Abstract
Background:
Thoracic interfascial plane blocks and modification (PECS) have recently gained popularity for analgesic potential during breast surgery. We evaluate/consolidate the evidence on opioid-sparing effect of PECS blocks in comparison with conventional intravenous analgesia (IVA) and paravertebral block (PVB).
Materials and Methods:
Prospective, randomized controlled trials comparing PECS block to conventional IVA or PVB in patients undergoing breast surgery published till June 2017 were searched in the medical database. Comparisons were made for 24-h postoperative morphine consumption and intraoperative fentanyl-equivalent consumption.
Results:
Final analysis included nine trials (PECS vs. IVA 4 trials and PECS vs. PVB 5 trials). PECS block showed a decreased intraoperative fentanyl consumption over IVA by 49.20 mcg (95% confidence interval [CI] =42.67–55.74) (I2 = 98.47%, P < 0.001) and PVB by 15.88 mcg (95% CI = 12.95–18.81) (I2 = 95.51%, P < 0.001). Postoperative, 24-h morphine consumption with PECS block was lower than IVA by 7.66 mg (95% CI being 6.23–9.10) (I2 = 63.15, P < 0.001) but was higher than PVB group by 1.26 mg (95% CI being 0.91–1.62) (I2 = 99.53%, P < 0.001). Two cases of pneumothorax were reported with PVB, and no complication was reported in any other group.
Conclusions:
Use of PECS block and its modifications with general anesthesia for breast surgery has significant opioid-sparing effect intraoperatively and during the first 24 h after surgery. It also has higher intraoperative opioid-sparing effect when compared to PVB. During the 1st postoperative day, PVB has slightly more morphine sparing potential that may however be associated with higher complication rates. The present PECS block techniques show marked interstudy variations and need standardization.
Keywords: Breast augmentation surgery, breast surgery, pectoral blocks, postoperative pain, regional anesthesia, serratus plane block
Introduction
The transversus abdominis plane (TAP) block has become the preferred and safe analgesic technique for abdominal surgeries over the last decade. The advent of ultrasound-guided regional anesthesia has further enhanced anesthesiologist's skills in such peripheral block. Analogous, to the TAP block, similar idea of blocking thoracic spinal nerves has also attracted recent attention. Blanco[1] described the technique of injecting local anesthetic into the interfascial muscle planes within the anterior thoracic wall and named it the “PECS” block. The idea was simple and innovative yet safer than all other regional anesthesia options available for the thoracic dermatomes. Over the last few years, many anesthesiologists have evaluated the analgesic efficacy of PECS block in various thoracic surgeries such as insertion of breast expanders, pacemakers, video-assisted thoracoscopic surgery (VATS), chest tube insertion, and breast cancer surgeries.[2,3,4] As many anesthesiologists incorporated these blocks in their clinical practice, many modifications were also developed over time. Classically, injection between pectoralis major and pectoralis minor was labeled as PECS-I and injection between pectoralis minor was called the PECS-II block.[5] Moving further, more modifications that involved injecting local anesthetic between serratus anterior and the intercostal muscle were described.[6] All these modifications aimed to improve the safety and the accuracy of the block.
The future potential of this block can be adjudged from the fact that within the span of last 5 years or so, many anesthesiologists have adopted these techniques in their clinical practice. Further, numerous trials focusing on the analgesic potential of PECS block have been conducted globally. Breast surgery has been the key area of utility for this block. Comparisons have been made with conventional intravenous analgesic (IVA) regimens and with the popular paravertebral block (PVB). It is intuitive that the PECS block is much less invasive compared to the PVB.[7] However, its comparative analgesic ability remains yet to be completely quantified. We, in this meta-analysis, consolidate the available evidence comparing PECS block and its modifications to the commonly used analgesic techniques used in patients undergoing unilateral breast surgery.
Materials and Methods
We conducted this meta-analysis abiding to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [Figure 1].[8] For the appropriate identification of the potential trials that could be utilized in our analysis, we adopted the Population, Intervention, Control and Outcome Study (PICOS) design [Table 1]. After extensive literature search, all trials were abstracted into a standardized PICOS format. The relevance of abstracted trials to our study aim was assessed by two independent reviewers. Randomized controlled trials comparing PECS block's analgesic potential in unilateral breast surgery to PVB or IVA regimens were included. Comparative, postoperative intravenous morphine equivalents consumption during the first 24 h was evaluated as the primary outcome in our pooled analysis. Parameters that were consistently compared and documented across various trials were also planned to be included as explorative outcomes. The salient features of trials included in the final analysis that met the above criterion are shown in Table 2.
Figure 1.
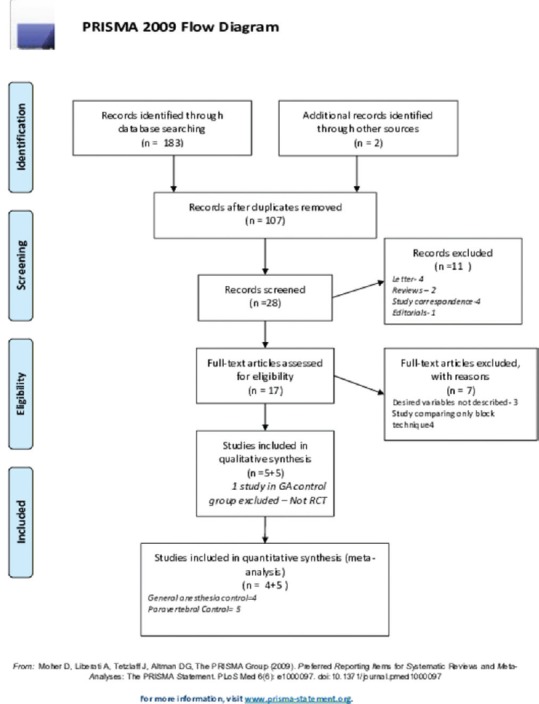
Preferred Reporting Items for Systematic Review and Meta-Analysis flow diagram illustrating flowchart outlining retrieved, excluded, and included studies
Table 1.
Population, intervention, control and outcome study data extraction framework
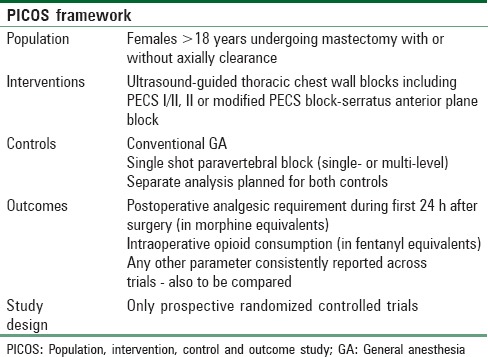
Table 2.
Characteristics of included studies
Literature search strategy
Online literature available on Medline, EMBASE, Scopus, Cochrane Central Register of Controlled Trials, Science Citation Index (SCI) Expanded, Google Scholar, Clinical Trials Registry and Meta-register of controlled for published manuscripts till June 3, 2017, was searched by two independent reviewers. Bibliographies and references of selected publications and reviews and editorials on analgesic regimens for breast surgery were also screened using Web of Science (SCI/Social SCI). The following medical subject heading (MeSH) terms were searched for in the above said database - Randomized controlled trial PECS block, PECS vs. Paravertebral, Serratus anterior plane block breast surgery, morphine sparing PECS block breast surgery. We excluded the following terms from the search string – retrospective cohort trial, video-assisted thoracoscopic surgery, breast expander analgesia. We strictly adhered to include only prospective randomized controlled trials only. We included only trials where PECS block was used for breast surgery for oncological surgery. We also avoided trials that used additional nerve blocks in combination with PECS block to evaluate efficacy of PECS block alone. Our search targeted to include research articles published either as full manuscripts or meeting abstracts in only after stringent peer review. We also manually searched the references of comparable meta-analysis for relevant trials. Our search extended to include trials published in both English and non-English languages. Once the abstract was analyzed by the searching reviewer and found appropriate the full text of the article was studied. The decision to include a trial into the pooled analysis was based on the assessment by two independent reviewers. Any disagreements on including a study were harmonized by consensus and arbitration by a third neutral reviewer. Methodological bias and study quality of the of the included trials were assessed based on the recommendations by the Cochrane Collaboration by another independent neutral researcher.[18]
Data extraction and principal endpoints
Pertinent data were extracted from the full-text manuscript of each included study. These data were gathered using a standardized data extraction form prepared in Microsoft Excel for Windows (Microsoft Inc., USA). The following data were extracted from each of the included trials - year and country of publication, study design, nature of breast surgery, analgesic regimen used (intravenous, PECS block, PVB, patient-controlled analgesia), local anesthetic used for block, strength and volume of local anesthetic for block, vertebral level of block (for PVB), single level or multilevel block, numeric pain scores (NPSs) reported by patient-on the day of surgery (within 6 h of surgery), intraoperative opioid use in fentanyl equivalents, total opioid consumption in the postoperative period during first 24 h (in morphine equivalents), comparative postoperative nausea vomiting (PONV) incidence. We attempted to extract frequency data of individual complications for detailed analysis; however, reporting was very inconsistent among trials with most trials just grouping complications, and thus, an analysis was not possible. If, in any trial, the data were found to be incomplete, attempts were made to contact the corresponding author via the e-mail for the relevant data. Wherever the data of interest were expressed as median and interquartile range, authors were contacted for the mean and standard deviation (SD) values. However, if no response was obtained, we estimated the mean and SD using the validated Hozo's formula.[19,20] In trials where variance associated with means was not reported, we imputed these variances as per Cochrane Collaboration recommendations using mean from available variances from other included studies.[21,22] All the trials reporting postoperative opioid consumption expressed values as “morphine equivalents.” Intraoperative opioid consumption was reported by most of the trials in terms of fentanyl equivalents. Wherever values were reported in terms of any other opioid, conversions were made based upon the well-established evidence-based dose conversion recommendations.[23] All our pooled analysis could be made for two separate comparisons:
PECS block versus conventional analgesic regimens that included the use of IVA as opioids
PECS block versus the single shot PVB.
The following variables were pooled for both the above comparisons:
Postoperative opioid consumption - This included total opioid consumption during the first 24 h after surgery
Intraoperative opioid consumption - This included the opioid analgesics consumed during the surgery. Most studies reported the doses in fentanyl equivalents. If, however, doses were reported in any other form of opioid, it was converted into intravenous fentanyl equivalents based on the potency charts.
We attempted to generate pooled comparison for other variables – such as NPSs during recovery stay, time to first analgesia, and PONV rates. These variables were not reported across more than two trials, and PONV rates had zero values in most trials. Thus, pooling such values has almost no statistical meaning.
Statistical methods
The statistical analysis of the pooled data was performed using Comprehensive Meta-analysis-Version 2 (Biostat Inc., USA). I2 statistic was used to quantify the heterogeneity between the trials. Meta-analysis was performed using fixed-effect modeling and subsequently random-effect modeling if heterogeneity was found to be higher than >40%. Values of I2 <40% were considered nonsignificant, 40%–60% were considered to represent moderate heterogeneity, and 60%–90% were reported as high heterogeneity. Results were expressed as pooled means/pooled mean difference for continuous variables with 95% confidence interval [CI]. P = 0.05 was considered statistically significant.
Risk of bias assessment
All relevant trials those were included in the present comparison were reviewed manually by a neutral reviewer for methodological bias. Criteria that were used for assessing the risk of bias were based upon the recommendations of the Cochrane Collaboration[24] and included method of randomization; concealed treatment allocation; blinding during pre-, peri-, and postoperative care; blinded data collection and analysis; blinded adjudication of study endpoints; and completeness of data. The graphical synopsis of the above assessment was constructed using the software Review Manager 5 (Cochrane Collaboration).
Studies were also assessed for a possible publication bias initially using a funnel plot and later quantified using the Egger's test.
Results
During our preliminary search, we found a total of 186 publications matching our search criterion in the above database. From these, duplicate search results were removed using Endnote (Thompson Reuters, USA). No unpublished/incomplete trial was found suitable during the search. One trial by Jabbar et al.[12] was identified by manual search of references using Google Scholar. We did not find any non-English trial to be suitable. Trial by Morioka et al.[25] closely met our inclusion criterion (PECS block vs. IVA) but was eventually excluded as it was a retrospective cohort comparison and not a prospective randomized controlled trial. Eventually, we found four suitable trials evaluating PECS block to IVA regimens and five trials comparing PECS to PVB for breast surgery. Of these nine trials, four used bupivacaine and two trials used levobupivacaine and ropivacaine each. El-Sheikh et al.[17] did not describe the local anesthetic used rather continued to mention local anesthetic throughout the manuscript. Six of the included trials preferred to perform the block before general anesthesia under sedation [Table 2]. Only Gupta et al.[13] used PECS block after inducing general anesthesia to the patient. Jabbar et al. in their abstract did not describe the timing of the block. None of the trials that used PECS block (or modifications) under sedation reported significant patient discomfort. No complications related to PECS block procedure (pneumothorax, bleeding, etc. were reported by any of the trials). Complications (if any) in case of control group are reported in Table 2.
Our results were divided into two separate comparisons with PECS block:
PECS block versus intravenous analgesia groups
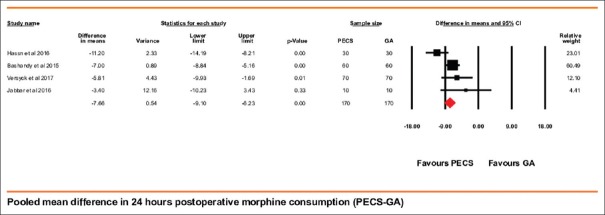
Postoperative morphine consumption
Data for this comparison were available in all the four trials that included 170 patients each in the PECS block and the control group. Patients receiving PECS block showed significantly lower morphine requirements in the first 24 h after the surgery. Overall PECS block showed a morphine sparing effect of 7.66 (95% CI being 6.23–9.10) mg, P < 0.001 [Figure 2]. The mean morphine consumption in the control group was 11.34 mg and this reduction meant a drop of nearly 67.55% in the total opioid consumption. The heterogeneity for this comparison was 63.15%. To explore this high heterogeneity, we performed a “single study removal method sensitivity analysis.” The study by Hassn et al. contributed highest to the heterogeneity and upon its removal heterogeneity dropped to zero percent. The effect size however did not change after its exclusion.
Figure 2.
Forest plot showing pooled mean difference in postoperative morphine equivalents consumption during first 24 h after surgery (PECS block group – general anesthesia control group). Solid diamond at the bottom of comparison denotes the final net effect
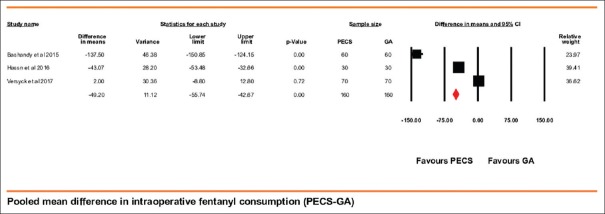
Intraoperative fentanyl consumption
There was marked variation in intraoperative fentanyl consumption across the studies. Values were available for three of the four included trials for this variable. Cumulative values were available for 160 patients in each group. Jabbar et al. did not report the dose fentanyl consumed during the surgery. Mean fentanyl consumption in patients receiving PECS block was lower by 49.20 (95% CI being 42.67–55.74) mcg, P < 0.001. The heterogeneity for this comparison was high being 98.47% [Figure 3]. We used a sensitivity analysis using the “single study removal method” to explore the high heterogeneity. A trial by Versyck et al. contributed the highest toward the total heterogeneity and its removal dropped the heterogeneity to 92.73%.
Figure 3.
Forest plot showing pooled mean difference in intraoperative fentanyl equivalents during the intraoperative period (PECS block group – general anesthesia control group). Solid diamond at the bottom of comparison denotes the final net effect
PECS block versus paravertebral block
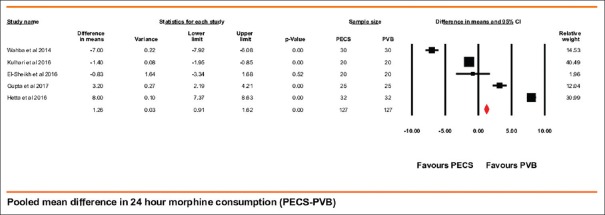
Postoperative morphine consumption
These data were available in five trials that included 127 patients in both PECS group and paravertebral group. Morphine consumption was lower with the use of PVB by 1.26 (95% CI being 0.91–1.62) mg, P < 0.001 [Figure 4]. This comparison had very high heterogeneity with I2 being 99.53% (random-effect modeling). A study by Wahba et al. contributed the highest to the heterogeneity. On sensitivity analysis using the single study removal technique, there was a further drop in heterogeneity by 18% although the effect size did not change significantly. The mean morphine consumption in the PVB group was 11.24, which was around 11.20% less than that reported in the PECS cumulative group.
Figure 4.
Forest plot showing pooled mean difference in postoperative morphine equivalents consumption during first 24 h after surgery (PECS block group – paravertebral control group). Solid diamond at the bottom of comparison denotes the final net effect
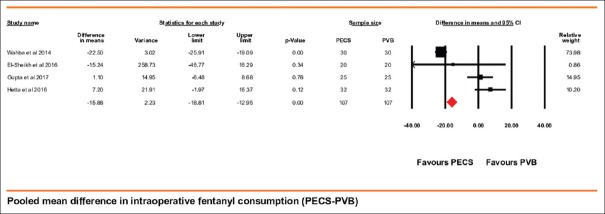
Intraoperative fentanyl consumption
Intraoperative fentanyl consumption was reported by four trials that included 107 patients in both the groups. Kulhari et al. did not report the intraoperative fentanyl consumption. PECS block group performed better and required smaller dose of fentanyl. Paravertebral group required 15.88 (95% CI being 12.95–18.81) mcg more fentanyl than PECS block group (P < 0.001) [Figure 5]. The heterogeneity of the above-pooled analysis was 95.51% (random effects modeling). We explored for this high heterogeneity using single study removal method. The study by Wahba et al. contributed highest to the heterogeneity, and upon its removal, it dropped to 29.93%; however, the net beneficial effect of block drooped to only 2.95 mcg.
Figure 5.
Forest plot showing pooled mean difference in intraoperative fentanyl equivalents during the intraoperative period (PECS block group – paravertebral block control group). Solid diamond at the bottom of comparison denotes the final net effect
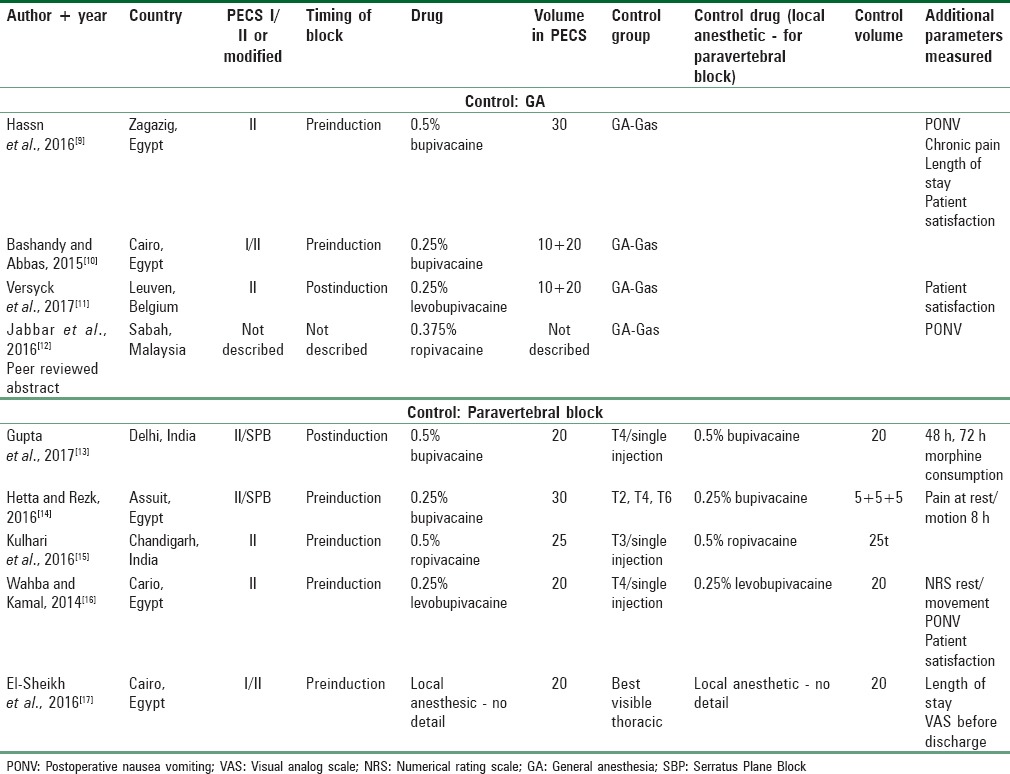
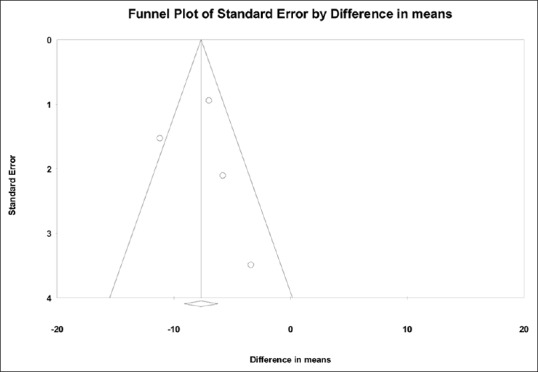
Assessment of publication bias
Primary variable (postoperative morphine consumption) was assessed for possible publication in both the comparisons. The funnel plot showed symmetrical study distribution in both general anesthesia comparison [Figure 6] and PVB comparison [Figure 7]. Further, the Egger's regression test for general anesthesia control group showed the intercept at −2.12 with a P = 0.70, and for PVB group, the intercept was at −5.32 with a P = 0.80. Thus, publication bias was unlikely in both the comparisons.
Figure 6.
Funnel plot evaluating publication bias for postoperative morphine consumption (comparing PECS block to general anesthesia control). A positive publication bias is unlikely with X-intercept at −2.12 with P = 0.70 (2-tailed)
Figure 7.
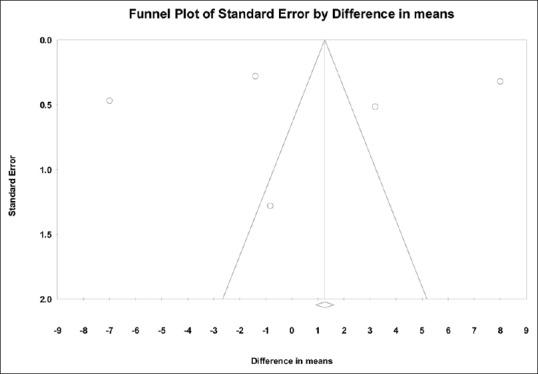
Funnel plot evaluating publication bias for postoperative morphine consumption (comparing PECS block to paravertebral control). A positive publication bias is unlikely with X-intercept at −5.32 With P = 0.80 (two-tailed)
Study quality assessment
Quality assessment for bias in the included studies was carried out as per other published meta-analysis and the guidelines laid by the Cochrane Collaboration. These results are shown in Figure 8. We used Review Manager Version 5.3 (Cochrane Collaboration) for this evaluation and image generation.
Figure 8.
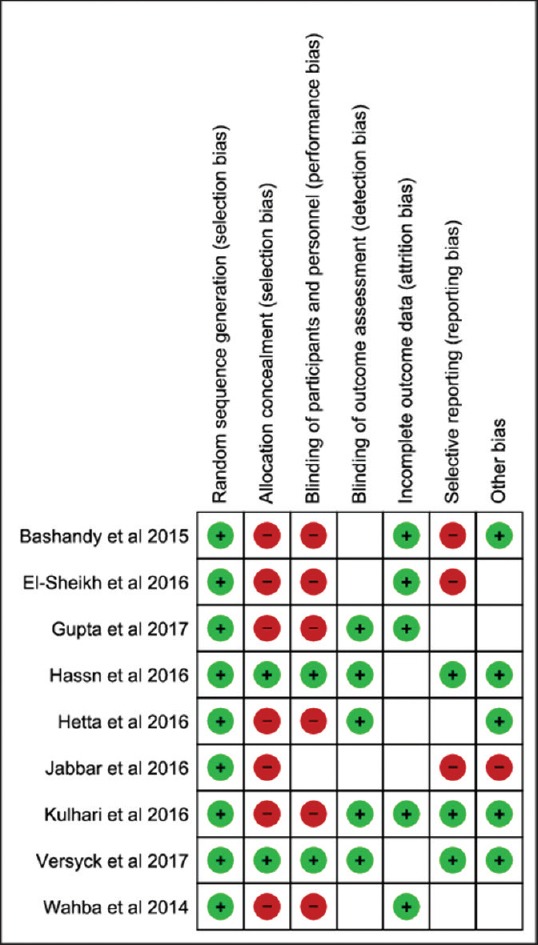
Risk of bias - Summary of all analyzed studies as per the Cochrane Collaboration reformations
Discussion
Thoracic wall interfascial plane blocks have a shallow learning curve. They are emerging as a safe and effective option for analgesia in breast surgery. The present meta-analysis is a first step toward consolidation of the available evidence. Our results have many clinical implications. First and foremost being that the use of PECS block (or its modifications) has a significant opioid-sparing effect in the perioperative period. The use of PECS block in the perioperative period reduced the morphine requirements by nearly 2/3rd. Many of the included studies targeted to maintain NPS below 3; thus, the target level of analgesia was comparable across the trials. Groups that used blocks were able to attain this target using much smaller doses of opioids. This has far lasting effect as opioid use in the perioperative period is known to be directly associated with pulmonary complication and nausea vomiting.[26] Interestingly, most of the studies performed the block in awake patients (under sedation); however, none found/reported patient discomfort.
The analgesic effect of block is clearly demonstrable during the intraoperative period. This was evident based on the reduced fentanyl requirements. An important aspect of our results is that although the PVB outperformed the PECS block in the postoperatively (although marginally), the use of PECS block lowered intraoperative fentanyl more. This can be related to one of the known disadvantage of PVB. It is known to have slow onset and takes longer to reach a peak effect.[27] Studies have reported time to surgical anesthesia more than 20 min with the use of PVB.[28] For breast surgery, these values can be significant, so till the peak effect of the block is attained; patient may have already required opioid supplementation. The analgesic benefits of PECS block clearly extend beyond the immediate intraoperative period. In an interesting volunteer-based study, Blanco et al.[29] demonstrated that the sensory blockade of serratus anterior plane block can last up to 840 min. As a result, the PECS block is expected to have sustained analgesic effects. This again is supported by our demonstration of morphine requirement reduction spanning to 24 h after surgery.
Our results also demonstrate that for postoperative pain, PVB has slightly better efficacy than PECS block. Although PVB has nearly 11% lower analgesic requirement, this does come at a price. PVB is relatively challenging to perform and in more invasive in nature. It is not uncommon to miss the vertebral transverse process even under ultrasound guidance and advance the needle further into pleura causing pneumothorax while performing the block.[30] El-Sheikh et al. (included in our analysis) reported a 10% pneumothorax rate with PVB. Thoracic epidurals can provide dense analgesia for the thoracic dermatomes; however, their use is limited by strong safety concerns. Analogous to this thoracic paravertebral is also relatively an invasive procedure. Having complications related to central neuraxial block is not completely ruled out.[31] The aim of bringing out these limitations with PVB is not to discourage its use; however, its use needs to be evaluated against the other safer available options. In the hands of an expert with ultrasound, these complication rates may reduce further with practice.
In our analysis, we faced many challenges. All the pooled results suffered high heterogeneity. This is attributed to variations in the PECS blocks used. Many trials included in our analysis not only used different approaches for the block, but also there was significant variation in the nature, concentration, and volume of the local anesthetic used. All these factors could have led to high variation in the block efficacy and thus the resultant heterogeneity. However, there are learning points from this aspect as well. It simply could imply the need for standardization of the block technique and the drug doses/volumes. Understandably, PECS block is a relatively new technique and variation in block performance is likely to persist in the early phase. Our present meta-analysis demonstrating early yet clear benefits would draw away inhibitions of anesthesiologists to adopt these techniques.
Our meta-analysis has many limitations. As already stated, the high heterogeneity could be because of the lack of uniformity of block techniques across countries. Once the block is more commonly used, it is likely the techniques will further evolve into a more uniform procedure. As we explored for the heterogeneity in our results, removal of studies with significant methodological variations brought down the heterogeneity. We were able to point out the possibility of methodological variations as primary source of heterogeneity as most of the effect sizes (baring intraoperative fentanyl consumption in PVB comparison) remained almost unaffected after this analysis. This further supports the possibility of interstudy block technique variation as the cause of pooled heterogeneity. We attempted to compare variables such as time to first analgesia and NPSs at various time points in the postoperative period. However, both these variables were only appropriately reported in two trials. Mathematically, it would be meaningless to calculate pooled values for less than three comparisons. We also attempted to compare the PONV rates; however, mathematical pooling was not possible as most of the trials reported zero incidence. We also planned to compare other complication rates (more so in the control group); however, the reporting was nonuniform and a valid pooling was not feasible. Furthermore, as a number of studies currently are few, we cannot negate the possibility of Type I error in our analysis with certainty.
Conclusions
Use of PECS block and its modifications with general anesthesia for breast surgery has significant opioid-sparing effect intraoperatively and during the first 24 h after surgery. It also has higher intraoperative opioid sparing effect when compared to PVB. During the 1st postoperative day, PVB has slightly more morphine sparing potential that may however be associated with higher complication rates. The present PECS block techniques show marked interstudy variations and need standardization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blanco R. The ‘pecs block’: A novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 2.Fujiwara A, Komasawa N, Minami T. Pectoral nerves (PECS) and intercostal nerve block for cardiac resynchronization therapy device implantation. Springerplus. 2014;3:409. doi: 10.1186/2193-1801-3-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alfaro de la Torre P, Wayne Jones J, Jr, López Álvarez S, Diéguez Garcia P, Garcia de Miguel FJ, Monzon Rubio EM, et al. Axillary local anesthetic spread after the thoracic interfacial ultrasound block – A cadaveric and radiological evaluation. Braz J Anesthesiol. [Last accessed on 2016 Jun 22]. [Doi: 10.1016/j.bjane.2015.04.007] Available from: http://www.sciencedirect.com/science/article/pii/S0104001416300616 .
- 4.Okmen K, Okmen BM, Uysal S. Serratus anterior plane (SAP) block used for thoracotomy analgesia: A case report. Korean J Pain. 2016;29:189–92. doi: 10.3344/kjp.2016.29.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: A new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18:E421–4. [PubMed] [Google Scholar]
- 7.Calì Cassi L, Biffoli F, Francesconi D, Petrella G, Buonomo O. Anesthesia and analgesia in breast surgery: The benefits of peripheral nerve block. Eur Rev Med Pharmacol Sci. 2017;21:1341–5. [PubMed] [Google Scholar]
- 8.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassn AM, Zanfaly HE, Biomy TA. Pre-emptive analgesia of ultrasound-guided pectoral nerve block II with dexmedetomidine – Bupivacaine for controlling chronic pain after modified radical mastectomy. Res Opin Anesth Intensive Care. 2016;3:6. [Google Scholar]
- 10.Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: A randomized clinical trial. Reg Anesth Pain Med. 2015;40:68–74. doi: 10.1097/AAP.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 11.Versyck B, van Geffen GJ, Van Houwe P. Prospective double blind randomized placebo-controlled clinical trial of the pectoral nerves (Pecs) block type II. J Clin Anesth. 2017;40:46–50. doi: 10.1016/j.jclinane.2017.03.054. [DOI] [PubMed] [Google Scholar]
- 12.Jabbar A, Soo C, Cheah S, Shim J, Fong K, LMH Ng. Randomized controlled trial of ultrasound-guided pectoral nerves block in unilateral breast surgery with axillary clearance-An interim report? J Health Transl Med eJournal. [Last accessed on 2017 Jun 28]. Available from: http://e-journal.um.edu.my/public/article-view.php?id=9691 .
- 13.Gupta K, Srikanth K, Girdhar KK, Chan V. Analgesic efficacy of ultrasound-guided paravertebral block versus serratus plane block for modified radical mastectomy: A randomised, controlled trial. Indian J Anaesth. 2017;61:381–86. doi: 10.4103/ija.IJA_62_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hetta DF, Rezk KM. Pectoralis-serratus interfascial plane block vs. thoracic paravertebral block for unilateral radical mastectomy with axillary evacuation. J Clin Anesth. 2016;34:91–7. doi: 10.1016/j.jclinane.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: A randomized controlled trial. Br J Anaesth. 2016;117:382–6. doi: 10.1093/bja/aew223. [DOI] [PubMed] [Google Scholar]
- 16.Wahba SS, Kamal SM. Thoracic paravertebral block versus pectoral nerve block for analgesia after breast surgery. Egypt J Anaesth. 2014;30:129–35. [Google Scholar]
- 17.El-Sheikh SM, Fouad A, Bashandy GN, AL-Azzb MA, Gamal RM. Ultrasound guided modified pectoral nerves block versus thoracic paravertebral block for perioperative analgesia in major breast surgery. Med J Cairo Univ. 2016;84:189–95. [Google Scholar]
- 18.Gurusamy KS, Gluud C, Nikolova D, Davidson BR. Assessment of risk of bias in randomized clinical trials in surgery. Br J Surg. 2009;96:342–9. doi: 10.1002/bjs.6558. [DOI] [PubMed] [Google Scholar]
- 19.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh PM, Arora S, Borle A, Varma P, Trikha A, Goudra BG, et al. Evaluation of etomidate for seizure duration in electroconvulsive therapy: A systematic review and meta-analysis. J ECT. 2015;31:213–25. doi: 10.1097/YCT.0000000000000212. [DOI] [PubMed] [Google Scholar]
- 21.Thiessen Philbrook H, Barrowman N, Garg AX. Imputing variance estimates do not alter the conclusions of a meta-analysis with continuous outcomes: A case study of changes in renal function after living kidney donation. J Clin Epidemiol. 2007;60:228–40. doi: 10.1016/j.jclinepi.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 22.Chowdhry AK, Dworkin RH, McDermott MP. Meta-analysis with missing study-level sample variance data. Stat Med. 2016;35:3021–32. doi: 10.1002/sim.6908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gordon DB, Stevenson KK, Griffie J, Muchka S, Rapp C, Ford-Roberts K, et al. Opioid equianalgesic calculations. J Palliat Med. 1999;2:209–18. doi: 10.1089/jpm.1999.2.209. [DOI] [PubMed] [Google Scholar]
- 24.Lundh A, Gøtzsche PC. Recommendations by cochrane review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. 2008;8:22. doi: 10.1186/1471-2288-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morioka H, Kamiya Y, Yoshida T, Baba H. Pectoral nerve block combined with general anesthesia for breast cancer surgery: A retrospective comparison. JA Clin Rep. 2015;1:15. doi: 10.1186/s40981-015-0018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: Population based cohort study. BMJ. 2014;348:g1251. doi: 10.1136/bmj.g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Işıl CT, Çınar AS, Oba S, Işıl RG. Comparison of spinal anaesthesia and paravertebral block in unilateral inguinal hernia repair. Turk J Anaesthesiol Reanim. 2014;42:257–63. doi: 10.5152/TJAR.2014.75508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weltz CR, Klein SM, Arbo JE, Greengrass RA. Paravertebral block anesthesia for inguinal hernia repair. World J Surg. 2003;27:425–9. doi: 10.1007/s00268-002-6661-5. [DOI] [PubMed] [Google Scholar]
- 29.Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: A novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–13. doi: 10.1111/anae.12344. [DOI] [PubMed] [Google Scholar]
- 30.Thavaneswaran P, Rudkin GE, Cooter RD, Moyes DG, Perera CL, Maddern GJ, et al. Brief reports: Paravertebral block for anesthesia: A systematic review. Anesth Analg. 2010;110:1740–4. doi: 10.1213/ANE.0b013e3181da82c8. [DOI] [PubMed] [Google Scholar]
- 31.Taylor A, Butt W, Rosenfeld J, Shann F, Ditchfield M, Lewis E, et al. A randomized trial of very early decompressive craniectomy in children with traumatic brain injury and sustained intracranial hypertension. Childs Nerv Syst. 2001;17:154–62. doi: 10.1007/s003810000410. [DOI] [PubMed] [Google Scholar]