Abstract
Background
The value of transcervical arterial ligation during transoral robotic surgery (TORS) as a measure to decrease postoperative bleeding incidence or severity is unclear.
Methods
A retrospective single institution study was performed to identify risk factors for hemorrhage after TORS for oropharyngeal squamous cell carcinoma (SCC).
Results
Overall, 13.2% of patients (35/265) experience postoperative hemorrhage. T classification, perioperative use of anticoagulants, surgeon experience >50 cases, and tumor subsite were not predictors of postoperative hemorrhage. Of this cohort, 28% underwent prophylactic arterial ligation. The overall incidence of bleeding was not significantly decreased in patients who underwent arterial ligation (12.1% vs 13.6%; p = .84). However, arterial ligation significantly reduced the incidence of major and severe bleeding events (1.3% vs 7.8%; p = .04). Radiation before TORS was a risk factor for major and severe postoperative hemorrhage (p < .02).
Conclusion
Transcervical arterial ligation during TORS may reduce the severity of postoperative hemorrhagic events.
Keywords: transoral robotic surgery (TORS), robotic surgery, hemorrhage, arterial ligation
INTRODUCTION
Approximately 15,500 cases of oropharyngeal cancer will be diagnosed in 2015.1 Of these, approximately 70% of cases will be human papillomavirus (HPV)-associated tumors.2 The current landscape of head and neck cancer epidemiology and treatment is evolving with the increasing incidence of HPV-associated squamous cell carcinoma (SCC). Although these patients generally have outstanding oncologic outcomes with concurrent chemoradiation (CRT),3 the incidence of severe late toxicity has shown to be as high as 35%.4 Concerns regarding treatment-related toxicity as well as the morbidity of classic transcervical and transmandibular approaches to the oropharynx have driven a rising interest in transoral robotic surgery (TORS). TORS has now established itself as a common treatment modality in the multidisciplinary management of oropharyngeal SCC.5 Although there is a current lack of published prospective outcome data, recent retrospective reports on locoregional control and survival are encouraging.6 Like any surgical procedure, understanding its place in a treatment paradigm requires understanding relevant complications. Like many oropharyngeal surgeries, bleeding is the most common complication after TORS.7,8 Other complications include dysphagia, lingual or glossopharyngeal nerve injury, and velopharyngeal insufficiency. Bleeding rates after TORS have been variable in the literature, with rates ranging from 3.1% to 13.1%.7–13 Rates have generally been greater than that seen with adult tonsillectomy, which, in a recent study of >7000 adult tonsillectomies, had a postoperative bleeding rate of 4.8%.14 Postoperative oropharyngeal hemorrhage, particularly when severe, can lead to airway compromise, aspiration, asphyxiation, and cardiopulmonary arrest. The most common time for postoperative hemorrhage is postoperative days 8 to 10.9,11,13
Risk factors and strategies for prevention of postoperative bleeding are not clearly delineated in the literature. However, the most important factors in preventing hemorrhage are a meticulous surgical technique and a thorough understanding of “inside-out” oropharyngeal anatomy. This anatomy is well described in cadaveric and animal-based studies from our institution and the University of Pennsylvania.15,16
Factors discussed in the literature as potential contributors to postoperative bleeding have included surgical experience, tumor size, previous radiotherapy, and use of anticoagulants. The significance of each these factors, however, remains unclear. In 1 survey-based study of >2000 TORS procedures, surgical experience of >50 TORS cases was associated with reduced overall complications and reduced bleeding events.8 No other studies have documented such an association between surgeon experience and bleeding risk.
Concurrent transcervical arterial ligation of branches of the external carotid system during TORS has been proposed as one potential method of altering the incidence or severity of postoperative bleeding.8,9,11,13 However, the value of this intervention as a method to reduce postoperative hemorrhage is unclear. Some have suggested that ligation reduces the incidence of severe or catastrophic bleeding.9,13
A previous study at this institution demonstrated that arterial ligation was associated with a nonsignificant trend toward reduced severe bleeding events from 7.3% to 3.0%.13 This finding ultimately led to a change in practice at our institution toward most patients undergoing arterial ligation during TORS. This retrospective study is a continuation of that previous study to document the results of this institutional change in practice. As such, the primary purpose of this study was to reinvestigate bleeding trends after TORS and specifically assess the value of arterial ligation in reducing the severity of postoperative bleeds.
MATERIALS AND METHODS
After study approval by the University of Pittsburgh Institutional Review Board, we reviewed the medical records of 318 patients who underwent TORS from December 2009 to August 2015. Inclusion criteria for this study included TORS performed for oropharyngeal SCC and follow-up of >1 month. Patients undergoing TORS for surgical salvage after definitive radiation or CRT were included. We excluded patients who underwent robot-assisted open oropharyngeal resections. With application of these criteria, 265 patients were identified for analysis.
Data were collected through independent review of the electronic medical records at our institution. All patients underwent TORS using the da Vinci surgical robot (Intuitive Surgical, Sunnyvale, CA) with a site-specific operative approach. Procedures were performed by 3 experienced TORS surgeons. Patients undergoing TORS for identification of an unknown primary tumor underwent palatine tonsillectomy and base of tongue resection.
Basic information extracted from the records included patient demographics, date of presentation, surgical procedure, and clinical course. The following parameters were used in our analysis of risk for postoperative hemorrhage: age, sex, indication for surgery (known primary vs unknown primary), history of radiotherapy to the upper aerodigestive tract, T classification, oropharyngeal tumor subsite (tonsil, base of tongue [BOT], or other), use of perioperative anticoagulants agents (including antiplatelet agents), surgeon experience >50 cases, and performance of a prophylactic transcervical arterial ligation of the ipsilateral external carotid system. The type of arterial ligation was also studied.
The primary outcome studied was postoperative oropharyngeal hemorrhage. Bleeding severity was classified using a scheme developed at the Mayo Clinic.9 This classification scheme can be found in Table 1. For the purposes of this analysis, we chose to analyze risk factors for all postoperative bleeding events and the subset of major and severe bleeding events. Major and severe bleeding events were felt to represent the most significant risk to patients because of the associated risk of airway compromise.
TABLE 1.
Mayo Clinic classification scheme for postoperative hemorrhage.9
| Minor | Any description of visualized bright red blood or blood clots resolved without operative management whether or not physician evaluation or hospitalization occurred. |
| Intermediate | Diffuse venous oozing or small arterial source bleeding resulting in operating room evaluation or intervention managed with monopolar or bipolar cautery. |
| Major | Brisk or copious bleeding requiring operative intervention managed with transoral or transcervical vessel ligation, or interventional radiology embolization. |
| Severe | Bleeding resulting in life-threatening medical complications such as:
|
Reproduced with permission from JAMA Otolaryngol–Head Neck Surg 2013;139:1212–1218. © 2013 American Medical Association. All rights reserved.
Descriptive statistics of all study variables were generated with the assistance of commercial statistical software (SPSS version 20.0; IBM SPSS, Chicago, IL). Univariate logistic regression was performed to identify predictors of postoperative bleeding events and the subset of major/ severe events. All statistical tests were 2-sided and p values were evaluated such that consideration for statistical significance was p < .05.
RESULTS
A total of 265 patients underwent TORS for oropharyngeal SCC at our institution from 2009 to 2015. Patient demographics can be found in Table 2. The mean age on presentation was 59 years and 80% of patients were men. HPV status of the tumor, assessed by p16 immunostaining, was positive in 83.9% of cases (219/265). TORS was performed for identification of an unknown primary in 22.7% of patients (60/265). Of the entire cohort, 15.9% had a history of radiotherapy. Tumor classifications were as follows: T1 = 117 of 265; T2 = 77 of 265; and T3 = 27 of 265. The remaining patients had an unknown primary or the T classification was unable to be assessed through review of the medical records. With respect to subsite, 43% of tumors (114/265) were located in the tonsils and 46% in the BOT (122/265). A total of 27.9% of patients (74/265) underwent transcervical arterial ligation, whereas 76.6% (202/265) underwent neck dissection concurrent with TORS.
TABLE 2.
Patient demographics and rates of postoperative hemorrhage after transoral robotic surgery.
| No. of patients (N)* | Total patients (n = 265) | Postoperative hemorrhage (n = 35) | p value | Major / severe postoperative hemorrhage (n = 16) | p value | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| N | % | N | % | N | % | |||
| Age, y, mean | 59 | 58 | .09 | 56 | .08 | |||
| Sex | ||||||||
| Male | 214 | 80.0 | 32 | 15.0 | .09 | 2 | 0.0 | .74 |
| Female | 51 | 20.0 | 3 | 6.0 | 14 | 0.1 | ||
| Known primary | ||||||||
| Yes | 205 | 77.3 | 32 | 15.6 | .03 | 16 | 7.8 | .02 |
| No | 60 | 22.7 | 3 | 5.0 | 0 | 0.0 | ||
| Surgeon experience >50 cases | ||||||||
| Yes | 127 | 47.9 | 18 | 14.1 | .78 | 4 | 3.1 | .07 |
| No | 138 | 52.1 | 17 | 12.3 | 12 | 8.6 | ||
| History of radiation | ||||||||
| Yes | 41 | 15.9 | 9 | 22.0 | .06 | 6 | 14.6 | .02 |
| No | 223 | 84.1 | 25 | 11.2 | 10 | 4.5 | ||
| T classification | ||||||||
| T1 | 117 | 44.1 | 12 | 10.3 | .43 | 4 | 3.4 | .20 |
| T2 | 77 | 29.0 | 14 | 18.2 | 8 | 10.4 | ||
| T3 | 27 | 10.1 | 4 | 14.8 | 2 | 7.4 | ||
| Tumor subsite | ||||||||
| Tonsil | 114 | 43.0 | 15 | 13.2 | .53 | 6 | 5.3 | .65 |
| BOT | 122 | 46.0 | 18 | 14.8 | 9 | 7.4 | ||
| Other | 29 | 10.9 | 2 | 6.9 | 1 | 3.4 | ||
| Anticoagulant | ||||||||
| Yes | 62 | 23.7 | 11 | 17.7 | .23 | 6 | 9.7 | .22 |
| No | 202 | 76.2 | 24 | 11.9 | 10 | 5.0 | ||
| Transcervical arterial ligation | ||||||||
| Yes | 74 | 27.9 | 9 | 12.1 | 1 | 1.3 | ||
| No | 191 | 72.0 | 26 | 13.6 | .75 | 15 | 7.8 | .04 |
Abbreviation: BOT, base of tongue.
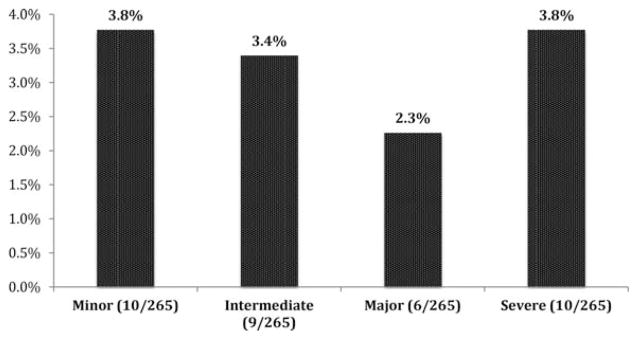
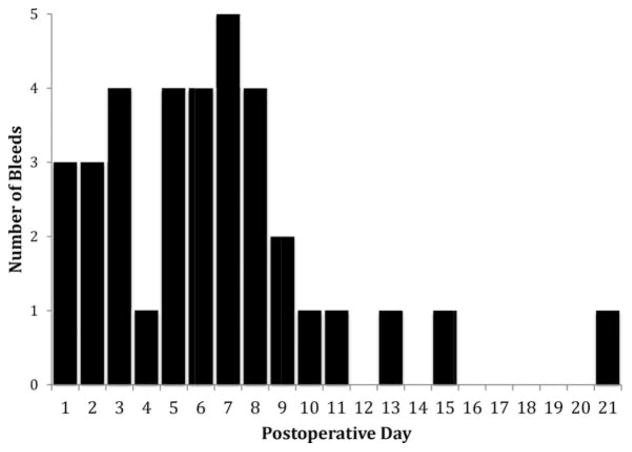
Overall, 13.2% of patients (35/265) experienced varying degrees of postoperative hemorrhage. In 71.4% of the cases (25/35), the patient was taken to the operating room for control. The distribution of bleeds based on severity can be found in Figure 1 and was as follows: minor = 3.7% (10/35); intermediate = 3.3% (9/35); major = 2.2% (6/35); and severe = 3.7% (10/35). The median day of presentation for postoperative bleeding was postoperative day 6 (see Figure 2). The hemorrhage was classified as major or severe in 6.0% of cases (16/265).
FIGURE 1.
Classification of postoperative oropharyngeal bleeding (N = 35/265) by severity.
FIGURE 2.
Timing of postoperative bleeding after transoral robotic surgery (median, day 6). Number of postoperative bleeding events by postoperative day. One outlier was excluded (>3 SD from mean).
Age, sex, use of perioperative anticoagulants, and surgeon experience >50 cases were not found to be significant predictors of postoperative hemorrhage or hemorrhage severity. There was also no relationship between T classification or subsite and postoperative bleeding events.
TORS for identification of an unknown primary was associated with lower absolute rates of postoperative hemorrhage (5.0% vs 15%; p < .03). There were no major or severe bleeding events in this group.
A history of radiotherapy to the upper aerodigestive tract was a significant predictor of major/severe postoperative bleeding events. The incidence of major/severe bleeding events in this cohort was 14.6% versus 4.5% in the nonirradiated cohort (p < .02). There was a higher absolute rate of bleeding of any severity in the radiated cohort (22.0 vs 11.2%), but this was not statistically significant. Of the patients with a history of radiation, 12 patients underwent transcervical arterial ligation and there was a trend toward reduced major/severe postoperative hemorrhage with transcervical arterial ligation (20.7% vs 0%; p = .15), but this relationship was not statistically significant.
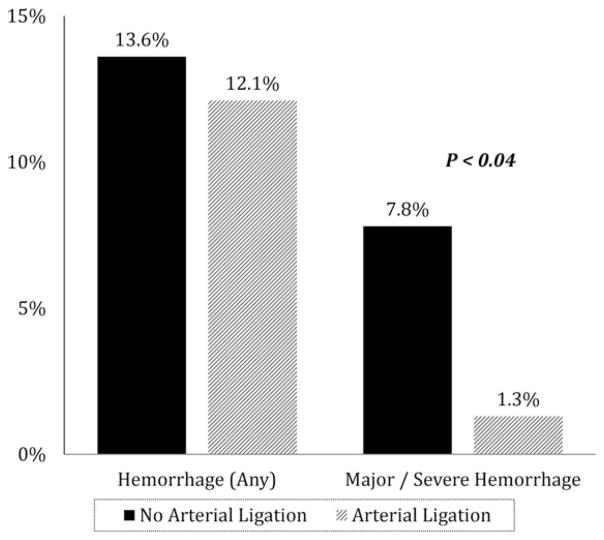
The performance of a transcervical arterial ligation was protective against postoperative major/severe bleeding (p < .04). Of the 74 patients who underwent arterial ligation concurrent with TORS, only 1 patient (1.3%) had a postoperative major/severe bleed. In the subset that did not undergo arterial ligation, the rate of major/severe bleeding was 7.8%. Transcervical arterial ligation did not alter the absolute rate of postoperative hemorrhage (p < .75; see Figure 3). The need for return to the operating room was decreased in the cohort that underwent ligation, but this was not statistically significant (55% vs 76%; p = .32).
FIGURE 3.
Postoperative hemorrhage versus performance of transcervical arterial ligation.
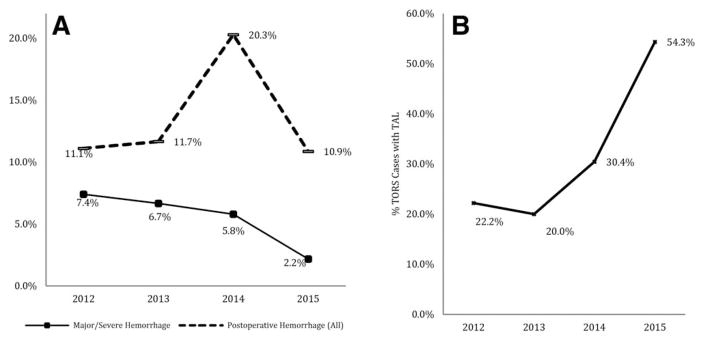
The percentage of TORS resections performed with concurrent arterial ligation increased from 22.2% in 2012 to 54.3% in 2015. With that increase, there has been a decrease in the incidence of major/severe bleeding from 7.4% in 2012 to 2.2% in 2015 (see Figure 4). There was an unusually high number of postoperative bleeds (20.3%, 14/69) seen in 2014 and it is unclear why that was the case. This was due to an elevated number of minor/intermediate bleeds. The data from 2014 have been reviewed, and although the cohort treated in 2014 had a higher frequency of past radiotherapy (16/69), they were otherwise similar to past years in terms of distribution of tumor size, surgeon experience, surgical indications, and use of anticoagulants.
FIGURE 4.
Trend in postoperative hemorrhage (A) since implementation of transcervical arterial ligation in 2012. (B) Percentage of transoral robotic surgery cases performed with transcervical arterial ligation over time.
There are 2 general approaches to arterial ligation among our surgeons. Ligation was performed in all cases at the time of primary neck dissection, and silk sutures were used to ligate individual vessels. The first method is ligation of the proximal stump of the external carotid artery (ECA). The second is distal ligation of individual branches of the ECA. The most frequent arteries ligated were the lingual, facial, and ascending pharyngeal arteries. There was no difference in rates of absolute postoperative bleeding between the 2 methods (p < .7). Only 1 severe bleed occurred in the 74 patients who had arterial ligations. This patient underwent ligation of the proximal ECA and then had severe postoperative hemorrhage from a lingual artery pseudoaneurysm identified on angiography.
There were no complications associated with performance of a transcervical arterial ligation. Specifically, there were no major vascular injuries, cranial nerve palsies, or adverse neurologic sequelae. There were no postoperative pharyngocutaneous fistulas. Two patients had intraoperative communication between the oropharyngeal surgical site and the neck, which was repaired primarily.
Overall, 8 patients underwent angiography and endovascular intervention for postoperative bleeding. Only 1 patient had a vessel abnormality noted (lingual pseudoaneurysm). In 7 of 8 cases, no bleeding vessel was appreciated and the patient underwent empiric embolization of an ipsilateral external carotid branch.
DISCUSSION
Over the last 10 years, the interest in TORS as part of the multidisciplinary management of patients with oropharyngeal SCC has increased markedly. TORS is a relatively new technique, but early retrospective reports of both oncologic and functional outcomes are encouraging.6,17 The largest multi-institutional retrospective series documenting oncologic outcomes was recently published by de Almeida et al,6 documenting a 2-year locoregional control rate of 91.8%. Rates of chronic gastrostomy tube dependence after TORS and risk-adjusted adjuvant therapy are 0% to 7%.17 With increasing experience with TORS, we are also starting to understand the complication profile as well.
Bleeding after transoral robotic surgery is the most common and most feared complication. Understanding the associated risks and methods of preventing postoperative hemorrhage is of upmost interest to the head and neck surgeon. In a retrospective report from our institution, we previously have reported a trend toward reduced severity of postoperative hemorrhage with arterial ligation.13 At the University of Pittsburgh, this prompted a change in practice with increasing use of arterial ligation demonstrated in Figure 4. The purpose of this study was to reexamine our data with the addition of 80 patients and 31 cases of vessel ligation.
In terms of rates of overall postoperative bleeding, only the indication for surgery (resection of a known primary) was associated with a significantly increased risk of postoperative bleeding. In our series, TORS performed for identification of an unknown primary was associated with a low rate of postoperative hemorrhage (5%) and no patients experienced major or severe hemorrhage. These patients infrequently undergo concurrent neck dissection during this procedure making performance of a transcervical arterial ligation generally impractical. This outcome makes intuitive sense as the plane of dissection utilized in TORS performed for identification of unknown primary tumors is submucosal compared with a deeper, intramuscular plane utilized when TORS is performed for resection of a known primary tumor. Based on the low risk of bleeding with this procedure in our series, we do not perform arterial ligation during TORS for unknown primary identification.
Understanding the incidence and risk profile for major or severe bleeding was the primary purpose of the study, as these are the patients faced with an immediate threat to life with these events. In our cohort of 265 patients, 2 patients died in the immediate postoperative period from oropharyngeal bleeding and asphyxiation. Parameters associated with increased rates of major/severe postoperative bleeding were a history of radiotherapy, TORS for a known primary tumor, and lack of a transcervical arterial ligation. Interestingly, T classification, tumor subsite, perioperative use of anticoagulants, and surgeon experience >50 cases did not influence rates of major/severe hemorrhage.
Radiotherapy was statistically the strongest predictor of postoperative major/severe hemorrhage (p < .02). Patients with a history of radiotherapy (n = 41) had a 14.6% overall rate of major/severe hemorrhage in our series. In the subset of irradiated patients who underwent transcervical arterial ligation, there were no cases of major/severe hemorrhage (0%; 0/12), but this relationship was not statistically significant. Several studies have documented increased risks of perioperative complications in the setting of salvage surgery.18 Radiation has a multitude of physiologic effects at the levels of the macrovasculature and microvasculature. These include premature atherosclerosis, weakening of the arterial wall, and fragmentation of elastic filaments. Concurrent CRT has also been shown to cause spontaneous oropharyngeal hemorrhage in the absence of surgical intervention through vascular erosion at the site of the primary tumor.19 Radiotherapy often increases surgical difficulty because of fibrosis and obliteration of tissue planes. Previously irradiated patients, in this series, have a high rate of postoperative hemorrhage. Although statistically insignificant, it seems that this subset of patients may benefit from arterial ligation. In the irradiated patient who will not undergo neck dissection concurrent with TORS, strong consideration must be given to prophylactic tracheostomy for postoperative airway protection.
Currently, there is no consensus on the value of transcervical arterial ligation during TORS. Some have noted trends in reduction of bleeding incidence or severity, whereas others have seen no change. In this study, arterial ligation had no impact on the overall incidence of postoperative bleeding events but did reduce the risk of major/ severe postoperative bleeding events (1.3% vs 7.8%; p < .04). The relationship, interestingly, seems independent of surgeon experience. In this study, there was no difference in the incidence or severity of bleeding events with increasing surgeon experience. In cases in which the surgeon’s experience exceeded 50 cases (n = 127), 4 major/ severe bleeds were seen in patients who did not undergo ligation (5%) compared with 0 major/severe bleeds in the ligated subset. With the gradual implementation of arterial ligation at our institution, our major and severe bleeding events have become more infrequent. Based on our experience, we are performing arterial ligation in all cases in which a concurrent neck dissection is done. There have been no intraoperative or postoperative complications related to arterial ligation. Two approaches to vascular ligation have been practiced in our center, one being ligation of the main ECA trunk and the other of distal ligation of individual branches. Although we did not observe significant differences between these approaches in our study, the one severe bleeding event that followed arterial ligation occurred after ECA trunk ligation in a patient who developed a lingual artery pseudoaneurysm. Distal ligation theoretically prevents arterial backflow and reduces intravascular pressures most efficiently at the surgical site. With these considerations in mind, we feel that arterial ligation is most appropriately performed through distal dissection of branches into the parapharyngeal space and selective ligation.
The ability to perform arterial ligation is only one of the many benefits associated with performing with a neck dissection concurrent with TORS. In addition to this, performing a neck dissection in the primary versus delayed setting offers increased patient convenience, potentially less anesthetic morbidity, and does not have the potential to delay adjuvant therapy. For all these reasons, we have made it our routine practice to perform neck dissection with all TORS cases when clinically indicated.
There were limitations to this study and potential bias primarily related to its retrospective design. The number of patients who ultimately underwent arterial ligation may have been underestimated given that obtaining this information was heavily dependent on the surgeon’s operative report. Additionally, we were unable to develop a multivariate regression because of the fact that only 1 patient had postoperative major or severe bleeding after undergoing arterial ligation. We have clearly shown a reduction in severity in postoperative bleeding over the 5-year TORS experience at our institution. In this study, the benefit of arterial ligation is independent of levels of surgeon experience. However, we did see a trend toward reduced severity of bleeding with surgeon experience. The relative contributions of vessel ligation and improved transoral hemostatic interventions from experience cannot be demonstrated from our study. A larger study in the future may more clearly delineate this relationship.
CONCLUSION
TORS is a safe and feasible operative approach to resection of appropriately selected oropharyngeal tumors. Hemorrhage after TORS, although infrequent, can be severe and potentially lethal. Transcervical arterial ligation reduces the severity of postoperative bleeding events and should be considered in all TORS cases in which a neck dissection is performed concurrently. Patients undergoing salvage TORS after radiotherapy have an increased risk of hemorrhage after TORS and transcervical arterial ligation or prophylactic tracheotomy should be considered at the time of surgery.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C. Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol. 2015;33:3235–3242. doi: 10.1200/JCO.2015.61.6995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Machtay M, Moughan J, Trotti A, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol. 2008;26:3582–3589. doi: 10.1200/JCO.2007.14.8841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holsinger FC, Ferris RL. Transoral endoscopic head and neck surgery and its role within the multidisciplinary treatment paradigm of oropharynx cancer: robotics, lasers, and clinical trials. J Clin Oncol. 2015;33:3285–3292. doi: 10.1200/JCO.2015.62.3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Almeida JR, Li R, Magnuson JS, et al. Oncologic outcomes after transoral robotic surgery: a multi-institutional study. JAMA Otolaryngol Head Neck Surg. 2015;141:1043–1051. doi: 10.1001/jamaoto.2015.1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinstein GS, O’Malley BW, Jr, Magnuson JS, et al. Transoral robotic surgery: a multicenter study to assess feasibility, safety, and surgical margins. Laryngoscope. 2012;122:1701–1707. doi: 10.1002/lary.23294. [DOI] [PubMed] [Google Scholar]
- 8.Chia SH, Gross ND, Richmon JD. Surgeon experience and complication with transoral robotic surgery (TORS) Otolaryngol Head Neck Surg. 2013;149:885–892. doi: 10.1177/0194599813503446. [DOI] [PubMed] [Google Scholar]
- 9.Pollei TR, Hinni ML, Moore EJ, et al. Analysis of postoperative bleeding and risk factors in transoral surgery of the oropharynx. JAMA Otolaryngol Head Neck Surg. 2013;139:1212–1218. doi: 10.1001/jamaoto.2013.5097. [DOI] [PubMed] [Google Scholar]
- 10.Laccourreye O, Malinvaud D, Garcia D, et al. Postoperative hemorrhage after transoral oropharyngectomy for cancer of the lateral oropharynx. Ann Otol Rhinol Laryngol. 2015;124:361–367. doi: 10.1177/0003489414558109. [DOI] [PubMed] [Google Scholar]
- 11.Asher SA, White HN, Kejner AE, Rosenthal EL, Carroll WR, Magnuson JS. Hemorrhage after transoral robotic-assisted surgery. Otolaryngol Head Neck Surg. 2013;149:112–117. doi: 10.1177/0194599813486254. [DOI] [PubMed] [Google Scholar]
- 12.Lörincz BB, Möckelmann N, Busch CJ, Knecht R. Functional outcomes, feasibility, and safety of resection of transoral robotic surgery: a single-institution series of 35 consecutive cases of transoral robotic surgery for oropharyngeal squamous cell carcinoma. Head Neck. 2015;37:1618–1624. doi: 10.1002/hed.23809. [DOI] [PubMed] [Google Scholar]
- 13.Mandal R, Duvvuri U, Ferris RL, Kaffenberger TM, Choby GW, Kim S. Analysis of post-transoral robotic-assisted surgery hemorrhage: frequency, outcomes, and prevention. Head Neck. 2016;38(Suppl 1):E776–E782. doi: 10.1002/hed.24101. [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharyya N, Kepnes LJ. Revisits and postoperative hemorrhage after adult tonsillectomy. Laryngoscope. 2014;124:1554–1556. doi: 10.1002/lary.24541. [DOI] [PubMed] [Google Scholar]
- 15.Wang C, Kundaria S, Fernandez–Miranda J, Duvvuri U. A description of arterial variants in the transoral approach to the parapharyngeal space. Clin Anat. 2014;27:1016–1022. doi: 10.1002/ca.22273. [DOI] [PubMed] [Google Scholar]
- 16.Hockstein NG, Weinstein GS, O’Malley BW., Jr Maintenance of hemostasis in transoral robotic surgery. ORL J Otorhinolaryngol Relat Spec. 2005;67:220–224. doi: 10.1159/000088012. [DOI] [PubMed] [Google Scholar]
- 17.Hutcheson KA, Holsinger FC, Kupferman ME, Lewin JS. Functional outcomes after TORS for oropharyngeal cancer: a systematic review. Eur Arch Otorhinolaryngol. 2015;272:463–471. doi: 10.1007/s00405-014-2985-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodwin WJ., Jr Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means? Laryngoscope. 2000;110(3 Pt 2 Suppl 93):1–18. doi: 10.1097/00005537-200003001-00001. [DOI] [PubMed] [Google Scholar]
- 19.Self EM, Bumpous J, Ziegler C, Wilson L, Potts K. Risk factors for hemorrhage after chemoradiation for oropharyngeal squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2013;139:356–361. doi: 10.1001/jamaoto.2013.103. [DOI] [PubMed] [Google Scholar]