 50 homolog (Transformation-related gene 3 protein) (TRG-3) |
| SELENBP1, SBP | Selenium-binding protein 1 (56 kDa selenium-binding protein) (SBP56) (SP56) |
| SFXN1 | Sideroflexin-1 (Tricarboxylate carrier protein) (TCC) |
| SH3GLB2, KIAA1848, PP578 | Endophilin-B2 (SH3 domain-containing GRB2-like protein B2) |
| SIRT2, SIR2L, SIR2L2 | NAD-dependent protein deacetylase sirtuin-2 (EC 3.5.1.-) (Regulatory protein SIR2 homolog 2) (SIR2-like protein 2) |
| SLC25A13, ARALAR2 | Calcium-binding mitochondrial carrier protein Aralar2 (Citrin) (Mitochondrial aspartate glutamate carrier 2) (Solute carrier family 25 member 13) |
| SLC25A18, GC2 | Mitochondrial glutamate carrier 2 (GC-2) (Glutamate/H(+) symporter 2) (Solute carrier family 25 member 18) |
| SLC25A5, ANT2 | ADP/ATP translocase 2 (ADP, ATP carrier protein 2) (ADP, ATP carrier protein, fibroblast isoform) (Adenine nucleotide translocator 2) (ANT 2) (Solute carrier family 25 member 5) (Cleaved into: ADP/ATP translocase 2, N-terminally processed) |
| SLC9A3R1, NHERF, NHERF1 | Na(+)/H(+) exchange regulatory cofactor NHE-RF1 (NHERF-1) (Ezrin-radixin-moesin-binding phosphoprotein 50) (EBP50) (Regulatory cofactor of Na(+)/H(+) exchanger) (Sodium-hydrogen exchanger regulatory factor 1) (Solute carrier family 9 isoform A3 regulatory factor 1) |
| SSBP1, SSBP | Single-stranded DNA-binding protein, mitochondrial (Mt-SSB) (MtSSB) (PWP1-interacting protein 17) |
| TPD52 | Tumor protein D52 (Protein N8) |
| TPM1, C15orf13, TMSA | Tropomyosin alpha-1 chain (Alpha-tropomyosin) (Tropomyosin-1) |
| TPM2, TMSB | Tropomyosin beta chain (Beta-tropomyosin) (Tropomyosin-2) |
| TPM3 | Tropomyosin alpha-3 chain (Gamma-tropomyosin) (Tropomyosin-3) (Tropomyosin-5) (hTM5) |
| TPM4 | Tropomyosin alpha-4 chain (TM30p1) (Tropomyosin-4) |
| TUBA1A, TUBA3 | Tubulin alpha-1A chain (Alpha-tubulin 3) (Tubulin B-alpha-1) (Tubulin alpha-3 chain) (Cleaved into: Detyrosinated tubulin alpha-1A chain) |
| TUBB, TUBB5, OK/SW-cl.56 | Tubulin beta chain (Tubulin beta-5 chain) |
| TUBB4B, TUBB2C | Tubulin beta-4B chain (Tubulin beta-2 chain) (Tubulin beta-2C chain) |
| TUFM | Elongation factor Tu, mitochondrial (EF-Tu) (P43) |
| UQCRB, UQBP | Cytochrome b-c1 complex subunit 7 (Complex III subunit 7) (Complex III subunit VII) (QP-C) (Ubiquinol-cytochrome c reductase complex 14 kDa protein) |
| UQCRFS1 | Cytochrome b-c1 complex subunit Rieske, mitochondrial (EC 1.10.2.2) (Complex III subunit 5) (Cytochrome b-c1 complex subunit 5) (Rieske iron-sulfur protein) (RISP) (Ubiquinol-cytochrome c reductase iron-sulfur subunit) (Cleaved into: Cytochrome b-c1 complex subunit 11 (Complex III subunit IX) (Ubiquinol-cytochrome c reductase 8 kDa protein)) |
| UQCRFS1P1, UQCRFSL1 | Putative cytochrome b-c1 complex subunit Rieske-like protein 1 (Ubiquinol-cytochrome c reductase Rieske iron-sulfur subunit pseudogene 1) |
| UQCRH | Cytochrome b-c1 complex subunit 6, mitochondrial (Complex III subunit 6) (Complex III subunit VIII) (Cytochrome c1 non-heme 11 kDa protein) (Mitochondrial hinge protein) (Ubiquinol-cytochrome c reductase complex 11 kDa protein) |
| USMG5, DAPIT, HCVFTP2, PD04912 | Upregulated during skeletal muscle growth protein 5 (Diabetes-associated protein in insulin-sensitive tissues) (HCV F-transactivated protein 2) |
| VCP | Transitional endoplasmic reticulum ATPase (TER ATPase) (EC 3.6.4.6) (15S Mg(2+)-ATPase p97 subunit) (Valosin-containing protein) (VCP) |
| VDAC1, VDAC | Voltage-dependent anion-selective channel protein 1 (VDAC-1) (hVDAC1) (Outer mitochondrial membrane protein porin 1) (Plasmalemmal porin) (Porin 31HL) (Porin 31HM) |
| VDAC2 | Voltage-dependent anion-selective channel protein 2 (VDAC-2) (hVDAC2) (Outer mitochondrial membrane protein porin 2) |
| VDAC3 | Voltage-dependent anion-selective channel protein 3 (VDAC-3) (hVDAC3) (Outer mitochondrial membrane protein porin 3) |
| VIM | Vimentin |
| YWHAE | 14-3-3 protein epsilon (14-3-3E) |
| YWHAZ | 14-3-3 protein zeta/delta (Factor activating exoenzyme S) (FAS) (Protein kinase C inhibitor protein 1) (KCIP-1) |
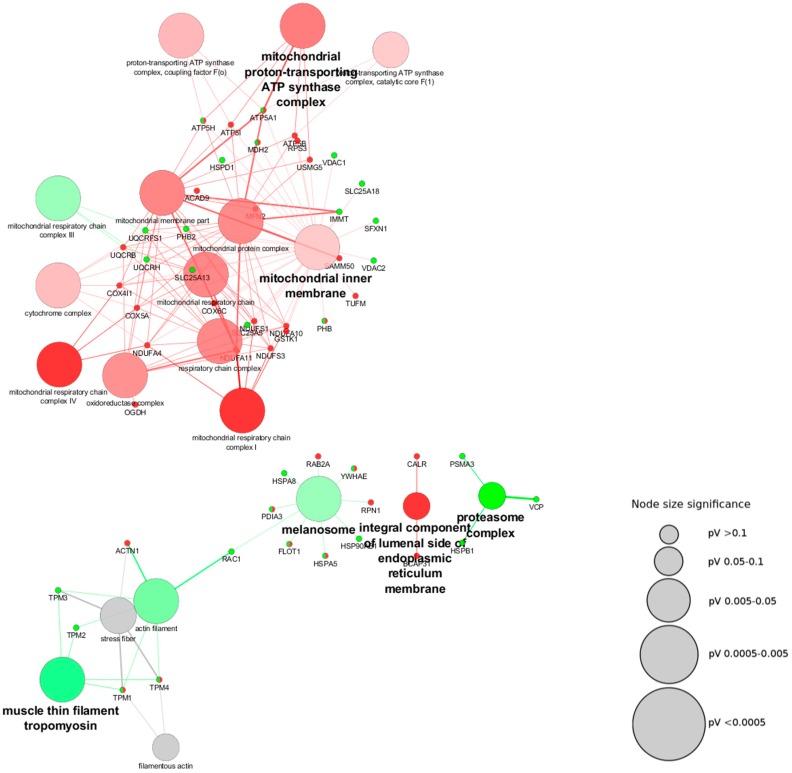
As a first approach we assessed the cellular components, which are represented by these proteins using the plugin ClueGO in Cytoscape software (Figure 1). In Figure 4 it is possible to see the network built from the different cellular components and their upregulation (green nodes) or downregulation (red nodes) in Parkinson’s disease. The cluster of proteins that were found to be upregulated fall into diverse cellular components: mitochondrial respiratory chain Complex III, proteasome complex, muscle thin filament tropomyosin, and melanosome. On the other hand, the downregulated are represented by: inner mitochondrial membrane, integral component of the lumenal side of the endoplasmic reticulum membrane, and mitochondrial proton-transporting ATP synthase complex.
Figure 4.
Cytoscape network of the main cellular components associated with mitochondrial-shaping proteins in the context of Parkinson’s disease. The binding partners of the mitochondrial-shaping proteins found to be modified in different proteomics-based approaches in the context of Parkinson’s disease according to the Human Integrated Protein-Protein Interaction rEference (HIPPIE) and appearing as modified in proteomics-based studies on Parkinson’s disease were subjected to network analysis using the plugin ClueGo from the software Cytoscape to analyze the cellular components represented by the proteins from the list. Gray scale nodes correspond to cellular components that were found to be equally up- and downregulated in different studies, while green and red nodes are representative of upregulated and downregulated cellular components respectively, in the context of Parkinson’s disease. The increase in green and red color gradient represents higher amounts of the contribution of up- and downregulated proteins, respectively. The size of the nodes is indicative of their statistical significance.
The proteins used to search for the binding partners were mitochondrial proteins, thus alterations in the mitochondrial cellular components were expected. In this regard, the downregulation of the inner mitochondrial membrane and the mitochondrial proton-transporting ATP synthase complex was anticipated. Several of the proteins found to be altered in the context of Parkinson’s disease (Table 2) are proteins located at the inner mitochondrial membrane, and the alteration of these components has also previously been described in the pathology [7].
Interestingly, it has been shown that the ubiquitin-proteasome system regulates the level of proteins targeted to the mitochondrial intermembrane space, and this process depends on the mitochondrial intermembrane space import machinery [102]. Additionally, it has been shown that the ubiquitin-proteasome system acts on the regulation of the mitochondrial biogenesis [103]. In this study, we found an upregulation of the proteasome, which corroborates the evidence of its dysfunction in Parkinson’s disease [103,104]. ROS levels are increased in Parkinson’s disease and are responsible for the oxidative modification of lipids, DNA, and proteins [105]. These modifications might lead to misfolded proteins and aggregation [106]. Mitochondrial proteins might be dysfunctional due to the harmful effects of ROS, which not only might modify the folded proteins, but also affect the incorporation of newly synthetized mitochondrial proteins since they are translated in the cytosol and must be transported unfolded into the mitochondria [103]. In an oxidative stress scenario, as in Parkinson’s disease, the risk of the alteration of unfolded proteins and consequent removal by the proteasome is higher, reducing the amount of mitochondrial proteins available. Besides, it is known that outer mitochondrial membrane proteins involved in mitochondrial fusion are regulated by ubiquitination and that this process is induced by stress [19].
Mitochondrial dynamics not only relies on mitochondrial fusion and fission proteins, but also on the contact sites between mitochondria and the ER, which are fundamental for the initial fission process [107]. It has been described that the shape-forming proteins control mitochondrial morphology by mediating the attachment of the mitochondria to the cytoskeleton and the ER [107,108], and they can also connect the inner and outer mitochondrial membranes, hence influencing the import and assembly of mitochondrial proteins [109]. Regarding the upregulation of the melanosome as a cellular component, although it is an organelle not present in neuronal cells, when we look closely at the proteins contributing to this node, we find that three of the proteins are heat shock proteins. These proteins are key components in ensuring proper protein function and are expressed in response to stress, controlling the subsequent degradation of misfolded proteins, which is also in line with the upregulation of the proteasome complex and the occurrence of the oxidative stress characteristic of the disorder.
The mitochondrial cytochrome bc1 complex from the respiratory chain (Complex III) is one of the main producers of ROS, together with the Complex I [110]. Although Complex I release superoxide into the mitochondrial matrix, Complex III does it into the intermembrane space and the cytosol [111]. In the pathobiology of Parkinson’s disease, it is well accepted that there is an increase in ROS leading to oxidative stress [105], which is in agreement with the upregulation of the cellular mitochondria component of the respiratory chain Complex III found in our analysis. This complex is localized in the inner mitochondrial membrane, at the cristae, and has three transmembrane subunits in which the prosthetic groups involved in the redox reactions are located. They must be dimerized for proper functioning, which is also dependent on the mitochondrial membrane potential [110], suggesting that alterations in the organization of the inner mitochondrial membrane might affect their function.
A closer look at the network shows that “muscle thin filament tropomyosin” is connected to cellular components related to the actin cytoskeleton (“actin filament”, “stress fiber”, and “filamentous actin”). As described above, the cytoskeleton also plays a role in the dynamics and movement of the mitochondria [108]. Interestingly, in the context of Parkinson’s disease some models (both genetic and drug-based) showed a negative impact on the dynamics of the actin cytoskeleton and the formation of stress fibers [108,112,113].
3.3. Biological Processes Associated with Mitochondrial-Shaping Proteins Affected in Parkinson’s Disease
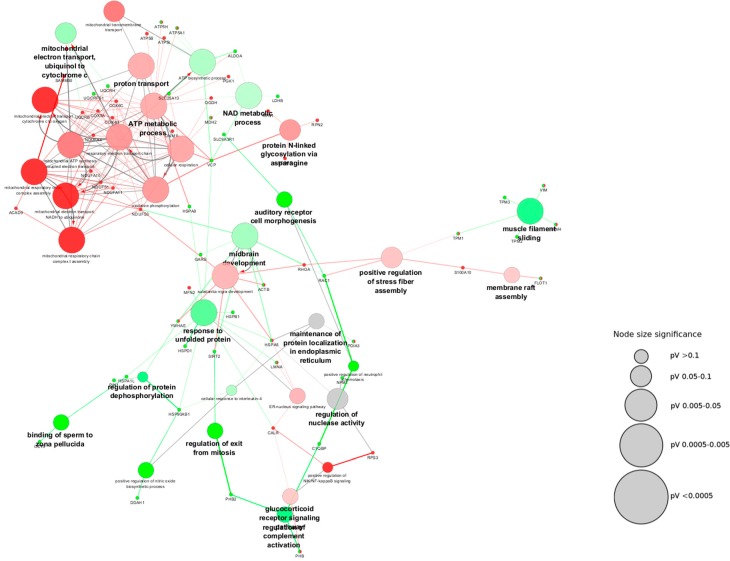
To obtain information on the biological processes related to the mitochondrial-shaping proteins affected in Parkinson’s disease, we undertook a bioinformatic approach using the plugin ClueGo from the Cystoscope software (Figure 5 and Table 4). This plugin allows the extraction of the biological meaning of large lists of proteins [114]. Overall, around 44% altered processes are related to energy production by the mitochondria. This contribution was expected since the dysfunction of this organelle is a hallmark of the disease.
Figure 5.
Cytoscape network of the main biological processes associated with mitochondrial-shaping proteins in the context of Parkinson’s disease. The binding partners of the mitochondrial-shaping proteins found modified in different proteomics-based approaches in the context of Parkinson’s disease were subjected to network analysis using the plugin ClueGo from the software Cytoscape to analyze the biological processes affected in the disease. Gray scale nodes correspond to biological pathways that were found to be equally up- and downregulated in different studies, while green and red nodes are representative of upregulated and downregulated biological pathways, respectively, in the context of Parkinson’s disease. The increase in green and red color gradient represents higher amounts of the contribution of up- and downregulated proteins, respectively. The size of the nodes is indicative of their statistical significance.
Table 4.
List of biological processes related to the mitochondrial-shaping proteins affected in Parkinson’s disease.
| Upregulated | Downregulated |
|---|---|
| ATP biosynthetic process | ATP metabolic process |
| Positive regulation of nitric oxide biosynthetic process | Membrane raft assembly |
| Response to unfolded protein | Positive regulation of stress fiber assembly |
| Auditory receptor cell morphogenesis | Gluthatione derivative biosynthetic process |
| Binding of sperm to zona pellucida | Protein N-linked glycosylation via asparagine |
| Regulation of protein dephosphorylation | Glucocorticoid receptor signaling pathway |
| Mitochondrial electron transport ubiquinol to cytochrome c | ER-nucleus signaling pathway |
| Regulation of exit from mitosis | Substantia nigra development |
| NAD metabolic process | Positive regulation of NFkB signaling |
| Muscle filament sliding | Mitochondrial transmembrane transport |
| Regulation of complement activation | Mitochondrial electron transport cytochrome c to oxygen |
| Midbrain development and positive regulation of neutrophil chemotaxis | Respiratory electron transport chain |
| Oxidative phosphorylation | |
| Mitochondrial respiratory chain Complex I assembly | |
| Mitochondrial electron transport NADH to ubiquinone | |
| Mitochondria respiratory chain complex assembly | |
| Mitochondrial ATP synthesis coupled to electron transport | |
| Cellular respiration and proton transport |
Interestingly, other biological processes are related to the occurrence of oxidative stress and the respective alterations in proteins, which is also a known characteristic of Parkinson’s disease [105]. In this regard, the positive regulation of the nitric oxide (NO) biosynthetic process have been shown to occur in this disorder, which is relevant for neuronal death. When NO synthases are ablated, animals are protected against the effect of the MPTP toxin [115]. It is also known that NO not only induces oxidative stress but also neuronal death [116,117]. The downregulation of the glutathione derivative biosynthetic process is also a characteristic of an oxidative stress scenario, which has also been described in Parkinson’s disease [118]. This peptide acts as a cellular antioxidant, which is produced by neurons and glial cells, and it has been proposed as an important molecule for therapeutic purposes in the context of Parkinson’s disease [118,119]. Moreover, the upregulation of the response to unfolded proteins is important in an oxidative stress scenario where proteins and peptides can be oxidatively modified with a harmful effect on their three-dimensional (3D) structure, with aggregation having a negative impact on their function [106]. Besides, protein oxidative modifications and aggregation have been also related to the decreased in glutathione levels [120].
As stated along this work, the cellular cytoskeleton is one of the mechanisms contributing to the definition of mitochondrial morphology [108]. In fact, modification of the actin cytoskeleton has been probed in Parkinson’s disease [108,112,113]. Mitochondrial fusion and fission processes are affected by the interaction of the mitochondria with the cytoskeleton. It has been described that the fusion process can be delayed when actin filaments are depolymerized [121]. The actin cytoskeleton is also involved in the fission process [38]. In our network, several processes are related to the actin cytoskeleton, such as the upregulation of the process of “muscle filament sliding” and the downregulation of the “positive regulation of stress fiber assembly”. Interestingly, after a closer look at the modified biological process of “binding of sperm to zona pellucida”, we observed that the proteins connected to this process are molecular chaperones and, remarkably, TCP-1-epsilon is known to play a role in the folding of actin and tubulin [122].
Regarding the “auditory receptor cell morphogenesis” biological processes, it is important to note that the protein Rac1 contributes to this pathway and is involved in the regulation of secretory processes, the phagocytosis of death cells, cell polarization, and the formation of membrane ruffles. In the context of Parkinson’s disease, it has been shown to contribute to a ROS generating pathway acting with Nox1, causing neuronal death [123]. Interestingly, the other component of this node is the NHERF-1 protein, which has been shown to act as a scaffold for connecting plasma membrane proteins with members of the ERM (ezrin/moesin/radixin) family, aiding in their link to the actin cytoskeleton for the regulation of their surface expression [124].
Within the highlighted process of “regulation of protein dephosphorylation” involved in the regulation of protein function, we found an interesting protein contribution to this pathway: the Peptidyl-prolyl cis-trans isomerase (Pin1). This protein has been shown to be involved in the disease, being upregulated in cellular and animal models as well as in SN in patients [125]. The alteration of this biological process might have an impact on stress responses, immune function, and neuronal survival [126]. Also, this pathway is fundamental for proper mitochondrial functioning and signaling since, in response to the metabolic state of the cell, mitochondrial proteins from the import machinery might be regulated by phosphorylation [127].
In the “regulation of exit from mitosis” process, two interesting proteins emerge: Prohibitin-2 and the NAD-dependent protein deacetylase sirtuin-2. The latter deacetylates lysines on histones, alpha-tubulin, and other proteins [128]. By acting on tubulin it has a direct impact on microtubule function. Tubulin can be subjected to different post-translational modifications with influence on the microtubule polymerization state and its function, such as acetylation [129]. This modification on the residue K40 has been reported to alter the interaction of proteins with the cytoskeleton, with subsequent impact on the intracellular transport along the microtubules [129]. As described in this work, this may affect mitochondria morphology and dynamics.
Parkinson’s disease has long been linked to increased inflammatory response [130]. In our analysis we found that the processes related to the inflammatory response were upregulated: “positive regulation of neutrophil chemotaxis” and “regulation of complement activation”. Interestingly, from the last process, two of the implicated proteins belong to the Prohibitin family, which have been described to be involved in the regulation of mitochondrial respiration [131]. Regarding the downregulation of the process of the “glucocorticoid receptor signaling pathway” it is important to note that a decrease in the levels of the glucocorticoid receptor in both the SN of patients and in animal models of the disease has been reported [132,133]. These receptors regulate inflammation and are dysregulated in microglia in the context of Parkinson’s disease. Dysregulation has been proposed to sustain the chronic inflammatory state observed in this disorder as well as the increased permeability of the blood brain barrier, which might increase neuronal vulnerability [132,133]. Another pathway related to the inflammatory process is downregulated: “positive regulation of NF-kB signaling”, in which the protein ribosomal protein S3 stands out. Interestingly, this protein has been proposed to protect the dopaminergic neurons from apoptosis [134].
Within the network, the biological processes of “midbrain development” and “substantia nigra development” share three proteins: Actin, Complex I 30 kD from the mitochondrial respiratory chain, and the 14-3-3 protein epsilon. As described previously, the dysfunction of Complex I from the mitochondrial respiratory chain was the first indication of the mitochondria involvement in the pathobiology of Parkinson’s disease [7,8]. The contribution of the cytoskeleton has also been shown, in which actin has a key role in the secretion of the synaptic vesicles content that might be then translated into a decrease in the content of neurotransmitters in the synaptic cleft [135]. Although the 14-3-3 protein is ubiquitously expressed and participates in the regulation of many signaling pathways, it has also been found to be a constituent of the Lewy bodies of Parkinson’s disease patients [136].
In Parkinson’s disease there is a critical modification in the lipid rafts composition, and increasing evidence shows their contribution to the disorder [137,138,139]. Lipid rafts have a role in diverse cellular processes such as membrane trafficking, signal transduction, and cytoskeletal organization. Their alteration can also have a negative impact on protein-protein interactions, which are fundamental processes for the formation of protein supercomplexes [138]. Interestingly, we found the process of “membrane raft assembly” to be downregulated. Not only was the protein Flotillin-1, a well-known component of the lipid rafts, found to contribute to this node, but also the protein S100A10. The S100 family of proteins are involved in several cellular processes such as the regulation of cell proliferation and differentiation, apoptosis, calcium homeostasis, energy metabolism, and inflammation. Interestingly, they also interact with cytoskeletal and other cellular proteins [140]. Some of the membrane proteins that interact with the S100A10 are: Annexin 2, ion channels, actin binding proteins, and the serotonin receptor [140]. This protein has been proposed to function on membrane repair and was shown to be downregulated in depressive-like states in mice, with its expression being regulated by neurotrophins [141,142].
N-glycosylation is a post-translational modification that is found in membrane proteins and secreted proteins; amongst them are growth factors and their receptors [143]. In our analysis, we found that the process of “protein N-linked glycosylation via asparagine” was downregulated. This modification takes places in the ER and in the Golgi, having an effect on protein function. Evidence show that N-glycosylation is important for proper neuronal function and has a role in synaptic transmission [144], hence having a profound impact on the disease [145].
The occurrence of a role of the ER stress in the context of Parkinson’s disease [146] is supported through new evidence, and the process of the “ER-nucleus signaling pathway” was found to be downregulated in our analysis. In this node, we found the LMNA. Lamins are filamentous proteins that contribute to the nucleus architecture and gene expression [147,148]. These proteins also interact with the actin cytoskeleton, which is known to be affected in Parkinson’s disease [108,112,113,149]. The other proteins (calreticulin and the heat shock 70 kDa protein 5) are chaperones involved in protein folding and the formation of multimeric complexes [150,151], playing a crucial role in an oxidative stress scenario. Additionally, in the case of fission, not only actin but also the ER is involved in the process of mitochondrial preconstruction and DRP1 assembly [107].
4. Discussion
Mitochondria are fundamental organelles for cells, working mainly on energy production, calcium homeostasis, and apoptosis. Defects in the mitochondrial respiratory chain have received much of the attention as a key player in the pathobiology of Parkinson’s disease [8,152]. However, additional modifications of the mitochondria are being increasingly reported [153,154]. Besides, it is now known that the inhibition of Complex I from the mitochondrial respiratory chain by MPP+ and rotenone does not directly trigger cytochrome c release but, instead, increases the amount of cytochrome c within the mitochondrial intermembrane space [155], indicating that there are other processes required to trigger neuronal death. Amongst them are changes in mitochondrial dynamics (i.e., alterations in the fusion and fission processes, alteration of cristae morphology) [85,156].
Increasing evidence shows that for proper mitochondrial function, processes like mitochondrial fusion, fission, and turnover are fundamental, and their dysfunction has been linked to different diseases [1,3]. In the context of Parkinson’s disease, an increase in mitochondrial fission has been reported [73,157,158], suggesting that this excessive fragmentation might then enhance cytochrome c release from mitochondria and subsequently triggering apoptosis [159]. However, we found the process of cristae remodeling to be more highlighted in our analysis regarding the alteration of the mitochondrial-shaping proteins in Parkinson’s disease. Notably, the alteration of the mitochondria cristae and membrane might affect the proper binding of cytochrome c, favoring its release to the cytosol and initiating the apoptotic process [155]. Some evidence of mitochondrial cristae remodeling exists in the context of Parkinson’s disease. One study using a cybrid cell line constructed with mitochondria DNA isolated from cells from Parkinson’s disease patients showed that there were deficiencies in both complexes of the mitochondrial respiratory chain I and IV, and cells contained a non-homogenous mitochondrial population with different morphologies ranging from enlarged to swollen and rounded in shape, which also displayed different mitochondrial membrane potential values [160]. At the ultrastructural level, some mitochondria from this cybrid displayed a decreased in the matrix density and contained a reduced number of cristae and a discontinuous outer mitochondrial membrane [160]. Similarly, in a study using transgenic mice for mutated α-synuclein, morphological alterations on the cristae were also observed, showing a disordered inner membrane and swollen matrix [34]. However, this type of study with samples from human patients is insufficient, and an increasing number of studies aiming at deciphering the ultrastructure of the mitochondria in Parkinson’s disease by electron and super-resolution microscopy are required.
It is known that cristae remodeling is fundamental during apoptosis for the proper release of cytochrome c [27], and that the cristae are the sites were the OXPHOS components are located (94% of Complex II and ATP synthase [161], and 85% of cytochrome c [27]). Compelling data indicate that the shape of the cristae is crucial for the modulation of the OXPHOS function [18], and relies on the cellular state [162,163]. Disruption of the cristae junctions is a result of the release of apoptotic factors from the mitochondria [27]. Remarkably, in our analysis most of the proteins involved in mitochondrial dynamics that were found to be altered in the context of Parkinson’s disease have been previously reported to play a role in the morphology of the cristae.
When imaging mitochondria, four main components can be distinguished at the ultrastructure level: the outer mitochondrial membrane (OMM), important for regulating membrane permeability and the import/export of mitochondrial proteins; the inner mitochondrial membrane (IMM), where the mitochondrial respiratory chain is placed (the invaginations of the IMM into the matrix are the so-called mitochondria cristae); the intermembrane space (IMS), which is the space between the two mitochondrial membranes; and the matrix, where the components of the tricarboxylic acid (TCA) cycle are located. The inner mitochondrial membrane is organized into three specialized zones: the inner boundary membrane, where the inner and outer membranes are associated, containing proteins of the protein import machinery; the cristae, which are the inner membrane invaginations that are enriched in proteins involved in protein translocation and synthesis as well as proteins involved in iron-sulfur biogenesis; and the cristae junctions, which are the portion of the cristae that are constricted and where the MICOS Complex is located [3].
Fundamental to cell survival is the implication of the mitochondria in the regulation of apoptosis. Within this organelle several pro-apoptotic proteins reside, triggering the apoptotic process when released into the cytosol. The permeabilization of the OMM constitutes a point of no return in the activation of this process, where the Bcl2 family of proteins participates in its regulation [164]. Interestingly, our network analysis highlighted the alteration on the permeability of membranes, supporting the apoptotic activation [165].
The OMM morphology is influenced by its interaction with the ER, ribosomes, the nucleus, and the cellular cytoskeleton [3]. Fundamental to the regulation of multiple cellular processes are the mitochondrial-ER contact sites [164]. In our network analysis, this intraorganellar interaction was highlighted as being altered in Parkinson’s disease. Amongst the cellular processes are: the regulation of the intracellular calcium levels, mitochondrial fission, the endowment of membranes to phagosomes, and the formation of the inflammasome [166]. It is now clear how the ER participates in the initiation of the mitochondrial fission process. The ER enwraps the mitochondria at the constriction site where the dynamin-like protein Drp1 responsible for the fission process localizes [107,167]. Additionally, actin polymerization and the ER protein inverted formin 2 (INF2) are involved in this process [38]. Interestingly, actin filaments polymerized around the constriction sites might constitute the pulling force for the fission process [38], and several processes related to the actin cytoskeleton were found to be altered in our analysis. Additionally, the actin cytoskeleton plays a fundamental role in synaptic vesicle secretion. The alteration of this process affects synaptic transmission in the disease. Not only actin but also calcium is involved in this process.
The regulation of calcium levels is also dependent on the mitochondria-ER crosstalk, and a modification of its homeostasis has been reported in Parkinson’s disease [168]. Mitochondrial calcium channels display low affinity for this ion, and for correct calcium entry into the mitochondria for the formation of the ER-mitochondrial contact sites is fundamental [169]. The relevance of this interaction has been shown by its involvement in the progression of Alzheimer’s disease, where it is upregulated [170]. When calcium accumulates within the mitochondria, oxidative phosphorylation and ATP production are enhanced [171]. In addition, different chaperones are involved in the stabilization of these contact sites and could coordinate signaling between mitochondria and the ER [166]. In this direction, we also found that the expression of the chaperone grp78 was altered [172]. The ER-mitochondria contact sites are also related with the ER-stress response, which might trigger apoptosis [173]. This pathway has also been shown to be active in the context of Parkinson’s disease [174]. Additionally, the calcium released by the ER at these contact sites might act as an amplifier of the apoptotic pathway [166]. Besides, the fission protein Fis1 has also been shown to facilitate the cleavage of the pro-apoptotic protein Bap31 [175]. Interestingly, these contact sites are not only relevant to the regulation of calcium levels, but also to ROS-mediating signaling [176].
Moreover, the ER contacts with the phagosomes and non-functional mitochondria degraded by mitophagy are recognized by specific OMM proteins [166]. MFN2 has also been indicated as critical to autophagosome formation, and the ER-mitochondria interaction is important for autophagosome formation [166,177]. Accumulating evidence shows that the ER might also be involved in the mitochondrial fusion process, since it was shown that mitofusin2 (MFN2) is necessary for the tethering of both organelles [178].
Relevant to proper neuronal function is the appropriate localization of the mitochondria within the synaptic terminals, where they can provide ATP for exocytosis and regulate calcium levels during synaptic transmission [179]. Mitochondria positioning within these terminals relies not only on mitochondrial fission [180], since only small mitochondria might fit into the terminals, but also in correct mitochondrial movement along microtubules and the actin cytoskeleton [164]. In this work, the network analysis of cellular components and biological pathways indicated that in the context of Parkinson’s disease actin filaments are affected [108,112,113]. In addition, dysregulation of the cellular microtubules has been reported, namely in the alteration of proteins involved in tubulin acetylation. Most of the drugs used to induce Parkinson’s disease modify microtubules, and specifically, acetylation has been shown to affect the interaction of proteins with the cytoskeleton [129]. Alteration of the cellular cytoskeleton might have an impact not only on mitochondrial fission but also distribution within neurons [181,182,183,184]. The modification of the actin cytoskeleton might also have an impact on the regulation of surface receptor distribution [124], which was highlighted in the present work.
The ATP produced by the mitochondria reaches the cytosol by its active transport through the adenine nucleotide translocator. To produce ATP, the processes of the TCA cycle and the respiratory chain/oxidative phosphorylation system act in conjunction. The last is located at the IMM. As a result of the mitochondrial respiratory chain deficiency, ATP production is reduced and ROS are increased, which leads to oxidative stress. This increase leads to modifications in protein, lipids, and DNA within the cells [185]. Amongst the modified lipids, the oxidation of cardiolipin from the IMM has been reported in the context of Parkinson’s disease [155], and its oxidation disrupts the normal binding of cytochrome c to the membrane [155]. Furthermore, ER is fundamental for providing membrane lipids to the mitochondria [186], highlighting again the importance of this crosstalk. Phosphatidic acid is considered a fusogenic lipid required for the fusion mediated by mitofusins [187]. Cardiolipin have been reported to control mitochondrial fission [188,189]. Interestingly, in the present work we found the expression of several cardiolipin binding proteins to be modified, which might impact the proper assembly of the mitochondrial membranes. Moreover, synaptic mitochondria present lower levels of cardiolipin, which has been pointed out as a lower threshold for the release of cytochrome c in the apoptotic process [164,190]. It has also been reported that synaptic mitochondria present higher sensitivity to the inhibition of the mitochondrial respiratory chain Complex I [191]. Detachment of cytochrome c from the membrane is necessary for cytochrome c release for apoptotic activation and cristae remodeling [27]. As discussed above, these fundamental processes have been emphasized by the high percentage of mitochondrial-shaping proteins found to be altered in the context of Parkinson’s disease in contrast with the proteins involved in fusion and fission.
The ER-mitochondrial connection is also important for the inflammatory response [192]. The activation of the inflammasome might occur under an oxidative stress scenario, i.e., Parkinson’s disease, where there is an increase in ROS production by the mitochondria [192]. Specific receptors are translocated to the ER-mitochondrial contact sites in response to inflammation [192]. Besides, relevant to the activation of this inflammasome is the VDAC channel located at the mitochondria. Knockdown of both VDAC1 and -2 abolishes the inflammasome formation [192]. Both channels were found to be downregulated in our study. Furthermore, these channels interact with Bcl-2 proteins, therefore enabling cell survival [192,193].
5. Conclusions
The DA neuron loss from the SN constitutes a hallmark of Parkinson’s disease. These neurons are known to be more susceptible than other DA neurons in the brain, and some of the referred sources for this vulnerability are associated with mitochondria. A more complex picture of the alterations of the mitochondria in Parkinson’s disease is arising in addition to the widely known deficit in the mitochondrial Complex I dysfunction. Through the so-called “mitochondrial life cycle”, these organelles can modulate their function and perform quality control. Accumulating evidence shows that there is a correlation between the morphology of these organelles and the cellular energy status. Increasing efforts have been made to associate the morphology of the mitochondria to its function. Importantly for a neurodegenerative disease such as Parkinson’s disease, in which the causes have been linked to mitochondrial dysfunction, this type of analysis will aid in advancing the field, both in the pathobiology of the disease and the search for new therapies.
By network analysis we have correlated the changes in differentially expressed mitochondrial-shaping proteins in the context of Parkinson’s disease with the corresponding biological pathways affected in the disease. One of the most striking findings is related to the process of cristae remodeling, since most of the mitochondrial-shaping proteins found to be altered in the context of Parkinson’s disease participate in the maintenance of cristae shape. Remarkably, this alteration is evident in different human disorders, including Parkinson’s disease. Since these structures regulate protein and lipid distribution as well as soluble molecules (i.e., ADP and cytochrome c), their alteration might have a direct impact on neuronal physiology and survival.
In our opinion, although it is clear in the cellular and animal models of the disease that mitochondrial morphology is altered, more studies from post mortem tissue from patients are needed, aiming at unravelling the alterations of the mitochondrial morphology more specifically related to the cristae shape in the context of Parkinson’s disease. These studies would provide new insights into the development of new therapies or aid in biomarkers discovery. Identification of the mitochondrial components that play a role in the process of cristae remodeling might also be fundamental for these purposes.
Acknowledgments
This work was financed by FEDER—Fundo Europeu de Desenvolvimento Regional funds through the COMPETE 2020—Operacional Programme for Competitiveness and Internationalisation (POCI), Portugal 2020, and by Portuguese funds through FCT—Fundação para a Ciência e a Tecnologia/ Ministério da Ciência, Tecnologia e Inovação in the framework of the projects “Institute for Research and Innovation in Health Sciences” (POCI-01-0145-FEDER-007274), iBiMED (UID/BIM/04501/2013) and UnIC (UID/IC/00051/2013) research units, the COST ACTION CA15203, and the Investigator Grant to Rui Vitorino (IF/00286/2015). Ana Freitas acknowledges FCT for her Ph.D. scholarship (SFRH/BD/111423/2015), as does Sofia C. Guimaraes (SFRH/BPD/122920/2016), and Miguel Aroso (SFRH/BPD/123261/2016). Sara Rocha was founded by the project Norte-01-0145-FEDER-000008 -Porto Neurosciences and Neurologic Disease Research Initiative at I3S, supported by Norte Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, through the European Regional Development Fund (FEDER)”.
Abbreviations
| ABPL | actin-binding-like protein |
| ACAD9 | acyl-CoA dehydrogenase family member 9 |
| ACP2 | acid phosphatase 2, lysosomal |
| ACTB | actin beta |
| ACTBL2 | actin, beta like 2 |
| ACTN1 | actinin alpha 1 |
| AD030 | ORF name for Mitochondrial Fission Factor |
| AD033 | ORF name for mitochondrial Fission Factor |
| ADP | adenosine diphosphate |
| AHAS | acetolactate synthase-like protein |
| ALB | albumin |
| ALDA | aldolase, fructose-bisphosphate A |
| ALDH1B1 | aldehyde dehydrogenase 1 family member B1 |
| ALDH5 | Aldehyde dehydrogenase 5 |
| ALDHX | Aldehyde dehydrogenase X |
| ALDOA | aldolase, fructose-bisphosphate A |
| ALS2CR3 | Amyotrophic lateral sclerosis 2 chromosomal region candidate gene 3 protein |
| ANT2 | Adenine nucleotide translocator 2 |
| ANX2 | annexin 2 |
| ANX2L4 | annexin A2 |
| ANX2LG | annexin A2 ligand |
| ANXA2 | annexin A2 |
| APOA1 | apolipoprotein A1 |
| APOO | apolipoprotein O |
| APOOL | apolipoprotein O like |
| ARALAR1/AGC1 | aspartate-glutamate carrier 1 |
| ARALAR2/AGC2 | aspartate-glutamate carrier 2 |
| ARH12 | Aplysia ras-related homolog 12 |
| ARHA | Ras Homolog Gene Family, Member A |
| ATP | adenosine triphosphate |
| ATP5A | ATP synthase subunit alpha |
| ATP5A1 | ATP synthase subunit alpha subunit 1 |
| ATP5AL2 | ATP synthase subunit alpha |
| ATP5B | ATP synthase subunit beta |
| ATP5C1 | ATP synthase subunit gamma subunit 1 |
| ATP5D | ATP synthase subunit delta |
| ATP5E | ATP synthase subunit epsilon |
| ATP5F1 | ATP synthase F(0) complex subunit B1 |
| ATP5G1 | ATP synthase F(0) complex subunit C1 |
| ATP5G2 | ATP synthase F(0) complex subunit C2 |
| ATP5G3 | ATP synthase F(0) complex subunit C3 |
| ATP5H | ATP synthase subunit d |
| ATP5I | ATP synthase subunit e |
| ATP5J | ATP synthase-coupling factor 6 |
| ATP5J2 | ATP synthase subunit f |
| ATP5K | ATP synthase subunit e |
| ATP5L | ATP synthase subunit g |
| ATP5O | ATP synthase subunit O |
| ATPI | ATP synthase inhibitory factor |
| ATPIF1 | ATP synthase inhibitory factor subunit 1 |
| ATPM | ATP synthase subunit alpha, mitochondrial |
| ATPMB | ATP synthase subunit beta, mitochondrial |
| ATPSB | ATP synthase subunit beta |
| BHAK | Bcl-2 homologous antagonist killer |
| BAK | BCL2 antagonist killer 1 |
| BAP | B-cell receptor-associated protein |
| BAP31 | B cell receptor associated protein 31 |
| BAX | BCL2 associated X, apoptosis regulator |
| BCAP31 | B cell receptor associated protein 31 |
| BCL2 | B-cell lymphoma 2, apoptosis regulator |
| BCL2A1 | BCL2 related protein A1 |
| BCL2L11 | BCL2 like protein 11 |
| BCL2L3 | BCL2 like protein 3 |
| BCL2L4 | BCL2 like protein 4 |
| BCL2L5 | BCL2 like protein 5 |
| BCL2L7 | BCL2 like protein 7 |
| BCR | Breakpoint cluster region protein |
| BFL1 | Bcl-2-related gene expressed in fetal liver |
| BID | BH3 interacting domain death agonist |
| BIK | BCL2 interacting killer |
| BIM | Bcl-2 Interacting Mediator of cell death |
| C11orf83 | chromosome 11 open reading frame 83 |
| C14orf151 | chromosome 14 open reading frame 151 |
| C14orf173 | chromosome 14 open reading frame 73 |
| C15orf13 | chromosome 15 open reading frame 13 |
| C19orf70 | chromosome 19 open reading frame 70 |
| C1orf151 | chromosome 1 open reading frame 151 |
| C1orf166 | chromosome 1 open reading frame 166 |
| C1QBP | complement C1q binding protein |
| C20orf52 | chromosome 20 open reading frame 52 |
| C2orf33 | chromosome 2 open reading frame 33 |
| C9orf54 | chromosome 9 open reading frame 54 |
| CAL1H | Calpactin I heavy polypeptide Protein |
| LPC2D | Lipocortin II |
| CAL1L | Calpactin-1 light chain |
| CALR | calreticulin |
| CCDC56 | Cytochrome c oxidase assembly factor 3 homolog |
| CCT5 | Chaperonin Containing TCP1 Subunit 5 |
| CCTE | Chaperonin Containing TCP1, Subunit epsilon |
| CDM | Caldesmon |
| CDN1 | synonym for Bcl-2 homologous antagonist/killer |
| CGI-106 | comparative gene identification 106 |
| CGI-135 | comparative gene identification 135 |
| CGI-51 | comparative gene identification 51 |
| CGI-61 | comparative gene identification 61 |
| CHCHD3 | coiled-coil-helix-coiled-coil-helix domain containing 3 |
| CLP11 | human gene encoding p11 |
| CMAR | Cell matrix adhesion regulator |
| COA3 | cytochrome c oxidase assembly factor 3 |
| COX4 | Cytochrome c oxidase subunit 4 isoform 1 |
| COX4I1 | cytochrome c oxidase subunit 4I1 |
| COX4I2 | Cytochrome c oxidase subunit 4 isoform 2 |
| COX5A | Cytochrome c oxidase subunit 5A |
| COX5B | Cytochrome c oxidase subunit 5B |
| COX6A1 | Cytochrome c oxidase subunit 6A1 |
| COX6A2 | Cytochrome c oxidase subunit 6A2 |
| COX6B1 | Cytochrome c oxidase subunit 6B1 |
| COX6B2 | Cytochrome c oxidase subunit 6B2 |
| COX6C | Cytochrome c oxidase subunit 6C |
| COX7A1 | Cytochrome c oxidase subunit 7A1 |
| COX7A2 | Cytochrome c oxidase subunit 7A2 |
| COX7B | Cytochrome c oxidase subunit 7B |
| COX7B2 | Cytochrome c oxidase subunit 7B2 |
| COX7C | Cytochrome c oxidase subunit 7C |
| COX8A | Cytochrome c oxidase subunit 8A |
| COX8C | cytochrome c oxidase subunit 8C |
| CPRP1 | synonym of Mitofusin 2 |
| CRTC | Calreticulin |
| CXorf33 | Chromosome X open reading frame 33 |
| CYC1 | Ubiquinol-Cytochrome-C Reductase Complex Cytochrome C1 Subunit |
| CYPA | Peptidyl-prolyl cis-trans isomerase A |
| DA | dopaminergic |
| DAPIT | Diabetes-associated protein in insulin-sensitive tissues |
| DDAH | dimethylarginine dimethylaminohydrolase |
| DDAH1 | dimethylarginine dimethylaminohydrolase 1 |
| DDOST | dolichyl-diphosphooligosaccharide--protein glycosyltransferase non-catalytic subunit |
| DHC1 | Cytoplasmic dynein 1 heavy chain 1 |
| DIC | Mitochondrial dicarboxylate carrier |
| DJ-1 | Protein/nucleic acid deglycase DJ-1 |
| DLP1 | dynamin like protein 1 |
| DNA | Deoxyribonucleic acid |
| DNAJC19 | DnaJ heat shock protein family (Hsp40) member C19 |
| DNCH1 | Cytoplasmic dynein 1 heavy chain 1 |
| DNCL | Dynein light chain 1 |
| DNECL | Cytoplasmic dynein 1 heavy chain 1 |
| DNM1L | dynamin 1 like |
| DNM2 | dynamin 2 |
| DRP1 | dynamin related protein 1 |
| DXS1357E | p28 synonym |
| DYHC | Cytoplasmic dynein 1 heavy chain 1 |
| DYN2 | dynamin 2 |
| DYNC1H1 | dynein cytoplasmic 1 heavy chain 1 |
| EC | Enzyme Commission number |
| EEF1A | eukaryotic translation elongation factor 1 alpha 1 |
| EEF1A1 | eukaryotic translation elongation factor 1 alpha 1 |
| EEF1B | Elongation factor 1-beta |
| EEF1B2 | Elongation factor 1-beta |
| EF1A | Elongation factor 1-alpha 1 |
| EF1B | Elongation factor 1-beta |
| EFE2 | endomyocardial fibroelastosis |
| EIF5A | eukaryotic translation initiation factor 5A |
| ER | endoplasmic reticulum |
| ERM | ezrin/moesin/radixin |
| ERP57 | Endoplasmic reticulum resident protein 57 |
| ERP60 | Endoplasmic reticulum resident protein 60 |
| FAM121A | Family With Sequence Similarity 121A |
| FAM121B | Family With Sequence Similarity 121A |
| FAM73A | Family With Sequence Similarity 73A |
| FAM73B | Family With Sequence Similarity 73B |
| FIS1 | fission, mitochondrial 1 |
| FKBP4 | FK506 binding protein 4 |
| FKBP52 | Peptidyl-prolyl cis-trans isomerase FKBP4 |
| FLN2 | filamin 2 |
| FLNC | filamin C |
| FLOT1 | flotillin 1 |
| FTSH1 | ATP-dependent zinc metalloprotease YME1L1 |
| FUBP1 | far upstream element binding protein 1 |
| FUNDC1 | FUN14 domain containing 1 |
| G4.5 | synonym of Tafazzin |
| GARS | glycyl-tRNA synthetase |
| GC1QBP | complement C1q binding protein |
| GC2 B415 | Glutamate carrier 2 |
| GDAP1 | ganglioside induced differentiation associated protein 1 |
| GIDE | Mitochondrial ubiquitin ligase activator of NFKB 1 |
| GIG20 | growth-inhibiting gene 20 |
| GIG42 | growth-inhibiting gene 42 |
| GL004 | synonym of MFF |
| GRP58 | 58 kDa glucose-regulated protein |
| GRP75 | 75 kDa glucose-regulated protein |
| GRP78 | 78 kDa glucose-regulated protein |
| GRS | Glasgow rearranged sequence |
| GSTK1 | glutathione S-transferase kappa 1 |
| GSTO1 | glutathione S-transferase omega 1 |
| GSTTLP28 | Glutathione S-transferase omega-1 |
| HABP1 | Hyaluronan Binding Protein 1 |
| HACBP | High Affinity Calcium-Binding Protein |
| HBEBP2 | HBEAG-binding protein 2 |
| HBPA1 | hematopoietic BCL2-related protein A1 |
| HC8 | human proteasome alpha-subunit C8 |
| HCVFTP2 | HCV F-Transactivated Protein 2 |
| HDCMD47P | synonym of Glutathione S-transferase Subunit 13 |
| hfzo1 | human fuzzy onions 1 |
| HIPPIE | Human Integrated Protein-Protein Interaction rEference web tool |
| HMP | synonym for inner membrane mitochondrial protein |
| HSC70 | Heat shock cognate 71 kDa protein |
| HSP27 | Heat shock protein beta-1 |
| HSP28 | Heat shock protein beta-1 |
| HSP60 | heat shock protein family D (Hsp60) |
| HSP73 | Heat shock cognate 71 kDa protein |
| HSP90AB1 | heat shock protein 90 alpha family class B member 1 |
| HSP90B | heat shock protein 90 alpha family class B |
| HSPA10 | Heat shock cognate 71 kDa protein |
| HSPA1L | heat shock protein family A (Hsp70) member 1 like |
| HSPA5 | heat shock protein family A (Hsp70) member 5 |
| HSPA8 | heat shock protein family A (Hsp70) member 8 |
| HSPA9 | heat shock protein family A (Hsp70) member 9 |
| HSPA9B | heat shock protein family A (Hsp70) member 9 |
| HSPB1 | heat shock protein family B (small) member 1 |
| HSPC009 | ORF name for Cytochrome c oxidase assembly factor 3 homolog |
| HSPC108 | ORF name for Stomatin-like protein 2 |
| HSPC2 | Heat shock protein HSP 90-beta |
| HSPC242 | ORF name for Mitochondrial fission process protein 1 |
| HSPC263 | ORF name for Ubiquitin thioesterase OTUB1 |
| HSPCB | Heat shock protein HSP 90-beta |
| HSPD1 | heat shock protein family D (Hsp60) member 1 |
| IF(1) | Inhibitor Of F(1)F(O)-ATPase |
| ILVBL | gene ilvB acetolactate synthase like |
| IMM | inner mitochondrial membrane |
| IMMT | inner membrane mitochondrial protein |
| IMS | intermembrane space |
| INF2 | protein inverted formin 2 |
| IPS1 | Interferon beta promoter stimulator protein 1 |
| KIAA0098 | synonym of CCT5 |
| KIAA0115 | synonym of DDOST |
| KIAA0214 | synonym of Mitofusin-2 |
| KIAA0313 | synonym of RAPGEF2 |
| KIAA0325 | synonym of DYNC1H1 |
| KIAA0348 | synonym of SYNJ2 |
| KIAA0491 | synonym of SH3GLB1 |
| KIAA0549 | synonym of TRAK2 |
| KIAA0567 | synonym of Dynamin-like 120 kDa protein |
| KIAA1042 | synonym of TRAK1 |
| KIAA1271 | synonym of MAVS |
| KIAA1848 | synonym of SH3GLB2 |
| LDHB | lactate dehydrogenase B |
| LEM6 | Ligand effect modulator 6 |
| LENG7 | Elongation factor 1-alpha 1 |
| LETM1 | leucine zipper and EF-hand containing transmembrane protein 1 |
| LGALS1 | Lectin galactoside-binding soluble 1 |
| LMN1 | Prelamin-A/C |
| LMNA | Lamin A |
| MADH2 | Mothers against decapentaplegic homolog 2 |
| MADR2 | Mad-related protein 2 Protein |
| MAP3K5 | Mitogen-activated protein kinase kinase kinase 5 |
| MAPL | Mitochondrial ubiquitin ligase activator of NFKB 1 |
| MARCH5 | membrane associated ring-CH-type finger 5 |
| MAVS | mitochondrial antiviral signaling protein |
| MCL1 | Induced myeloid leukemia cell differentiation protein Mcl-1 |
| MDH2 | malate dehydrogenase 2 |
| MFF | mitochondrial fission factor |
| MFN1 | mitofusin 1 |
| MFN2 | mitofusin 2 |
| MIC 27 | synonym for MICOS complex subunit MIC27 |
| MIC10 | synonym for MICOS complex subunit MI10 |
| MIC13 | synonym for MICOS complex subunit MIC13 |
| MIC19 | synonym for MICOS complex subunit MIC19 |
| MIC23 | synonym for MICOS complex subunit MIC23 |
| MIC26 | synonym for MICOS complex subunit MIC26 |
| MIC60 | synonym for MICOS complex subunit MIC60 |
| MICOS | mitochondrial contact site and cristae organizing system |
| MID49 | Mitochondrial dynamics protein MID49 |
| MID51 | Mitochondrial dynamics protein MID51 |
| MIEF1 | mitochondrial elongation factor 1 |
| MIEF2 | mitochondrial elongation factor 2 |
| MIG10 | Abnormal cell migration protein 10 |
| MIG5 | Abnormal cell migration protein 5 |
| MIGA1 | mitoguardin 1 |
| MIGA2 | mitoguardin 2 |
| MINOS1 | mitochondrial inner membrane organizing system 1 |
| MINOS2 | Mitochondrial Inner Membrane Organizing System 2 |
| MINOS3 | Mitochondrial Inner Membrane Organizing System 3 |
| Mito_shape | Mitochondrial shaping proteins |
| MITRAC12 | Cytochrome c oxidase assembly factor 3 homolog |
| MPP+ | 1-methyl-4-phenylpyridinium |
| MPRP1 | multidrug resistance protein 1 |
| MPTP | 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine |
| MT-ATP6 | Mitochondrially Encoded ATP Synthase 6 |
| MT-ATP8 | Mitochondrially Encoded ATP Synthase 8 |
| MT-CO1 | Mitochondrially Encoded Cytochrome C Oxidase I |
| MT-CO2 | Mitochondrially Encoded Cytochrome C Oxidase II |
| MT-CO3 | Mitochondrially Encoded Cytochrome C Oxidase III |
| MT-CYB | Mitochondrially Encoded Cytochrome B |
| MTFP1 | mitochondrial fission process 1 |
| mt-HSP70 | mitochondrial heat shock protein family A (Hsp70) |
| MTP18 | Mitochondrial fission process protein 1 |
| MUL1 | mitochondrial E3 ubiquitin protein ligase 1 |
| MULAN | Mitochondrial ubiquitin ligase activator of NFKB 1 |
| My022 | ORF name for Mitochondrial fission process protein 1 |
| My025 | ORF name for MICOS complex subunit MIC26 |
| My032 | ORF name for ATP synthase subunit d |
| MYL6 | myosin light chain 6 |
| NAD | nicotinamide adenine dinucleotide oxidized |
| NADH | nicotinamide adenine dinucleotide reduced |
| NBK | Bcl-2-interacting killer |
| NDUFA10 | NADH:ubiquinone oxidoreductase subunit A10 |
| NDUFA11 | NADH:ubiquinone oxidoreductase subunit A11 |
| NDUFA4 | NADH Dehydrogenase (Ubiquinone) 1 Alpha Subcomplex, 4 |
| NDUFS1 | NADH:ubiquinone oxidoreductase core subunit S1 |
| NDUFS3 | NADH:ubiquinone oxidoreductase core subunit S3 |
| NEDD8 | neural precursor cell expressed, developmentally down-regulated 8 |
| NFE2L2 | nuclear factor, erythroid 2 like 2 |
| NFKB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NHERF | Na(+)/H(+) exchange regulatory cofactor NHE-RF1 |
| NHERF1 | Na(+)/H(+) exchange regulatory cofactor NHE-RF1 |
| NHERF-1 protein | Na(+)/H(+) exchange regulatory cofactor NHE-RF1 |
| NIMA | never in mitosis gene a |
| NO | nitric oxide |
| Nox1 | NADPH oxidase 1 |
| NPM | nucleophosmin |
| NPM1 | nucleophosmin 1 |
| NRAPGEP | Rap guanine nucleotide exchange factor 2 |
| NRF1 | nuclear respiratory factor 1 |
| NRF2 | Nuclear factor erythroid 2-related factor 2 |
| OAT | ornithine aminotransferase |
| OGDH | oxoglutarate dehydrogenase |
| OIP106 | O-linked N-acetylglucosamine transferase interacting protein 106 |
| OK/SW-cl.110 | ORF name for Phosphoglycerate kinase 1 |
| OK/SW-cl.56 | ORF name for Tubulin beta chain |
| OK/SW-cl.82 | ORF name for 40S ribosomal protein S15a |
| OMA1 | Overlapping Activity With M-AAA Protease |
| OMM | outer mitochondrial membrane |
| OPA1 | Optic Atrophy Protein 1 |
| OST48 OK/SW-cl.45 | synomym for Dolichyl-diphosphooligosaccharide--protein glycosyltransferase 48 kDa subunit |
| OTB1 | Ubiquitin thioesterase OTUB1 |
| OTU1 | Ubiquitin thioesterase OTUB1 |
| OTUB1 | OTU deubiquitinase, ubiquitin aldehyde binding 1 |
| OXPHOS | oxidative phosphorylation |
| PARK2 | E3 ubiquitin-protein ligase parkin |
| PARL | presenilin associated rhomboid like |
| PD | Parkinson’s disease |
| PD04912 | ORF name for Up-regulated during skeletal muscle growth protein 5 |
| PDIA3 | protein disulfide isomerase family A member 3 |
| PDZGEF1 | Rap guanine nucleotide exchange factor 2 |
| PERC | Peroxisome proliferator-activated receptor gamma coactivator 1-beta |
| PGAM5 | Serine/threonine-protein phosphatase PGAM5 |
| PGC1 | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PGC1A | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PGC1B | Peroxisome proliferator-activated receptor gamma coactivator 1-beta |
| PGK1 | phosphoglycerate kinase 1 |
| PGKA | Phosphoglycerate kinase 1 |
| PGN | paraplegin |
| PHB | prohibitin |
| PHB2 | prohibitin 2 |
| PIG4 | ORF name for MICOS complex subunit MIC60 |
| PIG52 | ORF name for MICOS complex subunit MIC60 |
| PIN1 | peptidylprolyl cis/trans isomerase, NIMA-interacting 1 |
| PINK1 | PTEN-induced putative kinase 1 |
| PLD6 | phospholipase D family member 6 |
| PP578 | ORF name for Endophilin-B2 |
| PPARGC1 | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PPARGC1A | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PPARGC1B | Peroxisome proliferator-activated receptor gamma coactivator 1-beta |
| PPIA | peptidylprolyl isomerase A |
| PRDX4 | peroxiredoxin 4 |
| PRELI | Protein Of Relevant Evolutionary And Lymphoid Interest |
| PRELID1 | PRELI domain-containing protein 1 |
| PRI | synonym for Ribonuclease inhibitor |
| PRKN | parkin RBR E3 ubiquitin protein ligase |
| PRO0903 | ORF name for Serum albumin |
| PRO1708 | ORF name for Serum albumin |
| PRO2044 | ORF name for Serum albumin |
| PRO2207 | ORF name for Presenilins-associated rhomboid-like protein |
| PRO2619 | ORF name for Serum albumin |
| PRO2675 | ORF name for Serum albumin |
| PSARL | Presenilins-associated rhomboid-like protein |
| PSC8 | Proteasome component C8 |
| PSEC0112 | ORF name for Mitoguardin 2 |
| PSMA3 | proteasome subunit alpha 3 |
| PTPN5 | protein tyrosine phosphatase, non-receptor type 5 |
| QIL1 | synonym for Chromosome 19 Open Reading Frame 70 |
| RAB14 | Ras-related protein Rab-14 |
| RAB2 | Ras-related protein Rab2 |
| RAB2A | Ras-related protein Rab-2A |
| RAC1 | Ras-related C3 botulinum toxin substrate 1 |
| RAPGEF2 | Rap guanine nucleotide exchange factor 2 |
| REA | synonym for Prohibitin-2 |
| RHO12 | ras homolog family member |
| RHOA | ras homolog family member A |
| RING-type E3 | really interesting new gene type E3 |
| RNF153 | Ring Finger Protein 153 |
| RNF218 | Ring Finger Protein 218 |
| RNH | Ribonuclease inhibitor |
| RNH1 | ribonuclease/angiogenin inhibitor 1 |
| ROMO1 | reactive oxygen species modulator 1 |
| ROS | reactive oxygen species |
| RPN1 | Ribophorin I |
| RPN2 | ribophorin II |
| RPS15A | ribosomal protein S15a |
| RPS3, OK/SW-cl.26 | symbol and ORF name for 40S ribosomal protein S3 |
| S100A10 | S100 calcium binding protein A10 |
| SAM50 | Sorting and assembly machinery component 50 homolog |
| SAMM50 | Sorting and assembly machinery component 50 homolog |
| SBBI12 | ORF name for PRELI domain-containing protein 1 |
| SBP | selenium binding protein |
| SELENBP1 | selenium binding protein 1 |
| SF2P32 | nuclear splicing factor |
| SFXN1 | sideroflexin 1 |
| SH3 | SRC Homology 3 Domain |
| SH3GLB1 | SH3 domain containing GRB2 like, endophilin B1 |
| SH3GLB2 | SH3 domain containing GRB2 like, endophilin B2 |
| SIR2L | SIR2-like protein |
| SIR2L2 | SIR2-like protein 2 |
| SIRT2 | sirtuin 2 |
| SLC20A4 | solute carrier family 20 member 4 |
| Slc25A | solute carrier family 25 |
| SLC25A10 | solute carrier family 25 member 10 |
| SLC25A11 | solute carrier family 25 member 11 |
| SLC25A12 | solute carrier family 25 member 12 |
| SLC25A13 | solute carrier family 25 member 13 |
| SLC25A18 | solute carrier family 25 member 18 |
| SLC25A38 | solute carrier family 25 member 38 |
| SLC9A3R1 | solute carrier family 9 (sodium/hydrogen exchanger), member 3 regulator 1 |
| SLP2 | Stomatin-like protein 2 |
| SMAD2 | Mothers against decapentaplegic homolog 2 |
| SMCR7 | Smith-Magenis Syndrome Chromosomal Region Candidate Gene 7 Protein |
| SMCR7L | Smith-Magenis Syndrome Chromosomal Region Candidate Gene 7 Protein-like |
| SN | Substantia nigra |
| SPG7 | Paraplegin |
| SSBP | single stranded DNA binding protein |
| SSBP1 | single stranded DNA binding protein 1 |
| STOML2 | stomatin like 2 |
| SYNJ2 | synaptojanin 2 |
| TAZ | tafazzin |
| TC25 | Ras-Like Protein TC25 |
| TCA | tricarboxylic acid cycle |
| TCF6 | Transcription factor |
| TCF6L2 | Transcription Factor 6-Like 2 |
| TCP-1-epsilon | T-complex protein 1 subunit epsilon |
| TFAM | transcription factor A, mitochondrial |
| TIM14 | Mitochondrial Import Inner Membrane Translocase Subunit TIM14 |
| TIMM14 | Translocase Of Inner Mitochondrial Membrane 14 |
| TMSA | Tropomyosin alpha-1 chain |
| TMSB | tropomyosin Beta |
| TPD52 | tumor protein D52 |
| TPM1 | tropomyosin 1 |
| TPM2 | tropomyosin 2 |
| TPM3 | tropomyosin 3 |
| TPM4 | tropomyosin 4 |
| TRAK1 | trafficking kinesin protein 1 |
| TRAK2 | trafficking kinesin protein 2 |
| TRG3 | transformation-related gene 3 |
| TTC11 | tetratricopeptide Repeat Domain 11 |
| TUBA1A | tubulin alpha 1a |
| TUBA3 | tubulin alpha-3 chain |
| TUBB | tubulin beta class I |
| TUBB2C | Tubulin beta-4B chain |
| TUBB4B | tubulin beta 4B class IVb |
| TUBB5 | Tubulin beta chain |
| TUFM | Tu translation elongation factor, mitochondrial |
| UniProt | Universal Protein Resource |
| UNQ1866/PRO4302 | ORF name for MICOS complex subunit MIC26 |
| UNQ1868/PRO4304 | ORF name for ATP-dependent zinc metalloprotease YME1L1 |
| UNQ655/PRO1286 | ORF name for Ubiquinol-cytochrome-c reductase complex assembly factor 3 |
| UNQ696/PRO1341 | ORF name for Serum albumin |
| UNQ8193/PRO23204 | ORF for MICOS complex subunit MIC27 |
| UQBP | Ubiquinol-cytochrome c reductase complex 14 kDa protein |
| UQCC3 | ubiquinol-cytochrome c reductase complex assembly factor 3 |
| UQCR10 | Ubiquinol-Cytochrome C Reductase, Complex III Subunit X |
| UQCR11 | Ubiquinol-Cytochrome C Reductase, Complex III Subunit XI |
| UQCRB | ubiquinol-cytochrome c reductase binding protein |
| UQCRC1 | ubiquinol-cytochrome c reductase core protein 1 |
| UQCRC2 | ubiquinol-cytochrome c reductase core protein 2 |
| UQCRFS1 | ubiquinol-cytochrome c reductase, Rieske iron-sulfur polypeptide 1 |
| UQCRFS1 | ubiquinol-cytochrome c reductase, Rieske iron-sulfur polypeptide 1 |
| UQCRFS1P1 | ubiquinol-cytochrome c reductase, Rieske iron-sulfur polypeptide 1 pseudogene 1 |
| UQCRFSL1 | Ubiquinol-cytochrome c reductase Rieske iron-sulfur subunit pseudogene 1 |
| UQCRH | ubiquinol-cytochrome c reductase hinge protein |
| UQCRQ | ubiquinol-cytochrome c reductase complex ubiquinone-binding protein QP-C |
| USMG5 | Up-regulated during skeletal muscle growth protein 5 |
| VAT1 | vesicle amine transport 1 |
| VCP | valosin containing protein |
| VDAC1 | Voltage-dependent anion-selective channel protein 1 |
| VDAC2 | voltage dependent anion channel 2 |
| VDAC3 | voltage dependent anion channel 3 |
| VDAC | Voltage-dependent anion-selective channel |
| VIM | vimentin |
| VISA | Virus-induced-signaling adapter |
| YME1L | YME1-like protein 1 |
| YME1L1 | YME1-like protein 1 |
| YWHAE | tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein epsilon |
| YWHAZ | tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein zeta |
Supplementary Materials
The following are available online at www.mdpi.com/2076-3921/7/1/1/s1, Table S1: List of proteins found modified in different proteomics-based approaches in the context of Parkinson’s disease; Table S2: List of the binding partners of the “mitochondrial-shaping proteins found modified in Parkinson’s disease”; Table S3: List of the binding partners of the “mitochondrial-shaping proteins found modified in different proteomics-based approaches in the context of Parkinson’s disease according to the Human Integrated Protein-Protein Interaction reference” that are modified in Parkinson’s disease.
Author Contributions
Maria Gomez-Lazaro, Miguel Aroso, and Rui Vitorino conceived and designed the workflow of the paper; Maria Gomez-Lazaro, Sara Rocha, Sofia C. Guimaraes, Miguel Aroso, and Ana Freitas performed the literature search, collected the data meeting the criteria, performed the bioinformatics analysis and figures, and analyzed the data; Maria Gomez-Lazaro, Sara Rocha, Sofia C. Guimaraes, and Miguel Aroso wrote the paper; all authors revised the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Kasahara A., Scorrano L. Mitochondria: From cell death executioners to regulators of cell differentiation. Trends Cell Biol. 2014;24:761–770. doi: 10.1016/j.tcb.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Anesti V., Scorrano L. The relationship between mitochondrial shape and function and the cytoskeleton. Biochim. Biophys. Acta. 2006;1757:692–699. doi: 10.1016/j.bbabio.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 3.Pernas L., Scorrano L. Mito-morphosis: Mitochondrial fusion, fission, and cristae remodeling as key mediators of cellular function. Annu. Rev. Physiol. 2016;78:505–531. doi: 10.1146/annurev-physiol-021115-105011. [DOI] [PubMed] [Google Scholar]
- 4.Gao J., Wang L., Liu J., Xie F., Su B., Wang X. Abnormalities of mitochondrial dynamics in neurodegenerative diseases. Antioxidants. 2017;6:25. doi: 10.3390/antiox6020025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muangpaisan W., Mathews A., Hori H., Seidel D. A systematic review of the worldwide prevalence and incidence of Parkinson’s disease. J. Med. Assoc. Thail. 2011;94:749–755. [PubMed] [Google Scholar]
- 6.Antony P.M., Diederich N.J., Kruger R., Balling R. The hallmarks of Parkinson’s disease. FEBS J. 2013;280:5981–5993. doi: 10.1111/febs.12335. [DOI] [PubMed] [Google Scholar]
- 7.Schapira A.H., Cooper J.M., Dexter D., Jenner P., Clark J.B., Marsden C.D. Mitochondrial complex I deficiency in Parkinson’s disease. Lancet. 1989;1:1269. doi: 10.1016/S0140-6736(89)92366-0. [DOI] [PubMed] [Google Scholar]
- 8.Schapira A.H., Cooper J.M., Dexter D., Clark J.B., Jenner P., Marsden C.D. Mitochondrial complex I deficiency in Parkinson’s disease. J. Neurochem. 1990;54:823–827. doi: 10.1111/j.1471-4159.1990.tb02325.x. [DOI] [PubMed] [Google Scholar]
- 9.Haylett W., Swart C., van der Westhuizen F., van Dyk H., van der Merwe L., van der Merwe C., Loos B., Carr J., Kinnear C., Bardien S. Altered mitochondrial respiration and other features of mitochondrial function in parkin-mutant fibroblasts from Parkinson’s disease patients. Parkinson’s Dis. 2016;2016:1819209. doi: 10.1155/2016/1819209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hao L.Y., Giasson B.I., Bonini N.M. Dj-1 is critical for mitochondrial function and rescues pink1 loss of function. Proc. Natl. Acad. Sci. USA. 2010;107:9747–9752. doi: 10.1073/pnas.0911175107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmad T., Aggarwal K., Pattnaik B., Mukherjee S., Sethi T., Tiwari B.K., Kumar M., Micheal A., Mabalirajan U., Ghosh B., et al. Computational classification of mitochondrial shapes reflects stress and redox state. Cell Death Dis. 2013;4:e461. doi: 10.1038/cddis.2012.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haddad D., Nakamura K. Understanding the susceptibility of dopamine neurons to mitochondrial stressors in Parkinson’s disease. FEBS Lett. 2015;589:3702–3713. doi: 10.1016/j.febslet.2015.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Apweiler R., Bairoch A., Wu C.H., Barker W.C., Boeckmann B., Ferro S., Gasteiger E., Huang H., Lopez R., Magrane M., et al. Uniprot: The universal protein knowledgebase. Nucleic Acids Res. 2017;45:D158–D169. doi: 10.1093/nar/gkh131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friedman J.R., Mourier A., Yamada J., McCaffery J.M., Nunnari J. MICOS coordinates with respiratory complexes and lipids to establish inner mitochondrial membrane architecture. eLife. 2015;4 doi: 10.7554/eLife.07739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ikon N., Ryan R.O. Cardiolipin and mitochondrial cristae organization. Biochim. Biophys. Acta. 2017;1859:1156–1163. doi: 10.1016/j.bbamem.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koob S., Barrera M., Anand R., Reichert A.S. The non-glycosylated isoform of MIC26 is a constituent of the mammalian MICOS complex and promotes formation of crista junctions. Biochimi. Biophys. Acta. 2015;1853:1551–1563. doi: 10.1016/j.bbamcr.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Wilkens V., Kohl W., Busch K. Restricted diffusion of OXPHOS complexes in dynamic mitochondria delays their exchange between cristae and engenders a transitory mosaic distribution. J. Cell Sci. 2013;126:103–116. doi: 10.1242/jcs.108852. [DOI] [PubMed] [Google Scholar]
- 18.Cogliati S., Enriquez J.A., Scorrano L. Mitochondrial cristae: Where beauty meets functionality. Trends Biochem. Sci. 2016;41:261–273. doi: 10.1016/j.tibs.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 19.van der Bliek A.M., Shen Q., Kawajiri S. Mechanisms of mitochondrial fission and fusion. Cold Spring Harb. Perspect. Biol. 2013;5:a011072. doi: 10.1101/cshperspect.a011072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faccenda D., Tan C.H., Seraphim A., Duchen M.R., Campanella M. IF1 limits the apoptotic-signalling cascade by preventing mitochondrial remodelling. Cell Death Differ. 2013;20:686–697. doi: 10.1038/cdd.2012.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luna-Vargas M.P., Chipuk J.E. Physiological and pharmacological control of BAK, BAX, and beyond. Trends Cell Biol. 2016;26:906–917. doi: 10.1016/j.tcb.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campello S., Scorrano L. Mitochondrial shape changes: Orchestrating cell pathophysiology. EMBO Rep. 2010;11:678–684. doi: 10.1038/embor.2010.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scorrano L. Opening the doors to cytochrome c: Changes in mitochondrial shape and apoptosis. Int. J. Biochem. Cell Biol. 2009;41:1875–1883. doi: 10.1016/j.biocel.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 24.Valero J.G., Cornut-Thibaut A., Juge R., Debaud A.L., Gimenez D., Gillet G., Bonnefoy-Berard N., Salgado J., Salles G., Aouacheria A., et al. Micro-calpain conversion of antiapoptotic Bfl-1 (BCL2A1) into a prodeath factor reveals two distinct alpha-helices inducing mitochondria-mediated apoptosis. PLoS ONE. 2012;7:e38620. doi: 10.1371/journal.pone.0038620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wasilewski M., Scorrano L. The changing shape of mitochondrial apoptosis. Trends Endocrinol. Metab. 2009;20:287–294. doi: 10.1016/j.tem.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Yamaguchi R., Lartigue L., Perkins G., Scott R.T., Dixit A., Kushnareva Y., Kuwana T., Ellisman M.H., Newmeyer D.D. Opa1-mediated cristae opening is Bax/Bak and BH3 dependent, required for apoptosis, and independent of Bak oligomerization. Mol. Cell. 2008;31:557–569. doi: 10.1016/j.molcel.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scorrano L., Ashiya M., Buttle K., Weiler S., Oakes S.A., Mannella C.A., Korsmeyer S.J. A distinct pathway remodels mitochondrial cristae and mobilizes cytochrome c during apoptosis. Dev. Cell. 2002;2:55–67. doi: 10.1016/S1534-5807(01)00116-2. [DOI] [PubMed] [Google Scholar]
- 28.Germain M., Mathai J.P., McBride H.M., Shore G.C. Endoplasmic reticulum Bik initiates DRP1-regulated remodelling of mitochondrial cristae during apoptosis. EMBO J. 2005;24:1546–1556. doi: 10.1038/sj.emboj.7600592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ong S.B., Kalkhoran S.B., Hernandez-Resendiz S., Samangouei P., Ong S.G., Hausenloy D.J. Mitochondrial-shaping proteins in cardiac health and disease—The long and the short of it! Cardiovasc. Drugs Ther. Spons. Int. Soc. Cardiovasc. Pharmacother. 2017;31:87–107. doi: 10.1007/s10557-016-6710-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ban-Ishihara R., Tomohiro-Takamiya S., Tani M., Baudier J., Ishihara N., Kuge O. COX assembly factor ccdc56 regulates mitochondrial morphology by affecting mitochondrial recruitment of Drp1. FEBS Lett. 2015;589:3126–3132. doi: 10.1016/j.febslet.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 31.Richter-Dennerlein R., Korwitz A., Haag M., Tatsuta T., Dargazanli S., Baker M., Decker T., Lamkemeyer T., Rugarli E.I., Langer T. DNAJC19, a mitochondrial cochaperone associated with cardiomyopathy, forms a complex with prohibitins to regulate cardiolipin remodeling. Cell Metab. 2014;20:158–171. doi: 10.1016/j.cmet.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 32.Davey K.M., Parboosingh J.S., McLeod D.R., Chan A., Casey R., Ferreira P., Snyder F.F., Bridge P.J., Bernier F.P. Mutation of DNAJC19, a human homologue of yeast inner mitochondrial membrane co-chaperones, causes DCMA syndrome, a novel autosomal recessive Barth syndrome-like condition. J. Med. Genet. 2006;43:385–393. doi: 10.1136/jmg.2005.036657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee J.E., Westrate L.M., Wu H., Page C., Voeltz G.K. Multiple dynamin family members collaborate to drive mitochondrial division. Nature. 2016;540:139–143. doi: 10.1038/nature20555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen M., Chen Z., Wang Y., Tan Z., Zhu C., Li Y., Han Z., Chen L., Gao R., Liu L., et al. Mitophagy receptor FUNDC1 regulates mitochondrial dynamics and mitophagy. Autophagy. 2016;12:689–702. doi: 10.1080/15548627.2016.1151580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu L., Feng D., Chen G., Chen M., Zheng Q., Song P., Ma Q., Zhu C., Wang R., Qi W., et al. Mitochondrial outer-membrane protein FUNDC1 mediates hypoxia-induced mitophagy in mammalian cells. Nat. Cell Biol. 2012;14:177–185. doi: 10.1038/ncb2422. [DOI] [PubMed] [Google Scholar]
- 36.Gomes L.C., Scorrano L. Mitochondrial morphology in mitophagy and macroautophagy. Biochim. Biophys. Acta. 2013;1833:205–212. doi: 10.1016/j.bbamcr.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 37.John G.B., Shang Y., Li L., Renken C., Mannella C.A., Selker J.M., Rangell L., Bennett M.J., Zha J. The inner mitochondrial membrane protein mitofilin controls cristae morphology. Mol. Biol. Cell. 2005;16:1543–1554. doi: 10.1091/mbc.E04-08-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Korobova F., Ramabhadran V., Higgs H.N. An actin-dependent step in mitochondrial fission mediated by the ER-associated formin INF2. Science. 2013;339:464–467. doi: 10.1126/science.1228360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dimmer K.S., Navoni F., Casarin A., Trevisson E., Endele S., Winterpacht A., Salviati L., Scorrano L. LETM1, deleted in Wolf-Hirschhorn syndrome is required for normal mitochondrial morphology and cellular viability. Hum. Mol. Genet. 2008;17:201–214. doi: 10.1093/hmg/ddm297. [DOI] [PubMed] [Google Scholar]
- 40.Koshiba T. Mitochondrial-mediated antiviral immunity. Biochim. Biophys. Acta. 2013;1833:225–232. doi: 10.1016/j.bbamcr.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 41.Perciavalle R.M., Stewart D.P., Koss B., Lynch J., Milasta S., Bathina M., Temirov J., Cleland M.M., Pelletier S., Schuetz J.D., et al. Anti-apoptotic MCL-1 localizes to the mitochondrial matrix and couples mitochondrial fusion to respiration. Nat. Cell Biol. 2012;14:575–583. doi: 10.1038/ncb2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morciano G., Giorgi C., Balestra D., Marchi S., Perrone D., Pinotti M., Pinton P. MCL-1 involvement in mitochondrial dynamics is associated with apoptotic cell death. Mol. Biol. Cell. 2016;27:20–34. doi: 10.1091/mbc.E15-01-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen H., Detmer S.A., Ewald A.J., Griffin E.E., Fraser S.E., Chan D.C. Mitofusins Mfn1 and Mfn2 coordinately regulate mitochondrial fusion and are essential for embryonic development. J. Cell Biol. 2003;160:189–200. doi: 10.1083/jcb.200211046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Y., Liu X., Bai J., Tian X., Zhao X., Liu W., Duan X., Shang W., Fan H.Y., Tong C. Mitoguardin regulates mitochondrial fusion through mitopld and is required for neuronal homeostasis. Mol. Cell. 2016;61:111–124. doi: 10.1016/j.molcel.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 45.Wai T., Langer T. Mitochondrial dynamics and metabolic regulation. Trends Endocrinol. Metab. 2016;27:105–117. doi: 10.1016/j.tem.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 46.Yin X., Manczak M., Reddy P.H. Mitochondria-targeted molecules MitoQ and SS31 reduce mutant huntingtin-induced mitochondrial toxicity and synaptic damage in Huntington’s disease. Hum. Mol. Genet. 2016;25:1739–1753. doi: 10.1093/hmg/ddw045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dinkova-Kostova A.T., Abramov A.Y. The emerging role of Nrf2 in mitochondrial function. Free Radic. Biol. Med. 2015;88:179–188. doi: 10.1016/j.freeradbiomed.2015.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bereiter-Hahn J., Jendrach M. Mitochondrial dynamics. Int. Rev. Cell Mol. Biol. 2010;284:1–65. doi: 10.1016/S1937-6448(10)84001-8. [DOI] [PubMed] [Google Scholar]
- 49.Dabrowska A., Venero J.L., Iwasawa R., Hankir M.K., Rahman S., Boobis A., Hajji N. PGC-1alpha controls mitochondrial biogenesis and dynamics in lead-induced neurotoxicity. Aging. 2015;7:629–647. doi: 10.18632/aging.100790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patten D.A., Wong J., Khacho M., Soubannier V., Mailloux R.J., Pilon-Larose K., MacLaurin J.G., Park D.S., McBride H.M., Trinkle-Mulcahy L., et al. Opa1-dependent cristae modulation is essential for cellular adaptation to metabolic demand. EMBO J. 2014;33:2676–2691. doi: 10.15252/embj.201488349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hall A.R., Burke N., Dongworth R.K., Hausenloy D.J. Mitochondrial fusion and fission proteins: Novel therapeutic targets for combating cardiovascular disease. Br. J. Pharmacol. 2014;171:1890–1906. doi: 10.1111/bph.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang Z., Jiang H., Chen S., Du F., Wang X. The mitochondrial phosphatase PGAM5 functions at the convergence point of multiple necrotic death pathways. Cell. 2012;148:228–243. doi: 10.1016/j.cell.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 53.Merkwirth C., Dargazanli S., Tatsuta T., Geimer S., Lower B., Wunderlich F.T., von Kleist-Retzow J.C., Waisman A., Westermann B., Langer T. Prohibitins control cell proliferation and apoptosis by regulating opa1-dependent cristae morphogenesis in mitochondria. Genes Dev. 2008;22:476–488. doi: 10.1101/gad.460708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buhlman L., Damiano M., Bertolin G., Ferrando-Miguel R., Lombes A., Brice A., Corti O. Functional interplay between parkin and Drp1 in mitochondrial fission and clearance. Biochim. Biophys. Acta. 2014;1843:2012–2026. doi: 10.1016/j.bbamcr.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 55.LeBleu V.S., O’Connell J.T., Gonzalez Herrera K.N., Wikman H., Pantel K., Haigis M.C., de Carvalho F.M., Damascena A., Domingos Chinen L.T., Rocha R.M., et al. PGC-1alpha mediates mitochondrial biogenesis and oxidative phosphorylation in cancer cells to promote metastasis. Nat. Cell Biol. 2014;16:992–1003. doi: 10.1038/ncb3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shao D., Liu Y., Liu X., Zhu L., Cui Y., Cui A., Qiao A., Kong X., Chen Q., Gupta N., et al. PGC-1 beta-regulated mitochondrial biogenesis and function in myotubes is mediated by Nrf-1 and ERR alpha. Mitochondrion. 2010;10:516–527. doi: 10.1016/j.mito.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 57.Sesaki H., Dunn C.D., Iijima M., Shepard K.A., Yaffe M.P., Machamer C.E., Jensen R.E. Ups1p, a conserved intermembrane space protein, regulates mitochondrial shape and alternative topogenesis of Mgm1p. J. Cell Biol. 2006;173:651–658. doi: 10.1083/jcb.200603092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hartmann B., Wai T., Hu H., MacVicar T., Musante L., Fischer-Zirnsak B., Stenzel W., Graf R., van den Heuvel L., Ropers H.H., et al. Homozygous YME1L1 mutation causes mitochondriopathy with optic atrophy and mitochondrial network fragmentation. eLife. 2016;5:e16078. doi: 10.7554/eLife.16078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gomes L.C., Di Benedetto G., Scorrano L. During autophagy mitochondria elongate, are spared from degradation and sustain cell viability. Nat. Cell Biol. 2011;13:589–598. doi: 10.1038/ncb2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shaltouki A., Sivapatham R., Pei Y., Gerencser A.A., Momcilovic O., Rao M.S., Zeng X. Mitochondrial alterations by PARKIN in dopaminergic neurons using PARK2 patient-specific and PARK2 knockout isogenic IPSC lines. Stem Cell Rep. 2015;4:847–859. doi: 10.1016/j.stemcr.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Norton M., Ng A.C., Baird S., Dumoulin A., Shutt T., Mah N., Andrade-Navarro M.A., McBride H.M., Screaton R.A. ROMO1 is an essential redox-dependent regulator of mitochondrial dynamics. Sci. Signal. 2014;7:ra10. doi: 10.1126/scisignal.2004374. [DOI] [PubMed] [Google Scholar]
- 62.Karbowski M., Jeong S.Y., Youle R.J. Endophilin B1 is required for the maintenance of mitochondrial morphology. J. Cell Biol. 2004;166:1027–1039. doi: 10.1083/jcb.200407046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang Y.H., Wang J.Q., Wang Q., Wang Y., Guo C., Chen Q., Chai T., Tang T.S. Endophilin B2 promotes inner mitochondrial membrane degradation by forming heterodimers with endophilin B1 during mitophagy. Sci. Rep. 2016;6:25153. doi: 10.1038/srep25153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang C., Shi Z., Zhang L., Zhou Z., Zheng X., Liu G., Bu G., Fraser P.E., Xu H., Zhang Y.W. Appoptosin interacts with mitochondrial outer-membrane fusion proteins and regulates mitochondrial morphology. J. Cell Sci. 2016;129:994–1002. doi: 10.1242/jcs.176792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kumar S., Pan C.C., Shah N., Wheeler S.E., Hoyt K.R., Hempel N., Mythreye K., Lee N.Y. Activation of mitofusin2 by smad2-RIN1 complex during mitochondrial fusion. Mol. Cell. 2016;62:520–531. doi: 10.1016/j.molcel.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nemoto Y., De Camilli P. Recruitment of an alternatively spliced form of synaptojanin 2 to mitochondria by the interaction with the PDZ domain of a outer mitochondrial membrane protein. EMBO J. 1999;18:2991–3006. doi: 10.1093/emboj/18.11.2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gonzalvez F., D’Aurelio M., Boutant M., Moustapha A., Puech J.P., Landes T., Arnaune-Pelloquin L., Vial G., Taleux N., Slomianny C., et al. Barth syndrome: Cellular compensation of mitochondrial dysfunction and apoptosis inhibition due to changes in cardiolipin remodeling linked to tafazzin (TAZ) gene mutation. Biochim. Biophys. Acta. 2013;1832:1194–1206. doi: 10.1016/j.bbadis.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 68.Acehan D., Xu Y., Stokes D.L., Schlame M. Comparison of lymphoblast mitochondria from normal subjects and patients with barth syndrome using electron microscopic tomography. Lab. Investig. J. Tech. Methods Pathol. 2007;87:40–48. doi: 10.1038/labinvest.3700480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Desmurs M., Foti M., Raemy E., Vaz F.M., Martinou J.C., Bairoch A., Lane L. C11orf83, a mitochondrial cardiolipin-binding protein involved in bc1 complex assembly and supercomplex stabilization. Mol. Cell. Biol. 2015;35:1139–1156. doi: 10.1128/MCB.01047-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Eura Y., Ishihara N., Oka T., Mihara K. Identification of a novel protein that regulates mitochondrial fusion by modulating mitofusin (Mfn) protein function. J. Cell Sci. 2006;119:4913–4925. doi: 10.1242/jcs.03253. [DOI] [PubMed] [Google Scholar]
- 71.Oliveros J.C. Venny. [(accessed on 29 August 2017)]; An Interactive Tool for Comparing Lists with Venn’s Diagrams. Available online: http://bioinfogp.cnb.csic.es/tools/venny/index.html.
- 72.Alanis-Lobato G., Andrade-Navarro M.A., Schaefer M.H. Hippie v2.0: Enhancing meaningfulness and reliability of protein-protein interaction networks. Nucleic Acids Res. 2017;45:D408–D414. doi: 10.1093/nar/gkw985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gomez-Lazaro M., Bonekamp N.A., Galindo M.F., Jordan J., Schrader M. 6-hydroxydopamine (6-OHDA) induces Drp1-dependent mitochondrial fragmentation in SH-SY5Y cells. Free Radic. Biol. Med. 2008;44:1960–1969. doi: 10.1016/j.freeradbiomed.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 74.Yang Y., Lu B. Mitochondrial morphogenesis, distribution, and Parkinson disease: Insights from pink1. J. Neuropathol. Exp. Neurol. 2009;68:953–963. doi: 10.1097/NEN.0b013e3181b2048c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Winklhofer K.F., Haass C. Mitochondrial dysfunction in Parkinson’s disease. Biochim. Biophys. Acta. 2010;1802:29–44. doi: 10.1016/j.bbadis.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 76.Wiemerslage L., Ismael S., Lee D. Early alterations of mitochondrial morphology in dopaminergic neurons from Parkinson’s disease-like pathology and time-dependent neuroprotection with D2 receptor activation. Mitochondrion. 2016;30:138–147. doi: 10.1016/j.mito.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 77.Van Laar V.S., Berman S.B. Mitochondrial dynamics in Parkinson’s disease. Exp. Neurol. 2009;218:247–256. doi: 10.1016/j.expneurol.2009.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee H.J., Khoshaghideh F., Lee S., Lee S.J. Impairment of microtubule-dependent trafficking by overexpression of alpha-synuclein. Eur. J. Neurosci. 2006;24:3153–3162. doi: 10.1111/j.1460-9568.2006.05210.x. [DOI] [PubMed] [Google Scholar]
- 79.Gillardon F. Leucine-rich repeat kinase 2 phosphorylates brain tubulin-beta isoforms and modulates microtubule stability—A point of convergence in Parkinsonian neurodegeneration? J. Neurochem. 2009;110:1514–1522. doi: 10.1111/j.1471-4159.2009.06235.x. [DOI] [PubMed] [Google Scholar]
- 80.Lutz A.K., Exner N., Fett M.E., Schlehe J.S., Kloos K., Lammermann K., Brunner B., Kurz-Drexler A., Vogel F., Reichert A.S., et al. Loss of parkin or PINK1 function increases Drp1-dependent mitochondrial fragmentation. J. Biol. Chem. 2009;284:22938–22951. doi: 10.1074/jbc.M109.035774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sandebring A., Thomas K.J., Beilina A., van der Brug M., Cleland M.M., Ahmad R., Miller D.W., Zambrano I., Cowburn R.F., Behbahani H., et al. Mitochondrial alterations in PINK1 deficient cells are influenced by calcineurin-dependent dephosphorylation of dynamin-related protein 1. PLoS ONE. 2009;4:e5701. doi: 10.1371/journal.pone.0005701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dagda R.K., Gusdon A.M., Pien I., Strack S., Green S., Li C., Van Houten B., Cherra S.J., 3rd, Chu C.T. Mitochondrially localized PKA reverses mitochondrial pathology and dysfunction in a cellular model of Parkinson’s disease. Cell Death Differ. 2011;18:1914–1923. doi: 10.1038/cdd.2011.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Van Laar V.S., Arnold B., Cassady S.J., Chu C.T., Burton E.A., Berman S.B. Bioenergetics of neurons inhibit the translocation response of parkin following rapid mitochondrial depolarization. Hum. Mol. Genet. 2011;20:927–940. doi: 10.1093/hmg/ddq531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen Y., Csordas G., Jowdy C., Schneider T.G., Csordas N., Wang W., Liu Y., Kohlhaas M., Meiser M., Bergem S., et al. Mitofusin 2-containing mitochondrial-reticular microdomains direct rapid cardiomyocyte bioenergetic responses via interorganelle Ca(2+) crosstalk. Circ. Res. 2012;111:863–875. doi: 10.1161/CIRCRESAHA.112.266585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zuchner S., Mersiyanova I.V., Muglia M., Bissar-Tadmouri N., Rochelle J., Dadali E.L., Zappia M., Nelis E., Patitucci A., Senderek J., et al. Mutations in the mitochondrial GTPase mitofusin 2 cause charcot-marie-tooth neuropathy type 2A. Nat. Genet. 2004;36:449–451. doi: 10.1038/ng1341. [DOI] [PubMed] [Google Scholar]
- 86.Hoekstra J.G., Cook T.J., Stewart T., Mattison H., Dreisbach M.T., Hoffer Z.S., Zhang J. Astrocytic dynamin-like protein 1 regulates neuronal protection against excitotoxicity in Parkinson disease. Am. J. Pathol. 2015;185:536–549. doi: 10.1016/j.ajpath.2014.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jin J., Hulette C., Wang Y., Zhang T., Pan C., Wadhwa R., Zhang J. Proteomic identification of a stress protein, mortalin/mthsp70/GRP75: Relevance to Parkinson disease. Mol. Cell. Proteom. 2006;5:1193–1204. doi: 10.1074/mcp.M500382-MCP200. [DOI] [PubMed] [Google Scholar]
- 88.Jakobs S., Wurm C.A. Super-resolution microscopy of mitochondria. Curr. Opin. Chem. Biol. 2014;20:9–15. doi: 10.1016/j.cbpa.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 89.Jans D.C., Wurm C.A., Riedel D., Wenzel D., Stagge F., Deckers M., Rehling P., Jakobs S. Sted super-resolution microscopy reveals an array of minos clusters along human mitochondria. Proc. Natl. Acad. Sci. USA. 2013;110:8936–8941. doi: 10.1073/pnas.1301820110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pfanner N., van der Laan M., Amati P., Capaldi R.A., Caudy A.A., Chacinska A., Darshi M., Deckers M., Hoppins S., Icho T., et al. Uniform nomenclature for the mitochondrial contact site and cristae organizing system. J. Cell Biol. 2014;204:1083–1086. doi: 10.1083/jcb.201401006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ott C., Ross K., Straub S., Thiede B., Gotz M., Goosmann C., Krischke M., Mueller M.J., Krohne G., Rudel T., et al. Sam50 functions in mitochondrial intermembrane space bridging and biogenesis of respiratory complexes. Mol. Cell. Biol. 2012;32:1173–1188. doi: 10.1128/MCB.06388-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tondera D., Grandemange S., Jourdain A., Karbowski M., Mattenberger Y., Herzig S., Da Cruz S., Clerc P., Raschke I., Merkwirth C., et al. SLP-2 is required for stress-induced mitochondrial hyperfusion. EMBO J. 2009;28:1589–1600. doi: 10.1038/emboj.2009.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Steglich G., Neupert W., Langer T. Prohibitins regulate membrane protein degradation by the m-AAA protease in mitochondria. Mol. Cell. Biol. 1999;19:3435–3442. doi: 10.1128/MCB.19.5.3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nijtmans L.G., de Jong L., Artal Sanz M., Coates P.J., Berden J.A., Back J.W., Muijsers A.O., van der Spek H., Grivell L.A. Prohibitins act as a membrane-bound chaperone for the stabilization of mitochondrial proteins. EMBO J. 2000;19:2444–2451. doi: 10.1093/emboj/19.11.2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Paumard P., Vaillier J., Coulary B., Schaeffer J., Soubannier V., Mueller D.M., Brethes D., di Rago J.P., Velours J. The ATP synthase is involved in generating mitochondrial cristae morphology. EMBO J. 2002;21:221–230. doi: 10.1093/emboj/21.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Habersetzer J., Larrieu I., Priault M., Salin B., Rossignol R., Brethes D., Paumard P. Human F1F0 ATP synthase, mitochondrial ultrastructure and OXPHOS impairment: A (super-) complex matter? PLoS ONE. 2013;8:e75429. doi: 10.1371/journal.pone.0075429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Strauss M., Hofhaus G., Schroder R.R., Kuhlbrandt W. Dimer ribbons of ATP synthase shape the inner mitochondrial membrane. EMBO J. 2008;27:1154–1160. doi: 10.1038/emboj.2008.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cereghetti G.M., Stangherlin A., Martins de Brito O., Chang C.R., Blackstone C., Bernardi P., Scorrano L. Dephosphorylation by calcineurin regulates translocation of Drp1 to mitochondria. Proc. Natl. Acad. Sci. USA. 2008;105:15803–15808. doi: 10.1073/pnas.0808249105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schaefer M.H., Fontaine J.F., Vinayagam A., Porras P., Wanker E.E., Andrade-Navarro M.A. Hippie: Integrating protein interaction networks with experiment based quality scores. PLoS ONE. 2012;7:e31826. doi: 10.1371/journal.pone.0031826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Schaefer M.H., Lopes T.J., Mah N., Shoemaker J.E., Matsuoka Y., Fontaine J.F., Louis-Jeune C., Eisfeld A.J., Neumann G., Perez-Iratxeta C., et al. Adding protein context to the human protein-protein interaction network to reveal meaningful interactions. PLoS Comput. Biol. 2013;9:e1002860. doi: 10.1371/journal.pcbi.1002860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Suratanee A., Schaefer M.H., Betts M.J., Soons Z., Mannsperger H., Harder N., Oswald M., Gipp M., Ramminger E., Marcus G., et al. Characterizing protein interactions employing a genome-wide sirna cellular phenotyping screen. PLoS Comput. Biol. 2014;10:e1003814. doi: 10.1371/journal.pcbi.1003814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bragoszewski P., Gornicka A., Sztolsztener M.E., Chacinska A. The ubiquitin-proteasome system regulates mitochondrial intermembrane space proteins. Mol. Cell. Biol. 2013;33:2136–2148. doi: 10.1128/MCB.01579-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bragoszewski P., Turek M., Chacinska A. Control of mitochondrial biogenesis and function by the ubiquitin-proteasome system. Open Biol. 2017;7:170007. doi: 10.1098/rsob.170007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cook C., Petrucelli L. A critical evaluation of the ubiquitin-proteasome system in Parkinson’s disease. Biochim. Biophys. Acta. 2009;1792:664–675. doi: 10.1016/j.bbadis.2009.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hwang O. Role of oxidative stress in Parkinson’s disease. Exp. Neurobiol. 2013;22:11–17. doi: 10.5607/en.2013.22.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Danielson S.R., Andersen J.K. Oxidative and nitrative protein modifications in Parkinson’s disease. Free Radic. Biol. Med. 2008;44:1787–1794. doi: 10.1016/j.freeradbiomed.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Friedman J.R., Lackner L.L., West M., DiBenedetto J.R., Nunnari J., Voeltz G.K. ER tubules mark sites of mitochondrial division. Science. 2011;334:358–362. doi: 10.1126/science.1207385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cartelli D., Casagrande F., Busceti C.L., Bucci D., Molinaro G., Traficante A., Passarella D., Giavini E., Pezzoli G., Battaglia G., et al. Microtubule alterations occur early in experimental Parkinsonism and the microtubule stabilizer epothilone D is neuroprotective. Sci. Rep. 2013;3:1837. doi: 10.1038/srep01837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jensen R.E. Control of mitochondrial shape. Curr. Opin. Cell Biol. 2005;17:384–388. doi: 10.1016/j.ceb.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 110.Bleier L., Drose S. Superoxide generation by complex III: From mechanistic rationales to functional consequences. Biochim. Biophys. Acta. 2013;1827:1320–1331. doi: 10.1016/j.bbabio.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 111.Muller F.L., Liu Y., Van Remmen H. Complex III releases superoxide to both sides of the inner mitochondrial membrane. J. Biol. Chem. 2004;279:49064–49073. doi: 10.1074/jbc.M407715200. [DOI] [PubMed] [Google Scholar]
- 112.Cartelli D., Goldwurm S., Casagrande F., Pezzoli G., Cappelletti G. Microtubule destabilization is shared by genetic and idiopathic Parkinson’s disease patient fibroblasts. PLoS ONE. 2012;7:e37467. doi: 10.1371/annotation/6db7193b-913a-42f2-aa7c-139d6e15142a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Passmore J.B., Pinho S., Gomez-Lazaro M., Schrader M. The respiratory chain inhibitor rotenone affects peroxisomal dynamics via its microtubule-destabilising activity. Histochem. Cell Biol. 2017;148:331–341. doi: 10.1007/s00418-017-1577-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bindea G., Mlecnik B., Hackl H., Charoentong P., Tosolini M., Kirilovsky A., Fridman W.H., Pages F., Trajanoski Z., Galon J. ClueGo: A cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics. 2009;25:1091–1093. doi: 10.1093/bioinformatics/btp101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tieu K., Ischiropoulos H., Przedborski S. Nitric oxide and reactive oxygen species in Parkinson’s disease. IUBMB Life. 2003;55:329–335. doi: 10.1080/1521654032000114320. [DOI] [PubMed] [Google Scholar]
- 116.Wei T., Chen C., Hou J., Xin W., Mori A. Nitric oxide induces oxidative stress and apoptosis in neuronal cells. Biochim. Biophys. Acta. 2000;1498:72–79. doi: 10.1016/S0167-4889(00)00078-1. [DOI] [PubMed] [Google Scholar]
- 117.Pierini D., Bryan N.S. Nitric oxide availability as a marker of oxidative stress. Methods Mol. Biol. 2015;1208:63–71. doi: 10.1007/978-1-4939-1441-8_5. [DOI] [PubMed] [Google Scholar]
- 118.Smeyne M., Smeyne R.J. Glutathione metabolism and Parkinson’s disease. Free Radic. Biol. Med. 2013;62:13–25. doi: 10.1016/j.freeradbiomed.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Baraibar M.A., Liu L., Ahmed E.K., Friguet B. Protein oxidative damage at the crossroads of cellular senescence, aging, and age-related diseases. Oxid. Med. Cell. Longev. 2012;2012:919832. doi: 10.1155/2012/919832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dasgupta A., Zheng J., Bizzozero O.A. Protein carbonylation and aggregation precede neuronal apoptosis induced by partial glutathione depletion. ASN Neuro. 2012;4:e00084. doi: 10.1042/AN20110064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mattenberger Y., James D.I., Martinou J.C. Fusion of mitochondria in mammalian cells is dependent on the inner mitochondrial membrane potential and independent of microtubules or actin. FEBS Lett. 2003;538:53–59. doi: 10.1016/S0014-5793(03)00124-8. [DOI] [PubMed] [Google Scholar]
- 122.Brackley K.I., Grantham J. Activities of the chaperonin containing TCP-1 (CCT): Implications for cell cycle progression and cytoskeletal organisation. Cell Stress Chaperones. 2009;14:23–31. doi: 10.1007/s12192-008-0057-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Choi D.H., Cristovao A.C., Guhathakurta S., Lee J., Joh T.H., Beal M.F., Kim Y.S. NADPH oxidase 1-mediated oxidative stress leads to dopamine neuron death in Parkinson’s disease. Antioxid. Redox Signal. 2012;16:1033–1045. doi: 10.1089/ars.2011.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Murthy A., Gonzalez-Agosti C., Cordero E., Pinney D., Candia C., Solomon F., Gusella J., Ramesh V. NHE-RF, a regulatory cofactor for Na(+)-H+ exchange, is a common interactor for merlin and ERM (MERM) proteins. J. Biol. Chem. 1998;273:1273–1276. doi: 10.1074/jbc.273.3.1273. [DOI] [PubMed] [Google Scholar]
- 125.Ghosh A., Saminathan H., Kanthasamy A., Anantharam V., Jin H., Sondarva G., Harischandra D.S., Qian Z., Rana A., Kanthasamy A.G. The Peptidyl-prolyl Isomerase Pin1 Up-regulation and Proapoptotic Function in Dopaminergic Neurons: Relevance to the pathogenesis of Parkinson disease. J. Biol. Chem. 2013;288:21955–21971. doi: 10.1074/jbc.M112.444224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Braithwaite A.W., Del Sal G., Lu X. Some p53-binding proteins that can function as arbiters of life and death. Cell Death Differ. 2006;13:984–993. doi: 10.1038/sj.cdd.4401924. [DOI] [PubMed] [Google Scholar]
- 127.Schmidt O., Harbauer A.B., Rao S., Eyrich B., Zahedi R.P., Stojanovski D., Schonfisch B., Guiard B., Sickmann A., Pfanner N., et al. Regulation of mitochondrial protein import by cytosolic kinases. Cell. 2011;144:227–239. doi: 10.1016/j.cell.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 128.North B.J., Marshall B.L., Borra M.T., Denu J.M., Verdin E. The human Sir2 ortholog, Sirt2, is an NAD+-dependent tubulin deacetylase. Mol. Cell. 2003;11:437–444. doi: 10.1016/S1097-2765(03)00038-8. [DOI] [PubMed] [Google Scholar]
- 129.Janke C. The tubulin code: Molecular components, readout mechanisms, and functions. J. Cell Biol. 2014;206:461–472. doi: 10.1083/jcb.201406055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Loeffler D.A., Camp D.M., Conant S.B. Complement activation in the Parkinson’s disease substantia nigra: An immunocytochemical study. J. Neuroinflamm. 2006;3:29. doi: 10.1186/1742-2094-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Coates P.J., Nenutil R., McGregor A., Picksley S.M., Crouch D.H., Hall P.A., Wright E.G. Mammalian prohibitin proteins respond to mitochondrial stress and decrease during cellular senescence. Exp. Cell Res. 2001;265:262–273. doi: 10.1006/excr.2001.5166. [DOI] [PubMed] [Google Scholar]
- 132.Ros-Bernal F., Hunot S., Herrero M.T., Parnadeau S., Corvol J.C., Lu L., Alvarez-Fischer D., Carrillo-de Sauvage M.A., Saurini F., Coussieu C., et al. Microglial glucocorticoid receptors play a pivotal role in regulating dopaminergic neurodegeneration in Parkinsonism. Proc. Natl. Acad. Sci. USA. 2011;108:6632–6637. doi: 10.1073/pnas.1017820108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Herrero M.T., Estrada C., Maatouk L., Vyas S. Inflammation in Parkinson’s disease: Role of glucocorticoids. Front. Neuroanat. 2015;9:32. doi: 10.3389/fnana.2015.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ahn E.H., Kim D.W., Shin M.J., Kim Y.N., Kim H.R., Woo S.J., Kim S.M., Kim D.S., Kim J., Park J., et al. PEP-1-ribosomal protein S3 protects dopaminergic neurons in an MPTP-induced Parkinson’s disease mouse model. Free Radic. Biol. Med. 2013;55:36–45. doi: 10.1016/j.freeradbiomed.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 135.Morales M., Colicos M.A., Goda Y. Actin-dependent regulation of neurotransmitter release at central synapses. Neuron. 2000;27:539–550. doi: 10.1016/S0896-6273(00)00064-7. [DOI] [PubMed] [Google Scholar]
- 136.Kawamoto Y., Akiguchi I., Nakamura S., Honjyo Y., Shibasaki H., Budka H. 14-3-3 proteins in lewy bodies in Parkinson disease and diffuse lewy body disease brains. J. Neuropathol. Exp. Neurol. 2002;61:245–253. doi: 10.1093/jnen/61.3.245. [DOI] [PubMed] [Google Scholar]
- 137.Fabelo N., Martin V., Santpere G., Marin R., Torrent L., Ferrer I., Diaz M. Severe alterations in lipid composition of frontal cortex lipid rafts from Parkinson’s disease and incidental Parkinson’s disease. Mol. Med. 2011;17:1107–1118. doi: 10.2119/molmed.2011.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kubo S., Hatano T., Hattori N. Lipid rafts involvement in the pathogenesis of Parkinson’s disease. Front. Biosci. 2015;20:263–279. doi: 10.2741/4308. [DOI] [PubMed] [Google Scholar]
- 139.Cha S.H., Choi Y.R., Heo C.H., Kang S.J., Joe E.H., Jou I., Kim H.M., Park S.M. Loss of parkin promotes lipid rafts-dependent endocytosis through accumulating caveolin-1: Implications for Parkinson’s disease. Mol. Neurodegener. 2015;10:63. doi: 10.1186/s13024-015-0060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Donato R., Cannon B.R., Sorci G., Riuzzi F., Hsu K., Weber D.J., Geczy C.L. Functions of S100 proteins. Curr. Mol. Med. 2013;13:24–57. doi: 10.2174/156652413804486214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Warner-Schmidt J.L., Chen E.Y., Zhang X., Marshall J.J., Morozov A., Svenningsson P., Greengard P. A role for p11 in the antidepressant action of brain-derived neurotrophic factor. Biol. Psychiatry. 2010;68:528–535. doi: 10.1016/j.biopsych.2010.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rezvanpour A., Santamaria-Kisiel L., Shaw G.S. The S100A10-annexin A2 complex provides a novel asymmetric platform for membrane repair. J. Biol. Chem. 2011;286:40174–40183. doi: 10.1074/jbc.M111.244038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bieberich E. Synthesis, processing, and function of N-glycans in N-glycoproteins. Adv. Neurobiol. 2014;9:47–70. doi: 10.1007/978-1-4939-1154-7_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Scott H., Panin V.M. The role of protein N-glycosylation in neural transmission. Glycobiology. 2014;24:407–417. doi: 10.1093/glycob/cwu015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Picconi B., Piccoli G., Calabresi P. Synaptic dysfunction in Parkinson’s disease. Adv. Exp. Med. Biol. 2012;970:553–572. doi: 10.1007/978-3-7091-0932-8_24. [DOI] [PubMed] [Google Scholar]
- 146.Mercado G., Valdes P., Hetz C. An ercentric view of Parkinson’s disease. Trends Mol. Med. 2013;19:165–175. doi: 10.1016/j.molmed.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 147.Broers J.L., Ramaekers F.C., Bonne G., Yaou R.B., Hutchison C.J. Nuclear lamins: Laminopathies and their role in premature ageing. Physiol. Rev. 2006;86:967–1008. doi: 10.1152/physrev.00047.2005. [DOI] [PubMed] [Google Scholar]
- 148.Van de Vosse D.W., Wan Y., Wozniak R.W., Aitchison J.D. Role of the nuclear envelope in genome organization and gene expression. Wiley Interdiscip. Rev. Syst. Biol. Med. 2011;3:147–166. doi: 10.1002/wsbm.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Simon D.N., Zastrow M.S., Wilson K.L. Direct actin binding to A- and B-type lamin tails and actin filament bundling by the lamin A tail. Nucleus. 2010;1:264–272. doi: 10.4161/nucl.11799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nauseef W.M., McCormick S.J., Clark R.A. Calreticulin functions as a molecular chaperone in the biosynthesis of myeloperoxidase. J. Biol. Chem. 1995;270:4741–4747. doi: 10.1074/jbc.270.9.4741. [DOI] [PubMed] [Google Scholar]
- 151.Oka O.B., Pringle M.A., Schopp I.M., Braakman I., Bulleid N.J. Erdj5 is the ER reductase that catalyzes the removal of non-native disulfides and correct folding of the LDL receptor. Mol. Cell. 2013;50:793–804. doi: 10.1016/j.molcel.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Langston J.W., Ballard P.A., Jr. Parkinson’s disease in a chemist working with 1-methyl-4-phenyl-1,2,5,6-tetrahydropyridine. N. Engl. J. Med. 1983;309:310. doi: 10.1056/nejm198308043090511. [DOI] [PubMed] [Google Scholar]
- 153.Gautier C.A., Corti O., Brice A. Mitochondrial dysfunctions in Parkinson’s disease. Rev. Neurol. 2014;170:339–343. doi: 10.1016/j.neurol.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 154.Aroso M., Ferreira R., Freitas A., Vitorino R., Gomez-Lazaro M. New insights on the mitochondrial proteome plasticity in Parkinson’s disease. Proteom. Clin. Appl. 2016;10:416–429. doi: 10.1002/prca.201500092. [DOI] [PubMed] [Google Scholar]
- 155.Perier C., Tieu K., Guegan C., Caspersen C., Jackson-Lewis V., Carelli V., Martinuzzi A., Hirano M., Przedborski S., Vila M. Complex I deficiency primes Bax-dependent neuronal apoptosis through mitochondrial oxidative damage. Proc. Natl. Acad. Sci. USA. 2005;102:19126–19131. doi: 10.1073/pnas.0508215102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Waterham H.R., Koster J., van Roermund C.W., Mooyer P.A., Wanders R.J., Leonard J.V. A lethal defect of mitochondrial and peroxisomal fission. N. Engl. J. Med. 2007;356:1736–1741. doi: 10.1056/NEJMoa064436. [DOI] [PubMed] [Google Scholar]
- 157.Vila M., Przedborski S. Genetic clues to the pathogenesis of Parkinson’s disease. Nat. Med. 2004;10:S58–S62. doi: 10.1038/nm1068. [DOI] [PubMed] [Google Scholar]
- 158.Barsoum M.J., Yuan H., Gerencser A.A., Liot G., Kushnareva Y., Graber S., Kovacs I., Lee W.D., Waggoner J., Cui J., et al. Nitric oxide-induced mitochondrial fission is regulated by dynamin-related GTPases in neurons. EMBO J. 2006;25:3900–3911. doi: 10.1038/sj.emboj.7601253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Frank S., Gaume B., Bergmann-Leitner E.S., Leitner W.W., Robert E.G., Catez F., Smith C.L., Youle R.J. The role of dynamin-related protein 1, a mediator of mitochondrial fission, in apoptosis. Dev. Cell. 2001;1:515–525. doi: 10.1016/S1534-5807(01)00055-7. [DOI] [PubMed] [Google Scholar]
- 160.Trimmer P.A., Swerdlow R.H., Parks J.K., Keeney P., Bennett J.P., Jr., Miller S.W., Davis R.E., Parker W.D., Jr. Abnormal mitochondrial morphology in sporadic Parpkinson’s and Alzheimer’s disease cybrid cell lines. Exp. Neurol. 2000;162:37–50. doi: 10.1006/exnr.2000.7333. [DOI] [PubMed] [Google Scholar]
- 161.Gilkerson R.W., Selker J.M., Capaldi R.A. The cristal membrane of mitochondria is the principal site of oxidative phosphorylation. FEBS Lett. 2003;546:355–358. doi: 10.1016/S0014-5793(03)00633-1. [DOI] [PubMed] [Google Scholar]
- 162.Mannella C.A. Structure and dynamics of the inner mitochondrial membrane cristae. Biochim. Biophys. Acta. 2006;1763:542–548. doi: 10.1016/j.bbamcr.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 163.Zick M., Rabl R., Reichert A.S. Cristae formation-linking ultrastructure and function of mitochondria. Biochim. Biophys. Acta. 2009;1793:5–19. doi: 10.1016/j.bbamcr.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 164.Perier C., Bove J., Vila M. Mitochondria and programmed cell death in Parkinson’s disease: Apoptosis and beyond. Antioxid. Redox Signal. 2012;16:883–895. doi: 10.1089/ars.2011.4074. [DOI] [PubMed] [Google Scholar]
- 165.Vila M., Przedborski S. Targeting programmed cell death in neurodegenerative diseases. Nat. Rev. Neurosci. 2003;4:365–375. doi: 10.1038/nrn1100. [DOI] [PubMed] [Google Scholar]
- 166.Marchi S., Patergnani S., Pinton P. The endoplasmic reticulum-mitochondria connection: One touch, multiple functions. Biochim. Biophys. Acta. 2014;1837:461–469. doi: 10.1016/j.bbabio.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 167.Shim S.H., Xia C., Zhong G., Babcock H.P., Vaughan J.C., Huang B., Wang X., Xu C., Bi G.Q., Zhuang X. Super-resolution fluorescence imaging of organelles in live cells with photoswitchable membrane probes. Proc. Natl. Acad. Sci. USA. 2012;109:13978–13983. doi: 10.1073/pnas.1201882109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Sheehan J.P., Swerdlow R.H., Parker W.D., Miller S.W., Davis R.E., Tuttle J.B. Altered calcium homeostasis in cells transformed by mitochondria from individuals with Parkinson’s disease. J. Neurochem. 1997;68:1221–1233. doi: 10.1046/j.1471-4159.1997.68031221.x. [DOI] [PubMed] [Google Scholar]
- 169.Giacomello M., Drago I., Pizzo P., Pozzan T. Mitochondrial Ca2+ as a key regulator of cell life and death. Cell Death Differ. 2007;14:1267–1274. doi: 10.1038/sj.cdd.4402147. [DOI] [PubMed] [Google Scholar]
- 170.Hedskog L., Pinho C.M., Filadi R., Ronnback A., Hertwig L., Wiehager B., Larssen P., Gellhaar S., Sandebring A., Westerlund M., et al. Modulation of the endoplasmic reticulum-mitochondria interface in Alzheimer’s disease and related models. Proc. Natl. Acad. Sci. USA. 2013;110:7916–7921. doi: 10.1073/pnas.1300677110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gleichmann M., Mattson M.P. Neuronal calcium homeostasis and dysregulation. Antioxid. Redox Signal. 2011;14:1261–1273. doi: 10.1089/ars.2010.3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Szabadkai G., Bianchi K., Varnai P., De Stefani D., Wieckowski M.R., Cavagna D., Nagy A.I., Balla T., Rizzuto R. Chaperone-mediated coupling of endoplasmic reticulum and mitochondrial Ca2+ channels. J. Cell Biol. 2006;175:901–911. doi: 10.1083/jcb.200608073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Hayashi T., Su T.P. Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca2+ signaling and cell survival. Cell. 2007;131:596–610. doi: 10.1016/j.cell.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 174.Mercado G., Castillo V., Soto P., Sidhu A. ER stress and Parkinson’s disease: Pathological inputs that converge into the secretory pathway. Brain Res. 2016;1648:626–632. doi: 10.1016/j.brainres.2016.04.042. [DOI] [PubMed] [Google Scholar]
- 175.Iwasawa R., Mahul-Mellier A.L., Datler C., Pazarentzos E., Grimm S. Fis1 and Bap31 bridge the mitochondria-ER interface to establish a platform for apoptosis induction. EMBO J. 2011;30:556–568. doi: 10.1038/emboj.2010.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Verfaillie T., Rubio N., Garg A.D., Bultynck G., Rizzuto R., Decuypere J.P., Piette J., Linehan C., Gupta S., Samali A., et al. Perk is required at the ER-mitochondrial contact sites to convey apoptosis after ROS-based ER stress. Cell Death Differ. 2012;19:1880–1891. doi: 10.1038/cdd.2012.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hamasaki M., Furuta N., Matsuda A., Nezu A., Yamamoto A., Fujita N., Oomori H., Noda T., Haraguchi T., Hiraoka Y., et al. Autophagosomes form at ER-mitochondria contact sites. Nature. 2013;495:389–393. doi: 10.1038/nature11910. [DOI] [PubMed] [Google Scholar]
- 178.de Brito O.M., Scorrano L. Mitofusin 2 tethers endoplasmic reticulum to mitochondria. Nature. 2008;456:605–610. doi: 10.1038/nature07534. [DOI] [PubMed] [Google Scholar]
- 179.Keating D.J. Mitochondrial dysfunction, oxidative stress, regulation of exocytosis and their relevance to neurodegenerative diseases. J. Neurochem. 2008;104:298–305. doi: 10.1111/j.1471-4159.2007.04997.x. [DOI] [PubMed] [Google Scholar]
- 180.Brown M.R., Sullivan P.G., Geddes J.W. Synaptic mitochondria are more susceptible to Ca2+ overload than nonsynaptic mitochondria. J. Biol. Chem. 2006;281:11658–11668. doi: 10.1074/jbc.M510303200. [DOI] [PubMed] [Google Scholar]
- 181.Hollenbeck P.J. The pattern and mechanism of mitochondrial transport in axons. Front. Biosci. J. Virtual Libr. 1996;1:d91–d102. doi: 10.2741/A118. [DOI] [PubMed] [Google Scholar]
- 182.Jung C., Chylinski T.M., Pimenta A., Ortiz D., Shea T.B. Neurofilament transport is dependent on actin and myosin. J. Neurosci. Off. J. Soc. Neurosci. 2004;24:9486–9496. doi: 10.1523/JNEUROSCI.1665-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Schon E.A., Przedborski S. Mitochondria: The next (neurode) generation. Neuron. 2011;70:1033–1053. doi: 10.1016/j.neuron.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kim-Han J.S., Antenor-Dorsey J.A., O’Malley K.L. The Parkinsonian mimetic, MPP+, specifically impairs mitochondrial transport in dopamine axons. J. Neurosci. Off. J. Soc. Neurosci. 2011;31:7212–7221. doi: 10.1523/JNEUROSCI.0711-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Dauer W., Przedborski S. Parkinson’s disease: Mechanisms and models. Neuron. 2003;39:889–909. doi: 10.1016/S0896-6273(03)00568-3. [DOI] [PubMed] [Google Scholar]
- 186.Osman C., Voelker D.R., Langer T. Making heads or tails of phospholipids in mitochondria. J. Cell Biol. 2011;192:7–16. doi: 10.1083/jcb.201006159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Choi S.Y., Huang P., Jenkins G.M., Chan D.C., Schiller J., Frohman M.A. A common lipid links mfn-mediated mitochondrial fusion and snare-regulated exocytosis. Nat. Cell Biol. 2006;8:1255–1262. doi: 10.1038/ncb1487. [DOI] [PubMed] [Google Scholar]
- 188.Montessuit S., Somasekharan S.P., Terrones O., Lucken-Ardjomande S., Herzig S., Schwarzenbacher R., Manstein D.J., Bossy-Wetzel E., Basanez G., Meda P., et al. Membrane remodeling induced by the dynamin-related protein Drp1 stimulates Bax oligomerization. Cell. 2010;142:889–901. doi: 10.1016/j.cell.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Macdonald P.J., Stepanyants N., Mehrotra N., Mears J.A., Qi X., Sesaki H., Ramachandran R. A dimeric equilibrium intermediate nucleates Drp1 reassembly on mitochondrial membranes for fission. Mol. Biol. Cell. 2014;25:1905–1915. doi: 10.1091/mbc.E14-02-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kiebish M.A., Han X., Cheng H., Lunceford A., Clarke C.F., Moon H., Chuang J.H., Seyfried T.N. Lipidomic analysis and electron transport chain activities in c57bl/6j mouse brain mitochondria. J. Neurochem. 2008;106:299–312. doi: 10.1111/j.1471-4159.2008.05383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Davey G.P., Peuchen S., Clark J.B. Energy thresholds in brain mitochondria. Potential involvement in neurodegeneration. J. Biol. Chem. 1998;273:12753–12757. doi: 10.1074/jbc.273.21.12753. [DOI] [PubMed] [Google Scholar]
- 192.Zhou R., Yazdi A.S., Menu P., Tschopp J. A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469:221–225. doi: 10.1038/nature09663. [DOI] [PubMed] [Google Scholar]
- 193.Arbel N., Shoshan-Barmatz V. Voltage-dependent anion channel 1-based peptides interact with Bcl-2 to prevent antiapoptotic activity. J. Biol. Chem. 2010;285:6053–6062. doi: 10.1074/jbc.M109.082990. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.