Introduction
Since introduction of BRAF and MEK inhibition therapy, there has been a significant improvement in response rates, overall survival, and progression-free disease in melanoma patients.1, 2, 3 Combined BRAF and MEK inhibition, compared with BRAF inhibition alone, has shown to delay the emergence of resistance in patients suffering from BRAF V600–mutated advanced melanoma. It has become the standard of care in patients carrying this mutation.4 Several mechanisms of resistance to BRAF and MEK inhibition have been shown. Reactivation of the mitogen-activated protein kinase pathway is the major trigger in more than two-thirds of tumors.5
Case report
We report on a 63-year-old patient who had solely multiple eruptive verrucous epidermotropic melanoma metastases of the lower limb during BRAF and MEK inhibitor therapy with dabrafenib and trametinib. To our knowledge, this is the first description of a solely cutaneous progressive disease during BRAF and MEK therapy.
The patient had a primary nonulcerated melanoma of the left foot diagnosed in 2012. The Breslow tumor thickness was 2.5 mm. After the sentinel lymph node was diagnosed positive in the left groin, the patient underwent radical lymphadenectomy (2 of 12 lymph nodes positive). A mutational analysis revealed a BRAF V600E mutation. One year later, the patient presented to our ward with multiple liver and bone metastases.
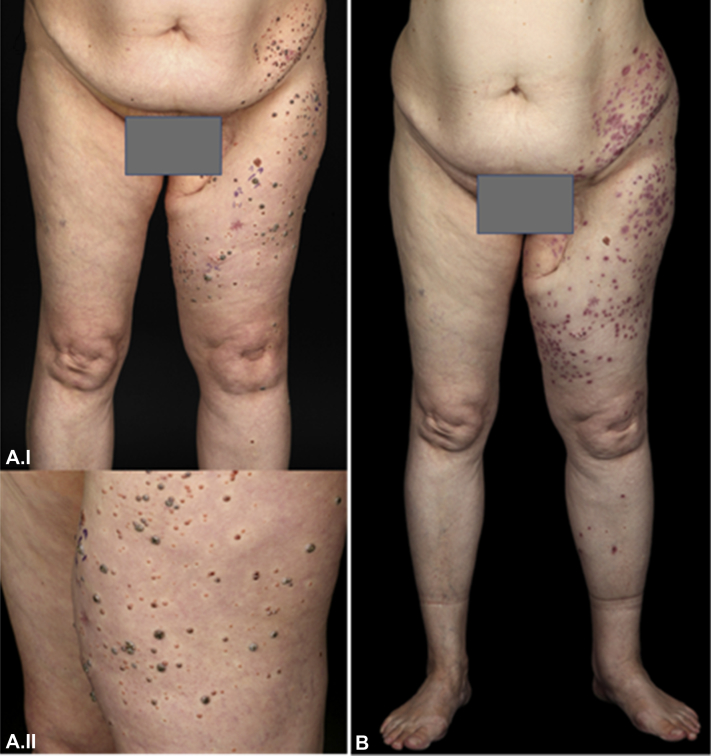
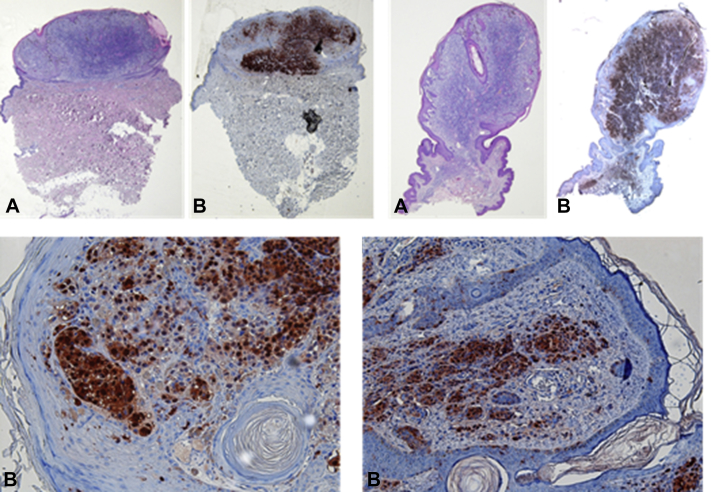
Because of the BRAF V600E mutation, the patient was treated with dabrafenib and trametinib. The medication was tolerated well and without any adverse effects. Radiology images showed partial response over 14 months. The patient was closely monitored with computed tomography scans of the body and cerebral magnetic resonance imaging every 2 to 3 months using RECIST 1.1. criteria. Suddenly after 14 months of treatment with dabrafenib and trametinib, the patient developed multiple verrucous epidermotropic nodules of the left limb and lower abdomen in May 2014 as presented in Fig 1, A. The bone and liver metastases remained stable. Most lesions presented with a white halo around the dark central nodule. Histologically, the lesions presented as epidermotropic, pleomorphic melanoma metastases, as shown in Fig 2. Solar elastosis was also present, highly suggesting previous sun damage to the skin. Four large cutaneous metastases were excised. Others were treated with CO2 laser therapy and topical imiquimod (Fig 1, B) showing complete resolutions after an initial inflammation owing to imiquimod treatment. The disease remained stable for another 7 months until February 2015, when the patient experienced a relapse with multiple para-aortal, parailiac, inguinal, and brain metastases. The treatment was switched to radiation therapy (brain and lymph node metastases) and ipilimumab. Because of progressive disease, the treatment was switched to pembrolizumab 3 months later. The patient deceased another 3 months later.
Fig 1.
A, Multiple verrucous epidermotropic melanoma metastases on the left leg/lower abdomen before therapy and B, 2 months after CO2 laser therapy and topical imiquimod therapy.
Fig 2.
Histology of epidermotropic melanoma metastases. (A, Hematoxylin-eosin stain; B, anti-S100B stain.)
Conclusion
We present a rare case of multiple eruptive verrucous epidermotropic melanoma metastases during treatment with BRAF and MEK inhibitors. Visceral metastases regressed or remained stable during this therapy. This finding could be because of the reactivation of the mitogen-activated protein kinase pathway known as the major trigger of resistance,5 solely in an epidermotropic melanoma cell subclone of our patient. Cutaneous metastases of malignant melanoma often represent the first sign of relapse of this fatal disease.6 Clinically and histologically cutaneous metastases present in various forms. Most commonly, cutaneous metastasis is primarily composed of epithelioid cells. However, epidermotropic metastases as seen in our case are rare.7
Our case shows that CO2 laser therapy and adjuvant imiquimod therapy8, 9 can be successfully applied to control the local appearance of epidermotropic melanoma metastases.
Footnotes
Funding sources: None.
Conflicts of interest: Jochen Utikal is on the advisory board or has received honoraria and travel support from Amgen, BMS, MSD, Novartis and Roche. Christoffer Gebhardt is on the advisory board or has received honoraria and travel support from BMS, MSD, Novartis and Roche. The rest of the authors have no conflicts to declare.
References
- 1.Ascierto P.A., McArthur G.A., Dréno B. Cobimetinib combined with vemurafenib in advanced BRAF(V600)-mutant melanoma (coBRIM): updated efficacy results from a randomised, double-blind, phase 3 trial. Lancet Oncol. 2016;17(9):1248–1260. doi: 10.1016/S1470-2045(16)30122-X. [DOI] [PubMed] [Google Scholar]
- 2.Long G.V., Stroyakovskiy D., Gogas H. Dabrafenib and trametinib versus dabrafenib and placebo for Val600 BRAF-mutant melanoma: a multicentre, double-blind, phase 3 randomised controlled trial. Lancet. 2015;386(9992):444–451. doi: 10.1016/S0140-6736(15)60898-4. [DOI] [PubMed] [Google Scholar]
- 3.Long G.V., Stroyakovskiy D., Gogas H. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N Engl J Med. 2014;371(20):1877–1888. doi: 10.1056/NEJMoa1406037. [DOI] [PubMed] [Google Scholar]
- 4.Stadler S., Weina K., Gebhardt C., Utikal J. New therapeutic options for advanced non-resectable malignant melanoma. Adv Med Sci. 2015;60(1):83–88. doi: 10.1016/j.advms.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Roesch A., Paschen A., Landsberg J., Helfrich I., Becker J.C., Schadendorf D. Phenotypic tumour cell plasticity as a resistance mechanism and therapeutic target in melanoma. Eur J Cancer. 2016;59:109–112. doi: 10.1016/j.ejca.2016.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Tas F., Erturk K. Recurrence behavior in early-stage cutaneous melanoma: pattern, timing, survival, and influencing factors. Melanoma Res. 2017;27(2):134–139. doi: 10.1097/CMR.0000000000000332. [DOI] [PubMed] [Google Scholar]
- 7.Plaza J.A., Torres-Cabala C., Evans H., Diwan H.A., Suster S., Prieto V.G. Cutaneous metastases of malignant melanoma: a clinicopathologic study of 192 cases with emphasis on the morphologic spectrum. Am J Dermatopathol. 2010;32(2):129–136. doi: 10.1097/DAD.0b013e3181b34a19. [DOI] [PubMed] [Google Scholar]
- 8.Utikal J., Zimpfer A., Thoelke A. Complete remission of multiple satellite and in-transit melanoma metastases after sequential treatment with isolated limb perfusion and topical imiquimod. Br J Dermatol. 2006;155(2):488–491. doi: 10.1111/j.1365-2133.2006.07333.x. [DOI] [PubMed] [Google Scholar]
- 9.Van Jarwaarde J.A., Wessels R., Nieweg O.E., Wouters M.W., van der Hage J.A. CO2 laser treatment for regional cutaneous malignant melanoma metastases. Dermatol Surg. 2015;41(1):78–82. doi: 10.1097/DSS.0000000000000251. [DOI] [PubMed] [Google Scholar]