Abstract
Ticks host a wide range of zoonotic pathogens and are a significant source of diseases that affect humans and livestock. However, little is known about the pathogens associated with bat ticks. We have collected ectoparasites from bat carcasses over a seven year period. Nucleic acids (DNA and RNA) were extracted from 296 ticks removed from bats and the species designation was confirmed in all ticks as Argas (Carios) vespertilionis. A subset of these samples (n = 120) were tested for the presence of zoonotic pathogens by molecular methods. Babesia species, Rickettsia spp., within the spotted fever group (SFG), and Ehrlichia spp. were detected in ticks removed from 26 bats submitted from 14 counties across England. The prevalence of Rickettsia spp. was found to be highest in Pipistrellus pipistrellus from southern England. This study suggests that the tick species that host B. venatorum may include the genus Argas in addition to the genus Ixodes. As A. vespertilionis has been reported to feed on humans, detection of B. venatorum and SFG Rickettsia spp. could present a risk of disease transmission in England. No evidence for the presence of flaviviruses or Issyk-Kul virus (nairovirus) was found in these tick samples.
Introduction
Bats (Chiroptera) are widely distributed across the United Kingdom (UK), with 17 species that breed indigenously1. Bats are recognized as reservoirs or carriers of numerous species of viruses, bacteria and protozoan parasites, many with zoonotic potential to infect humans2,3. They also host a range of ectoparasites that could play a role in the transmission of pathogenic organisms. During recent decades, increasing urbanisation and the adaptation of bats to urban habitats has increased the opportunities for contact between bats and bat-associated ticks with humans and domestic animals3–5. Ticks are obligate hematophagous arthropods that are considered second only to mosquitoes as vectors of pathogens that cause disease in humans and animals6. Bats are subject to parasitism by a number of specialized tick species7. Bats form roosts that they return to on a daily basis and can become infested with ticks. The adaptation of ticks to such environments is referred to as nidicolous or nest-dwelling behaviour. Nidicolous bat ticks include Argas vespertilionis (also known as Carios vespertilionis), Ixodes vespertilionis and I. ariadnae. Other tick species associated with bats include I. simplex, I. ricinus and Dermacentor reticulatus3,8. Both I. ricinus and A. vespertilionis are widely distributed across the UK9. These ticks can also bite humans and have the potential to transmit pathogens between bats and human4,10. The epidemiological significance for the transmission of diseases to humans from bats and bat ticks has become increasingly recognized although limited by our understanding of bat tick distribution and pathogen associations. A range of vector-borne pathogens have been detected in bat ticks including piroplasms (Babesia vesperuginis, B. crassa, B. canis, Theileria capreoli, and T. orientalis), Borrelia (Borrelia burgdorferi, Bo. CPB1), Rickettsia spp., Ehrlichia spp. and Issyk-kul virus3,4,11. Bo. burgdorferi sensu lato, the causative agent of Lyme disease, was detected in A. vespertilionis collected between 1896 and 1994 from England and Wales11. B. vesperuginis is hypothesized to be a vector-borne Babesia transmitted by A. vespertilionis that is virulent to some bat species12.
To estimate the burden of tick-borne diseases and host exposure to bat tick bites in the UK, detailed information about distribution and abundance of bat ticks and bat tick-borne diseases is critical. There have been no comprehensive reports regarding this field in the UK bat tick population comparable to similar studies in continental Europe3. In order to assess the risk of pathogen transmission from bat-associated ticks, the distribution and species abundance of ticks collected from bats across the UK has been investigated and tested for a range of tick-borne pathogens.
Results
Tick infestations of bats
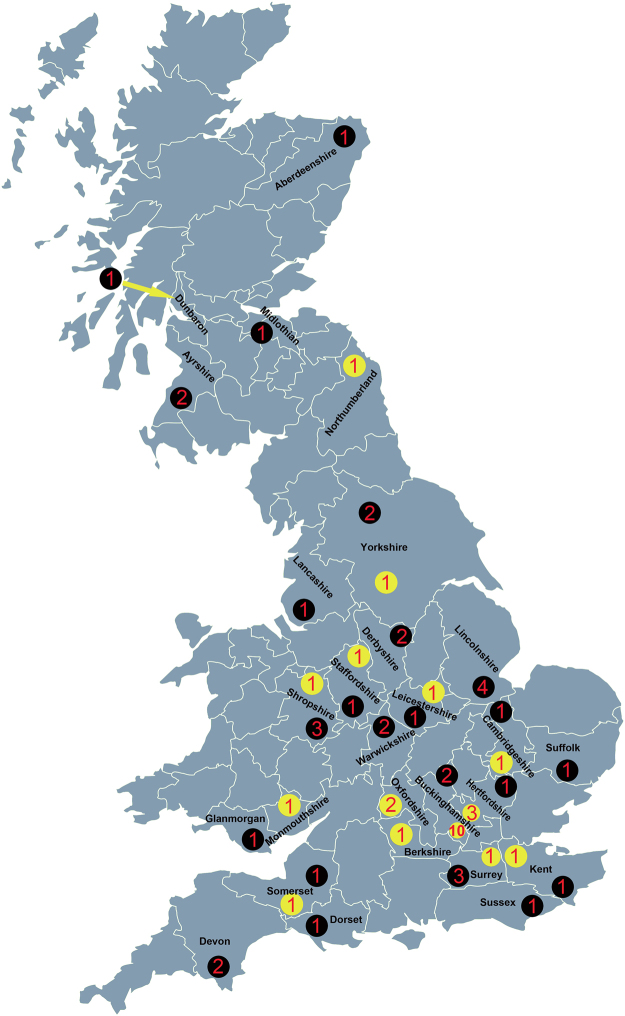
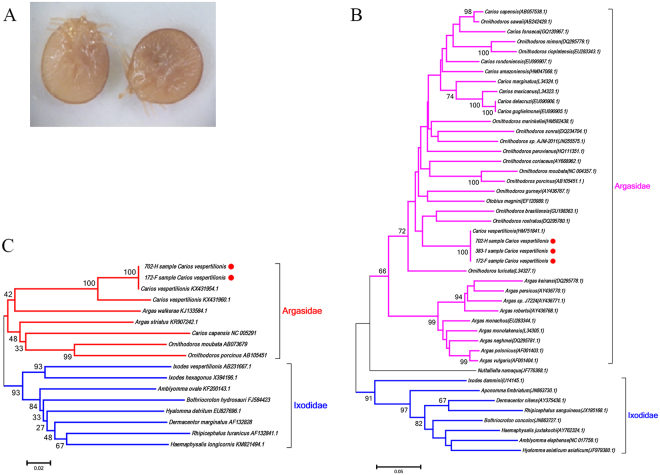
In order to assess the pathogens associated with UK bats, ectoparasites were collected from 62 infested bats submitted to APHA between 2007 and 2013 (total submissions were 7,606). The bat species were identified as Myotis daubentonii (n = 8), Pipistrellus pipistrellus (n = 38), Plecotus auritus (n = 5), Myotis natteri (n = 2), Eptesicus serotinus (n = 1), Myotis mystacinus (n = 3), Nyctalus noctula (n = 2) and Rhinolophus hipposideros (n = 2) (Supplementary Table S1). The species of one bat could not be determined due to carcass decomposition. The locations from where bats were submitted are shown in Fig. 1. A total of 296 ticks were removed from 26 bats and identified as larvae of A. vespertilionis based on morphology (Fig. 2A). Phylogenetic analyses using sequences derived from the cytochrome oxidase subunit I (COI) and 16 S ribosomal RNA (rRNA) confirmed this designation (Fig. 2B,C). No other tick species were identified in this study. Hundreds of bats were submitted from Scotland, and five were infested with ectoparasites but not ticks (Supplementary Table S1, Fig. 1). Of the nine species of bats included in the study, P. pipistrellus, Pl. auritus, and M. daubentonii were hosts of A. vespertilionis (Table 1).
Figure 1.
Map of Great Britain showing locations where bats were submitted and the ectoparasites sampled. The collection sites for bat ticks are marked with yellow dots, for other parasites such as fleas and mites with black dots. Numbers in yellow or black dots indicate the number of bats sampled from each county. This figure is not included in the Creative Commons licence for the article; all rights reserved. Taken from the Beijing Zcool Internet Technology Co., Ltd.
Figure 2.
Species identification of bat ticks through morphology and Neighbor Joining phylogenetic analyses based on COI and 16S rRNA. (A) A representative image of bat ticks removed from a UK bat. (B) Neighbor Joining phylogenetic analysis based on partial tick 16S rRNA sequence, (C) Neighbor Joining phylogenetic analysis based on partial tick COI sequence. Bootstrap values are indicated at the nodes. Scale bar indicates the degree of divergence represented by a given length of branch. The red dots indicate the sequences acquired in this study.
Table 1.
Summary of ticks collected from UK bats between 2007 and 2013.
| Tick | Bat species (number of ticks per number of bats) | |||||||
|---|---|---|---|---|---|---|---|---|
| Species | Pipistrellus pipistrellus | Plecotus auritus | Myotis daubentonii | Myotis nattereri | Eptesicus serotinus | Myotis mystacinus | Nyctalus noctula | Rhinolophus hippsideros |
| Argas vespertilions | 267/36 | 23/5 | 6/8 | 0/2 | 0/1 | 0/3 | 0/2 | 0/2 |
Detection of piroplasms in bat ticks
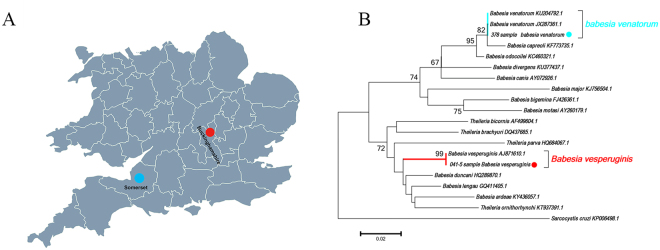
DNA sequences of piroplasms were detected in three bat ticks collected from Buckinghamshire and Somerset (Table 2, Fig. 3A). DNA sequence analysis of the amplicons derived from two A. vespertilionis removed from bat 041/2008 submitted from Buckinghamshire showed 100% identity with B. vesperuginis (AJ871610). A DNA sequence obtained from a bat tick removed from a Pl. auritus bat from Somerset (378/2013) shared 99% identity with B. venatorum (KU204792) and 98% with B. capreoli (KF773735). Phylogenetic analysis based on a partial sequence of 18 S rRNA (Fig. 3B) confirmed that the Babesia sequence derived from bat 041/2008 clustered with B. vesperuginis sequences while the Babesia sequence obtained from bat 378/2013 clustered with a clade including both B. venatorum (KU204792, JX287361) and B. capreoli (KF773735).
Table 2.
Molecular analyses of bat ticks for the presence of piroplasms.
| Tick species | Piroplasm positive/all analysed ticks | Results of sequencing (length, % identity, sample number) | Bat hosts | Locations of piroplasm positive ticks |
|---|---|---|---|---|
| Argas vespertilionis | 3/120 | Babesia vesperuginis (426 bp, 99%, 2) | Pipistrellus pipistrellus | Buckinghamshire |
| Babesia venatorum (426 bp, 99%, 1) | Plecotus auritus | Somerset |
Figure 3.
Detection and analysis of piroplasm DNA detected in ticks removed from UK bats. (A) Map showing the sampling sites of piroplasm-positive bat ticks. The red dot indicates the site of B. vesperuginis positive A. vespertilionis and the blue dot indicates the site of B. venatorum positive A. vesperitilionis. This figure is not included in the Creative Commons licence for the article; all rights reserved. Taken from Beijing Zcool Internet Technology Co., Ltd. (B) Neighbor Joining phylogenetic analysis based on partial 18S rRNA sequence of Babesia spp. Bootstrap values are indicated at the nodes. Scale bar indicates the degree of divergence represented by a given length of branch. The red dot indicates the sequence of B. vesperuginis and the blue dot indicates the sequence of B. venatorum acquired in this study.
Detection of Rickettsia spp
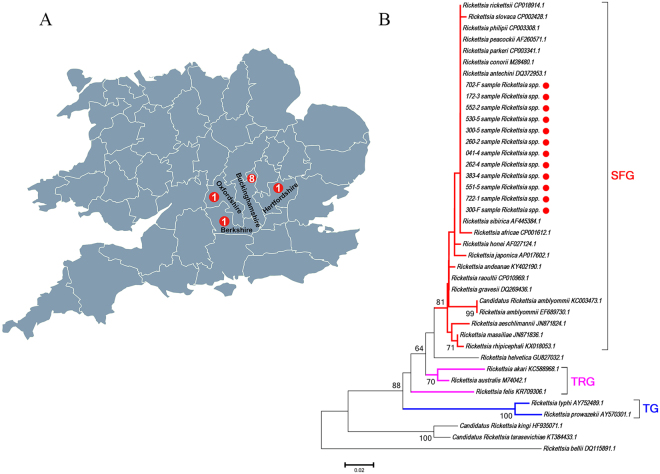
In previous reports, SFG Rickettsiae spp. such as R. helvetica and R. raoultii were detected in I. ricinus, Haemaphysalis punctata and D. reticulatus ticks in England and Wales13,14. In this study, Rickettsia spp. were detected in 16 bat ticks collected from 11 bats submitted from 4 counties of England (Buckinghamshire, Oxfordshire, Hertfordshire and Berkshire) (Table 3, Fig. 4A). Fifteen A. vespertilionis were removed from 10 P. pipistrellus, while one was removed from one Pl. auritus (Table 3). DNA sequence analysis of the 16 amplicons demonstrated that they shared 100% identity with the 17 kDa protein gene of Rickettsia spp. such as Rickettsia sibirica (MF002549.1) and Rickettsia conorii (MF002513.1). A phylogenetic tree based on a partial sequence of the 17 kDa gene of representative Rickettsia is shown in Fig. 4B. This demonstrates that all the Rickettsia sequences detected in this study clustered with species in the spotted fever group (SFG) including R. conorii (M28480), R. rickettsii (CP018914), and R. africae (CP001612).
Table 3.
Molecular analyses of bat ticks for the presence of Rickettsia.
| Tick species | Rickettsia positive/all analysed ticks | Results of sequencing (length, % identity, sample number) | Bat hosts, host number | Locations of positive ticks |
|---|---|---|---|---|
| Argas vespertilionis | 16/120 | Rickettsia spp. (434 bp, 99%, 1) | Plecotus auritus, 1 | Buckinghamshire |
| Rickettsia spp. (434 bp, 99%, 11) | Pipistrellus pipistrellus, 7 | Buckinghamshire | ||
| Rickettsia spp. (434 bp, 99%, 1) | Pipistrellus pipistrellus, 1 | Oxfordshire | ||
| Rickettsia spp. (434 bp, 99%, 2) | Pipistrellus pipistrellus, 1 | Hertfordshire | ||
| Rickettsia spp. (434 bp, 99%, 1) | Pipistrellus pipistrellus, 1 | Berkshire |
Figure 4.
Detection and analysis of Rickettsia spp. from UK bat ticks. (A) Map showing the sampling sites of Rickettsia spp. positive bat ticks. The red dots indicate the sites of Rickettsia spp positive A. vespertilionis. This figure is not included in the Creative Commons licence for the article; all rights reserved. Taken from Beijing Zcool Internet Technology Co., Ltd. (B) Neighbor Joining phylogenetic analysis based on a partial sequence of the 17 K Da protein gene of Rickettsia spp. Bootstrap values are indicated at the nodes. Scale bar indicates the degree of divergence represented by a given length of branch. The red dot indicates the sequence of Rickettsia spp. acquired in this study. Numbers in red dots indicate the number of bats with Rickettsia spp. positive ticks, sampled from each county.
Detection of Ehrlichia/Anaplasma spp
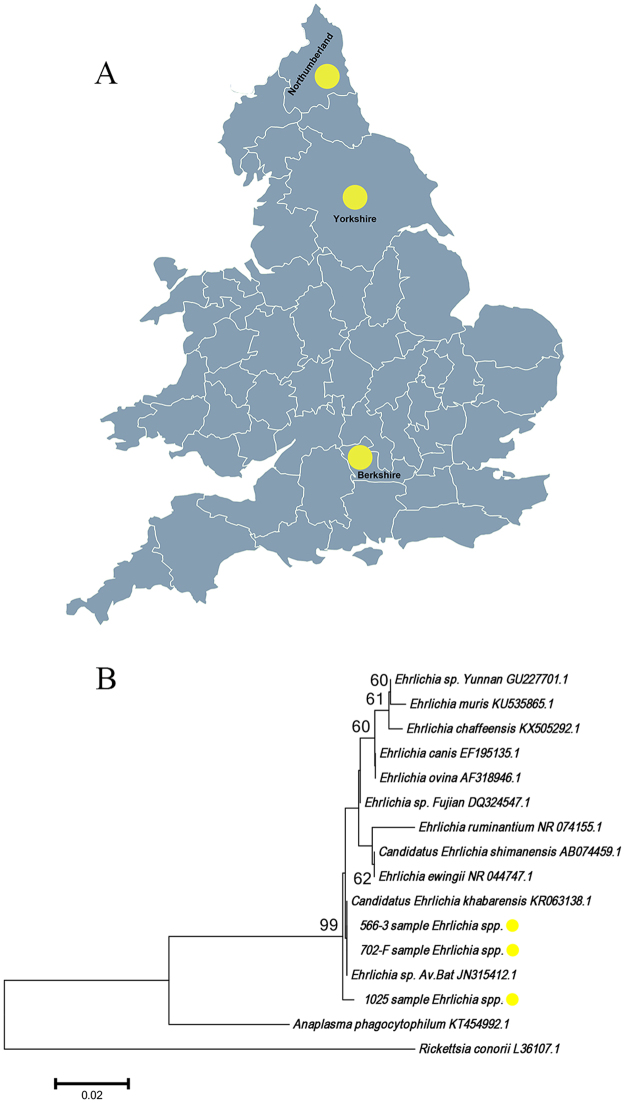
Ehrlichia canis has been detected in a dog with no history of travel outside the UK in a previous study15. In this study, DNA sequences of Ehrlichia/Anaplasma spp. were detected in 5 bat ticks collected from 3 bats (P. pipistrellus) submitted from 3 counties of England (Yorkshire, Northumberland and Berkshire) (Table 4, Fig. 5A). DNA sequence analysis of the 5 amplicons showed that they shared 99% sequence identity with the 16S rRNA of E. yunnan (GU227701.1). A phylogenetic tree based on 16S rRNA of the representative Ehrlichia/Anaplasma spp. is shown in Fig. 5B. This shows that all the Ehrlichia sequences detected in this study clustered in a clade that includes E. canis (EF195135.1) and uncultured Ehrlichia spp. (JN315412.1).
Table 4.
Molecular analyses of bat ticks for the presence of Ehrlichia.
| Tick species | Ehrlichia positive/all analysed ticks | Results of sequencing (length, % identity, sample number) | Bat hosts, host number | Locations of positive ticks |
|---|---|---|---|---|
| Argas vespertilionis | 5/120 | Ehrlichia spp. (675 bp, 99%, 1) | Pipistrellus pipistrellus, 1 | Berkshire |
| Ehrlichia spp. (675 bp, 99%, 1) | Pipistrellus pipistrellus, 1 | Northumberland | ||
| Ehrlichia spp. (675 bp, 99%, 3) | Pipistrellus pipistrellus, 1 | Yorkshire |
Figure 5.
Detection and analysis of Ehrlichia/Anaplasma spp. from UK bat ticks. (A) Map showing the sampling sites of Ehrlichia spp. positive A. vespertilionis (yellow dots). This figure is not included in the Creative Commons licence for the article; all rights reserved. Taken from Beijing Zcool Internet Technology Co., Ltd. (B) Neighbor Joining phylogenetic analysis based on a partial 16S rRNA sequence of Ehrlichia spp. Bootstrap values are indicated at the nodes. Scale bar indicates the degree of divergence represented by a given length of branch. The yellow dot indicates the sequence of Ehrlichia spp. acquired in this study.
Detection of Borrelia spp., Coxiella burnetii, Issyk-kul virus and Flaviviruses
A total of 120 A. vespertilionis were tested for the presence of Borrelia spp. and Coxiella burnetii DNA. Results were negative in all samples for these bacteria. The RNA samples prepared from 120 A. vespertilionis were screened for the presence of Issyk-kul virus and flaviviruses. All samples were also negative for these viruses.
Discussion
A range of hard ticks including I. vespertilionis, I. ariadnae, I. simplex, I. ricinus and D. reticulatus have been reported to infest bats3,16,17. I. vespertilionis and A. vespertilionis have previously been reported to be associated with bats in the UK and A. vespertilionis is believed to be widely distributed across England and the west of Scotland11. In this study, A. vespertilionis ticks were collected from 26 bat carcasses submitted from 14 counties of England (Fig. 1). P. pipistrellus, in addition to being the most abundant bat species in the UK and most commonly submitted for lyssavirus testing, was also the most commonly infested with bat ticks. This bat has been reported to host A. vespertilionis in other European studies18. The infestation rate for P. pipistrellus, Pl. auritus and M. daubentonii are separately 7.4, 11.5 and 2 per bat and generally the average for all three bat species is 7 ticks per bat. All bat ticks collected in this study were larvae and no adults or nymphs were found. In addition to ticks, we also collected other parasites such as fleas and mites (Supplementary Table S1), but these were not investigated further.
Due to the considerable lack of data in the literature concerning the zoonotic pathogens associated with bat ticks in the UK, nucleic acid extracts of 120 specimens were tested for the presence of a range of pathogens. The role of A. vespertilionis as a vector or reservoir of bacterial or protozoal pathogens in France had been reported4. B. vesperuginis DNA was identified in A. vespertilionis collected from P. pipistrellus in this study. This soft tick species has been incriminated as a vector of B. vesperuginis in Central Europe19 which has been reported to infect P. pipistrellus, several Myotis spp. (including M. daubentonii) and Pl. auritus in England12. Of particular interest was the detection of B. venatorum from one larva of A. vespertilionis infesting Pl. auritus from the county of Somerset (Fig. 3). B. venatorum is zoonotic with I. ricinus and I. simplex as vectors of this parasite. It is noteworthy that I. ricinus and I. simplex occur on bats and this suggests that bats may be carriers of this Babesia20. This suggests that A. vespertilionis is a potential host of B. venatorum in addition to the genus Ixodes, and that Pl. auritus may be infected with B. venatorum. As A. vespertilionis is the most common bat tick worldwide and is known to bite humans21,22, it could potentially transmit B. venatorum to humans as this is a known zoonotic pathogen23. Alternatively, these Argasid ticks are positive for Babesia through contact with infected bats and are not biological vectors.
Species in the genus Rickettsia are separated into three groups: The first, an ancestral group containing R. felis; A second, the typhus group (TG) which includes the agent of louse-borne epidemic typhus, R. prowazekii, and the agent of flea-borne murine typhus, R. typhi; Finally a third, the SFG, whose members are associated mainly with ticks24,25. Based on phylogenetic analysis of a partial sequence of the 17 kDa protein, we have demonstrated that the Rickettsia spp. detected in A. vespertilionis from the UK can be classified within the SFG Rickettsia. The result is consistent with the findings of Socolovschi and co-workers, who showed that Rickettsia spp. within the SFG were detected from 3 of 5 A. vespertilionis collected from a human dwelling in France4. In our study, all of the A. vespertilionis ticks in which Rickettsia spp. were detected were obtained from bats submitted from four adjacent counties, all located in southern England. Tick-borne Rickettsia spp. within the SFG are associated with several human diseases in Europe including Rickettsia conorii conorii, the agent of Mediterranean spotted fever (MSF), R. conorii israelensis (Israeli spotted fever); R. slovaca and R. raoultii agents of tick-borne lymphadenopathy (TIBONEL)26,27. SFG Rickettsia such as R. helvetica and R. raoultii have been detected in I. ricinus and D. reticulatus ticks in the UK13. However, no human cases of infection with Rickettsia spp. have been reported.
The presence of Ehrlichiae spp. DNA was detected in A. vespertilionis collected from three bats in this study. Ehrlichia/Anaplasma spp. DNA has been detected from A. vespertilionis in France4 and the sequence similarity between Ehrlichia sp. Av bat of France and the Ehrlichia spp. detected in this study is over 99.5%. The species and pathogenicity of Ehrlichia spp. detected in the UK requires further investigation.
A single larva of A. vespertilionis was found attached to a dead bat infected with a Borrelia spp. in the UK and A. vespertilionis may be the source of infection28. Also, Borrelia sp.CPB1 was detected from the A. vespertilionis in France4. In 1966, Coxiella burnetii, the agent of Q fever, was detected in A. vespertilionis collected from southern Kazakhstan29. Coxiella burnetii has been reported in livestock populations of England and Wales30. These findings suggest that A. vespertilionis ticks from UK may be the vectors or reservoirs for Borrelia spp. and Coxiella burnetii. However, neither of these pathogens was detected from the 120 A. vespertilionis collected from bats in this study suggesting that A. vespertilionis ticks in UK may not be a common host for Borrelia spp. and Coxiella burnetii until further evidence is found.
Evidence for the role of A. vespertilionis as vectors or reservoirs of viral pathogens is limited. In 1973, Issyk-Kul virus, assigned to the Bunyaviridae family, was isolated from bats (Nyctalus noctula, Myotis blythi and Vespertilio serotinus) and A. vespertilionis in Kyrgyzstan31. Recently, a novel Bunyavirus was isolated from A. vespertilionis in Japan, sharing between 76 and 79% identity with Issyk-Kul virus32. A number of viruses belonging to genus Flavivirus has been isolated from bats and this suggests that bat ticks have the potential to be vectors for flaviviruses33,34. In this study we screened 120 bat ticks of UK origin for both Issyk-Kul virus and flaviviruses. We were unable to demonstrate the presence of these viruses from this cohort. Potential reasons for this include true absence of virus from this tick population although the sample size was relatively small. Alternatively, more sensitive means of detection might be required or the samples experienced degradation of nucleic acid during storage prior to testing.
In conclusion, we have detected a range of potential pathogens in ticks associated with British bats. Previous reports have indicated that A. vespertilionis can bite humans. This suggests that they are a potential source of pathogens for those that have close contact with bats, particularly the common pipistrelle, could be at risk of exposure and re-emphasizes the need for bat handlers to wear appropriate personal protective equipment such as gloves to avoid exposure to both bat-borne and tick-borne pathogens.
Materials and Methods
Ectoparasite collection and identification
Bat carcasses were submitted to the Animal and Plant Health Agency as part of passive surveillance for lyssaviruses from 2007 to 2013, in particular for European Bat Lyssavirus type 2 (EBLV-2), which has previously been detected in the UK35. Bat speciation was based on morphology and the locations and dates of submission recorded. Ectoparasites (ticks, mites and fleas) were removed from each carcass from a total number of 7606 bats submitted to APHA between 2007 and 2013. These were immediately stored in 75% ethanol at room temperature. Morphological identification of ectoparasites was achieved through examination using a stereo microscope (SDZ-PL, Kyowa Instruments, Japan) with reference to standard morphological keys36.
Nucleic acid extraction
One hundred and twenty ticks were dried, and then washed three times with distilled water. All ticks were bisected with disposable scalpels; one half utilized for DNA extraction and the other half utilized for RNA extraction. DNA was extracted with the DNeasy Blood & Tissue kit (QIAGEN, Hilden, Germany) according to the manufacturer’s instructions. DNA was eluted in 80 μL elution buffer AE (provided with kit) and stored at −80 °C until tested. RNA was extracted with the RNeasy mini kit (QIAGEN, Hilden, Germany) according to the manufacturer’s instructions. RNA was eluted in 60 μl of RNase-free water (provided with kit) and stored at −80 °C until tested.
Molecular identification of tick species
Sequences of the 16S rRNA and COI genes were amplified by PCR using the primers listed in supplementary Table S2. PCR amplification was carried out using GoTaq G2 Flexi DNA polymerase (Promega, WI, USA). The reaction master mix was prepared according to the manufacture’s protocol and the PCR conditions described in previous studies were used37,38. All PCRs were run with positive and negative controls. PCR products were separated using gel electrophoresis in 1% agarose gels, stained with SYBR Safe DNA Gel Stain (Invitrogen, CA, USA) and visualized under ultra-violet light.
Detection of DNA pathogens
All primer sequences are provided in supplementary Table S2. Piroplasms were detected using primers PIROA and PIROB39. Rickettsia spp. were detected using a nested set of primers targeting the gene sequence of the 17 kDa protein40. Ehrlichia/Anaplasma spp. were detected using a hemi-nested primer set targeting the 16 S rRNA gene41. Borrelia spp. were detected using a primer pair that targeted the flagellin gene42. Coxiella burnetti was detected using a primer pair targeting the Cb IS 1111 element43. The reaction master mix was prepared according to the manufacture’s protocol and the PCR conditions described in previous studies were used.
Detection of RNA viruses
Reverse transcription was carried out with M-MLV reverse transcriptase (Promega, WI, USA) in a reaction volume of 40 μL, which included 18 μL of extracted RNA, 8 μL 5× RT buffer, 2 μL dNTP (10 mM), 3 μL DTT (0.1 M), 4 μL M-MLV reverse transcriptase (200 U/μL), 1 μL RNasin (40 U/μL), 2 μL 10× hexanucleotide mix, and 2 μL molecular grade water.
Detection of Flavivirus RNA was attempted using the hemi-nested -PCR targeting the RNA-dependent RNA polymerase gene, as described previously44. In brief, 5 μL cDNA was utilized as template for each reaction. The reaction master mix was prepared according to the manufacture’s protocol and the PCR conditions described in previous studies were used.
Detection of the Nairovirus, Issyk-Kul virus, was attempted using a hemi-nested PCR targeting the S segment of the virus genome using primers described in supplementary Table S2. After denaturation at 95 °C for 2 minutes (min), the reactions were cycled 45 times at 95 °C for 30 seconds (s), 50 °C for 30 s, and 72 °C for 50 s, followed by an elongation step at 72 °C for 7 min, finally the reactions were cooled down to 4 °C. The hemi-nested PCR reaction utilized 1 μl of the first PCR product as template with primers BUNV-F2/BUNV-R2 (Table S2). After denaturation at 95 °C for 2 min, the reactions were cycled 45 times at 95 °C for 30 s, 60 °C for 30 s, and 72 °C for 40 s, followed by an elongation step at 72 °C for 7 min, finally the reactions were cooled to 4 °C.
Sequence Analysis
DNA amplicons of the correct size were purified and sequenced as previously described39. Representative sequences were submitted to GenBank (supplementary Table S3). DNA sequences were assembled using Lasergene version 12.1 (DNASTAR) and edited in MEGA 5.045. Sequence alignments were conducted using ClustalW within MEGA 5.0, using default parameters (open gap penalty = 10.0, extend gap penalty = 5.0) before subsequently being checked by visual inspection. Genetic distances were calculated based on the K2P model for all pair-wise comparisons in the matrix using MEGA46. Bootstrapping (1000 replicates) was utilized to estimate node support. Pairwise deletion was used for gaps/missing data. Based on K2P distances, phylogenetic trees were constructed with the combined data sets of all major tick genera using the Neighbor-Joining method. For COI analysis, all codon positions and non-codon sites were tested combined.
Data availability
All data discussed in the manuscript is included in the paper.
Electronic supplementary material
Acknowledgements
This study was funded by the national science and technology support programs of China (Grant numbers: 2016YFD0501100, 2013BAD12B00). Testing for this study was funded by the UK Department for Environment, Food and Rural Affairs (Defra), the Scottish and Welsh Governments through grant SV3045. The authors would like to acknowledge the support of the Bat Conservation Trust in supporting surveillance in bats.
Author Contributions
N.J. and L.M.M. conceived the idea, J.L., M.M.F.M., H.G., L.P.P., L.M.H.T., performed the study, S.W., X.L., A.R.F., obtained funding for the study. All authors wrote and agreed the final version.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-20138-1.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Helversen, O.V., Nill, D. & Dietz, C. Bats of Britain, Europe and Northwest Africa. Bloomsbury Specialist (2009).
- 2.Calisher CH, Childs JE, Field HE, Holmes KV, Schountz T. Bats: important reservoir hosts of emerging viruses. Clin Microbiol Rev. 2006;19:531–545. doi: 10.1128/CMR.00017-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hornok S, et al. DNA of piroplasms of ruminants and dogs in Ixodid bat ticks. PLoS One. 2016;11:e0167735. doi: 10.1371/journal.pone.0167735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Socolovschi, C., Kernif, T., Raoult, D. & Parola, P. Borrelia, Rickettsia, and Ehrlichia species in bat ticks, France, 2010. Emerg Infect Dis. 18, 1966–1975 (2012). [DOI] [PMC free article] [PubMed]
- 5.Krauel JJ, LeBuhn G. Patterns of bat distribution and foraging activity in a highly urbanized temperate environment. PLoS One. 2016;11:e168927. doi: 10.1371/journal.pone.0168927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de la Fuente, J. et al. Tick-pathogen interactions and vector competence: Identification of molecular drivers for tick-borne diseases. Front Cell Infect Microbiol. 7, 114 (2017). [DOI] [PMC free article] [PubMed]
- 7.Dantas-Torres F, et al. Description of a new species of bat-associated argasid tick (Acari: Argasidae) from Brazil. J Parasitol. 2012;98:36–45. doi: 10.1645/GE-2840.1. [DOI] [PubMed] [Google Scholar]
- 8.Durden LA, Beckman KB, Gerlach RF. New records of ticks (Acari: Ixodidae) from dogs, cats, humans and some wild vertebrates in Alaska: invasion potential. J Med Entomol. 2016;53:1391–1395. doi: 10.1093/jme/tjw128. [DOI] [PubMed] [Google Scholar]
- 9.Jameson LJ, Medlock JM. Tick surveillance in Great Britain. Vector Borne Zoonotic Dis. 2011;11:403–412. doi: 10.1089/vbz.2010.0079. [DOI] [PubMed] [Google Scholar]
- 10.Jaenson TGT, et al. Geographical distribution, host association, and vector roles of ticks (Acari: Ixodidae, Argasidae) in Sweden. J. Med. Entomol. 1994;31:240–258. doi: 10.1093/jmedent/31.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hubbard MJ, Baker AS, Cann KJ. Distribution of Borrelia burgdorferi s.l. spirochaete DNA in British ticks (Argasidae and Ixodidae) since the 19th century, assessed by PCR. Med Vet Entomol. 1989;12:89–97. doi: 10.1046/j.1365-2915.1998.00088.x. [DOI] [PubMed] [Google Scholar]
- 12.Gardner RA, Molyneux DH. Babesia vesperuginis: natural and experimental infections in British bats (Microchiroptera) Parasitology. 1987;95:461–469. doi: 10.1017/S0031182000057887. [DOI] [PubMed] [Google Scholar]
- 13.Tijsse_Klasen E, et al. First detection of spotted fever group Rickettsiae in Ixodes ricinus and Dermacentor reticulatus ticks in the UK. Epidemiol Infect. 2011;139:524–529. doi: 10.1017/S0950268810002608. [DOI] [PubMed] [Google Scholar]
- 14.Tijsse-Klasen E, et al. Spotted fever group rickettsiae in Dermacentor reticulatus and Haemaphysalis punctata ticks in the UK. Parasit Vectors. 2013;6:212. doi: 10.1186/1756-3305-6-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson HE, Mugford AR, Humm KR, Kellett-Gregory LM. Ehrlichia canis infection in a dog with no history of travel outside the United Kingdom. J Small Anim Pract. 2013;54:425–427. doi: 10.1111/jsap.12088. [DOI] [PubMed] [Google Scholar]
- 16.Hornok S, et al. Contributions to the morphology and phylogeny of the newly discovered bat tick species, Ixodes ariadnae in comparison with I. vespertilionis and I. simplex. Parasit Vectors. 2015;8:47. doi: 10.1186/s13071-015-0665-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burazerovic J, et al. Ticks (Acari: Argasidae, Ixodidae) parasitizing bats in the central Balkans. Exp Appl Acarol. 2015;66:281–291. doi: 10.1007/s10493-015-9891-6. [DOI] [PubMed] [Google Scholar]
- 18.Hornok S, et al. High degree of mitochondrial gene heterogeneity in the bat tick species Ixodes verspertilionis, I. ariadnae and I. simplex from Eurasia. Parasit Vectors. 2015;8:457. doi: 10.1186/s13071-015-1056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hornok S, et al. Molecular investigations of the bat tick Argas vespertilionis (Ixodida: Argasidae) and Babesia vesperuginis (Apicomplexa: Piroplasmida) reflect “bat connection” between Central Europe and Central Asia. Exp Appl Acarol. 2017;72:69–77. doi: 10.1007/s10493-017-0140-z. [DOI] [PubMed] [Google Scholar]
- 20.Venclikova K, Mendel J, Betasova L, Hubalek Z, Rudolf I. First evidence of Babesia venatorum and Babesia capreoli in questing Ixodes ricinus ticks in the Czech Republic. Ann Agric Environ Med. 2015;22:212–214. doi: 10.5604/12321966.1152067. [DOI] [PubMed] [Google Scholar]
- 21.Wilhelmsson P, et al. Ixodes ricinus ticks removed from humans in Northern Europe: seasonal patterns of infestation, attachment sites and duration of feeding. Parasit Vectors. 2013;6:362. doi: 10.1186/1756-3305-6-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Estrada-Pena A, Jongejan F. Ticks feeding on humans: a review of records on human-biting Ixodoidea with special reference to pathogen transmission. Exp Appl Acarol. 1999;23:685–715. doi: 10.1023/A:1006241108739. [DOI] [PubMed] [Google Scholar]
- 23.Jiang JF, et al. Epidemiological, clinical, and laboratory characteristics of 48 cases of “Babesia venatorum” infection in China: a descriptive study. Lancet Infect Dis. 2015;15:196–203. doi: 10.1016/S1473-3099(14)71046-1. [DOI] [PubMed] [Google Scholar]
- 24.Brouqui P, Parola P, Fournier PE, Raoult D. Spotted fever rickettsioses in southern and eastern Europe. FEMS Immunol Med Microbiol. 2007;49:2–12. doi: 10.1111/j.1574-695X.2006.00138.x. [DOI] [PubMed] [Google Scholar]
- 25.Punda-Polic V, et al. Detection and identification of spotted fever group rickettsiae in ticks collected in southern Croatia. Exp Appl Acarol. 2002;28:169–176. doi: 10.1023/A:1025334113190. [DOI] [PubMed] [Google Scholar]
- 26.Parola P, Paddock CD, Raoult D. Tick-borne rickettsioses around the world: emerging diseases challenging old concepts. Clin Microbiol Rev. 2005;18:719–756. doi: 10.1128/CMR.18.4.719-756.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parola P, et al. Rickettsia slovaca and R. raoltii in tick-borne Rickettsioses. Emerg Infect Dis. 2009;15:1105–1108. doi: 10.3201/eid1507.081449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans NJ, Bown K, Timofte D, Simpson VR, Birtles RJ. Fatal borreliosis in bat caused by relapsing fever spirochete, United Kingdom. Emerg Infect Dis. 2009;15:1331–1333. doi: 10.3201/eid1508.090475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhmaeva ZM, Pchelkina AA, Belashova VS. [Spontaneous infection of Argas vespertilionis with Rickettsia burnetii in the south of Kazakhstan] Med Parazitol. 1966;35:595–596. [PubMed] [Google Scholar]
- 30.Jones RM, et al. Detection of Coxiella burnetii in placenta and abortion samples from British ruminants using real-time PCR. Vet Rec. 2010;167:965–967. doi: 10.1136/vr.c4040. [DOI] [PubMed] [Google Scholar]
- 31.Lvov DK, et al. “Issyk-Kul” virus, a new arbovirus isolated from bats and Argas (Carios) vespertilionis (Latr, 1802) in the Kirghiz S.S.R. Brief report. Arch Gesamte Virusforsch. 1973;42:207–209. doi: 10.1007/BF01270841. [DOI] [PubMed] [Google Scholar]
- 32.Oba et al. A novel Bunyavirus from the soft tick, Argas vespertilionis in Japan. J Vet Med Sci. 78, 443–445. [DOI] [PMC free article] [PubMed]
- 33.de Lamballerie X, et al. Genome sequence analysis of Tamana bat virus and its relationship with the genus Flavivirus. J Gen Virol. 2002;83:2443–2454. doi: 10.1099/0022-1317-83-10-2443. [DOI] [PubMed] [Google Scholar]
- 34.Tajima S, Takasaki T, Matsuno S, Nakayama M, Kurane I. Genetic characterization of Yokose virus, a flavivirus isolated from the bat in Japan. Virology. 2005;332:38–44. doi: 10.1016/j.virol.2004.06.052. [DOI] [PubMed] [Google Scholar]
- 35.Wise, E. L. et al. Passive surveillance of United Kingdom bats for lyssaviruses (2005–2015). Epidemiol Infect. 145, 2445–2457 (2017). [DOI] [PMC free article] [PubMed]
- 36.Hillyard, P. S. Argas (Carios) vespertilionis (Latreille, 1802) in Ticks of North-West Europe. 142–3 (Field Studies Council, 1996).
- 37.Krakowetz CN, Dergousoff SJ, Chilton NB. J Vector Ecol. 2010. Genetic variation in the mitochondrial 16S rRNA gene of the American dog tick, Dermacentor variabilis (Acari: Ixodidae) pp. 163–173. [DOI] [PubMed] [Google Scholar]
- 38.Folmer O, Black M, Hoeh W, Lutz R, Vrijenhoek R. DNA primers for amplification of mitochondrial cytochrome c oxidase subunit I from diverse metazoan invertebrates. Mol Mar Biol Biotechnol. 1994;3:294–299. [PubMed] [Google Scholar]
- 39.Fernández de Marco M, et al. Emergence of Babesia canis in southern England. Parasit Vectors. 2017;10:241. doi: 10.1186/s13071-017-2178-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anstead CA, Chilton NB. A novel Rickettsia species detected in Vole Ticks (Ixodes angustus) from Western Canada. Appl Environ Microbiol. 2013;79:7583–7589. doi: 10.1128/AEM.02286-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Teshale S, et al. Molecular detection of Anaplasma species in questing ticks (Ixodids) in Ethiopia. Asian Pac J Trop Dis. 2016;6:449–452. doi: 10.1016/S2222-1808(16)61066-6. [DOI] [Google Scholar]
- 42.Park HS, et al. Evaluation of groEL gene analysis for identification of Borrelia burgdorferi sensu lato. J Clin Microbiol. 2004;42:1270–1273. doi: 10.1128/JCM.42.3.1270-1273.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Capuano F, Proroga YTR, Mancusi A, Perugini AG, Berri M. Evaluation of DNA preparation methods combined with different PCR-based assays for Coxiella burnetii detection in milk. Large Anim Rev. 2016;22:59–62. [Google Scholar]
- 44.Abdel-Shafy S, Allam NAT. Quantitative real-time RT-PCR detection of flaviviruses associated with camel ticks in Egypt. Global Veterinaria. 2013;10:394–402. [Google Scholar]
- 45.Tamura K, et al. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aliabadian M, Kaboli M, Nijman V, Vences M. Molecular identification of birds: performance of distance-based DNA barcoding in three genes to delimit parapatric species. PLoS One. 2009;4:e4119. doi: 10.1371/journal.pone.0004119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data discussed in the manuscript is included in the paper.