Introduction
Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease that can involve oral mucosal membranes in up to 45% of patients.1 Oral presentation is commonly described as erythema involving multiple oral sites. Oral ulceration is relatively rare and occasionally resembles an erosive type of oral lichen planus (OLP).1, 2, 3, 4 Although there is some degree of histologic overlap between OLP and oral manifestations of SLE, a conclusive diagnosis can be made on direct immunofluorescence (DIF) assay results.5
Here, we present a case of a 42-year-old woman with SLE and bilateral buccal mucosal lesions that were clinically and histologically consistent with reticular OLP. These diagnoses were verified through DIF studies. To the best of our knowledge, synchronous presentation of SLE and reticular OLP has not been reported before.
Case report
A 42-year-old woman was seen at the oral medicine clinics of Riphah International University with a complaint of rough, white patches on her buccal mucosa present for ≥2 months. The patient's recent medical history included persistent low-grade fever for 9 months, malaise, and lethargy. She reported swelling around her knees, difficulty in fist closure, tingling in her fingers, and pain on movement of both small and large joints. She also experienced itching of facial skin, especially in the malar and forehead regions. The itching was exacerbated by exposure to sunlight. She had no evidence of cutaneous or nail lichen planus. Her only medication was an antidepressant that was discontinued by her rheumatologist. Doctors conducted multiple investigations for infectious diseases, all of which were negative. She was prescribed numerous courses of antibiotics, but there was no improvement in her symptoms. The last doctor that she saw recommended testing for antinuclear antibody titers, which were elevated (3.1 U/mL). Her medical history was unremarkable other than a minor myomectomy procedure performed several years prior.
Intraoral examination showed bilateral, white, lace-like (lichenoid) striations on the buccal mucosa (Fig 1). Pigmentation was also noted on the gingiva and buccal mucosa. On the basis of the patient's recent medical history, the increased antinuclear antibody values, and the presence of oral lichenoid lesions, SLE was the top contender in the differential diagnosis. An incisional biopsy of the buccal mucosal lesion was done with submission of tissue for both histopathology and DIF assay. The patient was also sent for double-stranded DNA (dsDNA) testing.
Fig 1.
White, lace-like striations consistent with a reticular-type oral lichen planus on the buccal mucosa.
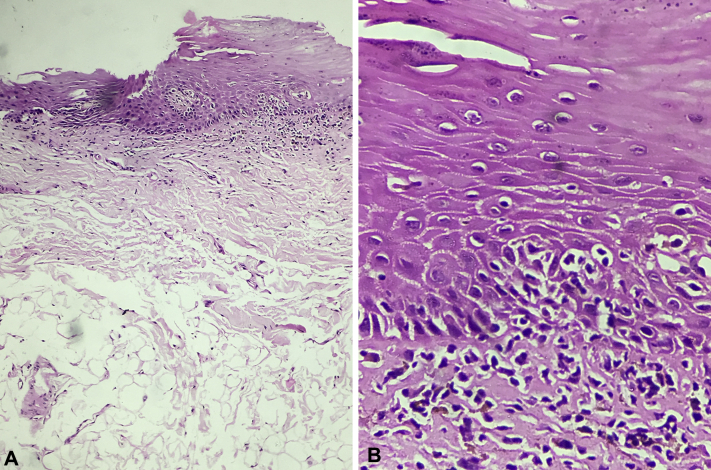
Sections from the buccal mucosal biopsy showed infiltration of chronic inflammatory cells through the basement membrane of the oral epithelium. A mild, band-like, lymphocytic infiltrate was also noted in the superficial connective tissue (Fig 2, A and B). DIF assay was negative for deposition of IgG, IgM, IgA, or C3 at the basement membrane zone. These results favored a diagnosis of reticular OLP and not SLE. However, the dsDNA test confirmed the coexistence of SLE (dsDNA antibody titer, 30 U/mL).
Fig 2.
A and B, Photomicrographs showing inflammatory cell infiltration of the basement membrane.
The patient was reassured about her oral presentation and referred to a rheumatologist for her SLE diagnosis. The rheumatologist started her on 400 mg of hydroxychloroquine and 60 mg of prednisone during the first month. Following improvement of her symptoms, the corticosteroid dose was gradually tapered down.
On 18-month follow-up, the patient's OLP was unaffected in appearance, and her SLE symptoms were under control by a maintenance dose of 200 mg of hydroxychloroquine and 5 mg of prednisone.
Discussion
Our case represents synchronous presentation of 2 distinct autoimmune entities. The dsDNA test was sufficient to confirm the diagnosis of SLE in our patient. However, the bilateral, lichenoid lesions on the buccal mucosa were clinically and histologically characteristic of OLP.6 Although fibrinogen results were not available from our lab, absence of IgG, IgM, and C3 deposits at the basement membrane zone during immunologic testing also supports this assertion.5
It is not uncommon to have >1 autoimmune disease in a single patient. Several reports are available in the literature on lupus erythematosus and lichen planus overlap syndrome, a disease in which the features of discoid lupus erythematosus and cutaneous lichen planus (CLP) are combined.7, 8, 9 A variant of the overlap syndrome, consisting of CLP and subacute cutaneous lupus erythematosus, has also been described.10 The common etiology of the 2 diseases is frequently cited as the reason for this coexistence.9, 10
Although our case appears similar to the overlap syndrome, the immunologic profiles of the SLE and OLP vary significantly. Coexistence of immunologic features of both discoid lupus erythematosus and CLP are essential for diagnosing the overlap syndrome; however, the DIF assay of our mucosal biopsy yielded negative results for SLE.9 Therefore, instead of diagnosing our case as an oral variant of the overlap syndrome, we prefer using the term synchronous presentation.
In conclusion, this case documents presentation of 2 distinct autoimmune entities, SLE and reticular OLP, in a 42-year-old woman. To the best of our knowledge, synchronous presentation of these 2 diseases has not been documented before.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Jonsson R., Heyden G., Westberg N.G., Nyberg G. Oral mucosal lesions in systemic lupus erythematosus–a clinical, histopathological and immunopathological study. J Rheumatol. 1984;11(1):38–42. [PubMed] [Google Scholar]
- 2.Urman J.D., Lowenstein M.B., Abeles M., Weinstein A. Oral mucosal ulceration in systemic lupus erythematosus. Arthritis Rheum. 1978;21(1):58–61. doi: 10.1002/art.1780210110. [DOI] [PubMed] [Google Scholar]
- 3.Sverzut A.T., Allais M., Mazzonetto R. Oral manifestation of systemic lupus erythematosus: lupus nephritis–report of a case. Gen Dent. 2008;56(1):35–41. [PubMed] [Google Scholar]
- 4.Khudhur A.S., Di Zenzo G., Carrozzo M. Oral lichenoid tissue reactions: diagnosis and classification. Expert Rev Mol Diagn. 2014;14(2):169–184. doi: 10.1586/14737159.2014.888953. [DOI] [PubMed] [Google Scholar]
- 5.Anuradha C., Malathi N., Anandan S., Magesh K. Current concepts of immunofluorescence in oral mucocutaneous diseases. J Oral Maxillofac Pathol. 2011;15(3):261–266. doi: 10.4103/0973-029X.86673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alrashdan M.S., Cirillo N., McCullough M. Oral lichen planus: a literature review and update. Arch Dermatol Res. 2016;308(8):539–551. doi: 10.1007/s00403-016-1667-2. [DOI] [PubMed] [Google Scholar]
- 7.Chopra A., Bahl R., Puri R., Gill S. Lichen planus and lupus erythematosus overlap syndrome. Indian J Dermatol Venereol Leprol. 1996;62(2):110–111. [PubMed] [Google Scholar]
- 8.Lospinoso D., Fernelius C., Edhegard K., Finger D., Arora N. Lupus erythematosus/lichen planus overlap syndrome: successful treatment with acitretin. Lupus. 2013;22(8):851–854. doi: 10.1177/0961203313492243. [DOI] [PubMed] [Google Scholar]
- 9.Demirci G.T., Altunay I.K., Sarikaya S., Sakiz D. Lupus erythematosus and lichen planus overlap syndrome: a case report with a rapid response to topical corticosteroid therapy. Dermatol Reports. 2011;3(3):e48. doi: 10.4081/dr.2011.e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sekar C.S., Rai R., Karthika N., Laila A. SCLE-LP overlap syndrome. Indian J Dermatol. 2011;56(2):209–210. doi: 10.4103/0019-5154.80420. [DOI] [PMC free article] [PubMed] [Google Scholar]