Bile acids were recently shown to regulate glucose homeostasis through diverse mechanisms involving the host and its microbiome. Herein, Shapiro et al. discuss the impact of bile acids on normal and impaired glycemic responses, including potential therapeutic implications in treating hyperglycemia and diabetes.
Abstract
Bile acids (BAs) are cholesterol-derived metabolites that facilitate the intestinal absorption and transport of dietary lipids. Recently, BAs also emerged as pivotal signaling molecules controlling glucose, lipid, and energy metabolism by binding to the nuclear hormone farnesoid X receptor (FXR) and Takeda G protein receptor 5 (TGR5) in multiple organs, leading to regulation of intestinal incretin secretion, hepatic gluconeogenesis, glycogen synthesis, energy expenditure, inflammation, and gut microbiome configuration. Alterations in BA metabolism and signaling are associated with obesity and type 2 diabetes mellitus (T2DM), whereas treatment of T2DM patients with BA sequestrants, or bariatric surgery in morbidly obese patients, results in a significant improvement in glycemic response that is associated with changes in the BA profile and signaling. Herein, we review the roles of BAs in glucose metabolism in health and disease; highlight the limitations, unknowns, and challenges in understanding the impact of BAs on the glycemic response; and discuss how this knowledge may be harnessed to develop innovative therapeutic approaches for the treatment of hyperglycemia and diabetes.
Introduction
Bile acids (BAs) are a diverse group of amphipathic steroid molecules that enable micelle formation and facilitate intestinal absorption, emulsification, and transport of nutrients, lipids, and lipophilic vitamins. Recently, BAs were also recognized as a potent signaling molecules implicating pleiotropic physiological responses (Forman et al., 1995; Makishima et al., 1999), which includes glucose and energy metabolism (Ma et al., 2006; Kobayashi et al., 2007; Lefebvre et al., 2009). BAs are derived from catabolism of cholesterol in hepatocytes in a process that involves two principal pathways and activation of at least 17 hepatic enzymes. The classical pathway, which accounts for the majority of BA synthesis, is regulated by the rate-limiting enzyme cholesterol 7α-hydroxylase (CYP7A1). The alternative pathway involves an initial enzymatic step catalyzed by sterol-27-hydroxlase (CYP27A1), followed by BA hydroxylation by oxysterol 7α-hydroxylase (CYP7B1). Both pathways generate primary BAs that are actually the end products of cholesterol and are subsequently conjugated with taurine or glycine (Anderson et al., 1972; Ishibashi et al., 1996; Schwarz et al., 1996).
Upon synthesis, BAs are secreted by hepatocytes and drained into the gallbladder via the biliary tree. Postprandial contraction of the gallbladder releases BAs to the duodenum. In the intestine, primary BAs can be deconjugated and 7α-dehydroxylated by the gut bacteria to form secondary BAs, leading to even higher heterogeneity in this group of molecules (Kellogg and Wostmann, 1969; Yesair and Himmelfarb, 1970; Gilliland and Speck, 1977; Eyssen et al., 1983; Jones et al., 2008; Devlin and Fischbach, 2015; Wahlström et al., 2016). Intestinal BAs are actively reabsorbed in the terminal ileum and recirculated to the liver via the portal vein. In the liver, BAs are reconjugated and resecreted together with newly synthesized BAs. This efficient process, which allows recovery of the vast majority of BAs, is known as enterohepatic circulation (Vlahcevic et al., 1971; Angelin et al., 1982).
A minor fraction of BAs escape the enterohepatic circulation, and these molecules are either excreted with the feces or reach the systemic circulation (Ahlberg et al., 1977). The latter enable activation of BA signaling outside the enterohepatic system, where they regulate a plethora of processes such as lipid and glucose homeostasis, energy expenditure, intestinal mobility, inflammation, configuration, and growth of the gut microbiome and even skeletal muscle mass (Kirwan et al., 1975; Islam et al., 2011; Wang et al., 2011; Guo et al., 2016; Wahlström et al., 2016; Benoit et al., 2017). Dysregulated metabolism and signaling of BAs are suggested to play roles in several diseases, including dyslipidemia, fatty liver disease, diabetes, obesity, atherosclerosis, cholestasis, gallstones, and cancer (Kuipers et al., 2007; Bernstein et al., 2009; Pols et al., 2011; Li and Chiang, 2014). In this review, we will discuss the role of BAs in regulation of the glycemic control in health and in type 2 diabetes mellitus (T2DM). Other roles and functions of BAs are concisely discussed elsewhere (de Aguiar Vallim et al., 2013).
BA signaling and regulation of the glycemic response
Two main receptors, farnesoid X receptor FXR (also known as NR1H4) and the G protein–coupled BA receptor TGR5 (also known as GPBAR1, M-BAR, and BG37), mediate BA signaling. Other suggested BA receptors include vitamin D receptor (VDR; Makishima et al., 2002), pregnane X receptor (PXR; Staudinger et al., 2001), sphingosine-1-phosphate receptor 2 (S1PR2; Nagahashi et al., 2016), muscarinic M2 receptor (Sheikh Abdul Kadir et al., 2010), and constitutive androstane receptor (CAR; Cheng et al., 2017), which mainly regulate detoxification of the hepatotoxic species of BAs in addition to hepatic lipid and sterol metabolism.
FXR
Both conjugated and nonconjugated BAs bind FXR, with chenodeoxycholic acid (CDCA) being the most potent agonist of this receptor (Makishima et al., 1999; Parks et al., 1999; Wang et al., 1999). FXR is ubiquitously expressed in tissues and organs, including the liver, gut (Forman et al., 1995; Seol et al., 1995), white adipose tissues (Cariou et al., 2006), and heart (Zhang et al., 2003), enabling BA-mediated regulation of different physiological functions.
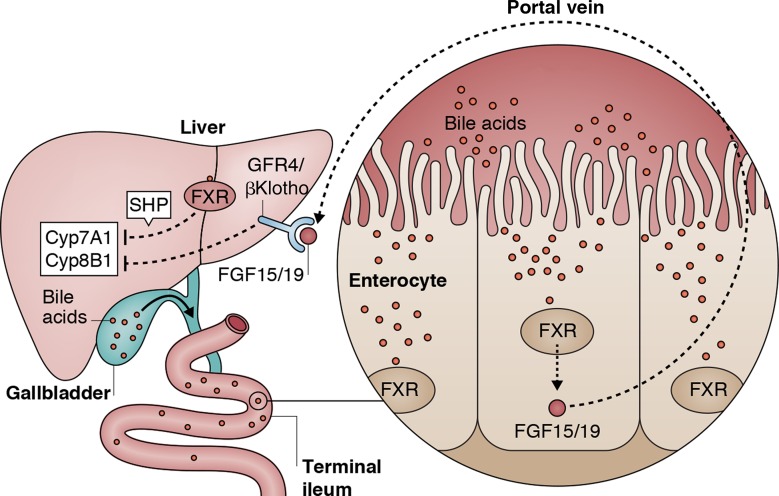
FXR forms a heterodimer with retinoic X receptor (RXR), thereby suppressing the expression of CYP7A1, the rate-limiting enzyme in BA biosynthesis, leading to attenuated hepatic conversion of cholesterol to BAs. CYP7A1-dependent suppression by FXR is mediated by two mechanisms: (1) in the liver, FXR induces the expression of the small heterodimer partner (SHP), which in turn inhibits CYP7A1 expression; (2) in the gut, FXR increases the levels of circulating fibroblast growth factor 19 (FGF19; FGF15 in mice), which reduces the expression of CYP7A1 and cytochrome P450 12a-hydroxylase B1 (CYP8B1), leading to inhibition of BA synthesis (Fig. 1). The effects of intestinal FGF15/19 suppression on hepatic CYP7A1 and CYP8B1 are mediated by hepatic FGF4/βKlotho receptor (FGFR4/βKlotho; Goodwin et al., 2000; Inagaki et al., 2005; Fig. 1). Overexpression of CYP7A1 in obese mice causes weight reduction and protection from glucose intolerance, insulin resistance, dyslipidemia (Li et al., 2010), liver steatosis, inflammation, and fibrosis (Liu et al., 2016), suggesting that hepatic expression of CYP7A1 alleviates metabolic derangements associated with obesity.
Figure 1.
Regulation of BA synthesis by repression of Cyp7a1 is mediated by FXR signaling. BA-FXR signaling in the liver activates SHP, which negatively controls Cyp7A1 expression. Intestinal BA-FXR signaling induces FGF15/19 expression. Release of intestinal FGF15/19 followed by binding of FGF15/19 to hepatic FGFR4/βKlotho leads to repression of hepatic Cyp7A1 and Cyp8B1.
Postprandial activation of FXR in various organs leads to repression of gene expression by induction of SHP (Goodwin et al., 2000) and suppression of autophagy by blocking both cAMP-response element–binding protein (CREB; Seok et al., 2014) and peroxisome proliferator-activated receptor-α (PPARα) activation (Lee et al., 2014). Furthermore, posttranslational modifications of FXR modulate its own activity, thus impacting lipid and glucose sensing in both the fed and fasting states. These include glucose-stimulated O-GlcNAcylation of FXR that enhances FXR activity (Berrabah et al., 2014). The transcriptional activity of FXR is regulated by phosphorylation mediated by protein kinase C (PKC; Gineste et al., 2008) or adenosine monophosphate–activated protein kinase (AMPK; Lien et al., 2014), and BA-FXR activation leads to enhanced FXR phosphorylation and proteasomal degradation of FXR (Hashiguchi et al., 2016). FXR methylation supports the transactivation of FXR and FXR target genes (Balasubramaniyan et al., 2012). In addition to methylation, acetylation increases FXR stability but inhibits FXR-RXRα dimerization, DNA binding, and transactivation activity and is regulated by p300 and Sirtuin-1 (SIRT1; Kemper et al., 2009). FXR acetylation is enhanced in mice models of obesity and T2DM (Kemper et al., 2009), and FXR acetylation exacerbates liver inflammation and glucose intolerance (Kim et al., 2015).
Obese mice lacking FXR feature lower body weight coupled with an improved glycemic response and insulin sensitivity (Prawitt et al., 2011; Zhang et al., 2012; Ryan et al., 2014). In contrast, lean mice lacking FXR display dyslipidemia associated with loss of insulin sensitivity and impaired glucose tolerance (Ma et al., 2006). Long-term oral supplementation of FXR agonist (GW4064) to obese and insulin-resistant mice led to exacerbated weight gain, dyslipidemia, and glucose intolerance (Watanabe et al., 2011). It is important to note that this effect was different from the improved insulin sensitivity that was observed upon short-term treatment with this agonist (Cariou et al., 2006). Collectively, whole-body manipulation of FXR affects different tissues leading to complex alterations in glucose and energy homeostasis.
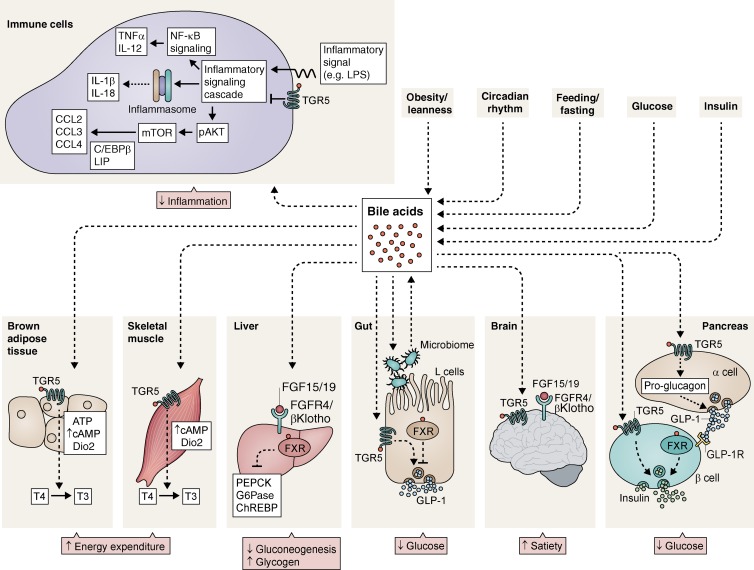
Hepatic BA-FXR signaling modulates postprandial glucose levels through decreased liver gluconeogenesis accompanied by induction of hepatic glycogen synthesis (Duran-Sandoval et al., 2005; Zhang et al., 2006; Potthoff et al., 2011; Fig. 2). Mice studies showed that after eating, induction of BAs secretion results in BA-FXR signaling in the liver, leading to stimulation of glycogen storage and inhibition of hepatic glycolytic and lipogenic gene expression, such as carbohydrate responsive element–binding protein (ChREBP) and sterol responsive element–binding protein 1 (SREBP1c; Watanabe et al., 2004; Duran-Sandoval et al., 2005; Ma et al., 2006; Fig. 2). Further studies in mice showed that FXR signaling in the liver causes repression of enzymes involved in hepatic gluconeogenesis including phosphoenolpyruvate carboxykinase (PEPCK) and glucose 6-phosphatase (G6Pase; Zhang et al., 2006; Potthoff et al., 2011; Fig. 2). However, the underlying mechanism governing FXR control of hepatic gluconeogenesis remains elusive and requires further investigation in both the fasting and postprandial state. Interestingly, several mice studies suggest that FXR signaling does not directly affect liver insulin sensitivity, but rather impacts peripheral insulin sensitivity in tissues such as adipose tissue and skeletal muscle (Cariou et al., 2006; Ma et al., 2006). A recent study by Kim et al. (Kim et al., 2017) reported that hepatic deletion of both FXR and SHP improves glucose tolerance and fatty acid metabolism in aged mice, reversing the aging phenotype of increased adiposity and impaired glucose sensing. This supports a key role of hepatic FXR-SHP signaling in controlling whole-body glucose and energy homeostasis.
Figure 2.
BA signaling controls the systemic glycemic response. In the liver BA-FXR signaling inhibits gluconeogenesis and promotes glycogen synthesis by negative regulation of PEPCK, G6Pase, and ChREBP. In intestinal L cells, BA-TGR5 signaling leads to GLP-1 expression and secretion, whereas BA-FXR signaling inhibits GLP-1 production. The gut microbiome controls BA diversity, whereas BA composition mediates gut microbiome configuration. In the brain, BA-TGR5 signaling mediates satiety. In skeletal muscles and brown adipose tissue, BA-TGR5 sensing promotes T4 conversion to T3, leading to increased energy expenditure. In the pancreas, both BA-TGR5 and BA-FXR signaling in β cells induces insulin production. Glucose-stimulated insulin release is additionally promoted by BA-TGR5 signaling in α cells, which causes conversion of proglucagon to GLP-1 and GLP-1 release. TGR5-BA in immune cells results in inhibition of NLRP3-inflammasome and attenuated inflammation. CCL, chemokine (C-C motif) ligand; Dio2, type 2 iodothyronine deiodinase; LIP, liver inhibitory protein; T4, thyroxine; T3, tri-iodothyronine.
BA-FXR–mediated induction of intestinal FGF15/19, leads to its binding to hepatic FGFR4/βKlotho, thereby contributing to hepatic glycogen synthesis and decreasing glycemia (Fig. 2; Kir et al., 2011). As such, FGF15 deficient mice featured hyperglycemia and impaired hepatic glycogen synthesis, which was ameliorated by FGF19 administration, suggesting a beneficial effect of FGF15/19 on energy and glucose metabolism (Kir et al., 2011). In concert, systemic administration of FGF19 to obese and diabetic mice induced an anti-diabetic effect (Fu et al., 2004). Similarly, a positive association between FGF19 and improved insulin sensitivity was demonstrated in T2DM patients who achieved normoglycemia as a result of a bariatric surgery Roux-en-Y gastric bypass (RYGB; Sachdev et al., 2016). Several downstream mechanisms have been suggested to explain the beneficial metabolic effects of FGF15/19, including inhibition of hepatic gluconeogenesis by modulating G6Pase and PEPCK (Potthoff et al., 2011) and stimulation of insulin-independent glycolysis in the brain (Morton et al., 2013). Additional mechanism for FGF19 function in the brain was demonstrated by Ryan et al. (Ryan et al., 2013), who administered FGF19 by intra-ventricular injection into the central nervous system of mice. This resulted in anorexigenic effect, weight loss and improved glucose metabolism, which were blunted by FGF19 inhibition, suggesting a role of FXR signaling in the satiety response (Fig. 2). Furthermore, recent study by Picard et al. (2016) revealed that FGF15 expression in the hypothalamus negatively regulates dorsal vagal complex neuronal activity, ultimately leading to lower glucagon secretion from pancreatic α cells. Collectively, these results suggest that intestinal, hepatic and neuronal activation of FGF15/19 provides a network of signals leading to systemic control of the glycemic response in normoglycemia and in T2DM (Fig. 2).
Several recent studies highlight an additional effect of FXR signaling in the gastrointestinal tract. Blocking intestinal FXR had a beneficial effect on glucose homeostasis and energy expenditure. In the intestine, FXR signaling improves the kinetics of glucose 6-phosphate (G6P) absorption, an affect which was mitigated in FXR-deficient mice (van Dijk et al., 2009). Mice with an isolated intestinal deficiency of FXR displayed protection from development of obesity and glucose intolerance (Li et al., 2013; Jiang et al., 2015b), suggesting a central role of intestinal FXR in driving obesity-associated pathologies. In agreement with these findings, several studies (Li et al., 2013; Jiang et al., 2015a,b; Xie et al., 2017) showed that obese and diabetic mice treated with intestinal FXR antagonists develop a significant reduction in glucose intolerance, insulin resistance, fatty liver as well as elevated energy expenditure because of lower intestinal and total ceramide levels. Recently, Xie et al. (2017) reported that lower ceramide levels induced by blocking intestinal FXR led to attenuated hepatic gluconeogenesis by lowering liver mitochondrial acetyl-CoA levels and pyruvate carboxylase activity, thus adding another possible mechanism linking intestinal FXR signaling with hepatic regulation of gluconeogenesis. In contrast to studies presenting improved metabolic outcomes upon treatment with intestinal FXR antagonist or in mice lacking intestinal FXR, Fang et al. (2015) showed that the administration of intestinal FXR agonist fexaramine to obese and diabetic mice reduced weight gain, glucose intolerance and insulin resistance along with increased energy expenditure. However, the metabolic phenotype shown with fexaramine was abrogated in mice lacking TGR5, suggesting that this drug may partially regulate TGR5 signaling in addition to FXR signaling. Collectively, most studies demonstrate that activation of intestinal FXR has a detrimental effect on the glycemic response and energy expenditure in response to obesity, suggesting that inhibition of intestinal FXR signaling has a potential for treating hyperglycemia. Additional mechanisms of intestinal FXR signaling and its outcomes merit further studies, including possible effects on glucose turnover and G6P absorption (van Dijk et al., 2009).
TGR5
TGR5 is a G protein–coupled receptor expressed in many organs and tissues including the intestine, gallbladder, brown and white adipose tissues, skeletal muscle, brain and the pancreas. BA activation of TGR5 leads to cAMP production, which in turn activates protein kinase A (PKA) pathways in different tissues and cell types (Kawamata et al., 2003; Katsuma et al., 2005).
Activation of TGR5 by BAs promotes glucagon like peptide-1 (GLP-1) secretion from intestinal L cells (Fig. 2). This peptide acts on the pancreatic β cells and regulates glucose-stimulated insulin secretion (Katsuma et al., 2005; Fig. 2). TGR5 signaling in intestinal L cells was suggested to induce mitochondrial oxidative phosphorylation, a rise in the ATP/ADP ratio, subsequent closure of the ATP-dependent potassium channel (KATP) and enhanced mobilization of intracellular calcium, leading to GLP-1 secretion and improvement in glucose homeostasis (Thomas et al., 2009). Trabelsi et al. (2015) found that GLP-1 secretion by intestinal L cells is negatively regulated by FXR through inhibition of pro-glucagon gene expression and suppression of GLP-1 secretion (Fig. 2). These results suggest that BA activation of both TGR5 and FXR in intestinal L cells can induce opposite effects on GLP-1 secretion and production. However, TGR5 activation in L cells likely occurs rapidly after food ingestion, whereas activation of FXR induces a more delayed response that requires transcriptional activation. This difference leads to a temporal separation between postprandial positive effects of BA-TGR5 signaling on GLP-1 secretion and FXR-mediated inhibition of GLP-1 release (Trabelsi et al., 2015; Fig. 2). In accordance, several studies reported that T2DM patients who achieved normoglycemia as a result of RYGB bariatric surgery, featured a marked increase in fasting and postprandial BAs. The change in BA levels positively correlated with FGF19, GLP-1 and PYY (Dutia et al., 2015; Sachdev et al., 2016), but no causative relationship between BA-TGR5 signaling and incretin levels was pursued in these patients.
Mice overexpressing TGR5 that were fed a high-fat diet (HFD) featured improved glucose-stimulated insulin secretion compared with wild-type mice, and similar results were reported in obese and diabetic mice treated with TGR5 agonists exhibiting reduced hepatic glucose production (Thomas et al., 2009). Conversely, TGR5-deficient mice displayed glucose intolerance and impaired insulin secretion in response to obesity (Thomas et al., 2009) that were abrogated by the administration of TGR5 agonists (Pellicciari et al., 2009; Briere et al., 2015). In light of the beneficial effects of TGR5 signaling, a substantial reduction in hyperglycemia and elevated GLP-1 was observed in a small group of T2DM patients who received a high dose of the TGR5 agonist SB-756050 (Hodge and Nunez, 2016). However, studies in rodents show that the effect of systemic exposure to TGR5 agonists increases gallbladder volume (Briere et al., 2015). Thus, an ideal TGR5 agonist would be intestinal-specific agonist reaching L cells without affecting other systemic tissues. Indeed, Lasalle et al. (2017) recently described a novel topical intestinal agonist of TGR5 that was given orally to obese and insulin-resistant mice, leading to prominent elevation in GLP-1 levels along with significant improvement in glucose tolerance. Intestinal TGR5 agonist did not cause a significant change in gallbladder size in lean mice. The impact of intestinal TGR5 agonist on human gallbladder and its therapeutic potential for T2DM in humans requires further study.
In addition to GLP-1 modulation, TGR5 can induce cAMP-dependent thyroid hormone activating enzyme type 2 iodothyronine deiodinase, causing elevated energy expenditure in brown adipocytes and skeletal muscles. This is achieved by converting inactive thyroxine (T4) into active tri-iodothyronine (T3) that critically determinates thyroid hormone receptor regulation of energy expenditure (Watanabe et al., 2006; Fig. 2). In concert with the results in rodents, Patti et al. (2009) found that obese individuals who undergo RYGB had elevated levels of BAs that were inversely correlated with thyroid-stimulating hormone (TSH) levels compared with nonoperated obese controls. However, the mechanism of action of BAs on TSH production remains unknown.
Another mechanism possibly connecting BA signaling and elevated energy expenditure was proposed recently by Worthmann et al. (2017). They showed that cold exposure in mice triggered cholesterol lipoprotein uptake in brown adipose tissue and hepatic Cyp7b1 expression. This led to BA catabolism from cholesterol by the alternative pathway, which in turn caused modifications in the gut microbiome that facilitated adaptive thermogenesis. The authors observed lower hepatic expression of Cyp7b1 in obese patients with T2DM (Worthmann et al., 2017), but the clinical relevance of cold-induced BA synthesis remains unknown. Interestingly, oral supplementation of the BA CDCA to women led to increased brown adipose tissue activity and glucose uptake accompanied with increased energy expenditure, but the mechanism involved in BA stimulation of brown adipose tissue activity in humans is unclear (Broeders et al., 2015).
Pancreatic β cells express both TGR5 (Kumar et al., 2012) and FXR (Renga et al., 2010), promoting glucose-stimulated insulin secretion by increasing intracellular calcium concentration (Fig. 2). FXR additionally mediates the induction of insulin transcription (Renga et al., 2010). As mentioned in the FXR section, FXR-deficient mice are protected from obesity-induced glucose intolerance. Similar insulin levels and pancreatic islet mass were observed in obese mice lacking FXR and wild-type mice, suggesting that the protection from obesity and glucose tolerance that was found in FXR-deficient mice cannot be explained merely by compensation through enhanced β cell insulin secretion (Schittenhelm et al., 2015). Interestingly, pancreatic α cells also express TGR5. Activation of TGR5 by BA switches the α cell secretory phenotype from glucagon to GLP-1, thus promoting a paracrine effect on β cells to stimulate insulin secretion (Kumar et al., 2016; Fig. 2).
Collectively, manipulating FXR and TGR5 signaling in rodents and humans plays pivotal roles in regulating glucose metabolism via signaling in different organs (Fig. 2). In most studies, intestinal FXR activation causes deleterious effects on hyperglycemia, whereas TGR5 signaling improves glycemic control and energy homeostasis. Consequently, activation of TGR5 signaling coupled with blocking intestinal FXR may serve as an innovative approach for controlling the glycemic response in T2DM patients. However, the tissue-specific functions and the long-term effects of FXR and TGR5 signaling in different environmental conditions such as different diets and nutritional states, which modulates systemic glucose control, merits further investigation.
Factors regulating the BA pool
Several factors influence BA concentration and consequently BA-FXR and TGR5 signaling (Fig. 2). First, the concentration of BAs depends on food transit time. As such, BA pools are higher in the postprandial in comparison with the fasting state (Angelin et al., 1982; Li et al., 2012; Haeusler et al., 2016). This is a result of enhanced postprandial BAs secretion into the small intestine, increased enterohepatic reabsorption, and, possibly, enhanced transcription and activity of hepatic CYP7A1 (Li et al., 2012). Second, obesity impacts the BA pool (Fig. 2). In response to a mixed meal, obese subjects feature slightly higher circulating levels of BAs (Haeusler et al., 2016). More specifically, other studies showed that the changes in BA levels observed in obese subjects include alterations in the BA ratio and blunted excursion of glycine-conjugated BAs compared with lean subjects (Glicksman et al., 2010; Ahmad et al., 2013; Haeusler et al., 2016). The difference in BA composition between lean and obese subjects can be partially explained by the reduced expression of some hepatic BA transporters, coupled with an increase in 12-α hydroxylated BA synthesis (Haeusler et al., 2016). Third, insulin and glucose significantly alter BA composition and abundance (Fig. 2). Mice treated with streptozotocin to induce hyperglycemia or obese and diabetic mice display elevated serum levels of BAs and a larger BA pool. This effect could be mediated by induction of Cyp7a1 mRNA expression by increased acetylation and decreased methylation of the Cyp7a1 gene promoter (Li et al., 2012). Consistent with the results in rodents, humans undergoing oral glucose tolerance testing showed increased levels of several BAs (Shaham et al., 2008). An euglycemic-hyperinsulinemic clamp study in humans found that insulin acutely caused a significant reduction in circulating BAs and that this effect was blunted in obese subjects (Haeusler et al., 2016). In humans, elevated levels of 12-hydroxylated BAs were associated with insulin resistance (Haeusler et al., 2013). Haeusler et al. (2012) investigated the mechanism for this difference in the BA pool and found that in mice with normal physiology, insulin signaling activating FoxO1 maintains the production of 12-hydroxylated BAs by up-regulation of Cyp8b1 and normal FXR activity. In obese and insulin-resistant mice, the impaired insulin and FoxO1 signaling leads to an excess of 12-hydroxylated BAs. Fourth, the daily circadian rhythm influences the BA pool, leading to a significant increase after feeding (Gälman et al., 2005; Le Martelot et al., 2009; Fig. 2). In mice, these diurnal changes seem to be regulated by the transcription of Cyp7a1 (Le Martelot et al., 2009), by the clock gene Rev-erbα (Duez et al., 2008), and by Fgf15 (Han et al., 2015). Finally, sex hormones were suggested to affect BA metabolism, but controversial findings have been reported on the differences in baseline fasting BA levels between men and women (Gälman et al., 2011; Ho et al., 2013; Bathena et al., 2015).
BAs and the gut microbiome
The gut microbiome plays key roles in BA synthesis, modification, and signaling by transforming host-derived primary BAs into secondary BAs and by their deconjugation (e.g., removal of glycine or taurine) via the enzymatic activity of bile salt hydrolases (Swann et al., 2011). Mice treated with antibiotics or germ-free mice displayed a predominance of primary BAs with a reduced secondary BA pool, suggesting a central role of the gut microbiome in generating BA diversity. The lower BA diversity in microbiome-depleted mice is accompanied by enhanced hepatic expression of CYP7A1 and reduced ileal expression of FGF15 and SHP (Sayin et al., 2013; Wahlström et al., 2016). These differences in gene expression were abrogated upon colonization of germ-free mice with bacteria (Wahlström et al., 2017). Sayin et al. (2013) showed that BA diversity is controlled by the gut microbiome in an FXR-dependent manner and that it affects the synthesis of primary BAs by regulating FGF15 and CYP7A1 expression along with conjugation and absorption of BAs. Moreover, several studies suggested that BAs may directly affect bacterial composition, creating a dynamic equilibrium between BAs and the gut microbiome composition and function (Islam et al., 2011; Kakiyama et al., 2013; Fig. 2).
BA-FXR signaling and the associated modification in microbiome composition may be clinically relevant, because the beneficial effects of bariatric surgery on glucose and body weight are also associated with changes in the gut microbial communities and are FXR dependent (Ryan et al., 2014; Parséus et al., 2017). Further investigation of the interactions between the gut microbiome and BA signaling, as well as their impact on glycemic control, may help to identify whether supplementation with certain BAs can change the microbiome configuration and therefore be used as a treatment for hyperglycemia. Studying the microbiome–BA axis may additionally lead to the identification of bacterial species that modulate BA signaling in a way that would enable targeted probiotics (Degirolamo et al., 2014) or prebiotics to improve the glycemic response in diabetic patients.
BAs and regulation of inflammation
Inflammation is another mechanism that could be involved in BA regulation of the glycemic response, because chronic low-grade inflammation is suggested to play a role in glucose homeostasis (Li et al., 2012). Studies in murine models and primary hepatocytes show that obeticholic acid (OCA) induced an anti-inflammatory response mediated by inhibition of NF-κB activity leading to reduced expression of proinflammatory cytokines (Liu et al., 2016), but there are controversial studies on the effect of OCA on insulin sensitivity in T2DM patients (Mudaliar et al., 2013; Neuschwander-Tetri et al., 2015). Inflammasomes are cytoplasmic innate immune protein complexes activated by both pathogens and endogenous tissue damage–related signals and have been suggested to play key roles in regulation of obesity and the glycemic response (Vandanmagsar et al., 2011; Henao-Mejia et al., 2012; Rathinam and Fitzgerald, 2016). Upon activation by one of a variety of different signals, NOD-like receptors (NLRs) form mature inflammasome complex. This results in activation of proinflammatory caspase, processing of mature cytokines such as IL-1β and IL-18, and a controlled cell death termed pyroptosis (Rathinam and Fitzgerald, 2016). Several studies showed that TGR5 induces an anti-inflammatory response in myeloid cells by suppressing proinflammatory cytokines (Wang et al., 2011; Högenauer et al., 2014; Perino et al., 2014). Perino et al. (2014) showed that in response to diet-induced obesity, wild-type mice transplanted with TGR5−/− bone marrow or mice with myeloid-specific deletion of TGR5 displayed exacerbated glucose intolerance, insulin resistance, and adipose tissue inflammation. Bone marrow–derived macrophages isolated from TGR5-depleted mice exhibited a significant reduction in LPS-induced chemokine expression and macrophage migration that was mediated by AKT-dependent activation of mTOR and CCAAT/enhancer binding protein β (C/EBP β). In concert, other studies (Pols et al., 2011; Wang et al., 2011; Högenauer et al., 2014; Guo et al., 2015; Su et al., 2017) showed that TGR5 activation inhibits LPS induction of proinflammatory cytokines and NF-κB phosphorylation and signaling, which was ablated in TGR5-deficient mice. Altogether, these studies suggest that TGR5 activation may decrease systemic inflammation and macrophage infiltration to adipose tissues that may possible lead to improved glucose and insulin sensitivity in obesity (Fig. 2). In line with the role of TGR5 in attenuated inflammation, Guo et al. (2016) demonstrated that BA-TGR5 signaling induces inhibition of the NLRP3 inflammasome, which in turn improved insulin sensitivity and glucose tolerance, suggesting a possible link between BA-TGR5 signaling in innate immune cells and metabolic functions (Fig. 2). Future studies will lead to mechanistic understanding of the interaction between BA signaling and immune cells and their effects on inflammation and glucose metabolism in health and in T2DM.
Clinical relevance of BA signaling in glycemic control
T1DM
The clinical impact of BAs on hyperglycemia and diabetes mellitus was almost exclusively investigated in studies focusing on T2DM in rodents and humans, as highlighted below. In contrast, the contribution of BAs to the pathogenesis of type 1 diabetes mellitus (T1DM) remains less characterized. A model for T1DM involves treatment of mice with streptozotocin, a drug exhibiting high toxicity to insulin-producing β cells. Upon development of T1DM in this model, mice display a significant rise in total BA level in serum, gallbladder and intestine while featuring lower levels of secondary BAs in the gallbladder and in the feces (Li et al., 2012). Similarly, children with T1DM (even when well controlled) harbor alterations in urine and serum BA composition compared with healthy controls (Balderas et al., 2013). Likewise, adults with well or poorly controlled T1DM showed an altered profile of circulating BAs in comparison to healthy adults (Dutta et al., 2016). Collectively, these studies suggest that alterations in BA composition in T1DM persist even after induction of normoglycemia, suggesting a potential yet unproven causal association between altered BA profile and the progression of T1DM that requires further study.
T2DM
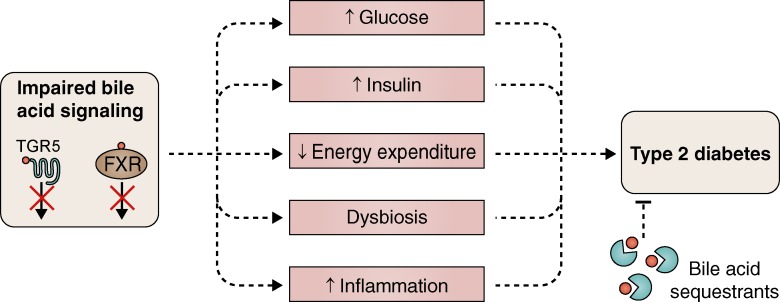
The contribution of BAs to the regulation of glycemic responses in T2DM was mainly demonstrated through the effects of BA sequestrants (Fig. 3) and the effects demonstrated in patients undergoing bariatric surgery, which dramatically impacts both glucose levels and BA profile.
Figure 3.
BAs and diabetes mellitus. Impaired BA signaling in the context of an altered glycemic response contributes to progression toward T2DM through multiple mechanisms.
BA sequestrants are orally administered nonabsorbable resins that lack systemic toxicity and have been used for treatment of dyslipidemia (Fonseca et al., 2010). Unexpectedly, BA sequestrants have beneficial effects on the glycemic control and insulin sensitivity in T2DM patients and diabetic rodents (Hansen et al., 2017). Hence, one BA sequestrant, colesevelam, is a US Food and Drug Administration–approved drug used to treat diabetes. T2DM patients treated for 12 weeks with colesevelam showed a significant reduction in HbA1c and postprandial glucose levels (Zieve et al., 2007), even when colesevelam was given in combination with other antidiabetic drugs (Fonseca et al., 2010), whereas healthy insulin-sensitive subjects remained unaffected by colesevelam treatment (Blahová et al., 2016). Some T2DM patients treated with colesevelam exhibited an increase in plasma triglyceride levels, which precludes colesevelam treatment in T2DM subjects with hyperglyceridemia (Fonseca et al., 2010). Obese and diabetic mice treated with colesevelam showed improved glycemic response mediated by a dual mechanism: (1) TGR5-mediated GLP-1 secretion in L cells and (2) intestinal proglucagon expression (Potthoff et al., 2013; Trabelsi et al., 2015). The beneficial metabolic effects of colesevelam were also dependent on FXR signaling because FXR deletion diminishes the effect of the drug (Prawitt et al., 2011; Trabelsi et al., 2015). Hypothetically, and similarly to BA sequestrants, future drugs impacting BA signaling may serve as future modalities for T2DM treatment.
Multiple studies in humans (Wickremesekera et al., 2005; Schauer et al., 2017) and rodents (Kohli et al., 2013) demonstrated the efficacy of bariatric surgery in improving and even normalizing blood glucose levels in T2DM. The improvement in the glycemic response is observed much earlier than weight loss (Wickremesekera et al., 2005), suggesting weight-independent beneficial effects of the surgery on glucose metabolism (Lutz and Bueter, 2014). Interestingly, bariatric surgery also influences BA metabolism and disrupts the enterohepatic circulation, thereby leading to a rise in BA levels (Ahmad et al., 2013). The mechanisms for the increase in BAs upon bariatric surgery are currently unclear and may include induction of BA reabsorption in the ileum with an opposite decrease of reabsorption in the liver after bile diversion (Bhutta et al., 2015; Goncalves et al., 2015), blunted hepatic glucose production, an increase in intestinal gluconeogenesis (Goncalves et al., 2015), and changes in gut microbial communities (Ryan et al., 2014). Other mechanisms that control BA pool upon bariatric surgery include modified activation of FXR and TGR5 signaling (Ryan et al., 2014; Ding et al., 2016; McGavigan et al., 2017). Alterations in BA pool were proposed to constitute one of the mechanisms that positively affect glucose metabolism after bariatric surgery (Ferrannini et al., 2015). Obese FXR-deleted mice that undergo bariatric surgery exhibit impaired weight loss and glucose tolerance improvement (Ryan et al., 2014), suggesting that BA-FXR signaling may govern weight and glucose control after bariatric surgery. Nevertheless, studies on the composition of the circulating BAs after bariatric surgery are inconsistent because of different measurement methods, lack of adjusted control groups, a focus on some (but not all) BAs in different human studies, and differences in surgical procedures between cohorts (Courcoulas et al., 2014; De Giorgi et al., 2015; Dutia et al., 2015; Sachdev et al., 2016). Additionally, several studies that followed T2DM subjects before and after RYGB showed that the changes in glucose tolerance and insulin sensitivity preceded the rise in BAs (Steinert et al., 2013; Jørgensen et al., 2015), pointing toward the possibility that the increase in BAs in the circulation after RYGB may not drive changes in the glycemic response but rather may constitute a secondary effect. Collectively, at present, the contribution of BAs to the regulation of glucose metabolism upon bariatric surgery remains unclear, with no clear-cut causative evidence linking postbariatric BA alterations with the postsurgical improvement in glucose control.
Another therapeutic approach for hyperglycemia and T2DM that manipulates BA levels involves inhibition of apical sodium-dependent bile acid transporter (ASBT). ASBT is expressed in the distal ileum and has an important role in BA reabsorption in the lumen of the small intestine, which is pivotal for enterohepatic recirculation. ASBT inhibitors reduce ileal BA absorption and induce BA excretion in the feces. In the liver, ABST inhibitors stimulate BA production by induction of Cyp7a1 and Cyp8b1 and suppression of Fgf15 expression in the ileum (Rao et al., 2016). Importantly, ASBT inhibitors improve insulin sensitivity and reduce hyperglycemia and elevated incretin levels in rodent models of diabetes (Chen et al., 2012; Wu et al., 2013) and diet-induced obesity and glucose intolerance (Rao et al., 2016). Further studies are required to determine the efficacy and safety of ASBT inhibitors in patients with T2DM.
Challenges and future perspectives
The knowledge gained from observations in mice and humans enhances our understanding that some BAs may play important roles in regulating the glycemic response in health and in T2DM. Mechanisms for these effects are diverse, as BA-FXR and TGR5 signaling modulates incretin excretion, hepatic glucose homeostasis, inflammation, energy expenditure, all of which have been convincingly shown to exert major implications on glucose and energy metabolism. Furthermore, the cross-talk between BAs and the gut microbiome leads to cross-regulation of both BAs and microbiome composition, the balance of which may impact the glycemic response. Thus, impaired BA signaling along with associated dysbiosis may contribute to T2DM and other metabolic complications associated with obesity (Fig. 3).
However, major challenges limit our understanding of BA contribution to the glycemic response in human health and disease. One major limitation relates to the fact that mice and humans are inherently different in many aspects related to BA biology. For example, mice and humans have different BA compositions, potentially leading to different physiological effects and interventional outcomes in respective studies. For example, mice produce the potent FXR antagonist tauro-β-muricholic acid (T-β-MCA), which is resistant to bacterial bile salt hydrolase and thus can maintain intestinal stability and serve as an intestinal FXR antagonist. As such, oral administration of a T-β-MCA derivative, glycine-β-muricholic acid (Gly-MCA), decreased murine FXR signaling in the ileum, resulting in improved obesity, insulin resistance, and liver steatosis associated with lower serum levels of ceramides (Jiang et al., 2015a,b). In contrast, humans cannot produce T-β-MCA and instead bear CDCA and cholic acid (CA) as their predominant BAs. These molecules may mediate different downstream effects than those seen in rodents. Another example of such functional interspecies variation includes the preferential induction in mice of intestinal FGF15 in response to FXR activation in contrast to a preferential induction of FGF19 in response to the same stimulus in humans. Thus, extrapolation of results obtained in mouse-based FGF15 studies to humans should be performed with caution. Even more generally, translation of mouse-based findings suggesting regulatory roles of BAs in glycemic responses may not necessarily translate to humans.
Additional limitations are related to the inherent variability in the composition and function of the gut microbiome in humans. This results in varying and highly person-specific BA profiles, which differentially impact disease pathogenesis and possibly the response to BA-associated medical interventions.
With those limitations and challenges notwithstanding, the use of synthetic antagonists of intestinal FXR (Cariou et al., 2006; Ma et al., 2006; Prawitt et al., 2011; Li et al., 2013; Jiang et al., 2015b; Xie et al., 2017) and agonists of TGR5 (Watanabe et al., 2006; Thomas et al., 2009; Kumar et al., 2012; Briere et al., 2015; Fang et al., 2015; Hodge and Nunez, 2016) showed promising preliminary results in improving glycemic control in obese and diabetic rodents. Intestinal FXR antagonists attenuated hepatic gluconeogenesis and lowered intestinal and serum ceramides, whereas TGR5 agonists promoted GLP-1 secretion from L cells and activated thermogenesis in brown adipocytes. Hence, an ideal treatment for hyperglycemia may combine intestinal-specific FXR antagonists, which would prevent undesirable effects stemming from hepatic FXR signaling, with TGR5 agonists. This tissue restriction is important because mice featuring a full-body deletion of FXR developed a high incidence of hepatic cancers (Kim et al., 2007; Yang et al., 2007), whereas mice featuring a liver-specific deficiency of FXR exhibited increased cholic acid–induced liver tumors (Kong et al., 2016). TGR5 activation can be developed for T2DM treatment in rodents and humans (Hodge and Nunez, 2016), but a systemic TGR5 agonist may increase gallbladder volume (Briere et al., 2015). Accordingly, an optimal intestine-specific TGR5 agonist would be able to induce secretion of incretins from L cells without producing other systemic adverse effects. Unfortunately, restricting TGR5 activation to the gut would impede the beneficial effects of TGR5 on energy metabolism in brown adipose tissue. Collectively, developing intestinal-specific FXR antagonists and TGR5 agonists may constitute a promising future approach for hyperglycemia treatment. A cautionary note is that the long-term effects of blocking intestinal FXR and activation of TGR5 in T2DM patients merit future evaluation.
FGF19 represents another potential BA-related therapeutic target. It is increasingly evident that intestinal induction of FGF19 by FXR signaling is positively correlated with glucose homeostasis (Fu et al., 2004; Kir et al., 2011; Sachdev et al., 2016). Moreover, FGF19 administration to obese and diabetic mice improved the glycemic response (Fu et al., 2004), whereas FGF19 was elevated in T2DM subjects after the achievement of normoglycemia (Sachdev et al., 2016). Together, this indicates that FGF19 induction may potentially serve as a novel therapeutic modality contributing to glycemic control in T2DM. However, FGF19 expression can also promote hepatocellular carcinoma (Sawey et al., 2011). Designing FGF19 analogues that retain the intestinal BA regulatory activity without promoting hepatic carcinogenesis (Zhou et al., 2014) could potentially improve glycemic control in diabetic patients while maintaining an adequate safety profile.
Collectively, the effect of BAs on metabolic functions is highly complex and tightly regulated, yet therapeutic approaches targeting BA signaling hold promise in contributing to improved glycemic responses in patients with T2DM and potentially in T1DM. The major challenge is the development of a drug that manipulates BA signaling in a tissue-specific manner that can significantly normalize the glycemic response without causing significant adverse effects. Such intervention may potentially contribute to the treatment and prevention of a variety of chronic metabolic syndrome–related diseases.
Acknowledgments
We thank the members of the Elinav laboratory for discussions and apologize to authors whose work was not cited because of space constraints.
H. Shapiro holds the Vera Rosenberg Schwartz Research Chair; A.A. Kolodziejczyk is supported by a European Molecular Biology Organization Long-Term Fellowship. E. Elinav is supported by Y. and R. Ungar, the Gurwin Family Fund for Scientific Research, the Leona M. and Harry B. Helmsley Charitable Trust, the Crown Endowment Fund for Immunological Research, the estate of J. Gitlitz, the estate of L. Hershkovich, the Benoziyo Endowment Fund for the Advancement of Science, the Adelis Foundation, J.L. and V. Schwartz, A. and G. Markovitz, A. and C. Adelson, the French National Center for Scientific Research, D.L. Schwarz, the Vera Rosenberg Schwartz Research Fellow Chair, L. Steinberg, J.N. Halpern, A. Edelheit, the European Research Council, Marie Curie Integration, the German-Israeli Foundation for Scientific Research and Development, the Israel Science Foundation, the Minerva Foundation, the Helmholtz Foundation, and the European Foundation for the Study of Diabetes. E. Elinav holds the Sir Marc and Lady Tania Feldmann Professorial Chair in Immunology, is a senior fellow of the Canadian Institute for Advanced Research, and is an international scholar at the Bill and Melinda Gates Foundation and Howard Hughes Medical Institute.
The authors declare no competing financial interests.
References
- Ahlberg J., Angelin B., Björkhem I., and Einarsson K.. 1977. Individual bile acids in portal venous and systemic blood serum of fasting man. Gastroenterology. 73:1377–1382. [PubMed] [Google Scholar]
- Ahmad N.N., Pfalzer A., and Kaplan L.M.. 2013. Roux-en-Y gastric bypass normalizes the blunted postprandial bile acid excursion associated with obesity. Int. J. Obes. 37:1553–1559. 10.1038/ijo.2013.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K.E., Kok E., and Javitt N.B.. 1972. Bile acid synthesis in man: metabolism of 7α-hydroxycholesterol-14C and 26-hydroxycholesterol-3H. J. Clin. Invest. 51:112–117. 10.1172/JCI106780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelin B., Björkhem I., Einarsson K., and Ewerth S.. 1982. Hepatic uptake of bile acids in man. Fasting and postprandial concentrations of individual bile acids in portal venous and systemic blood serum. J. Clin. Invest. 70:724–731. 10.1172/JCI110668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramaniyan N., Ananthanarayanan M., and Suchy F.J.. 2012. Direct methylation of FXR by Set7/9, a lysine methyltransferase, regulates the expression of FXR target genes. Am. J. Physiol. Gastrointest. Liver Physiol. 302:G937–G947. 10.1152/ajpgi.00441.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balderas C., Rupérez F.J., Ibañez E., Señorans J., Guerrero-Fernández J., Casado I.G., Gracia-Bouthelier R., García A., and Barbas C.. 2013. Plasma and urine metabolic fingerprinting of type 1 diabetic children. Electrophoresis. 34:2882–2890. [DOI] [PubMed] [Google Scholar]
- Bathena S.P., Thakare R., Gautam N., Mukherjee S., Olivera M., Meza J., and Alnouti Y.. 2015. Urinary bile acids as biomarkers for liver diseases I. Stability of the baseline profile in healthy subjects. Toxicol. Sci. 143:296–307. 10.1093/toxsci/kfu227 [DOI] [PubMed] [Google Scholar]
- Benoit B., Meugnier E., Castelli M., Chanon S., Vieille-Marchiset A., Durand C., Bendridi N., Pesenti S., Monternier P.A., Durieux A.C., et al. 2017. Fibroblast growth factor 19 regulates skeletal muscle mass and ameliorates muscle wasting in mice. Nat. Med. 23:990–996. [DOI] [PubMed] [Google Scholar]
- Bernstein H., Bernstein C., Payne C.M., and Dvorak K.. 2009. Bile acids as endogenous etiologic agents in gastrointestinal cancer. World J. Gastroenterol. 15:3329–3340. 10.3748/wjg.15.3329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrabah W., Aumercier P., Gheeraert C., Dehondt H., Bouchaert E., Alexandre J., Ploton M., Mazuy C., Caron S., Tailleux A., et al. 2014. Glucose sensing O-GlcNAcylation pathway regulates the nuclear bile acid receptor farnesoid X receptor (FXR). Hepatology. 59:2022–2033. 10.1002/hep.26710 [DOI] [PubMed] [Google Scholar]
- Bhutta H.Y., Rajpal N., White W., Freudenberg J.M., Liu Y., Way J., Rajpal D., Cooper D.C., Young A., Tavakkoli A., and Chen L.. 2015. Effect of Roux-en-Y gastric bypass surgery on bile acid metabolism in normal and obese diabetic rats. PLoS One. 10:e0122273 10.1371/journal.pone.0122273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blahová T., Peterková L., Leníček M., Vlachová M., Zemánková K., Adámková V., Vítek L., and Kovář J.. 2016. The effect of colesevelam treatment on bile acid and lipid metabolism and glycemic control in healthy men. Physiol. Res. 65:995–1003. [DOI] [PubMed] [Google Scholar]
- Briere D.A., Ruan X., Cheng C.C., Siesky A.M., Fitch T.E., Dominguez C., Sanfeliciano S.G., Montero C., Suen C.S., Xu Y., et al. 2015. Novel Small Molecule Agonist of TGR5 Possesses Anti-Diabetic Effects but Causes Gallbladder Filling in Mice. PLoS One. 10:e0136873 10.1371/journal.pone.0136873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broeders E.P., Nascimento E.B., Havekes B., Brans B., Roumans K.H., Tailleux A., Schaart G., Kouach M., Charton J., Deprez B., et al. 2015. The Bile Acid Chenodeoxycholic Acid Increases Human Brown Adipose Tissue Activity. Cell Metab. 22:418–426. 10.1016/j.cmet.2015.07.002 [DOI] [PubMed] [Google Scholar]
- Cariou B., van Harmelen K., Duran-Sandoval D., van Dijk T.H., Grefhorst A., Abdelkarim M., Caron S., Torpier G., Fruchart J.C., Gonzalez F.J., et al. 2006. The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice. J. Biol. Chem. 281:11039–11049. 10.1074/jbc.M510258200 [DOI] [PubMed] [Google Scholar]
- Chen L., Yao X., Young A., McNulty J., Anderson D., Liu Y., Nystrom C., Croom D., Ross S., Collins J., et al. 2012. Inhibition of apical sodium-dependent bile acid transporter as a novel treatment for diabetes. Am. J. Physiol. Endocrinol. Metab. 302:E68–E76. 10.1152/ajpendo.00323.2011 [DOI] [PubMed] [Google Scholar]
- Cheng S., Zou M., Liu Q., Kuang J., Shen J., Pu S., Chen L., Li H., Wu T., Li R., et al. 2017. Activation of Constitutive Androstane Receptor Prevents Cholesterol Gallstone Formation. Am. J. Pathol. 187:808–818. 10.1016/j.ajpath.2016.12.013 [DOI] [PubMed] [Google Scholar]
- Courcoulas A.P., Goodpaster B.H., Eagleton J.K., Belle S.H., Kalarchian M.A., Lang W., Toledo F.G., and Jakicic J.M.. 2014. Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial. JAMA Surg. 149:707–715. 10.1001/jamasurg.2014.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Aguiar Vallim T.Q., Tarling E.J., and Edwards P.A.. 2013. Pleiotropic roles of bile acids in metabolism. Cell Metab. 17:657–669. 10.1016/j.cmet.2013.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Giorgi S., Campos V., Egli L., Toepel U., Carrel G., Cariou B., Rainteau D., Schneiter P., Tappy L., and Giusti V.. 2015. Long-term effects of Roux-en-Y gastric bypass on postprandial plasma lipid and bile acids kinetics in female non diabetic subjects: A cross-sectional pilot study. Clin. Nutr. 34:911–917. 10.1016/j.clnu.2014.09.018 [DOI] [PubMed] [Google Scholar]
- Degirolamo C., Rainaldi S., Bovenga F., Murzilli S., and Moschetta A.. 2014. Microbiota modification with probiotics induces hepatic bile acid synthesis via downregulation of the Fxr-Fgf15 axis in mice. Cell Reports. 7:12–18. 10.1016/j.celrep.2014.02.032 [DOI] [PubMed] [Google Scholar]
- Devlin A.S., and Fischbach M.A.. 2015. A biosynthetic pathway for a prominent class of microbiota-derived bile acids. Nat. Chem. Biol. 11:685–690. 10.1038/nchembio.1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding L., Sousa K.M., Jin L., Dong B., Kim B.W., Ramirez R., Xiao Z., Gu Y., Yang Q., Wang J., et al. 2016. Vertical sleeve gastrectomy activates GPBAR-1/TGR5 to sustain weight loss, improve fatty liver, and remit insulin resistance in mice. Hepatology. 64:760–773. 10.1002/hep.28689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duez H., van der Veen J.N., Duhem C., Pourcet B., Touvier T., Fontaine C., Derudas B., Baugé E., Havinga R., Bloks V.W., et al. 2008. Regulation of bile acid synthesis by the nuclear receptor Rev-erbalpha. Gastroenterology. 135:689–698. 10.1053/j.gastro.2008.05.035 [DOI] [PubMed] [Google Scholar]
- Duran-Sandoval D., Cariou B., Percevault F., Hennuyer N., Grefhorst A., van Dijk T.H., Gonzalez F.J., Fruchart J.C., Kuipers F., and Staels B.. 2005. The farnesoid X receptor modulates hepatic carbohydrate metabolism during the fasting-refeeding transition. J. Biol. Chem. 280:29971–29979. 10.1074/jbc.M501931200 [DOI] [PubMed] [Google Scholar]
- Dutia R., Embrey M., O’Brien C.S., Haeusler R.A., Agénor K.K., Homel P., McGinty J., Vincent R.P., Alaghband-Zadeh J., Staels B., et al. 2015. Temporal changes in bile acid levels and 12α-hydroxylation after Roux-en-Y gastric bypass surgery in type 2 diabetes. Int. J. Obes. 39:806–813. 10.1038/ijo.2015.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta T., Kudva Y.C., Persson X.M., Schenck L.A., Ford G.C., Singh R.J., Carter R., and Nair K.S.. 2016. Impact of Long-Term Poor and Good Glycemic Control on Metabolomics Alterations in Type 1 Diabetic People. J. Clin. Endocrinol. Metab. 101:1023–1033. 10.1210/jc.2015-2640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyssen H., De Pauw G., Stragier J., and Verhulst A.. 1983. Cooperative formation of omega-muricholic acid by intestinal microorganisms. Appl. Environ. Microbiol. 45:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang S., Suh J.M., Reilly S.M., Yu E., Osborn O., Lackey D., Yoshihara E., Perino A., Jacinto S., Lukasheva Y., et al. 2015. Intestinal FXR agonism promotes adipose tissue browning and reduces obesity and insulin resistance. Nat. Med. 21:159–165. 10.1038/nm.3760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrannini E., Camastra S., Astiarraga B., Nannipieri M., Castro-Perez J., Xie D., Wang L., Chakravarthy M., and Haeusler R.A.. 2015. Increased Bile Acid Synthesis and Deconjugation After Biliopancreatic Diversion. Diabetes. 64:3377–3385. 10.2337/db15-0214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca V.A., Handelsman Y., and Staels B.. 2010. Colesevelam lowers glucose and lipid levels in type 2 diabetes: the clinical evidence. Diabetes Obes. Metab. 12:384–392. 10.1111/j.1463-1326.2009.01181.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman B.M., Goode E., Chen J., Oro A.E., Bradley D.J., Perlmann T., Noonan D.J., Burka L.T., McMorris T., Lamph W.W., et al. 1995. Identification of a nuclear receptor that is activated by farnesol metabolites. Cell. 81:687–693. 10.1016/0092-8674(95)90530-8 [DOI] [PubMed] [Google Scholar]
- Fu L., John L.M., Adams S.H., Yu X.X., Tomlinson E., Renz M., Williams P.M., Soriano R., Corpuz R., Moffat B., et al. 2004. Fibroblast growth factor 19 increases metabolic rate and reverses dietary and leptin-deficient diabetes. Endocrinology. 145:2594–2603. 10.1210/en.2003-1671 [DOI] [PubMed] [Google Scholar]
- Gälman C., Angelin B., and Rudling M.. 2005. Bile acid synthesis in humans has a rapid diurnal variation that is asynchronous with cholesterol synthesis. Gastroenterology. 129:1445–1453. 10.1053/j.gastro.2005.09.009 [DOI] [PubMed] [Google Scholar]
- Gälman C., Angelin B., and Rudling M.. 2011. Pronounced variation in bile acid synthesis in humans is related to gender, hypertriglyceridaemia and circulating levels of fibroblast growth factor 19. J. Intern. Med. 270:580–588. 10.1111/j.1365-2796.2011.02466.x [DOI] [PubMed] [Google Scholar]
- Gilliland S.E., and Speck M.L.. 1977. Deconjugation of bile acids by intestinal lactobacilli. Appl. Environ. Microbiol. 33:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gineste R., Sirvent A., Paumelle R., Helleboid S., Aquilina A., Darteil R., Hum D.W., Fruchart J.C., and Staels B.. 2008. Phosphorylation of farnesoid X receptor by protein kinase C promotes its transcriptional activity. Mol. Endocrinol. 22:2433–2447. 10.1210/me.2008-0092 [DOI] [PubMed] [Google Scholar]
- Glicksman C., Pournaras D.J., Wright M., Roberts R., Mahon D., Welbourn R., Sherwood R., Alaghband-Zadeh J., and le Roux C.W.. 2010. Postprandial plasma bile acid responses in normal weight and obese subjects. Ann. Clin. Biochem. 47:482–484. 10.1258/acb.2010.010040 [DOI] [PubMed] [Google Scholar]
- Goncalves D., Barataud A., De Vadder F., Vinera J., Zitoun C., Duchampt A., and Mithieux G.. 2015. Bile Routing Modification Reproduces Key Features of Gastric Bypass in Rat. Ann. Surg. 262:1006–1015. 10.1097/SLA.0000000000001121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin B., Jones S.A., Price R.R., Watson M.A., McKee D.D., Moore L.B., Galardi C., Wilson J.G., Lewis M.C., Roth M.E., et al. 2000. A regulatory cascade of the nuclear receptors FXR, SHP-1, and LRH-1 represses bile acid biosynthesis. Mol. Cell. 6:517–526. 10.1016/S1097-2765(00)00051-4 [DOI] [PubMed] [Google Scholar]
- Guo C., Qi H., Yu Y., Zhang Q., Su J., Yu D., Huang W., Chen W.D., and Wang Y.D.. 2015. The G-Protein-Coupled Bile Acid Receptor Gpbar1 (TGR5) Inhibits Gastric Inflammation Through Antagonizing NF-κB Signaling Pathway. Front. Pharmacol. 6:287 10.3389/fphar.2015.00287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo C., Xie S., Chi Z., Zhang J., Liu Y., Zhang L., Zheng M., Zhang X., Xia D., Ke Y., et al. 2016. Bile Acids Control Inflammation and Metabolic Disorder through Inhibition of NLRP3 Inflammasome. Immunity. 45:802–816. 10.1016/j.immuni.2016.09.008 [DOI] [PubMed] [Google Scholar]
- Haeusler R.A., Pratt-Hyatt M., Welch C.L., Klaassen C.D., and Accili D.. 2012. Impaired generation of 12-hydroxylated bile acids links hepatic insulin signaling with dyslipidemia. Cell Metab. 15:65–74. 10.1016/j.cmet.2011.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeusler R.A., Astiarraga B., Camastra S., Accili D., and Ferrannini E.. 2013. Human insulin resistance is associated with increased plasma levels of 12α-hydroxylated bile acids. Diabetes. 62:4184–4191. 10.2337/db13-0639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeusler R.A., Camastra S., Nannipieri M., Astiarraga B., Castro-Perez J., Xie D., Wang L., Chakravarthy M., and Ferrannini E.. 2016. Increased Bile Acid Synthesis and Impaired Bile Acid Transport in Human Obesity. J. Clin. Endocrinol. Metab. 101:1935–1944. 10.1210/jc.2015-2583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S., Zhang R., Jain R., Shi H., Zhang L., Zhou G., Sangwung P., Tugal D., Atkins G.B., Prosdocimo D.A., et al. 2015. Circadian control of bile acid synthesis by a KLF15-Fgf15 axis. Nat. Commun. 6:7231 10.1038/ncomms8231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen M., Sonne D.P., Mikkelsen K.H., Gluud L.L., Vilsbøll T., and Knop F.K.. 2017. Bile acid sequestrants for glycemic control in patients with type 2 diabetes: A systematic review with meta-analysis of randomized controlled trials. J. Diabetes Complications. 31:918–927. 10.1016/j.jdiacomp.2017.01.011 [DOI] [PubMed] [Google Scholar]
- Hashiguchi T., Arakawa S., Takahashi S., Gonzalez F.J., Sueyoshi T., and Negishi M.. 2016. Phosphorylation of Farnesoid X Receptor at Serine 154 Links Ligand Activation With Degradation. Mol. Endocrinol. 30:1070–1080. 10.1210/me.2016-1105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henao-Mejia J., Elinav E., Jin C., Hao L., Mehal W.Z., Strowig T., Thaiss C.A., Kau A.L., Eisenbarth S.C., Jurczak M.J., et al. 2012. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature. 482:179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho J.E., Larson M.G., Vasan R.S., Ghorbani A., Cheng S., Rhee E.P., Florez J.C., Clish C.B., Gerszten R.E., and Wang T.J.. 2013. Metabolite profiles during oral glucose challenge. Diabetes. 62:2689–2698. 10.2337/db12-0754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodge R.J., and Nunez D.J.. 2016. Therapeutic potential of Takeda-G-protein-receptor-5 (TGR5) agonists. Hope or hype? Diabetes Obes. Metab. 18:439–443. 10.1111/dom.12636 [DOI] [PubMed] [Google Scholar]
- Högenauer K., Arista L., Schmiedeberg N., Werner G., Jaksche H., Bouhelal R., Nguyen D.G., Bhat B.G., Raad L., Rauld C., and Carballido J.M.. 2014. G-protein-coupled bile acid receptor 1 (GPBAR1, TGR5) agonists reduce the production of proinflammatory cytokines and stabilize the alternative macrophage phenotype. J. Med. Chem. 57:10343–10354. 10.1021/jm501052c [DOI] [PubMed] [Google Scholar]
- Inagaki T., Choi M., Moschetta A., Peng L., Cummins C.L., McDonald J.G., Luo G., Jones S.A., Goodwin B., Richardson J.A., et al. 2005. Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab. 2:217–225. 10.1016/j.cmet.2005.09.001 [DOI] [PubMed] [Google Scholar]
- Ishibashi S., Schwarz M., Frykman P.K., Herz J., and Russell D.W.. 1996. Disruption of cholesterol 7alpha-hydroxylase gene in mice. I. Postnatal lethality reversed by bile acid and vitamin supplementation. J. Biol. Chem. 271:18017–18023. 10.1074/jbc.271.30.18017 [DOI] [PubMed] [Google Scholar]
- Islam K.B., Fukiya S., Hagio M., Fujii N., Ishizuka S., Ooka T., Ogura Y., Hayashi T., and Yokota A.. 2011. Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology. 141:1773–1781. 10.1053/j.gastro.2011.07.046 [DOI] [PubMed] [Google Scholar]
- Jiang C., Xie C., Li F., Zhang L., Nichols R.G., Krausz K.W., Cai J., Qi Y., Fang Z.Z., Takahashi S., et al. 2015a Intestinal farnesoid X receptor signaling promotes nonalcoholic fatty liver disease. J. Clin. Invest. 125:386–402. 10.1172/JCI76738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang C., Xie C., Lv Y., Li J., Krausz K.W., Shi J., Brocker C.N., Desai D., Amin S.G., Bisson W.H., et al. 2015b Intestine-selective farnesoid X receptor inhibition improves obesity-related metabolic dysfunction. Nat. Commun. 6:10166 10.1038/ncomms10166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones B.V., Begley M., Hill C., Gahan C.G., and Marchesi J.R.. 2008. Functional and comparative metagenomic analysis of bile salt hydrolase activity in the human gut microbiome. Proc. Natl. Acad. Sci. USA. 105:13580–13585. 10.1073/pnas.0804437105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jørgensen N.B., Dirksen C., Bojsen-Møller K.N., Kristiansen V.B., Wulff B.S., Rainteau D., Humbert L., Rehfeld J.F., Holst J.J., Madsbad S., and Clausen T.R.. 2015. Improvements in glucose metabolism early after gastric bypass surgery are not explained by increases in total bile acids and fibroblast growth factor 19 concentrations. J. Clin. Endocrinol. Metab. 100:E396–E406. 10.1210/jc.2014-1658 [DOI] [PubMed] [Google Scholar]
- Kakiyama G., Pandak W.M., Gillevet P.M., Hylemon P.B., Heuman D.M., Daita K., Takei H., Muto A., Nittono H., Ridlon J.M., et al. 2013. Modulation of the fecal bile acid profile by gut microbiota in cirrhosis. J. Hepatol. 58:949–955. 10.1016/j.jhep.2013.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katsuma S., Hirasawa A., and Tsujimoto G.. 2005. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem. Biophys. Res. Commun. 329:386–390. 10.1016/j.bbrc.2005.01.139 [DOI] [PubMed] [Google Scholar]
- Kawamata Y., Fujii R., Hosoya M., Harada M., Yoshida H., Miwa M., Fukusumi S., Habata Y., Itoh T., Shintani Y., et al. 2003. A G protein-coupled receptor responsive to bile acids. J. Biol. Chem. 278:9435–9440. 10.1074/jbc.M209706200 [DOI] [PubMed] [Google Scholar]
- Kellogg T.F., and Wostmann B.S.. 1969. Fecal neutral steroids and bile acids from germfree rats. J. Lipid Res. 10:495–503. [PubMed] [Google Scholar]
- Kemper J.K., Xiao Z., Ponugoti B., Miao J., Fang S., Kanamaluru D., Tsang S., Wu S.Y., Chiang C.M., and Veenstra T.D.. 2009. FXR acetylation is normally dynamically regulated by p300 and SIRT1 but constitutively elevated in metabolic disease states. Cell Metab. 10:392–404. 10.1016/j.cmet.2009.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D.H., Xiao Z., Kwon S., Sun X., Ryerson D., Tkac D., Ma P., Wu S.Y., Chiang C.M., Zhou E., et al. 2015. A dysregulated acetyl/SUMO switch of FXR promotes hepatic inflammation in obesity. EMBO J. 34:184–199. 10.15252/embj.201489527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim I., Morimura K., Shah Y., Yang Q., Ward J.M., and Gonzalez F.J.. 2007. Spontaneous hepatocarcinogenesis in farnesoid X receptor-null mice. Carcinogenesis. 28:940–946. 10.1093/carcin/bgl249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K.H., Choi S., Zhou Y., Kim E.Y., Lee J.M., Saha P.K., Anakk S., and Moore D.D.. 2017. Hepatic FXR/SHP axis modulates systemic glucose and fatty acid homeostasis in aged mice. Hepatology. 66:498–509. 10.1002/hep.29199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kir S., Beddow S.A., Samuel V.T., Miller P., Previs S.F., Suino-Powell K., Xu H.E., Shulman G.I., Kliewer S.A., and Mangelsdorf D.J.. 2011. FGF19 as a postprandial, insulin-independent activator of hepatic protein and glycogen synthesis. Science. 331:1621–1624. 10.1126/science.1198363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirwan W.O., Smith A.N., Mitchell W.D., Falconer J.D., and Eastwood M.A.. 1975. Bile acids and colonic motility in the rabbit and the human. Gut. 16:894–902. 10.1136/gut.16.11.894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi M., Ikegami H., Fujisawa T., Nojima K., Kawabata Y., Noso S., Babaya N., Itoi-Babaya M., Yamaji K., Hiromine Y., et al. 2007. Prevention and treatment of obesity, insulin resistance, and diabetes by bile acid-binding resin. Diabetes. 56:239–247. 10.2337/db06-0353 [DOI] [PubMed] [Google Scholar]
- Kohli R., Setchell K.D., Kirby M., Myronovych A., Ryan K.K., Ibrahim S.H., Berger J., Smith K., Toure M., Woods S.C., and Seeley R.J.. 2013. A surgical model in male obese rats uncovers protective effects of bile acids post-bariatric surgery. Endocrinology. 154:2341–2351. 10.1210/en.2012-2069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong B., Zhu Y., Li G., Williams J.A., Buckley K., Tawfik O., Luyendyk J.P., and Guo G.L.. 2016. Mice with hepatocyte-specific FXR deficiency are resistant to spontaneous but susceptible to cholic acid-induced hepatocarcinogenesis. Am. J. Physiol. Gastrointest. Liver Physiol. 310:G295–G302. 10.1152/ajpgi.00134.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuipers F., Stroeve J.H., Caron S., and Staels B.. 2007. Bile acids, farnesoid X receptor, atherosclerosis and metabolic control. Curr. Opin. Lipidol. 18:289–297. 10.1097/MOL.0b013e3281338d08 [DOI] [PubMed] [Google Scholar]
- Kumar D.P., Rajagopal S., Mahavadi S., Mirshahi F., Grider J.R., Murthy K.S., and Sanyal A.J.. 2012. Activation of transmembrane bile acid receptor TGR5 stimulates insulin secretion in pancreatic β cells. Biochem. Biophys. Res. Commun. 427:600–605. 10.1016/j.bbrc.2012.09.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar D.P., Asgharpour A., Mirshahi F., Park S.H., Liu S., Imai Y., Nadler J.L., Grider J.R., Murthy K.S., and Sanyal A.J.. 2016. Activation of Transmembrane Bile Acid Receptor TGR5 Modulates Pancreatic Islet α Cells to Promote Glucose Homeostasis. J. Biol. Chem. 291:6626–6640. 10.1074/jbc.M115.699504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalle M., Hoguet V., Hennuyer N., Leroux F., Piveteau C., Belloy L., Lestavel S., Vallez E., Dorchies E., Duplan I., et al. 2017. Topical Intestinal Aminoimidazole Agonists of G-Protein-Coupled Bile Acid Receptor 1 Promote Glucagon Like Peptide-1 Secretion and Improve Glucose Tolerance. J. Med. Chem. 60:4185–4211. 10.1021/acs.jmedchem.6b01873 [DOI] [PubMed] [Google Scholar]
- Lee J.M., Wagner M., Xiao R., Kim K.H., Feng D., Lazar M.A., and Moore D.D.. 2014. Nutrient-sensing nuclear receptors coordinate autophagy. Nature. 516:112–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefebvre P., Cariou B., Lien F., Kuipers F., and Staels B.. 2009. Role of bile acids and bile acid receptors in metabolic regulation. Physiol. Rev. 89:147–191. 10.1152/physrev.00010.2008 [DOI] [PubMed] [Google Scholar]
- Le Martelot G., Claudel T., Gatfield D., Schaad O., Kornmann B., Lo Sasso G., Moschetta A., and Schibler U.. 2009. REV-ERBalpha participates in circadian SREBP signaling and bile acid homeostasis. PLoS Biol. 7:e1000181 10.1371/journal.pbio.1000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., and Chiang J.Y.. 2014. Bile acid signaling in metabolic disease and drug therapy. Pharmacol. Rev. 66:948–983. 10.1124/pr.113.008201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Jiang C., Krausz K.W., Li Y., Albert I., Hao H., Fabre K.M., Mitchell J.B., Patterson A.D., and Gonzalez F.J.. 2013. Microbiome remodelling leads to inhibition of intestinal farnesoid X receptor signalling and decreased obesity. Nat. Commun. 4:2384 10.1038/ncomms3384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., Owsley E., Matozel M., Hsu P., Novak C.M., and Chiang J.Y.. 2010. Transgenic expression of cholesterol 7alpha-hydroxylase in the liver prevents high-fat diet-induced obesity and insulin resistance in mice. Hepatology. 52:678–690. 10.1002/hep.23721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., Francl J.M., Boehme S., Ochoa A., Zhang Y., Klaassen C.D., Erickson S.K., and Chiang J.Y.. 2012. Glucose and insulin induction of bile acid synthesis: mechanisms and implication in diabetes and obesity. J. Biol. Chem. 287:1861–1873. 10.1074/jbc.M111.305789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lien F., Berthier A., Bouchaert E., Gheeraert C., Alexandre J., Porez G., Prawitt J., Dehondt H., Ploton M., Colin S., et al. 2014. Metformin interferes with bile acid homeostasis through AMPK-FXR crosstalk. J. Clin. Invest. 124:1037–1051. 10.1172/JCI68815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Pathak P., Boehme S., and Chiang J.Y.. 2016. Cholesterol 7α-hydroxylase protects the liver from inflammation and fibrosis by maintaining cholesterol homeostasis. J. Lipid Res. 57:1831–1844. 10.1194/jlr.M069807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz T.A., and Bueter M.. 2014. The physiology underlying Roux-en-Y gastric bypass: a status report. Am. J. Physiol. Regul. Integr. Comp. Physiol. 307:R1275–R1291. 10.1152/ajpregu.00185.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma K., Saha P.K., Chan L., and Moore D.D.. 2006. Farnesoid X receptor is essential for normal glucose homeostasis. J. Clin. Invest. 116:1102–1109. 10.1172/JCI25604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makishima M., Okamoto A.Y., Repa J.J., Tu H., Learned R.M., Luk A., Hull M.V., Lustig K.D., Mangelsdorf D.J., and Shan B.. 1999. Identification of a nuclear receptor for bile acids. Science. 284:1362–1365. 10.1126/science.284.5418.1362 [DOI] [PubMed] [Google Scholar]
- Makishima M., Lu T.T., Xie W., Whitfield G.K., Domoto H., Evans R.M., Haussler M.R., and Mangelsdorf D.J.. 2002. Vitamin D receptor as an intestinal bile acid sensor. Science. 296:1313–1316. 10.1126/science.1070477 [DOI] [PubMed] [Google Scholar]
- McGavigan A.K., Garibay D., Henseler Z.M., Chen J., Bettaieb A., Haj F.G., Ley R.E., Chouinard M.L., and Cummings B.P.. 2017. TGR5 contributes to glucoregulatory improvements after vertical sleeve gastrectomy in mice. Gut. 66:226–234. 10.1136/gutjnl-2015-309871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton G.J., Matsen M.E., Bracy D.P., Meek T.H., Nguyen H.T., Stefanovski D., Bergman R.N., Wasserman D.H., and Schwartz M.W.. 2013. FGF19 action in the brain induces insulin-independent glucose lowering. J. Clin. Invest. 123:4799–4808. 10.1172/JCI70710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudaliar S., Henry R.R., Sanyal A.J., Morrow L., Marschall H.U., Kipnes M., Adorini L., Sciacca C.I., Clopton P., Castelloe E., et al. 2013. Efficacy and safety of the farnesoid X receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 145:574–582. 10.1053/j.gastro.2013.05.042 [DOI] [PubMed] [Google Scholar]
- Nagahashi M., Yuza K., Hirose Y., Nakajima M., Ramanathan R., Hait N.C., Hylemon P.B., Zhou H., Takabe K., and Wakai T.. 2016. The roles of bile acids and sphingosine-1-phosphate signaling in the hepatobiliary diseases. J. Lipid Res. 57:1636–1643. 10.1194/jlr.R069286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuschwander-Tetri B.A., Loomba R., Sanyal A.J., Lavine J.E., Van Natta M.L., Abdelmalek M.F., Chalasani N., Dasarathy S., Diehl A.M., Hameed B., et al. NASH Clinical Research Network . 2015. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 385:956–965. 10.1016/S0140-6736(14)61933-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks D.J., Blanchard S.G., Bledsoe R.K., Chandra G., Consler T.G., Kliewer S.A., Stimmel J.B., Willson T.M., Zavacki A.M., Moore D.D., and Lehmann J.M.. 1999. Bile acids: natural ligands for an orphan nuclear receptor. Science. 284:1365–1368. 10.1126/science.284.5418.1365 [DOI] [PubMed] [Google Scholar]
- Parséus A., Sommer N., Sommer F., Caesar R., Molinaro A., Ståhlman M., Greiner T.U., Perkins R., and Bäckhed F.. 2017. Microbiota-induced obesity requires farnesoid X receptor. Gut. 66:429–437. 10.1136/gutjnl-2015-310283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patti M.E., Houten S.M., Bianco A.C., Bernier R., Larsen P.R., Holst J.J., Badman M.K., Maratos-Flier E., Mun E.C., Pihlajamaki J., et al. 2009. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring). 17:1671–1677. 10.1038/oby.2009.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicciari R., Gioiello A., Macchiarulo A., Thomas C., Rosatelli E., Natalini B., Sardella R., Pruzanski M., Roda A., Pastorini E., et al. 2009. Discovery of 6alpha-ethyl-23(S)-methylcholic acid (S-EMCA, INT-777) as a potent and selective agonist for the TGR5 receptor, a novel target for diabesity. J. Med. Chem. 52:7958–7961. 10.1021/jm901390p [DOI] [PubMed] [Google Scholar]
- Perino A., Pols T.W., Nomura M., Stein S., Pellicciari R., and Schoonjans K.. 2014. TGR5 reduces macrophage migration through mTOR-induced C/EBPβ differential translation. J. Clin. Invest. 124:5424–5436. 10.1172/JCI76289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picard A., Soyer J., Berney X., Tarussio D., Quenneville S., Jan M., Grouzmann E., Burdet F., Ibberson M., and Thorens B.. 2016. A Genetic Screen Identifies Hypothalamic Fgf15 as a Regulator of Glucagon Secretion. Cell Reports. 17:1795–1806. 10.1016/j.celrep.2016.10.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pols T.W., Nomura M., Harach T., Lo Sasso G., Oosterveer M.H., Thomas C., Rizzo G., Gioiello A., Adorini L., Pellicciari R., et al. 2011. TGR5 activation inhibits atherosclerosis by reducing macrophage inflammation and lipid loading. Cell Metab. 14:747–757. 10.1016/j.cmet.2011.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potthoff M.J., Boney-Montoya J., Choi M., He T., Sunny N.E., Satapati S., Suino-Powell K., Xu H.E., Gerard R.D., Finck B.N., et al. 2011. FGF15/19 regulates hepatic glucose metabolism by inhibiting the CREB-PGC-1α pathway. Cell Metab. 13:729–738. 10.1016/j.cmet.2011.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potthoff M.J., Potts A., He T., Duarte J.A., Taussig R., Mangelsdorf D.J., Kliewer S.A., and Burgess S.C.. 2013. Colesevelam suppresses hepatic glycogenolysis by TGR5-mediated induction of GLP-1 action in DIO mice. Am. J. Physiol. Gastrointest. Liver Physiol. 304:G371–G380. 10.1152/ajpgi.00400.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prawitt J., Abdelkarim M., Stroeve J.H., Popescu I., Duez H., Velagapudi V.R., Dumont J., Bouchaert E., van Dijk T.H., Lucas A., et al. 2011. Farnesoid X receptor deficiency improves glucose homeostasis in mouse models of obesity. Diabetes. 60:1861–1871. 10.2337/db11-0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao A., Kosters A., Mells J.E., Zhang W., Setchell K.D., Amanso A.M., Wynn G.M., Xu T., Keller B.T., Yin H., et al. 2016. Inhibition of ileal bile acid uptake protects against nonalcoholic fatty liver disease in high-fat diet-fed mice. Sci. Transl. Med. 8:357ra122 10.1126/scitranslmed.aaf4823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathinam V.A., and Fitzgerald K.A.. 2016. Inflammasome Complexes: Emerging Mechanisms and Effector Functions. Cell. 165:792–800. 10.1016/j.cell.2016.03.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renga B., Mencarelli A., Vavassori P., Brancaleone V., and Fiorucci S.. 2010. The bile acid sensor FXR regulates insulin transcription and secretion. Biochim. Biophys. Acta. 1802:363–372. 10.1016/j.bbadis.2010.01.002 [DOI] [PubMed] [Google Scholar]
- Ryan K.K., Kohli R., Gutierrez-Aguilar R., Gaitonde S.G., Woods S.C., and Seeley R.J.. 2013. Fibroblast growth factor-19 action in the brain reduces food intake and body weight and improves glucose tolerance in male rats. Endocrinology. 154:9–15. 10.1210/en.2012-1891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan K.K., Tremaroli V., Clemmensen C., Kovatcheva-Datchary P., Myronovych A., Karns R., Wilson-Pérez H.E., Sandoval D.A., Kohli R., Bäckhed F., and Seeley R.J.. 2014. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 509:183–188. 10.1038/nature13135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachdev S., Wang Q., Billington C., Connett J., Ahmed L., Inabnet W., Chua S., Ikramuddin S., and Korner J.. 2016. FGF 19 and Bile Acids Increase Following Roux-en-Y Gastric Bypass but Not After Medical Management in Patients with Type 2 Diabetes. Obes. Surg. 26:957–965. 10.1007/s11695-015-1834-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawey E.T., Chanrion M., Cai C., Wu G., Zhang J., Zender L., Zhao A., Busuttil R.W., Yee H., Stein L., et al. 2011. Identification of a therapeutic strategy targeting amplified FGF19 in liver cancer by Oncogenomic screening. Cancer Cell. 19:347–358. 10.1016/j.ccr.2011.01.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayin S.I., Wahlström A., Felin J., Jäntti S., Marschall H.U., Bamberg K., Angelin B., Hyötyläinen T., Orešič M., and Bäckhed F.. 2013. Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab. 17:225–235. 10.1016/j.cmet.2013.01.003 [DOI] [PubMed] [Google Scholar]
- Schauer P.R., Bhatt D.L., Kirwan J.P., Wolski K., Aminian A., Brethauer S.A., Navaneethan S.D., Singh R.P., Pothier C.E., Nissen S.E., and Kashyap S.R.. STAMPEDE Investigators . 2017. Bariatric Surgery versus Intensive Medical Therapy for Diabetes—5-Year Outcomes. N. Engl. J. Med. 376:641–651. 10.1056/NEJMoa1600869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schittenhelm B., Wagner R., Kähny V., Peter A., Krippeit-Drews P., Düfer M., and Drews G.. 2015. Role of FXR in β-cells of lean and obese mice. Endocrinology. 156:1263–1271. 10.1210/en.2014-1751 [DOI] [PubMed] [Google Scholar]
- Schwarz M., Lund E.G., Setchell K.D., Kayden H.J., Zerwekh J.E., Björkhem I., Herz J., and Russell D.W.. 1996. Disruption of cholesterol 7alpha-hydroxylase gene in mice. II. Bile acid deficiency is overcome by induction of oxysterol 7alpha-hydroxylase. J. Biol. Chem. 271:18024–18031. 10.1074/jbc.271.30.18024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seok S., Fu T., Choi S.E., Li Y., Zhu R., Kumar S., Sun X., Yoon G., Kang Y., Zhong W., et al. 2014. Transcriptional regulation of autophagy by an FXR-CREB axis. Nature. 516:108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seol W., Choi H.S., and Moore D.D.. 1995. Isolation of proteins that interact specifically with the retinoid X receptor: two novel orphan receptors. Mol. Endocrinol. 9:72–85. [DOI] [PubMed] [Google Scholar]
- Shaham O., Wei R., Wang T.J., Ricciardi C., Lewis G.D., Vasan R.S., Carr S.A., Thadhani R., Gerszten R.E., and Mootha V.K.. 2008. Metabolic profiling of the human response to a glucose challenge reveals distinct axes of insulin sensitivity. Mol. Syst. Biol. 4:214 10.1038/msb.2008.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh Abdul Kadir S.H., Miragoli M., Abu-Hayyeh S., Moshkov A.V., Xie Q., Keitel V., Nikolaev V.O., Williamson C., and Gorelik J.. 2010. Bile acid-induced arrhythmia is mediated by muscarinic M2 receptors in neonatal rat cardiomyocytes. PLoS One. 5:e9689 10.1371/journal.pone.0009689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staudinger J.L., Goodwin B., Jones S.A., Hawkins-Brown D., MacKenzie K.I., LaTour A., Liu Y., Klaassen C.D., Brown K.K., Reinhard J., et al. 2001. The nuclear receptor PXR is a lithocholic acid sensor that protects against liver toxicity. Proc. Natl. Acad. Sci. USA. 98:3369–3374. 10.1073/pnas.051551698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinert R.E., Peterli R., Keller S., Meyer-Gerspach A.C., Drewe J., Peters T., and Beglinger C.. 2013. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring). 21:E660–E668. 10.1002/oby.20522 [DOI] [PubMed] [Google Scholar]
- Su J., Zhang Q., Qi H., Wu L., Li Y., Yu D., Huang W., Chen W.D., and Wang Y.D.. 2017. The G-protein-coupled bile acid receptor Gpbar1 (TGR5) protects against renal inflammation and renal cancer cell proliferation and migration through antagonizing NF-κB and STAT3 signaling pathways. Oncotarget. 8:54378–54387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann J.R., Want E.J., Geier F.M., Spagou K., Wilson I.D., Sidaway J.E., Nicholson J.K., and Holmes E.. 2011. Systemic gut microbial modulation of bile acid metabolism in host tissue compartments. Proc. Natl. Acad. Sci. USA. 108(Suppl 1):4523–4530. 10.1073/pnas.1006734107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas C., Gioiello A., Noriega L., Strehle A., Oury J., Rizzo G., Macchiarulo A., Yamamoto H., Mataki C., Pruzanski M., et al. 2009. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 10:167–177. 10.1016/j.cmet.2009.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trabelsi M.S., Daoudi M., Prawitt J., Ducastel S., Touche V., Sayin S.I., Perino A., Brighton C.A., Sebti Y., Kluza J., et al. 2015. Farnesoid X receptor inhibits glucagon-like peptide-1 production by enteroendocrine L cells. Nat. Commun. 6:7629 10.1038/ncomms8629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandanmagsar B., Youm Y.H., Ravussin A., Galgani J.E., Stadler K., Mynatt R.L., Ravussin E., Stephens J.M., and Dixit V.D.. 2011. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat. Med. 17:179–188. 10.1038/nm.2279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dijk T.H., Grefhorst A., Oosterveer M.H., Bloks V.W., Staels B., Reijngoud D.J., and Kuipers F.. 2009. An increased flux through the glucose 6-phosphate pool in enterocytes delays glucose absorption in Fxr-/- mice. J. Biol. Chem. 284:10315–10323. 10.1074/jbc.M807317200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahcevic Z.R., Miller J.R., Farrar J.T., and Swell L.. 1971. Kinetics and pool size of primary bile acids in man. Gastroenterology. 61:85–90. [PubMed] [Google Scholar]
- Wahlström A., Sayin S.I., Marschall H.U., and Bäckhed F.. 2016. Intestinal Crosstalk between Bile Acids and Microbiota and Its Impact on Host Metabolism. Cell Metab. 24:41–50. 10.1016/j.cmet.2016.05.005 [DOI] [PubMed] [Google Scholar]
- Wahlström A., Kovatcheva-Datchary P., Ståhlman M., Khan M.T., Bäckhed F., and Marschall H.U.. 2017. Induction of farnesoid X receptor signaling in germ-free mice colonized with a human microbiota. J. Lipid Res. 58:412–419. 10.1194/jlr.M072819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Chen J., Hollister K., Sowers L.C., and Forman B.M.. 1999. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol. Cell. 3:543–553. 10.1016/S1097-2765(00)80348-2 [DOI] [PubMed] [Google Scholar]
- Wang Y.D., Chen W.D., Yu D., Forman B.M., and Huang W.. 2011. The G-protein-coupled bile acid receptor, Gpbar1 (TGR5), negatively regulates hepatic inflammatory response through antagonizing nuclear factor κ light-chain enhancer of activated B cells (NF-κB) in mice. Hepatology. 54:1421–1432. 10.1002/hep.24525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M., Houten S.M., Wang L., Moschetta A., Mangelsdorf D.J., Heyman R.A., Moore D.D., and Auwerx J.. 2004. Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c. J. Clin. Invest. 113:1408–1418. 10.1172/JCI21025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M., Houten S.M., Mataki C., Christoffolete M.A., Kim B.W., Sato H., Messaddeq N., Harney J.W., Ezaki O., Kodama T., et al. 2006. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 439:484–489. 10.1038/nature04330 [DOI] [PubMed] [Google Scholar]
- Watanabe M., Horai Y., Houten S.M., Morimoto K., Sugizaki T., Arita E., Mataki C., Sato H., Tanigawara Y., Schoonjans K., et al. 2011. Lowering bile acid pool size with a synthetic farnesoid X receptor (FXR) agonist induces obesity and diabetes through reduced energy expenditure. J. Biol. Chem. 286:26913–26920. 10.1074/jbc.M111.248203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickremesekera K., Miller G., Naotunne T.D., Knowles G., and Stubbs R.S.. 2005. Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obes. Surg. 15:474–481. 10.1381/0960892053723402 [DOI] [PubMed] [Google Scholar]
- Worthmann A., John C., Rühlemann M.C., Baguhl M., Heinsen F.A., Schaltenberg N., Heine M., Schlein C., Evangelakos I., Mineo C., et al. 2017. Cold-induced conversion of cholesterol to bile acids in mice shapes the gut microbiome and promotes adaptive thermogenesis. Nat. Med. 23:839–849. 10.1038/nm.4357 [DOI] [PubMed] [Google Scholar]
- Wu Y., Aquino C.J., Cowan D.J., Anderson D.L., Ambroso J.L., Bishop M.J., Boros E.E., Chen L., Cunningham A., Dobbins R.L., et al. 2013. Discovery of a highly potent, nonabsorbable apical sodium-dependent bile acid transporter inhibitor (GSK2330672) for treatment of type 2 diabetes. J. Med. Chem. 56:5094–5114. 10.1021/jm400459m [DOI] [PubMed] [Google Scholar]
- Xie C., Jiang C., Shi J., Gao X., Sun D., Sun L., Wang T., Takahashi S., Anitha M., Krausz K.W., et al. 2017. An Intestinal Farnesoid X Receptor-Ceramide Signaling Axis Modulates Hepatic Gluconeogenesis in Mice. Diabetes. 66:613–626. 10.2337/db16-0663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F., Huang X., Yi T., Yen Y., Moore D.D., and Huang W.. 2007. Spontaneous development of liver tumors in the absence of the bile acid receptor farnesoid X receptor. Cancer Res. 67:863–867. 10.1158/0008-5472.CAN-06-1078 [DOI] [PubMed] [Google Scholar]
- Yesair D.W., and Himmelfarb P.. 1970. Hydrolysis of conjugated bile acids by cell-free extracts from aerobic bacteria. Appl. Microbiol. 19:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Kast-Woelbern H.R., and Edwards P.A.. 2003. Natural structural variants of the nuclear receptor farnesoid X receptor affect transcriptional activation. J. Biol. Chem. 278:104–110. 10.1074/jbc.M209505200 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Lee F.Y., Barrera G., Lee H., Vales C., Gonzalez F.J., Willson T.M., and Edwards P.A.. 2006. Activation of the nuclear receptor FXR improves hyperglycemia and hyperlipidemia in diabetic mice. Proc. Natl. Acad. Sci. USA. 103:1006–1011. 10.1073/pnas.0506982103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ge X., Heemstra L.A., Chen W.D., Xu J., Smith J.L., Ma H., Kasim N., Edwards P.A., and Novak C.M.. 2012. Loss of FXR protects against diet-induced obesity and accelerates liver carcinogenesis in ob/ob mice. Mol. Endocrinol. 26:272–280. 10.1210/me.2011-1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M., Wang X., Phung V., Lindhout D.A., Mondal K., Hsu J.Y., Yang H., Humphrey M., Ding X., Arora T., et al. 2014. Separating Tumorigenicity from Bile Acid Regulatory Activity for Endocrine Hormone FGF19. Cancer Res. 74:3306–3316. 10.1158/0008-5472.CAN-14-0208 [DOI] [PubMed] [Google Scholar]
- Zieve F.J., Kalin M.F., Schwartz S.L., Jones M.R., and Bailey W.L.. 2007. Results of the glucose-lowering effect of WelChol study (GLOWS): a randomized, double-blind, placebo-controlled pilot study evaluating the effect of colesevelam hydrochloride on glycemic control in subjects with type 2 diabetes. Clin. Ther. 29:74–83. 10.1016/j.clinthera.2007.01.003 [DOI] [PubMed] [Google Scholar]