Abstract
Background: There is a need to develop interventions that address the entire family after spinal cord injury (SCI), especially in Latin America, where rehabilitation resources are limited and little is known about family adjustment to SCI. Objective: To evaluate the short-term (post-intervention) and longer term (6-month) effectiveness of the newly developed, 8-session manualized family intervention for individuals with SCI and their family members compared to a control group. Methods: In this clinical demonstration project, longitudinal self-report data were collected from 8 individuals with SCI and their family members in Colombia, South America. The 8 families were randomly assigned to either the SCI intervention group or the waitlist control group. The intervention group included 10 individuals from 4 different families, with a mean age of 41.40 years (SD = 14.18). The control group was composed of 13 individuals from 4 different families with a mean age of 44.38 years (SD = 14.76). All participants completed Spanish versions of instruments that assessed depression (Patient Health Questionnaire-9), anxiety (Generalized Anxiety Disorder-7), burden (Zarit Burden Interview), and perceived problem-solving skills (Problem-Solving Inventory). Results: Results provide preliminary evidence that symptoms of depression, anxiety, and burden as well as problem-solving appraisals improved significantly for individuals who participated in the intervention, whereas no change in symptoms was observed among those in the waitlist control group. Conclusions: Findings suggest that this newly developed intervention for families facing SCI can be beneficial; however, this pilot study represents only the first step in the examination of the efficacy and effectiveness of this intervention.
Keywords: Colombia, family caregivers, intervention, mental health, spinal cord injury
Spinal cord injury (SCI) results in physical problems that can impair functional independence1 and engagement in daily physical activity2 and increase emotional difficulties, such as depression, anxiety,3–5 anger, and suicidality6 in the injured individuals. These sequelae create substantial life changes not only for individuals with SCI, but also for their family members.7 For family members of individuals with SCI, assuming a caregiving role can be associated with an increased sense of anxiety, emptiness, loneliness8; higher rates of depression4,9–11; poorer health-related quality of life12; and high levels of burden.13 It is crucial that interventions be developed that provide caregivers with ongoing support and care.14 Unfortunately, to our knowledge, few such interventions have been published.
Caregiver problem-solving skills have been one area of intervention focus. Elliott and colleagues developed a brief problem-solving training and psychoeducation intervention, which has been tested separately in both in-person15 and videoconference16 formats. Both administration formats demonstrated an ability to reduce dysfunctional caregiver problem-solving styles. No significant changes were observed in caregiver depression and social and physical functioning.15,16
Two other interventions with different emphases have also been developed. First, an adaptation of multiple-family group therapy for individuals with SCI and/or traumatic brain injury (TBI) and their caregivers demonstrated a reduction in caregiver burden, but no impact on depression, anger, quality of life, social support, or coping.17 Second, Schulz and colleagues13 reported that caregivers enrolled in a group that targeted both the individual with SCI and their caregivers that was designed to provide knowledge and cognitive/behavioral skills to reduce stress, improve health, and improve emotional well-being demonstrated clinically significant improvements in quality of life, depression, burden, and health symptoms as compared to caregivers in a comparable caregiver-only group or information-only control group.
These 4 interventions, 2 of which are administration variations of the problem-solving training, offer promising results. Three of them13,15,16 were evaluated via a randomized clinical trial, with all but the adaptation of multiple-family group therapy including control groups. However, there are gaps in the limited intervention research. Apart from Schulz and colleagues,13 who had a follow-up 6 months after the conclusion of their intervention, in the other 3 studies, the researchers did not assess whether the effects of the interventions extended past the conclusion of treatment. All 4 studies were directed at caregivers only or at patient-caregiver dyads; none included additional family members. Interventions that include as many family members as possible, and thus target the family as a system, might result in more improvements.
Additionally, the majority of intervention research has been carried out in North America or Western Europe. Intervention research on caregivers or family members of individuals with SCI in Latin America is scant.18 Results of studies utilizing samples of Latino individuals with SCI and their family members living in the United States suggest that cultural differences contribute to unique aspects of recovery. For example, strong biases exist against individuals with disability in Mexican-American culture as well as strong family, gender, and sex roles that are associated with increased anger, depression, and substance abuse during the first few years after SCI.19 Strengths of Latino culture include the importance of the nuclear and extended families in supporting recovery and rehabilitation19 and a strong sense of duty or obligation to care for loved ones at home, despite expected negative health consequences to the caregivers related to the physical demands of caregiving.6
There is a pointed need to develop interventions that address the entire family after SCI, especially in Latin America, where rehabilitation resources are limited and little is known about family adjustment to SCI. Therefore, the purpose of the proposed study was to evaluate the short-term (post intervention) and longer term (6 month) effectiveness of the newly developed, 8-session manualized family intervention for individuals with SCI and their family members compared to a control group across the areas of depression, anxiety, burden, and perceived problem-solving skills.
Method
Participants
Individuals with SCI and their family members were recruited from the Foundation for the Integral Development of People with Disabilities, a nonprofit organization that assists individuals with a variety of physical disabilities who are living in Neiva, Colombia. Individuals with SCI met the following inclusion criteria: (a) at least 18 years of age, (b) willing to participate with their family members in the intervention, (c) signed an informed consent form and release of medical records giving permission to obtain demographic and health information, (d) discharged from hospitalization for SCI at least 6 months prior, (e) fully oriented, exhibited no language or thought process issues, and able to follow commands, and (f) able to read and write.
Family members of the person with SCI met the following inclusion criteria: (a) at least 18 years of age, (b) signed an informed consent form, (c) related by blood or marriage and/or a close friend of the individual with SCI, (d) living in the household with the individual with SCI, and (e) able to read and write.
Families were excluded from this study if (a) an individual with SCI received primary care from a professional caregiver or other individual who lived outside of the household; (b) any family member, other than the individual with SCI, required professional care or close supervision for another illness; (c) any family member had a history of violence or physical abuse in the household, serious psychiatric or neurologic illness, active learning disability, aphasia, anosognosia (deficit of self-awareness), or active substance abuse; and (d) the individual with SCI lived alone.
Eight families were randomly assigned to either the SCI intervention or the waitlist control group. These families lived in rural areas, had no access to psychological or rehabilitation services after discharge from hospital, did not have a method of transportation, and lacked access to accessible equipment. See Table 1 for the composition of each family in both groups. The intervention group was comprised of 10 individuals from 4 different families. The mean age was 41.40 years (SD = 14.18). Close to half (4) were single, and half were male. Education levels varied, with 4 having some elementary school, 1 having completed elementary school, 1 having some high school, 3 having completed high school, and 1 having some bachelor's-level education. The majority (7) lived in extreme poverty, earning less than the minimum monthly wage (minimum monthly wage in Colombia is the equivalent of $210 US), whereas 3 had a monthly income that was 1 to 2 times higher than the minimum wage.
Table 1.
Family composition of intervention versus control groups
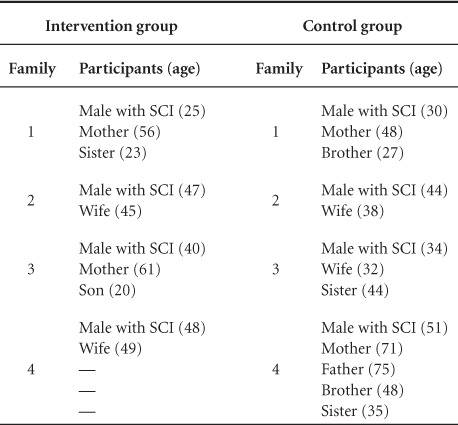
The control group was composed of 13 individuals from 4 different families. Mean age was 44.38 years (SD = 14.76). A little over half (7) were single, and 7 were male. Education levels varied, with 2 having completed elementary school, 3 having some high school, 1 having completed high school, 3 having completed technical training, 1 having some bachelor's-level education, 2 having an earned bachelor's degree, and 1 having an earned graduate degree. The majority (8) lived in extreme poverty, earning less than the minimum monthly wage, whereas 2 had a monthly income that was 4 to 5 times higher than the minimum wage.
Instruments
Participants completed a variety of self-report questionnaires to assess depression, anxiety, burden, and perceived problem-solving skills.
The Patient Health Questionnaire-9 (PHQ-9), a modified module of the Patient Health Questionnaire,20 was used to measure symptoms of depression among both individuals with SCI and their family members. Total scores could range from 0 to 27, with higher scores indicating higher levels of depression. Categories for symptom severity were as follows: 0–4 minimal, 5–9 mild, 10–14 moderate, 15–19 moderately severe, and 20–27 severe. The Spanish version21 used in this study is both reliable and valid in assessing depression in Spanish speakers.22,23
The Generalized Anxiety Disorder-7 (GAD-7)24 was completed by individuals with SCI and their family members as a measure of anxiety symptomatology. Total scores could range from 0 to 27, with higher scores indicating more severe anxiety symptoms. GAD-7 scores of 7 or below are considered to reflect anxiety symptoms that are not clinically significant enough to warrant diagnosis of any anxiety disorder, whereas scores of 8 or above suggest a possible anxiety disorder diagnosis. The Spanish version of this scale has shown adequate internal consistency (α = .94).25
The Zarit Burden Inventory (ZBI) was used to assess caregiver burden among family members only. This self-report questionnaire evaluates a caregiver's health condition, psychological well-being, financial situation, and social life in the context of the caregiver-patient relationship.26 Total scores can range from 0 to 88. Higher total scores indicate higher levels of caregiver distress. Additional cutoffs have been suggested as follows: scores of 0–21 reflect little or no burden, 21–40 reflect mild to moderate burden, 41–60 reflect moderate to severe burden, and 61–88 reflect severe burden. The Spanish version utilized in this study has demonstrated good construct validity and internal reliability in previous research.27
The Problem-Solving Inventory (PSI) was used to measure appraisal of personal problem-solving skills among individuals with SCI and their family members. The construct of problem-solving confidence is assessed with 11 items, approach-avoidance style is assessed with 16 items, and personal control is assessed with 5 items.28,29 All items are scored using a 6-point Likert-type scale (1 = strongly agree to 6 = strongly disagree). For each subscale, lower scores are generally considered to be more functional.29 Lower scores on the Problem-Solving Confidence subscale reflect higher levels of confidence; lower scores on the Approach-Avoidance subscale reflect a style of approaching, rather than avoiding problems; and lower scores on the Personal Control subscale reflect individuals' perceptions of their having higher personal control while dealing with their problems.30 The PSI has good internal consistency (r = .90) and test-retest reliability (r = .89).29 For the purposes of this study, one bilingual and bicultural researcher translated the PSI into Spanish. The Spanish and original English versions were compared by another bilingual and bicultural researcher, and any discrepancies between the 2 versions were resolved mutually by both researchers.
Procedure
This study was reviewed and approved by the local ethical and scientific committee, and no study procedures began without approval. Research staff reviewed records to identify individuals who had sought services for SCI between January 2010 and November 2013. A clinical professional psychologist (a licensed professional who completed a 5-year bachelor's degree in psychology from an accredited Colombian university) reviewed the medical records and identified 20 individuals with SCI who matched the inclusion/exclusion criteria of the study. The psychologist contacted eligible families and scheduled a group meeting to explain the study. Eight families agreed to participate. Of the 12 families who did not take part in the study, 6 declined participation because they lived in rural areas that were unaccessible to the research team, and the other 6 declined because the family members did not have the time to take part in all of the intervention sessions.
A random list of the families was generated and a coin flip determined whether the first family on the list would be assigned to the intervention group or the waitlist control group. In alternating fashion, each subsequent family on the list was assigned to the intervention or control group.
The intervention was delivered from November 2013 to January 2014 by a licensed psychologist who had completed a 5-year bachelor's degree in psychology. This psychologist received a 2-day in-person training from one of the co-developers of the intervention, as well as additional online consultation as needed. At this preliminary stage, no official assessment of fidelity was conducted. Another psychologist collected the assessment data from the individual with SCI and his/her family members in both groups when the intervention began (session 1), when the intervention ended (session 8), and at 6-month follow-up (8 months post baseline; June and July 2014). All 4 families began the intervention in November 2013, with each family participating separately as its own group. Data were collected from the control group families during the same time points in which the 4 intervention families completed their assessments. All participants completed all of their respective measures at each time point. All sessions and data collections for both groups took place in each family's home.
Intervention
Three of the authors (T.L., L.F.S, and J.C.A-L.) have extensive background and training in the respective areas of marriage and family therapy, cognitive-behavioral therapy, and rehabilitation psychology, with particular focus on individuals with traumatic injuries. Stemming from this group's research on traumatic injuries in Latin America and the United States of America, it was clear that most intervention development and testing has taken place outside of Latin America and that many Latin American countries lack rehabilitation resources for both injured individuals and their families. The 3 authors created this theoretically based intervention by pulling together a series of evidence-based strategies to help improve psychological functioning and well-being among Latin American families.
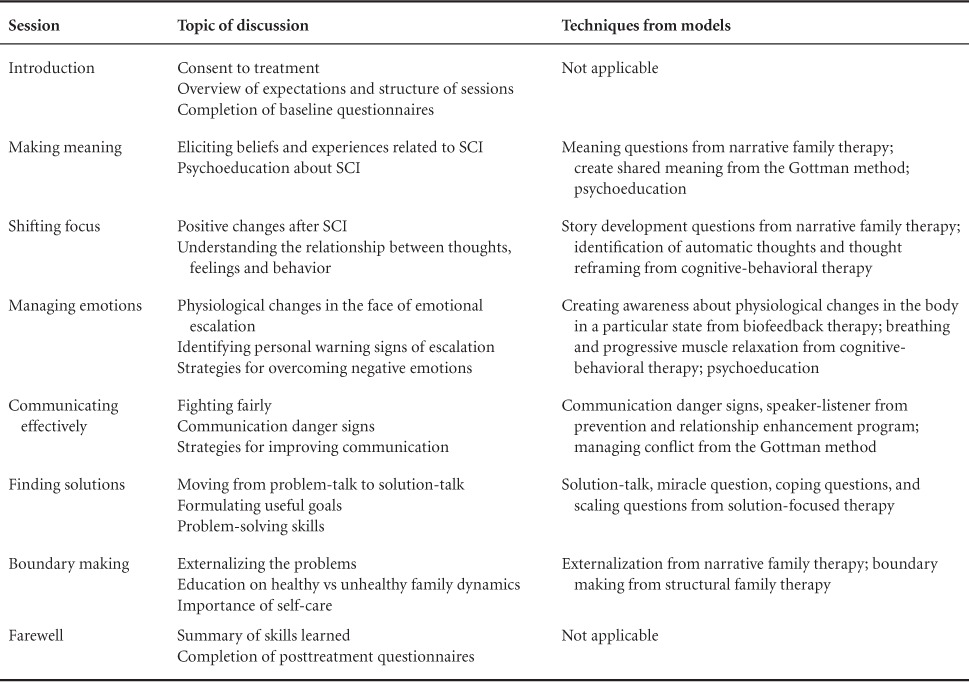
Although it was designed for use with families facing serious illness and injury in general, this intervention was originally developed for individuals with TBI and their family members to improve individual and family functioning. Strategies and elements from cognitive-behavioral therapy and family therapy, including structural family therapy, narrative therapy, and solution-focused therapy, were integrated to create a sequence of 8 weekly, 90-minute sessions that have educational and practical components related to common experiences reported by families facing TBI. The intervention was additionally adapted for use with families facing SCI by making the psychoeducational handout of session 2 specific to SCI. The content, strategies, and theoretical approach of each of the 8 sessions are summarized in Table 2. Each session begins with reflection on a quotation that is relevant to the week's topic, followed by review of the family's progress on assigned practice tasks. The majority of each session is devoted to learning background information about the topic, practicing new techniques, and applying those techniques to overcome the unique challenges that each family is facing. Each session ends with an assignment for the practice task to be completed. Though the intervention is manualized, families can apply the skills from each session to whatever issue or conflict they are facing.
Table 2.
Summary of session content, strategies, and theoretical models
The intervention was designed to be conducted in family-specific group sessions that involved both the individual with SCI and at least 2 family members. There was no limit to the number of family members who could take part in the intervention, but the family members who committed had to attend all of the sessions.
Analysis
Analyses were conducted using IBM SPSS 20.0 (2012; IBM, Inc., Armonk, NY). Demographic differences between the intervention and control groups were explored using t tests and chi-square analysis. Due to the small size in this pilot study, the distribution of scores on each test was tested for normality. The depression, anxiety, and problem-solving confidence scores were not normally distributed and could not be transformed into a normal distribution, so nonparametric tests were used to examine differences between the intervention and control groups over time. For the normally distributed data, 3 separate 2x3 repeated-measures multivariate analyses of variance (ANOVAs) with one fixed effect of treatment group (treatment group vs control group) and the repeated measures over time (baseline, post-intervention, and 6-month follow-up) were conducted; one each for burden, and appraisals of approach-avoidance problem-solving style and problem-solving personal control. For these analyses, data from individuals with SCI and their family members were treated as independent observations.
Results
Between the intervention and control groups, there were no significant differences in terms of sex, age, education, or income. Table 3 presents mean baseline scores for both groups for depression, anxiety, burden, and problem-solving appraisals as well as follow-up scores. Scores did not differ significantly between the intervention and control groups for depressive symptoms (U = 79.5, P = .38) and anxiety symptoms (U = 89.5, P = .13). The groups did differ significantly at baseline on burden among family members [t(13) = −2.99, P < .05]. Specifically, on average, participants in the intervention group endorsed a moderate to severe level of burden (M = 55.33, SD = 3.83), whereas those in the control group endorsed a mild to moderate level of burden (M = 30.67, SD = 19.75). There were no baseline differences between the intervention and control groups on problem-solving confidence (U = 92.0, P = .10), approach-avoidance [t(21) = −1.94, P = .07], or personal control [t(21) = −1.49, P = .15]. On average, scores on the Problem-Solving Confidence subscale for both groups reflected high confidence. In addition, scores on the Approach-Avoidance subscale suggested generally a style of approaching, rather than avoiding problems. Scores on the Personal Control subscale suggested positive perceptions of personal control in handling problems.
Table 3.
Mean scores (SD) for participants in both groups across 3 time points
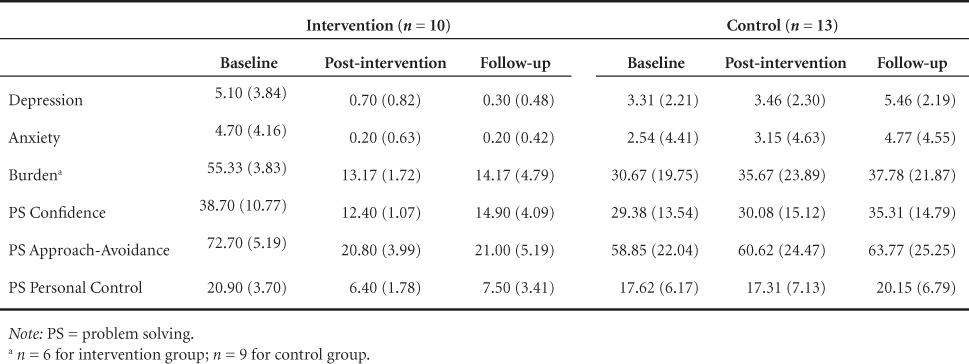
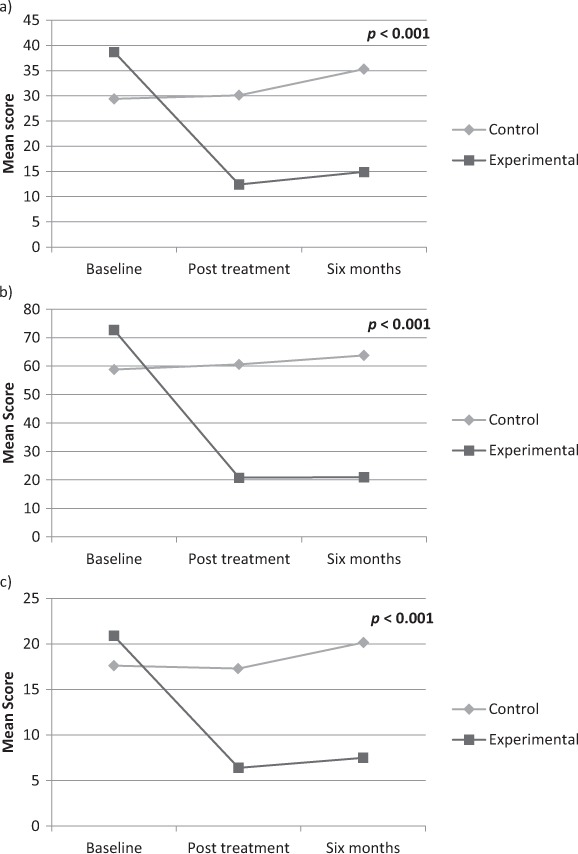
Results of the 2×3 repeated-measures ANOVAs showed a significant Group × Time interaction on burden [F(2, 26) = 199.41, P < .001, ηp2 = .94]. As seen in Figure 1, the scores in the intervention group improved significantly over time on burden, whereas the control group scores did not change significantly. Nonparametric tests were used to examine differences in depression and anxiety. The Friedman test that examines changes over time for the experimental and control groups combined showed similar scores over time for depression (Q = 3.81, P = .15) and anxiety (Q = 3.52, P = .17). The experimental group had significantly lower anxiety scores (U = 18.0, P < .01) and depression scores (U = 1.5, P < .001) at post treatment compared to the control group and significantly lower depression scores at 6 months (U = 22.0, P < .01).
Figure 1.
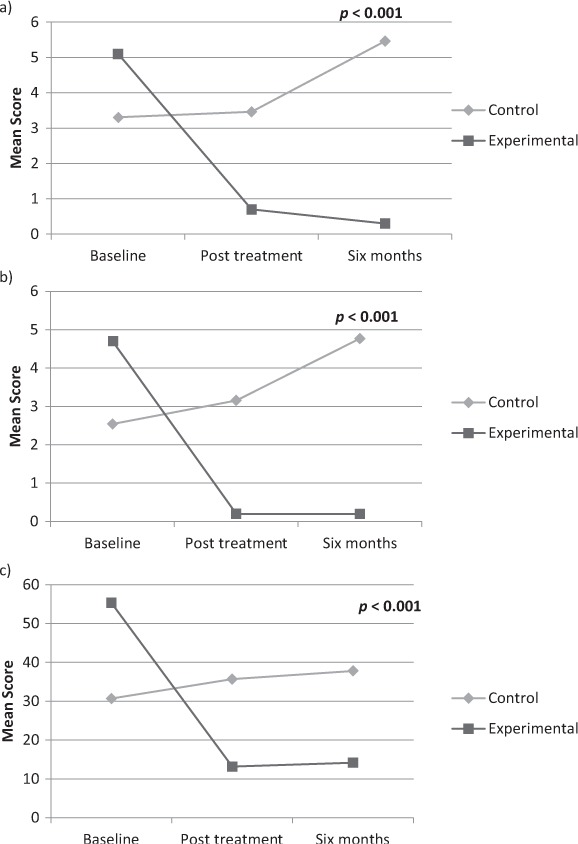
Change in mental health scores over time for intervention versus control groups. (a) Change in depression (Patient Health Questionnaire-9) scores; (b) change in anxiety (Generalized Anxiety Disorder-7) scores; (c) change in burden (Zarit Burden Interview) scores.
Results of the 2×3 repeated-measure ANOVAs showed that significant treatment Group × Time interactions were found for the problem-solving subscales of Approach-Avoidance [F(2, 42) = 195.77, P < .001, ηp2 = .90] and Personal Control [F(2, 42) = 91.09, P < .001, ηp2 = .81]. There were significant decreases in each of these 2 PSI subscale scores in the treatment group, but not the control group for the problem-solving variables. Nonparametric tests were used to examine differences in the Confidence subscale. The Friedman test that examines changes over time for the experiment and control groups combined showed a significant decrease in scores over time (Q = 6.28, P < .05). The experimental group had significantly lower scores than the control group at post treatment (U = 7.5, P < .001) and 6 months (U = 0, P < .001). See Figure 2 for graphs of each subscale score in the treatment and control groups over time. Note that lower scores on these subscales indicate improved performance.
Figure 2.
Change in problem solving scores over time for intervention versus control groups. (a) Change in problem-solving confidence scores; (b) change in problem-solving approach or avoidance style scores; (c) change in problem-solving personal control scores.
Discussion
The purpose of this pilot study was to evaluate the short-term and longer term effectiveness of a newly developed family intervention in a sample of individuals with SCI and their family members. Results provide preliminary evidence that symptoms of depression, anxiety, and burden as well as problem-solving appraisals improved significantly for individuals who participated in the intervention, compared to those in the waitlist control group.
It is difficult to determine how the baseline psychosocial functioning of individuals in the study sample compares to psychosocial functioning of other individuals with SCI and their family members in Colombia, South America. The present study is the first to report problem-solving appraisals among individuals with SCI and their family members in Colombia; there is only one other published study that examined psychosocial functioning among Colombian caregivers of individuals with SCI.30 In contrast to the findings of that study, no individuals with SCI or their family members in the present study endorsed clinical levels of depression or anxiety symptomatology at baseline. The low level of self-reported symptoms of depression and anxiety may be due in part because the participants' responses underrepresent true levels of depression and anxiety, due to stigma. Alternatively, as this sample was from a collectivistic culture in which family plays such an important role, the participants may have experienced high levels of social support that attenuated any depressive or anxious symptoms.
The caregivers in this study did endorse moderate levels of burden, which is in line with the findings of Arango-Lasprilla and colleagues.30 Additionally, there were baseline group differences in level of burden among family members. Even though there were no significant differences between injury severity or time since injury for the individuals with SCI across groups, it is possible that other factors not assessed in this study may explain the baseline differences in burden, such as time providing care, number of dependents, and level of social support. Results of studies with samples from other collectivistic cultures also support the idea that cultural differences contribute uniquely to caregiver outcomes. For example, although caregiver burden tends to be higher in partners of individuals with serious disabilities as compared to partners of individuals with minor disabilities in the United States,31 spousal caregivers in China reported relatively low levels of caregiver burden, most likely because Chinese families are still commonly extended and assistance from other family members is often available to relieve part of the burden of caregiving.4 Future studies should be conducted in Colombia and other Latin American countries to further explore possible cultural differences in psychosocial outcomes.
The effectiveness of the family intervention tested in this study and the apparent impact on the psychosocial functioning of both individuals with SCI and their family members can only be compared to the results of the other 4 published studies: the brief problem-solving training and psychoeducation intervention, delivered both in person15 and via videoconference16; the adaptation of multiple-family group therapy17; and the cognitive-behavioral skills group that targeted both the individual with SCI and a caregiver.13 Notably, the family intervention tested in the present study is the first to include anxiety as an outcome and demonstrated a significant reduction in anxiety symptoms. All of the other 4 published intervention studies examined the impact on depression, but only Schulz and colleagues'13 cognitive-behavioral skills group yielded a significant reduction in depression. Caregiver burden was only included as an outcome measure in the examination of the adaptation of multiple-family group therapy17 and the cognitive-behavioral skills group.13 Both interventions resulted in a significant reduction in burden, just as the family intervention tested in this study did. Out of the 4 published studies, the brief problem-solving training and psychoeducation intervention delivered both in person15 and via videoconference16 were the only 2 that explored the impact on problem-solving appraisals. Both of these intervention modalities demonstrated an ability to reduce dysfunctional caregiver problem-solving styles, as did the family intervention tested in the present study.
The family intervention tested in this study is the first one found to significantly improve psychosocial functioning in multiple domains – depression, anxiety, burden, and problem-solving – among individuals with SCI and their family members. The other 4 previously published studies resulted in significant change in some, but not all domains measured in this study. Additionally, unlike the other published interventions, the one tested in this study goes beyond basic training and psychoeducation. Founded upon the models and techniques of both family therapy and cognitive-behavioral therapy, this intervention was designed to enhance individual as well as family functioning. Given that SCI is a shared condition that impacts and is impacted by the family, it seems possible that this focus on family functioning resulted in better outcomes for individuals with SCI and their family members than any previously tested intervention.
The findings of this study should be considered in light of its limitations. Given that this was a pilot study, the sample size was small and did not allow for the examination of other factors that might impact responsiveness and learning during the intervention, such as level of injury. Further, the individuals with SCI and their family members all resided in rural Colombia. The extent to which the findings of this study can be generalized to Colombian families living in urban areas or to families facing SCI outside of this country is unknown. Future researchers might continue to test the effectiveness of this intervention with families in various countries. Outcome variables in the present study included measures of depression, anxiety, burden, and problem solving. It is not known whether the intervention would have an effect on other domains of participants′ functioning, such as quality of life, family functioning, and coping. The intervention was conducted with family members of adults with SCI at least 6 months after discharge. Future studies are needed to examine the effectiveness of the intervention with families of pediatric SCI patients, as well as adult SCI patients in the acute stage of recovery. The use of a waitlist control group instead of an attention-control group also limited the ability to determine whether the pre-post treatment changes in the intervention group reflect the impact of receiving any kind of professional service, given that this was a population living in extreme poverty without access to rehabilitation resources. Future studies utilizing an attention-control group might help elucidate this possibility. It is unclear whether the improvements observed in this pilot study will persist beyond 6 months after participation in the family intervention. It might be helpful for researchers to follow-up with families each year after their participation in the intervention to monitor their outcomes.
Conclusions
Whereas this pilot study represents only the first step in the examination of the effectiveness of a newly developed intervention for families facing SCI, findings provide initial evidence that it can improve levels of depression, anxiety, burden, and problem-solving appraisals in terms of confidence, approach-avoidance, and personal control. Further, as this is the first family intervention that includes family members living in the home in addition to the caregiver, these results suggest that inclusion of multiple family members and the emphasis on family functioning may be beneficial in both the short and the longer term.
Supplementary Material
Acknowledgments
The writing of this article was supported by the Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment; the Department of Veterans Affairs Mid-Atlantic Mental Illness Research, Education and Clinical Center; and the Hunter Holmes McGuire VA Medical Center.
The authors have no financial, consultant, institutional or other conflicts of interest to declare.
The participating agency's institutional review board approved this study, and informed consent was obtained after the details of the study were thoroughly explained to participants.
REFERENCES
- 1. DeSanto-Madeya S. Adaptation to spinal cord injury for families post-injury. Nurs Sci Q. 2009; 22 1: 57– 66. [DOI] [PubMed] [Google Scholar]
- 2. Vissers M, van den Berg-Emons R, Sluis T, Bergen M, Stam H, Bussmann H.. Barriers and facilitators of everyday physical activity in persons with a spinal cord injury after discharge from the rehabilitation centre. J Rehabil Med. 2008; 40: 461– 467. [DOI] [PubMed] [Google Scholar]
- 3. Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG.. Symptoms of major depression in people with spinal cord injury: Implications for screening. Arch Phys Med Rehabil. 2004; 85: 1749– 1756. [DOI] [PubMed] [Google Scholar]
- 4. Chan CK, Lee P, Lieh-Mak F.. Coping with spinal cord injury: Personal and marital adjustment in the Hong Kong Chinese setting. Spinal Cord. 2000; 38: 687– 696. [DOI] [PubMed] [Google Scholar]
- 5. Craig AR, Hancock KM, Dickson HG.. A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Paraplegia. 1994; 32: 675– 679. [DOI] [PubMed] [Google Scholar]
- 6. Lucke KT, Martinez H, Mendez TB, Arévalo-Flechas LC.. Resolving to go forward: The experience of Latino/Hispanic family caregivers. Qual Health Res. 2013; 23: 218– 230. [DOI] [PubMed] [Google Scholar]
- 7. Gary KW, Nicholls E, Shamburger A, Stevens LF, Arango-Lasprilla JC.. Do racial and ethnic minority patients fare worse after SCI? A critical review of the literature. NeuroRehabilitation. 2011; 29 3: 275– 293. [DOI] [PubMed] [Google Scholar]
- 8. Dickson A, O'Brien G, Ward R, Allan D, O'Carroll R.. The impact of assuming the primary caregiver role following traumatic spinal cord injury: An interpretive phenomenological analysis of the spouse's experience. Psychol Health. 2010; 25 9: 1101– 1120. [DOI] [PubMed] [Google Scholar]
- 9. Dreer LE, Elliott TR, Shewchuk R, Berry JW, Rivera P.. Family caregivers of persons with spinal cord injury: Predicting caregivers at risk for probable depression. Rehabil Psychol. 2007; 52 3: 351– 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Raj JT, Manigandan C, Jacob KS.. Leisure satisfaction and psychiatric morbidity among informal carers of people with spinal cord injury. Spinal Cord. 2006; 44 11: 676– 679. [DOI] [PubMed] [Google Scholar]
- 11. Weitzenkamp DA, Gerhart KA, Charlifue SW, Whiteneck GG, Savic G.. Spouses of spinal cord injury survivors: The added impact of caregiving. Arch Phys Med Rehabil. 1997; 78: 822– 827. [DOI] [PubMed] [Google Scholar]
- 12. Unalan H, Celik B, Sahin A, Caglar N, Esen S, Karamehmetoglu SS.. Quality of life after spinal cord injury: The comparison of the SF-36 Health Survey and its spinal cord injury-modified version in assessing the health status of people with spinal cord injury. Neurosurg Q. 2007; 17 3: 175– 179. [Google Scholar]
- 13. Schulz R, Czaja SJ, Lustig A, Zdaniuk B, Martire LM, Perdomo D.. Improving the quality of life of caregivers of persons with spinal cord injury: A randomized controlled trial. Rehabil Psychol. 2009; 54 1: 1– 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dickson A, O'Brien G, Ward R, Flowers P, Allan D, O'Carroll R.. Adjustment and coping in spousal caregivers following a traumatic spinal cord injury: An interpretive phenomenological analysis. J Health Psychol. 2011; 17 2: 247– 257. [DOI] [PubMed] [Google Scholar]
- 15. Elliott TR, Berry JW.. Brief problem-solving training for family caregivers of persons with recent-onset spinal cord injuries: A randomized controlled trial. J Clin Psychol. 2009; 65 4: 406– 422. [DOI] [PubMed] [Google Scholar]
- 16. Elliott TR, Brossart D, Berry JW, Fine PR.. Problem-solving training via videoconferencing for family caregivers of persons with spinal cord injuries: A randomized controlled trial. Behav Res Ther. 2008; 46: 1220– 1229. [DOI] [PubMed] [Google Scholar]
- 17. Rodgers ML, Strode AD, Norell DM, Short RA, Dyck DG, Becker B.. Adapting multiple-family group treatment for brain and spinal cord injury intervention development and preliminary outcomes. Am J Phys Med Rehabil. 2007; 86 6: 482– 492. [DOI] [PubMed] [Google Scholar]
- 18. Coleman JA, Harper LA, Perrin PB, . et al. Examining the relationship between health-related quality of life in individuals with spinal cord injury and the mental health of their caregivers in Colombia, South America. Int J Rehabil Res. 2013; 36: 308– 314. [DOI] [PubMed] [Google Scholar]
- 19. Newman JA, Reed BJ.. Mexican-American males with a spinal cord injury. SCI Psychol Process. 1998; 11 1: 14– 19. [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JBW.. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001; 16: 606– 613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wulsin L, Somoza E, Heck J.. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Prim Care Companion J Clin Psychiatry. 2002; 4: 191– 195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Diez-Quevado C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL.. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001; 63: 679– 686. [DOI] [PubMed] [Google Scholar]
- 23. Donlan W, Lee J.. Screening for depression among indigenous Mexican migrant farmworkers using the Patient Health Questionnaire-9. Psychol Rep. 2010; 106: 419– 432. [DOI] [PubMed] [Google Scholar]
- 24. Spitzer RL, Kroenke K, Williams JBW, Löwe BA.. Brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006; 166: 1092– 1097. [DOI] [PubMed] [Google Scholar]
- 25. García-Campayo J, Zamorano E, Ruiz MA, . et al. Cultural adaptation into Spanish of the Generalized Anxiety Disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcome. 2010; 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zarit SH, Reever KE, Bach-Peterson J.. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980; 20: 649– 655. [DOI] [PubMed] [Google Scholar]
- 27. Martín M, Salvadó I, Nadal S, . et al. Adaptación para nuestro medio de la Escala de Sobrecarga del Cuidador (Caregiver Burden Interview) de Zarit. Revista de Gerontología. 1996; 6: 338– 346. [Google Scholar]
- 28. Heppner PP, Petersen CH.. The development and implications of a personal problem-solving inventory. J Couns Psychol. 1982; 29 1: 66– 75. [Google Scholar]
- 29. Heppner PP, Witty TE, Dixon WA.. Problem-solving appraisal and human adjustment: A review of 20 years of research using the Problem Solving Inventory. Counsel Psychol. 2004; 32: 344– 428. [Google Scholar]
- 30. Arango-Lasprilla JC, Olivera Plaza SL, Drew A, . et al. Family needs and psychosocial functioning of caregivers of individuals with spinal cord injury in Colombia, South America. NeuroRehabilitation. 2010; 27: 83– 93. [DOI] [PubMed] [Google Scholar]
- 31. Post MWM, Bloeman J, de Witte LP.. Burden of support for partners or persons with spinal cord injuries. Spinal Cord. 2005; 43: 311– 319. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


