Abstract
Purpose:
Several devices are available to take care of difficult airway, but C-MAC D-Blade has scant evidence of its use in nasotracheal intubation in a difficult airway scenario.
Aims and Objectives:
We compared the C-MAC D-Blade videolaryngoscope™, and the standard Macintosh laryngoscope for nasal intubation in patients with difficult airways selected by El-Ganzouri risk index using parameters of time and attempts required for intubation, glottic view in terms of Cormack–Lehane grade, ease of intubation, success rate, use of accessory maneuvers, incidence of complications, and hemodynamic changes.
Methods:
One hundred American Society of Anesthesiologists (ASA) I–III patients aged 20–70 years with EGRI score 1–≤7 scheduled for head and neck surgery requiring nasal intubation. ASA IV patients, patients with mouth opening <2.5 cm, patients difficult to mask ventilate, and patients with hyperkalemia and history of malignant hyperthermia were excluded from the study. Primary outcome was time taken to intubation, and secondary outcomes were a number of attempts, glottic view in terms of C/L grade, use of accessory maneuvers, success rate, incidence of trauma, ease of intubation, and hemodynamic changes before and after intubation.
Results:
Time required for intubation was less (39.56 ± 15.65 s) in Group C than in Group M (50.34 ± 15.65 s). Cormack–Lehane Grade I and II view were more in C-MAC D-Blade group (P < 0.05). Success rate and ease of intubation were found to be more in C-MAC D-Blade group than in Macintosh group (P < 0.05). A number of attempts and incidence of complications such as trauma, bleeding, and failed intubation were greater in Macintosh group than in C-MAC D-Blade group. Hemodynamic changes were observed to be comparable in both the groups.
Conclusion:
C-MAC D-Blade videolaryngoscope™ is a better tool in anesthetic management of difficult airway for nasal intubation compared to conventional Macintosh laryngoscope.
Keywords: C-Mac D-Blade, Cormack–Lehane, El-Ganzouri risk index, time to intubation
Introduction
Head and neck carcinoma constitutes a major group of patients presenting for surgery. These patients often present with a difficult airway, especially patients having carcinoma of alveobuccal complex. Difficult and failed laryngoscopy and tracheal intubation cause increased morbidity and mortality among these patients.[1] The Macintosh laryngoscope necessitates alignment of the oropharyngeal–laryngeal axis to visualize the glottic opening and intubate the trachea; success relies on careful head positioning and consistent anatomy. When these conditions are not met, as seen in poor head extension, poor tissue mobility, limited mouth opening, enlarged tongue, or morbid obesity, the failure rate of intubation with conventional direct laryngoscopy increases.[2]
In recent years, videolaryngoscopes have played an increasingly important role in airway management in unanticipated difficult or failed endotracheal intubation. Videolaryngoscopy produces a view of the laryngeal inlet independent of the line of sight. C-Mac D-Blade is one such videolaryngoscope with pronounced elliptical curvature with the distal end facing distinctly upward.[3] C-Mac D-Blade has been used successfully for orotracheal intubation in various anticipated difficult airway scenarios such as morbid obesity, cervical spine immobilization, intensive care unit, and limited mouth opening.[4,5,6,7] Although other videolaryngoscopes such as Glidescope[8] and Airtraq[9] have been used for nasotracheal intubation, literature provides scant evidence for validating the use of C-Mac D-Blade for nasotracheal intubation.[10,11] Our aim was to compare the C-Mac D-Blade videolaryngoscope™ with the conventional Macintosh laryngoscope for nasal intubation in patients with difficult airway. The primary outcome of our study was the time taken to intubate, whereas the secondary outcomes of our study included comparison of glottic view, number of attempts, use of accessory maneuvers, success rate, ease of intubation, hemodynamic changes, and incidence of trauma during laryngoscopy and intubation. To the best of our knowledge, our study comparing C-Mac D-Blade videolaryngoscope™ with the conventional Macintosh laryngoscope for nasal intubation in adults with difficult airway was first of its kind.
Methods
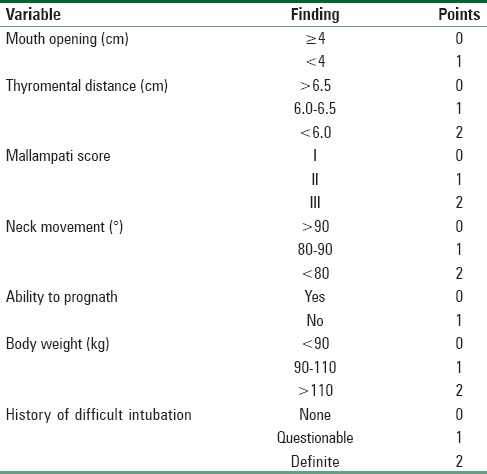
This trial is registered under CTRI with registration no CTRI/2017/03/008103. After obtaining approval (328/AN/DNB-38) from the Institutional Ethics Committee of Rajiv Gandhi Cancer Hospital and Research Centre, New Delhi (Chairperson Dr. TK Thusoo) on December 28, 2013, patients were enrolled in the study. Written and informed consent was taken from all the patients. One hundred American Society of Anesthesiologists (ASA) class I–III patients aged 20–70 years, scheduled for head and neck cancer surgeries requiring nasal intubation with El-Ganzouri risk index (EGRI) 1–≤7 were included in our study. Difficult airway is graded by EGRI for difficult airway prediction based on seven parameters (body weight [kg], modified Mallampati class, mouth opening [cm], thyromental distance [cm], neck movement [°], prognathism, and history of difficult airway) with a score ranging from 0 to 12 has been used in our study [Table 1]. ASA IV patients, patients with mouth opening <2.5 cm, patients difficult to mask ventilate, and patients with hyperkalemia and history of malignant hyperthermia were excluded from the study.
Table 1.
El-Ganzouri risk index
Patients were randomized to Group M (n = 50) and Group C (n = 50) by a randomized computer-generated table and the group allocation, and laryngoscope to be used was revealed just before laryngoscopy took place. The patient and the intubating anesthetists were blinded to the group allocation. All the intubations were performed by experienced operators who were arbitrarily defined as anesthetists who have performed at least twenty successful nasal or oral intubations with C-Mac D-Blade. A standard Portex 7 mm ID cuffed sterile endotracheal tube has been used in each intubation after prewarming and proper lubrication. Same size tube has been used in all cases to eliminate bias in hemodynamic parameters.
All patients posted for surgery undergo a thorough preanesthetic evaluation including detailed airway assessment, clinical history, and general and systemic examination. Relevant investigations pertaining to the case and coagulation profile were done. All patients were premedicated with tablet alprazolam 0.5 mg night before surgery and tablet ranitidine 150 mg and granisetron 2 mg orally 1 h before surgery.
In the operation theater, a peripheral intravenous access was secured, and standard monitoring applied. Xylometazoline 0.05% nasal drops were administered in bilateral nostrils. The patient's head was supported on a firm pillow of 7–8 cm height. After 3 min of preoxygenation, general anesthesia was induced with midazolam, injection fentanyl 2 μg/kg body weight, and propofol 1–1.5 mg/kg in titrated doses until loss of verbal contact. Neuromuscular blockade was achieved with injection succinylcholine 2 mg/kg body weight.
After disappearance of single twitch response to electrical stimulus of 40 mA at 1 Hz, Portex cuffed 7 mm ID endotracheal tube thermosoftened in warm normal saline was advanced through the right nostril till oropharynx. Either Macintosh or C-MAC D-Blade videolaryngoscope™ was used to perform the nasotracheal intubation as directed by randomization for each patient. The operator is blinded till the introduction of laryngoscope. Both the laryngoscopes were made available in the theater. Standard technique of introduction of Macintosh laryngoscope was used. Cormack–Lehane grade is assessed and conveyed by the intubating anesthetist, and endotracheal tube was advanced into the glottic inlet. If any difficulty is encountered, accessory maneuvers were used in the following order - first external laryngeal manipulation, then rotation of tube, followed by partial inflation of cuff, and finally use of Magill/Boedeker forceps. If intubation is still unsuccessful, then intubation attempt was repeated after adequate mask ventilation. Withdrawal of the laryngoscope from the mouth at any time is counted as one attempt. A maximum of three attempts were allowed. If intubation was still unsuccessful, intubation declared as failed and recorded. Then, C-Mac D-Blade was used by the same anesthetist as per study protocol in that case. If still intubation was not possible, fiber-optic bronchoscopic-guided intubation done or patient returned to spontaneous ventilation as judged appropriate as per institutional protocol.
C-Mac D-Blade was introduced from center of oral cavity over the tongue while directly looking inside the mouth. After that while looking at the liquid-crystal display screen, blade tip was introduced further so as to achieve the best glottic view by adjusting tip of blade in vallecula. The endotracheal tube was then advanced into the glottic inlet. If difficulty is encountered, same maneuvers were used 0 as for Macintosh blade one after the other in the same sequence or in combinations judged appropriate by the intubating anesthetist and recorded. Time taken to intubation (TTI) was recorded from the time of introduction of laryngoscope into mouth to appearance of three consecutive capnographs in the monitor using the timer incorporated in Primus Draeger Anesthesia Workstation. Heart rate and blood pressure were measured and recorded before induction and after 1 and 3 min of laryngoscopy and intubation. All the recordings were made by an independent observer, and at no point of time, the intubating anesthetist was allowed to know the timings. Saturation below 90% at any moment was considered as failure to intubate with that device, and institutional protocol for difficult airway management was followed. Complications due to nasal intubation were noted. The presence of blood in pharynx or on the laryngoscope blade was defined as intubation trauma. After intubation, the intubating anesthetist was asked to label the ease of intubation as easy or difficult and recorded. Passing of endotracheal tube through glottic inlet is shown in the Led monitor in Figure 1.
Figure 1.

Passing of endotracheal tube through the glottic inlet in the light emitting diode monitor
Statistical analysis
Our estimated sample size was based on time taken for nasal intubation (TTI). A sample size of thirty per group was calculated based on a mean difference of 10 s in TTI between Macintosh laryngoscope and C-Mac D-Blade videolaryngoscope, with a population variance of 10 s,[2] a two-sided alpha of 0.05, and a power of 90%. We have included fifty patients per group in our study.
Statistical testing was conducted with the Statistical Package for the Social Sciences system version SPSS17.0 (Chicago SPSS Inc). Continuous variables were expressed as frequencies and percentages. The comparison of normally distributed continuous variables between the groups was performed using Student's t-test. Nominal categorical data between the groups were compared using Chi-square test or Fisher's exact test as appropriate. Nonnormal distribution continuous variables were compared using Mann–Whitney U-test. For all statistical tests, P < 0.05 was considered statistically significant difference. This study adheres to the applicable equator guidelines.
Results
The first patient was recruited in Jan 2014 and the trial ended in December 2014 and the flow of participants during the study is depicted by the CONSORT flow diagram [Figure 2]. There were no dropouts from the study. Both groups were comparable with respect to age, ASA grades, gender, height, and EGRI scores [Table 2]. The mean time taken to intubate with Macintosh laryngoscope was 50.34 ± 26.76 s whereas with C-MAC D-Blade time taken was 39.56 ± 15.65 s in Group C (P < 0.05) and is statistically significant [Figure 3].
Figure 2.
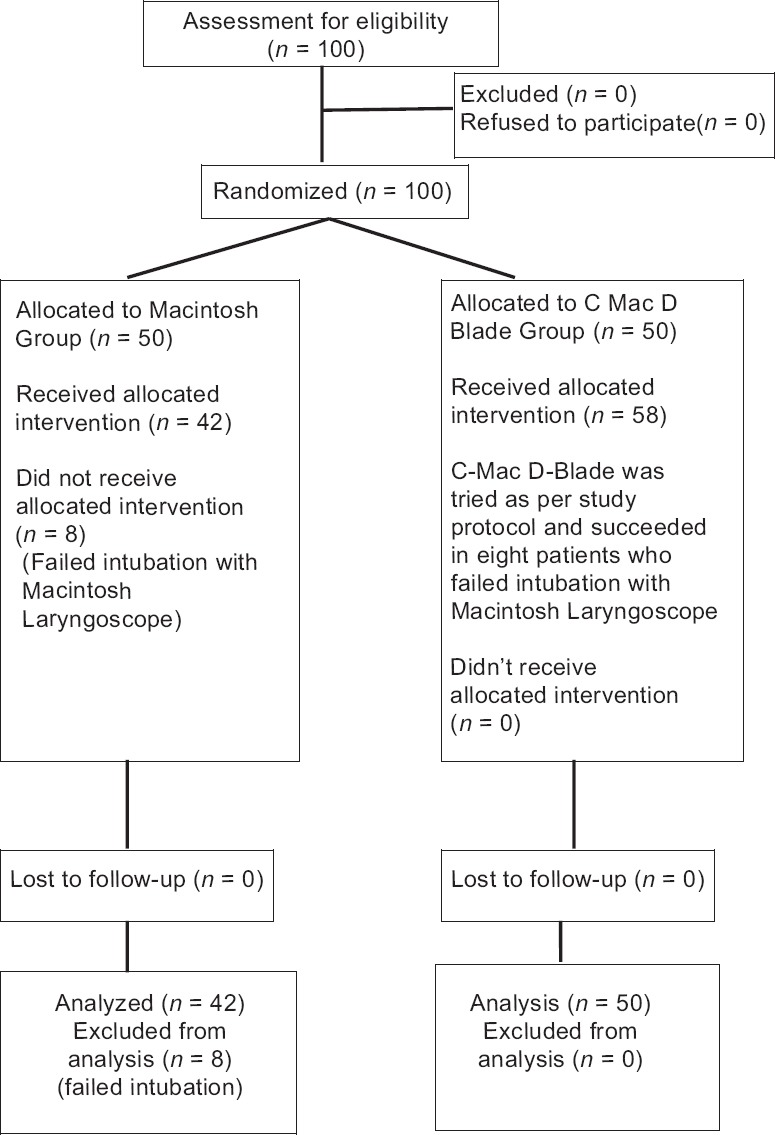
The CONSORT diagram showing the flow of participants through each stage of the trial
Table 2.
Baseline characteristics of the patient undergoing intubation using Macintosh and C Mac D Blade
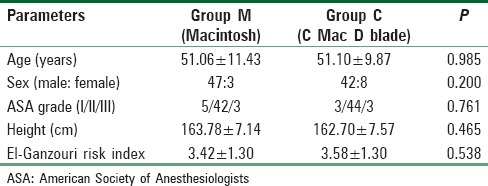
Figure 3.
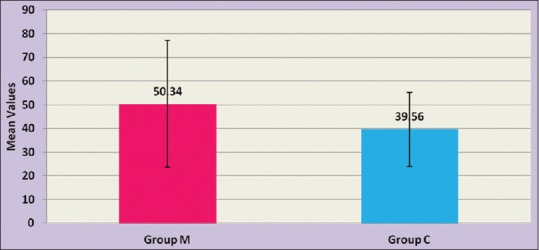
Graphic comparison of time taken to intubation between Group M and Group C
The percentage of Cormack–Lehane Grade 1 was much higher in the C-Mac D-Blade group as compared to Macintosh group [Table 3]. Eighty-six percent (43/50) patients had CL Grade 1 versus 30% (15/50, P < 0.001), 6% (3/50) patients had CL Grade IIa versus 16% (11/50, P = 0.041), 4% (2/50) had CL Grade IIb versus 16% (12/50, P = 0.008), 4% (2/50) had Grade III versus 22% (11/50, P = 0.015), and none versus 1 patient had CL Grade IV in C-Mac D-Blade and Macintosh group, respectively [Table 3].
Table 3.
Device performance in patients undergoing intubation with Macintosh and C Mac D Blade
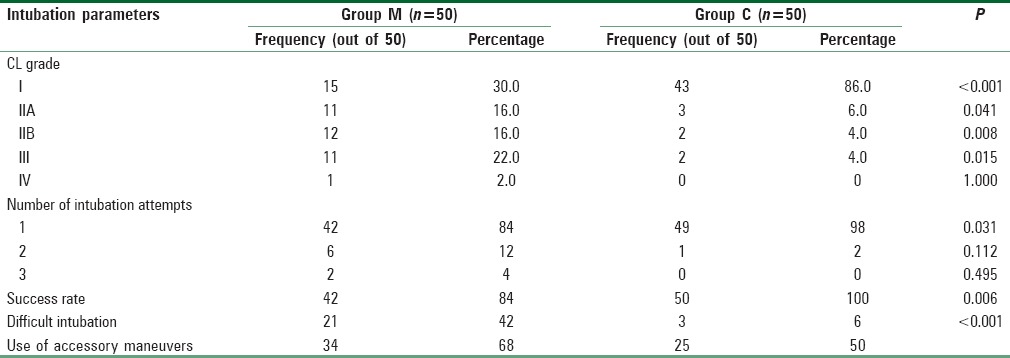
In Group C, 98% (49/50) patients were intubated in first attempt and one patient required second attempt due to inadequate exposure, and in Group M, 86%(42/50, P = 0.031) were intubated in first attempt, 12% (6/50) required second attempt, and 4% (2/50) patients require third attempt.
The success rate was 100% (50/50) with C-Mac D-Blade versus 84% (42/50) with Macintosh laryngoscope. Eight patients could not be intubated in Macintosh group in second or third attempt after using all accessory maneuvers [Table 3].
The use of accessory maneuvers was less in D-Blade group compared to Macintosh group. Nearly 52% (26/50) of patients were intubated directly without difficulty and 34% (17/50) required external laryngeal manipulation. In Macintosh group, 30% (15/50, P < 0.05) of patients were intubated directly without difficulty and 68% (34/50, P = 0.001) required external laryngeal manipulation. Both the groups were comparable in terms of using other accessory maneuvers such as tube rotation, partial inflation of cuff, and use of forceps to guide the tube [Table 3].
The intubating anesthetists considered 47/50 (94%) intubations as easy in D-Blade group versus 29/50 (58%) in the Macintosh group (P < 0.001).
Both the groups were comparable in terms of hemodynamic changes with respect to heart rate, systolic, diastolic, and mean blood pressure taken before induction and after 1 and 3 min of laryngoscopy and intubation [Figures 4 and 5].
Figure 4.
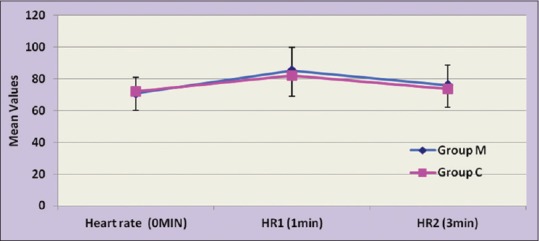
Graphic comparison of mean heart rate between Group M and Group C
Figure 5.
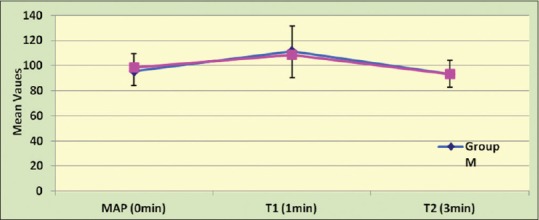
Graphic comparison of mean arterial pressure between Group M and Group C
In Group M, three patients had trauma in terms of blood on the laryngoscope blade or blood in the pharynx. There was no occurrence of trauma in D Blade group; however, results were comparable in both the groups.
Discussion
Management of airway is always a challenge for anesthetists mostly accomplished by conventional direct laryngoscope. However, direct laryngoscopy has inherent limitations because it requires a direct line of sight between the operator's eyes and the laryngeal inlet.[12] Videolaryngoscopes were designed to overcome the limitations associated with direct laryngoscopes and have shown great success in all scenarios of routine, emergency, and difficult airways. There are many studies comparing C-MAC videolaryngoscope with other airway devices in oral intubation, but little work has been done to compare the performance of videolaryngoscopes in nasal intubation in difficult airways.
Preoperative assessment of airway is utmost necessary to predict difficult airway. We have used EGRI in our study. el-Ganzouri et al. came up with this index test in 1996 and included seven parameters with a maximum score of 12, indicating more difficult airway in higher scores.[13] EGRI is comparable to other predictive risk indexes such as Wilson et al., Pottecher et al., and J Arne et al. simplified scores. Cortellazzi et al. used this risk index with Glidescope videolaryngoscope and found increased sensitivity, specificity, and low positive and low negative predictive values than with Macintosh laryngoscope.[14] We have included patients with EGRI score 1–7 in our study. Scores more than 7 were not included as they are more suitable for awake fiber-optic intubation as shown by Caldiroli and Cortellazzi in their study.[15] The incidence of patients in general population with high EGRI scores is also very less.
The TTI was 50 s (interquartile range: 34–77 s) in Group M, and in Group C, it was 39 s (interquartile range: 24–54 s, P = 0.016). The time taken after intubation to appearance of three consecutive capnographs, would be, on average, similar between the groups. The lesser TTI with D-Blade is due to several advantages of D-Blade over Macintosh laryngoscope. C-Mac D-Blade produces better glottic exposure with more Cormack–Lehane Grade I and II views than Macintosh laryngoscope. Patients could be intubated in a single attempt. Patients that could be intubated directly without difficulty or using only external laryngeal manipulation are more with D-Blade. Use of accessory maneuvers such as tube rotation, partial inflation of cuff, and use of forceps were less with D-Blade than Macintosh laryngoscope. Furthermore, laryngoscopy with D Blade does not require alignment of the pharyngeal, laryngeal, and oral axes for intubation which saves time and hence less TTI. Our results are supported by Jones et al.[16] and Shimada et al.[17] but differs from Ahmed[18] who found nasotracheal intubation with direct laryngoscope faster (45.1 ± 7.8 s) than with Glidescope (53.5 ± 14.7 s). This may be because of inadequate experience in handling videolaryngoscope which requires complex hand–eye coordination as they have mentioned in their study.
In our study, seven patients with CL Grade III and one patient with CL grade IV could not be intubated with Macintosh laryngoscope after repeated attempts and using all accessory maneuvers. As per study protocol when C-Mac D-Blade was used for intubation in these patients, all were successfully intubated; however, one patient required second attempt. This shows that C-Mac D-Blade improves glottic views in terms of Cormack–Lehane grading. This is supported by other studies done by Lili et al.,[19] Cavus et al.,[20] Kiliçaslan et al.,[21] and Serocki et al.[22]
Three out of eight patients that could not be intubated had EGRI 6, one patient had EGRI 5, two patients had EGRI 4, one patient had EGRI 3, and one had EGRI 2. This showed that patients with high EGRI scores are difficult to intubate with Macintosh blade. The patient with low EGRI scores that could not be intubated with direct laryngoscopy had restricted mouth opening as a major limitation along with other difficulty variables resulting in inadequate exposure.
In Group C out of fifty patients, 16 patients had EGRI 4, 4 patients had EGRI 5, four patients had EGRI 6, and one patient had EGRI 7. All these patients with high EGRI scores (EGRI 4-7) had multiple difficult airway parameters but were successfully intubated with C-MAC D-Blade in a single attempt except one patient requiring double attempt along with accessory maneuvers. If D-Blade had not been available, these patients would have required awake fiber-optic intubation.
The number of attempts required was significantly less with D-Blade as compared to Macintosh laryngoscope (P < 0.05). Only two out of eight patients that had multiple attempts could be intubated with Macintosh laryngoscope and six patients could not be intubated even after multiple attempts. However, when D-Blade was used in these patients, they were successfully intubated. The results were supported by studies done by Cavus et al.[20] and Abdullah et al.,[23] in which they found improved C/L views with C-Mac than with conventional direct laryngoscope. The use of forceps to guide the tube into the larynx may be more in our study as compared to study conducted by Jones et al.[16] This difference can be because we have included patients with difficult airway whereas their study was done with a preformed nasal tube in patients with normal airway. However, both the groups were comparable with regard to the use of forceps to guide the tube in our study.
There was the incidence of trauma in three cases in Group M (16%) and no trauma occurred in Group C during intubation. One patient had dental trauma during lifting of epiglottis and two patients had bleeding from ulcer site during laryngoscopy, suction catheter was used to clear the airway.
The difference in heart rate, systolic, diastolic, and mean blood pressure before and after intubation was comparable in both the groups. This may be because the magnitude of sympathetic stimulation was similar in both the groups and adequately blunted with drugs.
In our study, the operators knew that they were participating in a trial, had to handle a difficult airway, and that the intubation time was being recorded. This may lead to better clinical performance; however, it will be equally distributed between the two groups. The patients and the operator were blinded to the type of laryngoscope used (till introduction of laryngoscope). The observer assessing the outcomes of the trial was fully blinded until all data had been collected.
The intubations in our study were done by several experienced anesthetists. Hence, there may be possibility of bias in experience, time to intubation, number of attempts, and occurrence of bleeding.
Conclusion
When compared with DL, C-Mac D-Blade emerged as a better tool in managing difficult airway by nasal route in terms of time taken to intubation, success rate, number of attempts, ease of intubation, use of accessory maneuvers, and trauma. Furthermore, patients with high EGRI scores such as 5–7 could be easily managed with C-Mac D-Blade who would have otherwise required awake fiber-optic intubation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hall CE, Shutt LE. Nasotracheal intubation for head and neck surgery. Anaesthesia. 2003;58:249–56. doi: 10.1046/j.1365-2044.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 2.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 3.Missaghi SM, Krasser K, Zadrobilek E. The D-BLADE: A significantly modified blade for the storz C-MAC videolaryngoscopy system. Internet J Airway Manag. 2010-2011. [Last accessed on 2015 Jan 02]. p. 6. Available from: http://www.adair.at/ijam/volume06/newequipment07/default.htm .
- 4.Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–61. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 5.Cattano D, Corso RM, Altamirano AV, Patel CB, Meese MM, Seitan C, et al. Clinical evaluation of the C-MAC D-Blade videolaryngoscope in severely obese patients: A pilot study. Br J Anaesth. 2012;109:647–8. doi: 10.1093/bja/aes333. [DOI] [PubMed] [Google Scholar]
- 6.Koh JC, Lee JS, Lee YW, Chang CH. Comparison of the laryngeal view during intubation using Airtraq and Macintosh laryngoscopes in patients with cervical spine immobilization and mouth opening limitation. Korean J Anesthesiol. 2010;59:314–8. doi: 10.4097/kjae.2010.59.5.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noppens RR, Geimer S, Eisel N, David M, Piepho T. Endotracheal intubation using the C-MAC® video laryngoscope or the Macintosh laryngoscope: A prospective, comparative study in the ICU. Crit Care. 2012;16:R103. doi: 10.1186/cc11384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirabayashi Y, Hakozaki T, Fujisawa K, Hiruta M, Niwa Y, Sata N, et al. Nasal endotracheal intubation using GlideScope. Masui. 2007;56:962–4. [PubMed] [Google Scholar]
- 9.St. Mont G, Biesler I, Pförtner R, Mohr C, Groeben H. Easy and difficult nasal intubation – a randomised comparison of Macintosh vs. Airtraq® laryngoscopes. Anaesthesia. 2012;67:132–8. doi: 10.1111/j.1365-2044.2011.06943.x. [DOI] [PubMed] [Google Scholar]
- 10.Cavus E, Neumann T, Doerges V, Moeller T, Scharf E, Wagner K, et al. First clinical evaluation of the C-MAC D-Blade videolaryngoscope during routine and difficult intubation. Anesth Analg. 2011;112:382–5. doi: 10.1213/ANE.0b013e31820553fb. [DOI] [PubMed] [Google Scholar]
- 11.Al-Jadidi AM, Khan RM, Nair SV, Kaul N. Facilitated nasotracheal intubation in patient with restricted mouth opening aided by D-blade of C-Mac videolaryngoscope and Schroeder's directional stylet. Indian J Anaesth. 2012;56:422–3. doi: 10.4103/0019-5049.100840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levitan RM, Heitz JW, Sweeney M, Cooper RM. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–7. doi: 10.1016/j.annemergmed.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 13.el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–204. doi: 10.1097/00000539-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Cortellazzi P, Minati L, Falcone C, Lamperti M, Caldiroli D. Predictive value of the El-Ganzouri multivariate risk index for difficult tracheal intubation: A comparison of GlideScope videolaryngoscopy and conventional Macintosh laryngoscopy. Br J Anaesth. 2007;99:906–11. doi: 10.1093/bja/aem297. [DOI] [PubMed] [Google Scholar]
- 15.Caldiroli D, Cortellazzi P. A new difficult airway management algorithm based upon the El Ganzouri risk index and GlideScope® videolaryngoscope: A new look for intubation? Minerva Anestesiol. 2011;77:1011–7. [PubMed] [Google Scholar]
- 16.Jones PM, Armstrong KP, Armstrong PM, Cherry RA, Harle CC, Hoogstra J, et al. A comparison of GlideScope videolaryngoscopy to direct laryngoscopy for nasotracheal intubation. Anesth Analg. 2008;107:144–8. doi: 10.1213/ane.0b013e31816d15c9. [DOI] [PubMed] [Google Scholar]
- 17.Shimada M, Hirabayashi Y, Seo N. Nasotracheal intubation using GlideScope videolaryngoscope or Macintosh laryngoscope by novice laryngoscopists. Masui. 2010;59:1318–20. [PubMed] [Google Scholar]
- 18.Ahmed WG. GlideScope versus direct laryngoscope for nasotracheal intubation in oral and maxillofacial surgery patients with anticipated difficult airways. Ain Shams J Anesthesiol. 2012;5:201–6. [Google Scholar]
- 19.Lili X, Zhiyong H, Jianjun S. A comparison of the GlideScope with the Macintosh laryngoscope for nasotracheal intubation in patients with ankylosing spondylitis. J Neurosurg Anesthesiol. 2014;26:27–31. doi: 10.1097/ANA.0b013e31829a0491. [DOI] [PubMed] [Google Scholar]
- 20.Cavus E, Thee C, Moeller T, Kieckhaefer J, Doerges V, Wagner K. A randomised, controlled crossover comparison of the C-MAC videolaryngoscope with direct laryngoscopy in 150 patients during routine induction of anaesthesia. BMC Anesthesiol. 2011;11:6. doi: 10.1186/1471-2253-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiliçaslan A, Topal A, Erol A, Uzun ST. Comparison of the C-MAC D-Blade, conventional C-MAC, and Macintosh laryngoscopes in simulated easy and difficult airways. Turk J Anaesthesiol Reanim. 2014;42:182–9. doi: 10.5152/TJAR.2014.59672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Serocki G, Neumann T, Scharf E, Dörges V, Cavus E. Indirect videolaryngoscopy with C-MAC D-Blade and GlideScope: A randomized, controlled comparison in patients with suspected difficult airways. Minerva Anestesiol. 2013;79:121–9. [PubMed] [Google Scholar]
- 23.Abdullah MK, Waleed AA, Hazeem MF, Aziz AM. Use of Airtraq, C-Mac and GlideScope laryngoscope is better than Macintosh in novice medical students’ hands: A manikin study. Saudi J Anaesth. 2011;5:376–81. doi: 10.4103/1658-354X.87266. [DOI] [PMC free article] [PubMed] [Google Scholar]


