Sir,
A 23-year-old female was admitted to the surgery ward with the chief complaint of swelling over the left side of the back, with pus discharge for the last 16 days. Pain and swelling were accompanied by fever and chills. She underwent cesarean section delivery 20 days back at a local nursing home where spinal anesthesia was administered. She developed pain and redness over injection site on the 4th postoperative day. She consulted operating surgeon, and she was advised to consult a general surgeon. She came on the 20th postoperative day. On examination, she was found drowsy, dehydrated, and febrile (temperature 40.5°C). She had tachycardia and hypotension. Blood chemistry revealed hemoglobin of 8 g/dl, total white blood cell count of 26,000/cumm with and 15% band cells, serum creatinine of 2.0, and serum glutamic-pyruvic transaminase of 100 IU/L. Arterial blood gas analysis revealed mild metabolic acidosis. Intravenous antibiotics and vasopressors were started. After resuscitation for 2 h, she was shifted to operation room where debridement of devitalized tissue [Figure 1] was performed under total intravenous anesthesia. The condition of the patient became stable after 24 h and inotropes were tapered and stopped after 48 h. Daily debridement was carried out. Culture and biopsy reports came on the 4th day, which indicated infection with Escherichia coli, Bacteroides, and Mucormycetes. At the end of the tenth debridement, the wound was healthy with the clear margin and granulating base [Figure 2]. The patient underwent split-thickness grafting. The postoperative course was unremarkable.
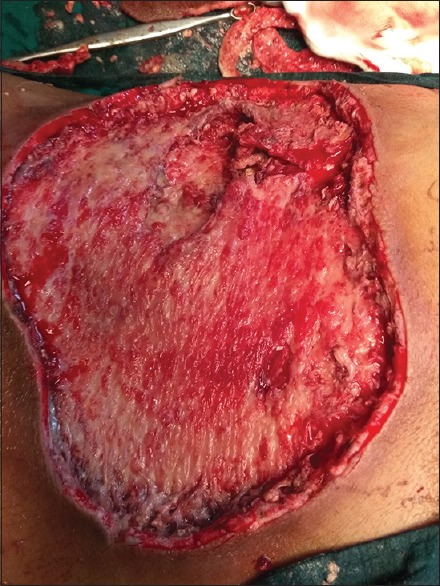
Figure 1.

Necrotizing fasciitis at the time of the first debridement: Necrotic material with exposed muscle and surrounding redness of the skin
Figure 2.
At the end of the tenth debridement: Clean base and surrounding clear margin
Necrotizing fasciitis is a spreading, severe inflammation or polymicrobial infection of the skin, subcutaneous tissue, adjacent fascia, and muscle sheath leading to necrosis. The affected area is erythematous, swollen, and painful, which progresses rapidly to blister and frank skin gangrene. Pain out of proportion to the physical signs and tachycardia are very much suggestive of necrotizing fasciitis. Foul-smelling discharge, sometimes described as dishwater necrosis, and loss of natural resistance of fascia to the finger are present (positive finger test).[1,2] The principles of management are fluid resuscitation and correction of electrolyte and acid-base imbalance, early initiation of antibiotics, surgical debridement of the affected area, and supportive measures for organ dysfunction.[3] Infectious complications associated with spinal anesthesia include abscess, meningitis, necrotizing fasciitis, arachnoiditis, paralysis, and death.[4] Potential routes for infectious complication in spinal anesthesia might be contaminated syringes, catheter hubs, local anesthetics, or breaches in aseptic technique.[4] Possible sources of infection suspected in this case include local anesthetic solution, nonadherence to strict aseptic precautions, skin flora of the patient, reuse of multidose vial, endogenous origin, and nasopharyngeal flora of anesthesiologist.
Important precautions to be taken in the operation theater include removal of watches and jewelry, handwashing with an antiseptic solution, use of surgical mask, cap and sterile gown, and gloves, skin disinfection with alcohol or chlorhexidine, and sterile draping.[4]
Only two cases have been reported in the literature with the bacterial infection, and this is the first instance where superadded mucormycosis infection was present.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I would like to acknowledge the help provided by Dr. B. C. Sharma for his assistance.
References
- 1.Andreasen TJ, Green SD, Childers BJ. Massive infectious soft-tissue injury: Diagnosis and management of necrotizing fasciitis and purpura fulminans. Plast Reconstr Surg. 2001;107:1025–35. doi: 10.1097/00006534-200104010-00019. [DOI] [PubMed] [Google Scholar]
- 2.Childers BJ, Potyondy LD, Nachreiner R, Rogers FR, Childers ER, Oberg KC, et al. Necrotizing fasciitis: A fourteen-year retrospective study of 163 consecutive patients. Am Surg. 2002;68:109–16. [PubMed] [Google Scholar]
- 3.Ustin JS, Malangoni MA. Necrotizing soft-tissue infections. Crit Care Med. 2011;39:2156–62. doi: 10.1097/CCM.0b013e31821cb246. [DOI] [PubMed] [Google Scholar]
- 4.Jankovi VN. Infectious complications of regional anaesthesia and analgesia. Period Biol. 2011;113:247–50. [Google Scholar]


