Abstract
Cardiac tamponade caused by perforation of the cardiac wall is a rare complication related to central venous catheter (CVC) placement. A 71-year-old female with a previous history of moderate aortic stenosis and kidney transplantation was admitted to hospital due to global heart failure and worsening of allograft function. Intensified hemodialysis was commenced through a CVC placed in the right subclavian vein. Chest radiography revealed catheter tip in the right atrium and no signs of pneumothorax. Thorough diagnostics outruled immediate life-threatening conditions, such as myocardial infarction and pulmonary embolism. However, not previously seen, 2 cm thick pericardial effusion without repercussion on the blood flow was visualized during echocardiography, predominantly reclining the free surface of the right atrium, with fibrin scar tissue covering the epicardium – it was the spot of spontaneously recovered cardiac wall perforation. Follow-up echocardiogram performed before the discharge showed regression of the previously found pericardial effusion.
Keywords: Cardiac perforation, central venous catheter, complications, pericardial effusion
Introduction
Central venous catheter (CVC) placement represents a simple, relatively safe, and commonly performed invasive procedure. Previously published studies reported mechanical complications rate of 0.25%–20%, with vascular or cardiac perforation being the most serious and life-threatening.[1,2] Although cardiac tamponade caused by perforation of the cardiac wall is a rare complication related to CVC, its mortality rates remain high thus requiring immediate diagnosis and treatment.[3] Presumption was made that the incidence of lethal complications of cardiac perforation could be reduced using soft J-tipped guide wires.[4] There are reports on cardiac tamponade due to soft J-tipped guide wires but in neither of these cases pathological reason for the perforation was identified.[5]
We herein present a case report of the asymptomatic, spontaneously recovered puncture of the cardiac wall.
Case Report
A 71-year-old Caucasian female with end-stage renal disease due to p-antineutrophil cytoplasmic antibodies-positive vasculitis underwent cadaveric kidney transplantation in April 2012. It is also important to emphasize that the patient had a previous history of moderate aortic stenosis with aortic valve area 1.5 cm2 but she rejected further diagnostics and treatment.
In May 2016, she presented to the emergency department with dyspnea, anasarca, and precordial oppressions. Signs of global heart failure were present and confirmed by the diagnostic imaging techniques. No bleeding tendency was present in patient's laboratory values– they included a red blood cell count 3.34 × 1012/L, Hg 91 g/L, platelet count 196 × 109/L, prothrombin time 0.98, international normalized ratio 1.02, and activated partial thromboplastin time 29.3 s. Cardiac enzymes were negative (creatine kinase –40 U/L, lactate dehydrogenase – low-density lipoprotein [LDH] 126 U/L, troponin 9 ng/L) and worsening of allograft function (creatinine 200 μmol/L, previously 153 μmol/L) was present. Thus, a double lumen CVC was placed in the right subclavian vein and intensified hemodialysis was commenced, the total of nine sessions. During the CVC insertion, the patient was restless and disorientated. The chest radiography revealed catheter tip in the right atrium and no signs of pneumothorax. However, due to further worsening of the symptoms-patient became hypotensive, dyspnoic, tachycardic, and agitated, she was immediately transferred to the Intensive Care Unit. There was no laboratory sign of bleeding (red blood cell count 3.42 × 1012/L, Hg 97 g/L, platelet count 186 × 109/L, LDH 110 U/L). Pulmonary angiography outruled pulmonary embolism or signs of pneumonia. However, in comparison to previous scans from June 2013, it revealed pericardial effusion 2 cm thick [Figure 1]. During the next 3 days, patients were stabilized with intravenous fluids without vasopressors, echocardiography was performed and showed concentric hypertrophy of the left ventricle, with ejection fraction 70%, and without regional hypocontractility. There was also pericardial effusion 2 cm thick and without repercussions on the blood flow, predominantly reclining the free surface of right atrium, with fibrin scar tissue covering the epicardium (differential diagnosis – spot of previous cardiac wall perforation, spontaneously recovered) [Figure 2]. With careful fluid administration and antibiotic treatment, the patient became hemodynamicaly stabile with good diuresis and stabile allograft function (creatinine after the discharge 147 μmol/L) without the need for dialysis treatment. Before the discharge, echocardiography was performed once more. The pericardial effusion was now in regression; it was 5–6 mm thick and without repercussions on the blood flow [Figure 3]. CVC was hence extirpated without further complications during the last outpatient clinic visit in June 2016.
Figure 1.
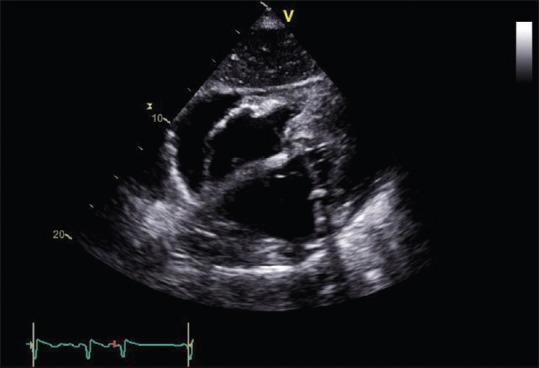
Initial echocardiographic examination – arrow points toward pericardial effusion 2 cm thick located next to the right atrium and atrioventricular groove
Figure 2.
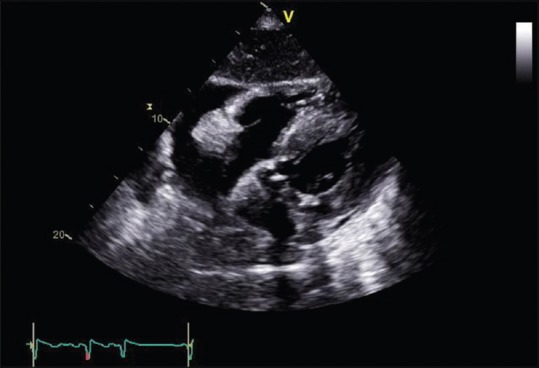
Third day echocardiographic examination – arrow points toward localized fibrin scar tissue situated on the epicardium of right atrium
Figure 3.
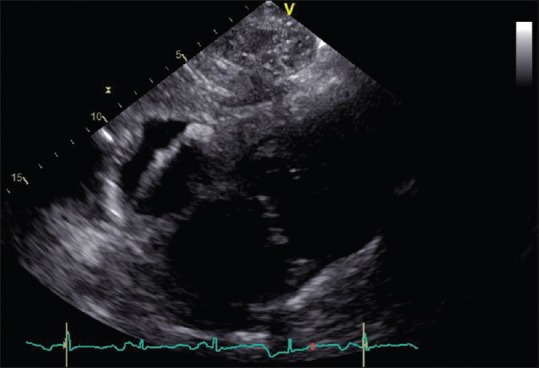
Echocardiographic examination before hospital discharge – pericardial effusion reduction
Discussion
Cardiac tamponade associated with CVCs is caused by a puncture of the cardiac wall, superior vena cava or inferior vena cava by guide wires, dilators, or catheters.[3] Isolated pericardial effusions are even more rare than tamponade, but they account for up to 0.7% of CVC-associated complications. Many of these patients had end-stage renal failure requiring hemodialysis.[6] A small perforation by a guide wire would more likely lead to hemorrhagic complications in hemodialyzed patients which have a tendency for hemorrhagic diathesis.
Malpositions and complications following CVC largely depend on the site of venous approach. There are few reports on prospective comparisons of internal jugular versus subclavian catheter insertion.[7] There were more arterial punctures, but fewer catheter malpositions with the jugular compared to subclavian approach. Based on previous experiences,[8] lack of imaging guidance during catheter insertion procedures, combined with the rapid progression to cardiac tamponade after catheter insertion, led to fatal injury.
Studies suggest that thin, flexible silastic catheters are less likely to perforate while an increased angle between the CVC tip and the cardiac/vessel wall increases the likelihood of perforation. Spontaneous closure of a small traumatic ventricular septal defect can occur, particularly if the defect is located entirely in the muscular portion of the ventricular septum[9] but to our knowledge there are no data on spontaneous atrial defect closure. An multi-slice computed tomography examination revealed not previously seen and localized pericardial effusion 1 cm thick around the puncture area of the myocard. Unfortunately, the perforation site was through atrium where the wall was much thinner. It is likely that both the thinning and the small perforation with the guide wire of dilator combined with increased bleeding due to diathesis in hemodialyzed patients led to the development of pericardial effusion.
The presented case is interesting for at least two reasons: unusual presentation without serious symptoms or fatal outcome and a spontaneous recovery within few days.
Conclusion
The events that led to the spontaneous closure of myocardial puncture and the presence of fibrin scar tissue covering the epicardium of the right atrium remain unclear. We have performed available radiologic diagnostics by which any other known causes of pericardial effusion located only around the right atrium were excluded. One of the possible explanations is that the patient was hypovolemic and dehydrated due to intensified dialysis and without the adequate hydration for which the central venous pressure was too low. This probably decreased the right atrium pressure and therefore stopped the bleeding earlier. Thankfully, a scar tissue was formed during the next few days and providing no need for invasive treatment. The most effective and reliable strategy for avoiding catheter-related serious complications seems to be CVC insertion under videofluoroscopic guidance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Robinson JF, Robinson WA, Cohn A, Garg K, Armstrong JD., 2nd Perforation of the great vessels during central venous line placement. Arch Intern Med. 1995;155:1225–8. [PubMed] [Google Scholar]
- 2.Scott WL. Central venous catheters. An overview of Food and Drug Administration activities. Surg Oncol Clin N Am. 1995;4:377–93. [PubMed] [Google Scholar]
- 3.Shamir MY, Bruce LJ. Central venous catheter-induced cardiac tamponade: A preventable complication. Anesth Analg. 2011;112:1280–2. doi: 10.1213/ANE.0b013e318214b544. [DOI] [PubMed] [Google Scholar]
- 4.Nowlen TT, Rosenthal GL, Johnson GL, Tom DJ, Vargo TA. Pericardial effusion and tamponade in infants with central catheters. Pediatrics. 2002;110(1 Pt 1):137–42. doi: 10.1542/peds.110.1.137. [DOI] [PubMed] [Google Scholar]
- 5.Blake PG, Uldall R. Cardiac perforation by a guide wire during subclavian catheter insertion. Int J Artif Organs. 1989;12:111–3. [PubMed] [Google Scholar]
- 6.Cavatorta F, Campisi S, Fiorini F. Fatal pericardial tamponade by a guide wire during jugular catheter insertion. Nephron. 1998;79:352. doi: 10.1159/000045064. [DOI] [PubMed] [Google Scholar]
- 7.Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: Internal jugular versus subclavian access – A systematic review. Crit Care Med. 2002;30:454–60. doi: 10.1097/00003246-200202000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Kalen V, Medige TA, Rinsky LA. Pericardial tamponade secondary to perforation by central venous catheters in orthopaedic patients. J Bone Joint Surg Am. 1991;73:1503–6. [PubMed] [Google Scholar]
- 9.Midell AI, Replogle R, Bermudez G. Spontaneous closure of a traumatic ventricular septal defect following a penetrating injury. Ann Thorac Surg. 1975;20:339–42. doi: 10.1016/s0003-4975(10)64227-0. [DOI] [PubMed] [Google Scholar]


