Abstract
Introduction
Brucellosis is communicable between humans and animals. In spite of having an active health care system. Iran is considered as an endemic area and it stands in the fourth place in world ranking. One of the common methods for identifying the disease incidence is a regression analysis. Therefore, the aim of the study was to investigate the trend of brucellosis incidence during 2006 to 2016 and the components affecting such disease.
Materials and Methods
This was a trend study which was conducted on the total of 144 brucellosis cases were recorded in the registration software in CDC of Iranian, Ministry of Health. We analyzed the changes in brucellosis incidence during 2006 to 2016 in Juybar province by the join point regression. Moreover, comparing the changes of incidence in one year intervals was also taken into account.
Results
The average age of patients was 18±29 years. About 60% of the patients were men, and 85.4% had used non-pasteurized dairy and meat products. The contact with animals had a significant difference between the two genders (P= 0.006). During 2006 to 2016, brucellosis incidence had a decreased trend about 15%. This trend had a breakpoint in a way that during 2006 to 2008, 66.2% decrease and during 2008 to 2016, 7% increase was observed that none of these annual percentage changes (APC) were statistically significant at p= 0.05. Also, APC of brucellosis incidence in groups below 20 and between 20 to 50 years old had a decrease in a way that in groups under 20, it had 26.7% decrease and it was statistically significant.
Conclusion
It is necessary to provide appropriate education training, information on the Human Brucellosis for the young and individuals with high risk professions. Moreover, some health behaviors such as not using non-pasteurized dairy, animals’ vaccinations, and awareness of the disease symptoms are needed.
Keywords: Brucellosis, Incidence, Trend analysis
1. INTRODUCTION
Brucellosis is a universally wide spread disease which is communicable between humans and animals (1), created by different varieties of Brucella bacteria (2, 3). Brucellosis can transfer of direct contact with the infected animals or their products such as meat or milk and contact with animals that had spontaneous abortion. Brucellosis in humans is indicative of the disease progression in animals (1) and due to the infections among domestic and wild animals, this disease is distributed worldwide (4) so that it can become endemic in some areas including West Mediterranean, Middle East, Central and Southern parts of USA and India (2, 3).
According to WHO reports, the number of people with brucellosis is 500,000 annually, but it seems that the number of infected people is more than that. That is to say, it is estimated that for each case with clinical symptoms, there are 12 cases without symptoms. In developed countries, just 4 to 10% of cases are diagnosed (5-7). Due to lack of information about incidence of the disease in humans and animals in many countries, inappropriate diagnostic equipment, and lack of valid reports, there are not any appropriate statistics about the prevalence rate of brucellosis (1). Despite of having an active health care system, Iran is considered as an endemic area and it stands in the fourth place in world ranking (6, 7). Although the rate of brucellosis incidence in Iran has decreased from 34 cases in each one hundred thousand people in 2005 to 26 cases in each one hundred thousand people in 2014, still various factors such as long borders of the country, large number of nomads, traditional methods of ranching, inappropriate supervision on dairy products and Importing Domestic Animals, failure to perform the correct and timely vaccination of them (8, 9), and lack of enough knowledge about the disease are known as the main reasons for difficulty in controlling brucellosis in Iran (9, 10). There is a significant difference in the disease prevalence in various parts of the country and the rate varies from 98 to 130 cases in each 100,000 people. Brucellosis prevalence is lower in southern area of the country and its prevalence varies in different seasons, but the highest rate is in the first half of the year (8). The incidence of brucellosis in Mazandaran province is 13.3 cases in each 100000 people and most prevalent age of the disease is 25 to 40 years. Although the disease had a decreasing trend during the recent years (11), it is still considered as a serious problem among various groups especially those living in villages (12). Moreover, brucellosis can create different challenges in developing agriculture and animal husbandry industries, physical disabilities, irregular attendance at work, and high treatment costs (13, 14). In a study focusing on epidemiologic and clinical components of brucellosis in north of Iran, it was observed that using fresh cheese and direct contact with the animals were the main risk factors in transition of the disease (15). One of the common methods for identifying the disease incidence is a regression analysis of the disease trend in which the independent variable is determined in fixed time intervals, and for each interval or distance, a separate regression line is allocated and the borders between breakpoints are identified (16). On the other hand, recognizing the conditions of brucellosis incidence during various times can help in controlling, predicting, supervising, revising the program, analyzing the policies and etiology of the disease. Reviewing the indices trend and considering their changes will assist the health care providers to evaluate the efficiency of health systems during various times and determines to what extend the implementation of programs using various facilities have been successful in reaching their goals.
Moreover, identifying the changes in the trend of diseases’ incidence can be of great significance in evaluating the efficiency of health controlling programs, the functions of treatment-health personnel, and decision-making in health programs.
2. METHOD
This was a trend study which was conducted on all recognized cases with brucellosis (144 patients) in Juybar province during 2006 to 2015 through census. The data was gathered through the registration software in Center for Disease Control of Iranian, Ministry of Health. Information of these people was entered into the software and the changes in brucellosis incidence in each year were taken into account. The join point regression software was used to analyze the changes in brucellosis incidence. This is one of the most appropriate software in a regression which can be employed for estimating regression variables, estimating breakpoints, and drawing the Linear graph. In order to estimate the regression variables, Least Squares Method was used. In addition, the trend of changes in brucellosis incidence was analyzed based on age and gender segregation, then the trend of disease changes over the years was analyzed between the groups. In order to summarize the incidence trend of brucellosis, the researchers made use of AAPC and for estimating the population statistics, the statistical calendar was used. Comparing the changes of brucellosis incidence in one year intervals was also taken into account.
3. RESULTS
The total number of recorded cases with brucellosis during 2006 to 2016 was 144 in Juybar. The average age ofpatients was 18±29 years and the age median was 25 years. The time average between observing the symptoms and detecting the disease was 20±39 days and the median was 12 days. About 78% of the patients were rural, 61.1% were men, and 85.4% of the patients had used non-pasteurized dairy and meat products. Only 27.1% of the animals were given vaccination. Other characteristics are shown in the Table 1. The results showed that, the contact with animals had a significant difference between the two genders (p-value= 0.006). That is to say, the cases with brucellosis were mostly in men than women. During 2006 to 2016, brucellosis incidence had a decreased trend about 15%. This trend had a breakpoint in a way that during 2006 to 2008, 66.2% decrease and during 2008 to 2016, 7% increase was observed. None of these annual percentage changes (APC) were statistically significant at α= 0.05 (Figure 1). During the study phase, the rate of brucellosis incidence in men had 5.6% and in women had 15.2% decreases. This trend had 54.7% decrease in women during 2006 to 2009 and it was statistically significant in α= 0.05. However, during 2009 to 2016 the trend had 11% increase which was not statistically significant (Figure 2). In the first five months of the year, brucellosis incidence had 58.1% increase which was not statistically significant and then it had 21.7% decrease which was statistically significant in α= 0.05. During 12 months, brucellosis incidence had 1.1% increase which was not statistically significant (Figure 3). Annual percentage changes of brucellosis incidence in groups below 20 and between 20 to 50 years old had a decrease in a way that in groups under 20, it had 26.7% decrease and it was statistically significant. But in groups between 20 to 50 years old, it had a breakpoint. That is, during 2006 to 2008 it experienced 71.6% decrease and during 2008 to 2016 it had 14.6% increase. In groups above 50, the changes had 9.1% increase which was not statistically significant (Figures 4, 5, 6). Also, Annual Percent Change of human brucellosis is shown in Table 2.
Table 1. Demographic, biologic and characters of human Brucellosis.
| Variables | frequency | percent | |
|---|---|---|---|
| Education | Illiterate | 38 | 26.4 |
| Primary | 22 | 15.3 | |
| High school | 50 | 34.7 | |
| Academic | 3 | 2.1 | |
| Unknown | 31 | 21.5 | |
| Job | Housekeeper | 38 | 26.4 |
| Self-employee | 6 | 4.2 | |
| Farmer or Rancher | 45 | 31.3 | |
| Laborer | 8 | 5.6 | |
| Student | 32 | 22.2 | |
| Unknown | 15 | 10.3 | |
| History of domestic live stock contact | Yes | 71 | 49.3 |
| No | 62 | 43.1 | |
| Unknown | 11 | 7.6 | |
| Type of domestic animals contact | Keeping animal | 15 | 10.4 |
| Slaughter | 10 | 6.9 | |
| Direct contact | 45 | 31.3 | |
| Unknown | 74 | 51.4 | |
| Type of unpasteurized product that used | Milk | 31 | 21.5 |
| Cheese | 28 | 19.4 | |
| Meet | 4 | 2.8 | |
| Milk and yogurt | 5 | 3.5 | |
| Ice cream | 7 | 4.9 | |
| Milk and cheese | 26 | 18.1 | |
| Cheese, ice cream, Milk and butter | 2 | 1.4 | |
| Unknown | 41 | 28.4 | |
| History of disease in other members of family | Yes | 21 | 14.6 |
| No | 119 | 82.6 | |
| Unknown | 4 | 2.8 | |
| Wright’s test | 1/80<= | 117 | 81.3 |
| 1/80>= | 25 | 17.4 | |
| Unknown | 2 | 1.3 | |
| 2ME test | 1/40<= | 58 | 40.3 |
| 1/40>= | 14 | 9.7 | |
| Unknown | 72 | 50 | |
| Type of case | New | 138 | 95.8 |
| Treatments failure | 6 | 4.2 | |
Figure 1. TheTrend of Brucellosis incidence in 2006-2016.
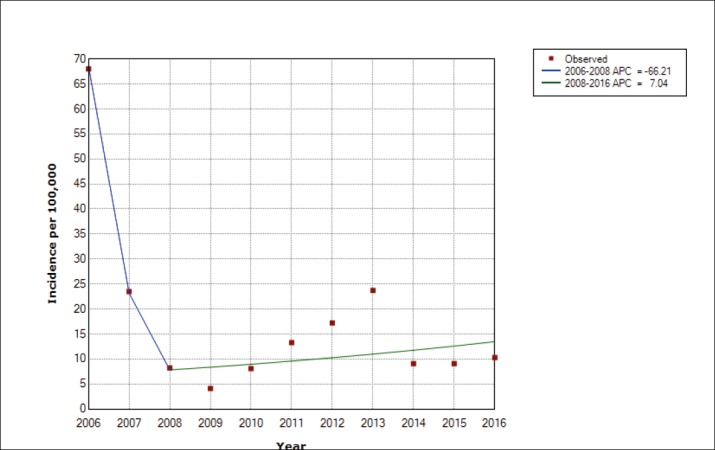
Figure 2. The incidence of brucellosis by gender in 2006-2016.
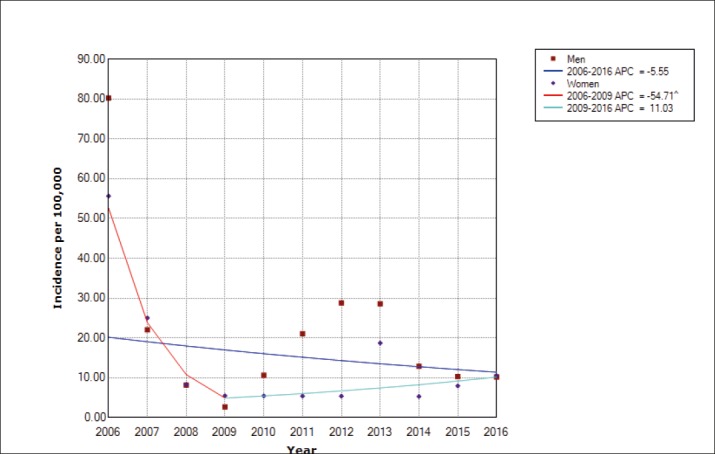
Figure 3. The incidence of brucellosis by month of years in 2006-2016.
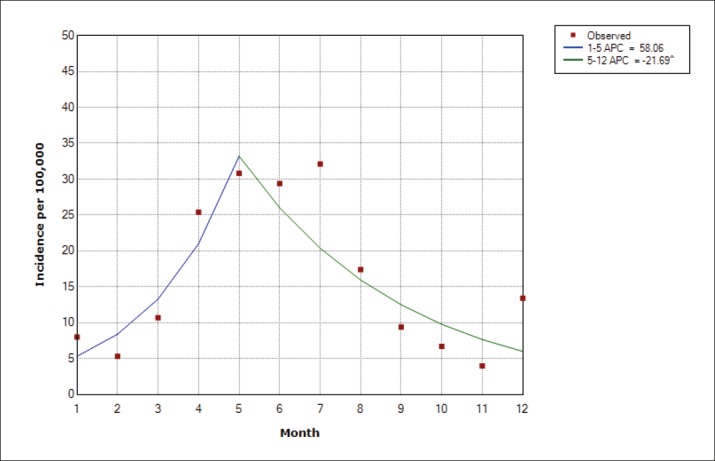
Figure 4. The incidence of brucellosis in the age group less than 20 years in 2006-2016.
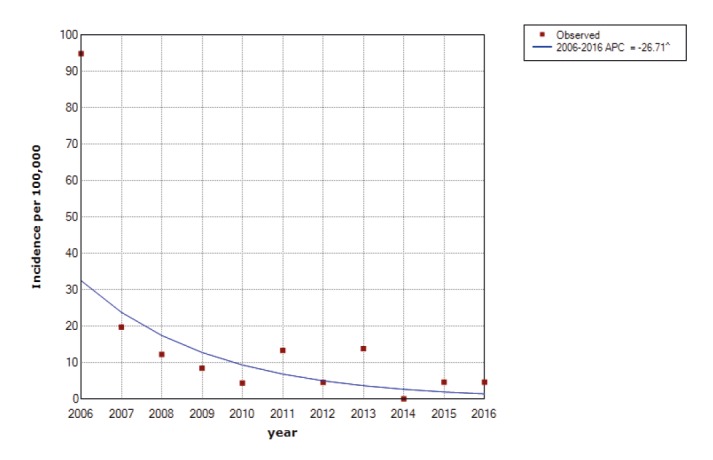
Figure 5. The incidence of brucellosis in the age group 20-50 years in 2006-2016.
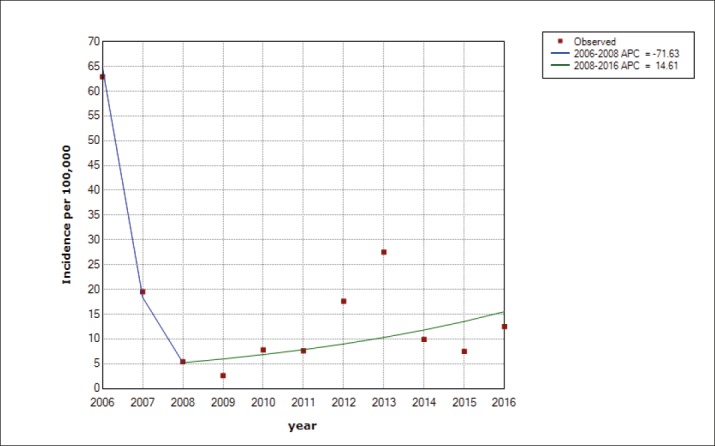
Figure 6. The incidence of brucellosis in the age group over 50 years in 2006-2016.
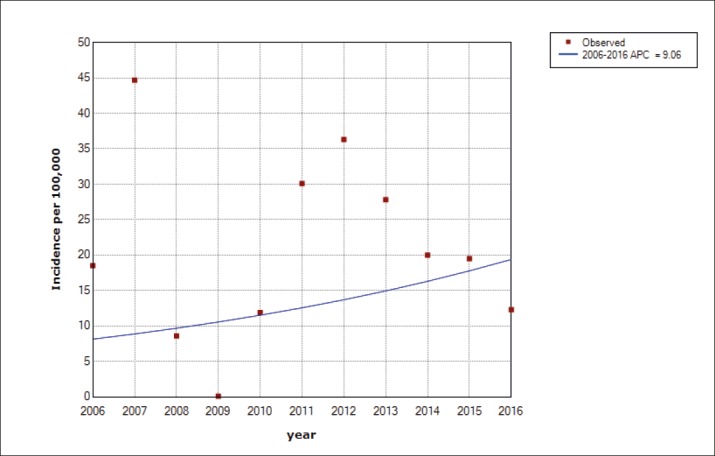
Table 2. Annual Percent Change of human brucellosis: By age, sex, incidence and months. *Annual Percent Change. ^The Annual Percent Change (APC) is significantly different from zero at alpha = 0.05.
| APC* (CI 95%) 2006-2016 | P value | Trend1 | APC (CI 95%) | P value | Trend 2 | APC (CI 95%) | P value | |
|---|---|---|---|---|---|---|---|---|
| Total incidence rate | -15(-38.5 to 17.6) | 0.3 | 2006-2008 | -66.2 (-94.7 to 116.1) | 0.2 | 2008-2016 | 7 (-12.6 to 31.1) | 0.4 |
| Men | -5.6(-22.2 to 14.7) | 0.5 | - | - | - | - | - | - |
| Women | -15.2 (-31.5 to 5.1) | 0.1 | 2006-2009 | -54.7^ (-78.7 to -3.6) | 0.0 | 2009-2016 | 11(-9.3 to 35.9) | 0.3 |
| 20> | -26.7^ (-45.6 to 1.2) | 0.0 | - | - | - | - | - | - |
| 20-50 | -13.3 (-41.6 to 28.6) | 0.5 | 2006-2008 | -71.6 (-97 to 170.5) | 0.2 | 2008-2016 | 14.6(10.4 to 46.6) | 0.2 |
| 50< | 9.1 (-25.1 to 58.9) | 0.6 | - | - | - | - | - | - |
| (January-December) | 1.1 (-18 to 24.7) | 0.9 | January-May | 58.1 (-9.6 to 176.4) | 0.1 | May-December | -21.7^(-38.2 to 0.8) | 0.0 |
4. DISCUSSION
Findings of the current study revealed that during 12 years of survey, the rate of the disease incidence experienced a decreasing trend until 2008 and after that there was increased insignificantly. The reason can be associated with the improvement of care system, health promotion and vaccination of domestic animals. According to the report Ministry of Health in 2013, the provinces are such as East Azerbaijan, Markazi, Hamdan, Lorestan, Kerman shah, and South Khorasan had a very high contamination (31 to 41 in each 100000 people) and provinces including Kurdestan, Zanjan, and Khorasan Razavi had high incidence (21 to 30 in each 100000 people) (7). According to the current study’s results, brucellosis incidence in areas under investigation was 17.7 cases in each 100 thousand people which are lower than the statistics reported by Ministry of Health. In developed countries, due to controlling brucellosis in animals, such disease is controlled in humans (11). Since there is a correlation between the population of animals in the area and the average of brucellosis incidence, it can be inferred that the high rate of incidence in some areas is highly correlated with animal populations. Regarding gender, in most of the studies the rate of the disease incidence in men is higher than that in women (3, 7-9). Similarly, in the present study male patients were 61.1% and female patients were 38.9% and the difference was statistically significant. In another study conducted by Soleimani, the number of men was 54.9% and the number of the women was 45.1% (6). More than 80% of the participants were villagers and the high rate of incidence is due to the great contact of this group to animals and their products. This was also the case in another study carried out by Hashtarkhani (17). In 14.6% of the cases, the disease was observed among family members in the last 12 months and this can be due to the great contract of the family members with infected animals and the use of infected products among them. There was a statistically significant relationship between the disease history among family members and their residential areas. That is to say, in villages the disease history among the family members was 12% and it can be concluded that due to the high contact of these people with domestic animals and their products, the probability of other family members to get infected with brucellosis is higher than usual. Due to the direct contact between human and infected animals, some jobs that can be considered as associated factors with the disease. In a study done in Eastern parts of the Iran, the housewives had the greatest rate of incidence and then the professions of farmer and the rancher were in the second ranking. The incidence of brucellosis had a decreasing trend among people below 50 years old, but an increasing trend among groups above 50. In a study conducted by Moradi et al., in Kurdistan, the highest rate of incidence was among people aged 25 to 44 years (18). Of the total number of patients, 85.4% had used non-pasteurized dairy. Using non-pasteurized milk with 21.5% and non-pasteurized cheese with 19.4% had the greatest role in brucellosis incidence. Similarly, in another studies carried out in Khorasan Razavi, it was reported that non-pasteurized milk and cheese can cause brucellosis more than any other dairy products (19).
In the current study, the average of starting the symptoms and detecting the disease was less than one month and in more than 50% of the cases in a study in Khorasan, this average was less than one month. However in another study in Kurdestan, the average of starting the symptoms and detecting the disease was 35.15 days (18).
Regarding the laboratory tests in current study, the amount of 1.1320 (24.1%) and 1.160 (26.1%) were more than other amounts, while in a study done in Maneh, Samalqan, in South Khorasan, the amount of a 1.160 and 1.80 had the highest frequency in patients. In 2ME test for the present study,1.80 (21.9%) and 1.160 (20. 6%) had the highest frequency which is in line with Maneh, Samalqan study. In Combos right test for this study, the amounts of 1.80 (5.5%) and 1.160 (5.4%) were repeated more than any other amounts, but in Maneh, Samalqan study, 1.320 and 1.160 has the highest frequency (8). In a study conducted by Farazi et al., a statistically significant difference in mean of right test among people above 45 and below 45 was observed that the difference was statistically significant (p<0.001) (20). Investigations revealed that only 27.1% of the domestic animals in the area had given vaccinations and the rest were reported to be vaccinated as soon as possible by the responsible centers. In this study it was reported that the disease incidence had an increasing trend in spring and summer but it was not statistically significant. Some various studies have focused on seasonal patterns in the incidence of brucellosis. In study in Germany revealed that majority of brucellosis cases were reported in summer (15). However a study done in Turkey indicated that spring season had the highest rate of brucellosis incidence (21). According to the results of some studies in Iran, it was indicated that the brucellosis incidence had an increasing trend during spring and summer seasons. In this regard, a study done in 2015 in Iran indicated that the highest rates of the disease incidence in the spring and summer were 34.4% and 32.2% respectively (22). This issue can be related to the factors such as animals’ breeding time, direct contact with the animals, collecting and distributing non-pasteurized milk and other dairy products, and using such products. Results of some other studies in Iran and other parts of the world are in line with the same findings (15, 23-26). Results of the current study indicated that changes of brucellosis incidence have observed a decrease in groups below 20 and 20 to 50 years old. That is to say, the decrease in groups below 20 years had a 26.7% decrease and it is statistically significant, in groups between 20 to 50 there was a breakpoint in which during 2006 to 2008, 71.6% decrease was observed and during 2008 to 2016, 14.6% increase was reported. In groups above 50 years old, 9.1% increase was observed which was not statistically significant. In a study conducted in Khorasan Razavi, the highest rate of incidence was in people aged 21 to 30 years (17). However in another study done in East Azarbaijan province, the highest rate was between individuals aged 40 to 50 (27) which is not in line with the current study’s findings. Professions and other activities related to domestic animals among groups aged 20 to 50 years can be highly relevant to the brucellosis incidence, especially in men.
5. CONCLUSION
It is necessary to provide appropriate education on the Human Brucellosis. Some health behaviors such as not using non-pasteurized dairy, animals’ vaccinations, and awareness of the disease symptoms for appropriate treatment are needed. It is important that a number of patients refer to private sections for treatment and it is not easy to discoveryall of the cases having brucellosis. Another limitation of the study was that since all data related to incidence of brucellosis are not recorded in health care centers, these issues can affect the obtained results of our study.
Acknowledgement
This paper was approved project with code 397(MazUMS 95) by Student Research Committee Faculty of Health, Mazandaran University of Medical Sciences.
Authors contribution
AM, M AA, FR, and GHA made the substantial contribution to conception, design, drafting the article and critical revision for important intellectual content. HS made final modification the article. All authors read and approved of the final manuscript.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zeinali M, Shirzadi MR, Hajrasoliha H. Tehran: Ministery of Health and Medical Education; 2012. National Guideline for Brucellosis Control. [Google Scholar]
- 2.Dean AS, Crump L, Greter H, Schelling E, Zinsstag J. Global burden of human brucellosis: a systematic review of disease frequency. PLoS Negl Trop Dis. 2012;6(10):e1865. doi: 10.1371/journal.pntd.0001865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Refai M. Incidence and control of brucellosis in the Near East region. Veterinary microbiology. 2002;90(1):81–110. doi: 10.1016/s0378-1135(02)00248-1. [DOI] [PubMed] [Google Scholar]
- 4.Hatami H. Tehran: Ministry of Health and Medical Education; 1999. Digital book of brucellosis; pp. 3–8. [Google Scholar]
- 5.Almasi-Hashiani A, Khodayari M, Eshrati B, Shamsi M. Factors affecting the interval between the onset and diagnosis of brucellosis in Markazi Province, Iran (2010-11) Arak Medical University Journal. 2012;14(7):21–30. [Google Scholar]
- 6.Mohammadian M, Mohammadian HA. Epidemiological characteristics and incidence rate of brucellosis over a period of 14 years in the Tiran-Karvan Township, Isfahan, Iran. Journal of Isfahan Medical School. 2014;32(293):1–7. [Google Scholar]
- 7.Mostafavi E, Asmand M. Trend of brucellosis in Iran from 1991 to 2008. Iranian Journal of Epidemiology. 2012;8(1):94–101. [Google Scholar]
- 8.Shoraka HR, Hosseini SH, Safavizadeh A, Avaznia A, Rajabzadeh R, Hejazi A. Epidemiological study of brucellosis in Maneh & Semelghan town, North Khorasan province, in 2008-2009. 2010. pp. 65–72.
- 9.Sofian M, Aghakhani A, Velayati AA, Banifazl M, Eslamifar A, Ramezani A. Risk factors for human brucellosis in Iran: a case-control study. International Journal of Infectious Diseases. 2008;2(2):157–61. doi: 10.1016/j.ijid.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Mahmoodabad SM, Barkhordari A, Nabizadeh M, Ayatollahi J. The Effect of Health Education on Knowledge, Attitude and Practice (KAP) of High School Students’ Towards Brucellosis in Yazd. World Applied Sciences Journal. 2008;5(4):522–4. [Google Scholar]
- 11.Kassiri H, Amani H, Lotfi M. Epidemiological, laboratory, diagnostic and public health aspects of human brucellosis in western Iran. Asian Pacific journal of tropical biomedicine. 2013;3(8):589–94. doi: 10.1016/S2221-1691(13)60121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hashemi SH, Gachkar L, Keramat F, Mamani M, Hajilooi M, Janbakhsh A, et al. Comparison of doxycycline–streptomycin, doxycycline–rifampin, and ofloxacin–rifampin in the treatment of brucellosis: a randomized clinical trial. International Journal of Infectious Diseases. 2012;16(4):e247–e51. doi: 10.1016/j.ijid.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Beheshti S, Rezaian G, Azad F, Faghiri Z, Taheri F. Seroprevalence of brucellosis and risk factors related to high risk occupational groups in Kazeroon, South of Iran. The international journal of occupational and environmental medicine. 2010 Apr;1(2) [PubMed] [Google Scholar]
- 14.Dastjerdi MZ, Nobari RF, Ramazanpour J. Epidemiological features of human brucellosis in central Iran, 2006-2011. Public Health. 2012;126(12):1058–62. doi: 10.1016/j.puhe.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Roushan MH, Mohrez M, Gangi SS, Amiri MS, Hajiahmadi M. Epidemiological features and clinical manifestations in 469 adult patients with brucellosis in Babol, Northern Iran. Epidemiology and infection. 2004;132(06):1109–14. doi: 10.1017/s0950268804002833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Dahouk S, Neubauer H, Hensel A, Schöneberg I, Nöckler K, Alpers K, et al. Changing epidemiology of human brucellosis, Germany, 1962-2005. Emerg Infect Dis. 2007 Dec;13(12):1895–900. doi: 10.3201/eid1312.070527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hashtarkhani S, Akbari M, Jarahi L, Etminiani K. Epidemiological characteristics and trend of incidence of human brucellosis in Razavi Khorasan province. Med J Mashhad. 2016;9:531–8. [Google Scholar]
- 18.Moradi G, Esmaiel Nasab N, Ghaderi E, Sofi Majidpour M, Salimzadeh H. Brucellosis in Kurdistan Province from 1997 to 2003. Annals of Alquds Medicine. 2006;2(1):32–7. [Google Scholar]
- 19.Hadjichristodoulou C, Papatheodorou C, Soteriades E, Panagakos G, Kastritis I, Goutziana G, et al. Epidemiological study of brucellosis in eight Greek villages using a computerised mapping programme. European journal of epidemiology. 1999;15(7):671–80. doi: 10.1023/a:1007673318947. [DOI] [PubMed] [Google Scholar]
- 20.Farazi AA, Sofian M, Ghazisaeedi M. Laboratory features of patients with Brucellosis and its association with titer of Wright agglutination test. ISMJ. 2014;17(5):860–6. [Google Scholar]
- 21.Alton GG, Jones LM. Second. Geneva: World Health Organization; 1967. Laboratory techniques in brucellosis. [PubMed] [Google Scholar]
- 22.Moosazadeh M, Nikaeen R. Seasonal Pattern of Brucellosis in Iran: A Systematic Review and Meta-Analysis. Iranian Journal of Health Sciences. 2016;4(1):62–72. [Google Scholar]
- 23.Geyik MF, Dikici B, Nas K, Hosoglu S. Complications of brucellosis in different age groups: a study of 283 cases in southeastern Anatolia of Turkey. Yonsei medical journal. 2003;44(1):33–44. doi: 10.3349/ymj.2003.44.1.33. [DOI] [PubMed] [Google Scholar]
- 24.Serra AJ, Godoy GP. Incidence, etiology and epidemiology of brucellosis in a rural area of the province of Lleida. Revista espanola de salud publica. 1999;74(1):45–53. [PubMed] [Google Scholar]
- 25.Buzgan T, Karahocagil MK, Irmak H, Baran AI, Karsen H, Evirgen O, et al. Clinical manifestations and complications in 1028 cases of brucellosis: a retrospective evaluation and review of the literature. International journal of infectious diseases. 2010;14(6):e469–e78. doi: 10.1016/j.ijid.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 26.Pérez-Rendón GJ, Almenara BJ, Rodríguez MA. The epidemiological characteristics of brucellosis in the primary health care district of Sierra de Cadiz. Atencion primaria/Sociedad Espanola de Medicina de Familia y Comunitaria. 1997;19(6):290–5. [PubMed] [Google Scholar]
- 27.Rahman A. Liège, Belgique: Belgian Development Cooperation: Université de Liège; 2015. Epidemiology of brucellosis in humans and domestic ruminants in Bangladesh. http://hdl.handle.net/2268/178980. [Google Scholar]


