Abstract
Background: Manual wheelchair users with spinal cord injury (SCI) are frequently diagnosed with subacromial impingement. Objective: To determine whether the pattern of muscle imbalance and impaired scapular stabilization in able-bodied (AB) adults with impingement is different from that in manual wheelchair users with SCI and impingement. Methods: The following measurements were collected from 22 adults with subacromial impingement (11 SCI, 11 AB): ratio of normalized muscle electrical activity of upper and lower trapezius (UT:LT) during arm abduction; force during abduction, adduction, internal rotation, external rotation, and push and pull; ratios of force for abduction to adduction (AB:ADD), internal to external rotation (IR:ER), and push to pull (PUSH:PULL). Results: Shoulders with impingement had significantly higher UT:LT activation (1.46 ± 0.52) than shoulders without impingement (0.93 ± 0.45) (P = .006), regardless of wheelchair user status. Significant differences between AB participants and those with SCI were observed for ABD:ADD (P = .005), PUSH:PULL (P = .012), and pull strength (P = .043). Participants with SCI had a significantly greater ABD:ADD (1.37 ± 0.36) than AB participants (1.04 ± 0.22) (P = .002) and a significantly greater PUSH:PULL (1.53 ± 0.36) than AB participants (1.26 ± 0.18) (P = .005) because of decreased strength in adduction (P = .021) and pull (P = .013). Conclusions: Strategies targeting the posterior shoulder girdle for AB adults are appropriate for manual wheelchair users with SCI and impingement and should focus on scapular retractors and arm adductors with emphasis on scapular depression and posterior tilting.
Keywords: physical therapy modalities, rehabilitation, shoulder impingement syndrome, spinal cord injury
Shoulder pain occurs in up to 83% of adults with spinal cord injury (SCI).1 In this population, shoulder pain is correlated with decreased quality of life, limited participation in daily activities, and decreased physical activity.1,2 Wheelchair propulsion, transfers, and other daily activities are performed exclusively with the upper body, predisposing individuals to overuse and muscle imbalance. Subacromial impingement is frequently cited as the cause of shoulder pain after SCI.3,4 Able-bodied (AB) adults with subacromial impingement demonstrate compromised scapular stabilization and altered muscle balance.5,6 Impaired scapular stabilization is defined as increased electrical activity in the upper trapezius (UT) compared with the lower trapezius (LT) during humeral elevation. Muscle imbalance is an alteration in typically observed strength ratios of muscle groups at the shoulder joint.
Alterations in muscle balance and scapular stabilization are contributing factors to impingement because they affect subacromial space height during humeral elevation. Scapular posterior tilt and upward rotation are necessary to maintain height of the subacromial space,7 which is accomplished by coordinated activity of the UT and LT along with the serratus anterior and rotator cuff.8 Muscle imbalance in the rotator cuff can contribute to poor centralization and increased anterior and superior translation of the humeral head, leading to impingement in the subacromial space.9 Observations of muscle strength and scapular stabilization in AB adults with impingement have revealed 3 important changes: (1) increased ratio of UT to LT electrical activity during abduction (UT:LT)5,10; (2) increased ratio of force for internal rotation (IR) to external rotation (ER) (IR:ER)11; and (3) increased ratio of force for abduction to adduction (ABD:ADD).12
The pattern of increased UT:LT, IR:ER, and ABD:ADD has not been well examined in manual wheelchair users with SCI and impingement. Current rehabilitation practice for this population is largely based on findings from AB adults with impingement. Several previous studies have demonstrated reduction in shoulder pain after a strength-training program for both AB adults and manual wheelchair users; however, these studies lack evaluation of changes in dynamic muscle force and measures of scapular stabilization.13–16 It is very possible that manual wheelchair users who have impingement may present with a different pattern of muscle imbalance and scapular stabilization because of the difference in upper extremity demands.
Manual wheelchair users with SCI demonstrate changes in scapular position during static activities such as sitting in a wheelchair or standing in a standing frame.17 During a transfer task, manual wheelchair users with impingement have demonstrated increased scapular anterior tilt18 and increased LT activity.19 Increased anterior tilt of the scapula has also been observed in AB adults with impingement,6 whereas LT activity is often decreased in AB adults with impingement. Increased activation of the UT compared with the LT allows for increased scapular anterior tilt, leading to a decrease in subacromial space and potential for impingement. Some previous studies6,18,19 indicate that the pattern of muscle imbalance and scapular stabilization and current treatment protocols based on findings from AB adults with impingement may not be appropriate for people with SCI. Because of the potential for poor surgical outcomes in people with SCI, it is imperative that conservative treatment protocols be optimized in this population.20
Isolated open-chain shoulder movements have been frequently used to evaluate shoulder strength in previous studies; however, wheelchair propulsion is a closed-chain push-dominant activity whose primary motion (closed-chain shoulder forward flexion) has not been well evaluated. In order to address this gap, we included a novel test of closed-chain flexion and extension. This multi-joint activity may be a better indicator of overall shoulder function and be more specific to manual wheelchair use.6,7
Objective
The objective of this study was to determine whether the pattern of muscle imbalance and impaired scapular stabilization observed in AB adults with impingement is different from that in manual wheelchair users with SCI who have impingement. We hypothesized that manual wheelchair users with SCI and impingement would demonstrate a pattern of muscle imbalance (increased ABD:ADD, increased IR:ER) and impaired scapular stabilization (increased UT:LT) to a greater extent than AB adults with impingement.
Methods
Design
We used a cohort study design to evaluate shoulder strength and scapular stabilization during a single testing session. If a participant had one shoulder with impingement and one shoulder without impingement, both shoulders were tested. In the case of bilateral impingement, only the more painful shoulder was included in the analysis. We also included one shoulder from each of 2 manual wheelchair users who did not have impingement in either shoulder. Each shoulder tested was identified as belonging to 1 of 4 groups: nonimpingement SCI (NI-SCI) (n = 8), impingement SCI (I-SCI) (n = 9), nonimpingement AB (NI-AB) (n = 10), or impingement AB (I-AB) (n = 10).
Participants
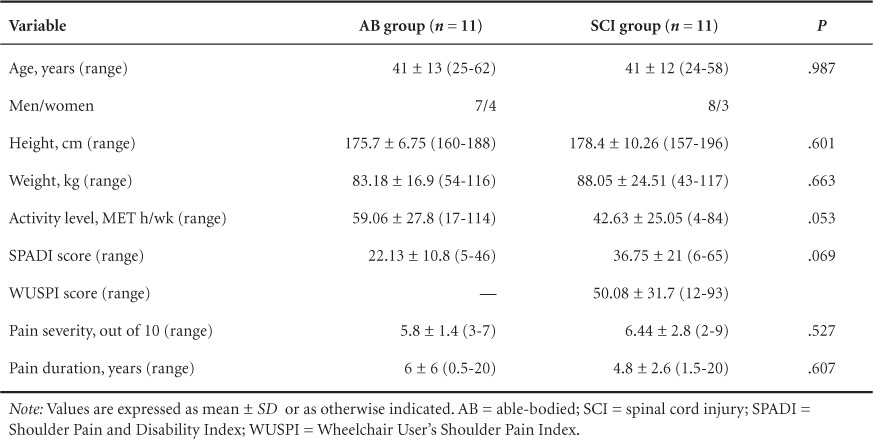
Participants with (n = 11; C7-T12) and without (n = 11) SCI were recruited from our local area (Table 1). Sample size was based on a preliminary power analysis to detect differences in UT:LT with 80% power and a moderate effect size (0.5).5,10 Inclusion criteria were 19 to 65 years of age; ability to raise both arms overhead; no shoulder surgery, fracture, subluxation, or dislocation in the past 5 years; and no known cardiovascular or pulmonary disease. Shoulders in the impingement group had at least 2 positive results of clinical tests for impingement (Neer, Hawkins-Kennedy, Empty Can) and negative test results for both labral tear (O'Brien's) and instability (Sulcus Sign).21 Additional inclusion criteria for the SCI group were 2 years or more post SCI (complete or incomplete, C7 or lower), use of manual wheelchair as primary means of mobility, and no current pressure ulcer greater than grade 2. Two participants with C7 injury performed manual muscle testing of the elbow extensors to confirm preservation of the C7 segment (all manual muscle tests = 5/5). All participants completed the Shoulder Pain and Disability Index (SPADI)22 and a 10-point visual analog scale (VAS) for pain level. Participants with SCI also completed the Wheelchair Users Shoulder Pain Index (WUSPI).23 Possible SPADI scores range from 0 to 100, and WUSPI scores range from 0 to 150. For both scales, lower scores indicate less pain and higher function. Participants also completed questionnaires regarding physical activity level, specific for AB subjects (International Physical Activity Questionnaire)24 or subjects with SCI (Physical Activity Scale for Individuals with Physical Disabilities).25 Both scales provide estimated metabolic equivalent (MET) hours per week of activity, indicating total energy expenditure.
Table 1.
Participant characteristics
Instrumentation
Isokinetic strength and muscle activity of UT and LT were determined by using an isokinetic dynamometer (Biodex Medical Systems, Shirley, NY) integrated with surface electromyography (EMG) (ADInstruments, Inc., Colorado Springs, CO). Bipolar surface electrodes were placed over the muscle belly, in line with the fibers of the UT and LT (Figure 1). A reference electrode was placed over the clavicle. Signals were amplified with a differential amplifier (ADInstruments, Inc.) with a high-input impedance (>15Ω at 100 Hz), a common mode rejection ratio of 85 dB at 60 Hz, and a bandwidth (−3 dB) of 20 to 2,000 Hz. Root mean square (RMS)–processed signals were collected in real time with a sampling rate of 2,000 Hz using a 16-bit A/D board (ADInstruments, Inc.). During pilot testing, our test-retest reliability of UT:LT during maximal arm abduction, determined on 2 separate occasions, was excellent (Cronbach's alpha > 0.9).
Figure 1.

(A) Determination of upper trapezius electrode placement, (B) determination of lower trapezius electrode placement, and (C) final electrode set-up (ground electrode over clavicle, not shown).
Testing procedure
All testing was performed in the laboratory and took approximately 90 minutes to complete. Before testing, participants performed a short warm-up. Resting levels of electrical activity of the UT and LT were recorded; EMG signal quality was verified, and maximal electrical activity was determined by having the participant perform maximal voluntary isometric contractions (MVICs) against a stationary lever arm for each muscle group.
For the LT muscle, the attachment was positioned diagonally overhead in 160° of forward flexion and 145° of abduction. Participants were instructed to keep their elbows straight while applying a backward force on the attachment as if they were winding up to throw a ball. For the UT muscle, the attachment was positioned at 90° of arm abduction and 5° of horizontal flexion. Participants were instructed to keep their elbows straight while applying an upward force as if they were going to perform a jumping jack. Participants performed three 5-second MVICs against the attachment while receiving encouragement from the principal investigator. A 15-second pause occurred between each contraction. EMG data collected during the MVICs were used to create a normalization reference for each participant. After signal filtering, the average RMS value for the middle 3 seconds of each contraction was calculated to determine the normalization value for each muscle group.
Isokinetic testing consisted of 3 protocols (Table 2): abduction and adduction in the frontal plane (Figure 2A), IR and ER in the scapular plane (Figure 2B), and closed-chain flexion (push) and closed-chain extension (pull) in the sagittal plane at waist level (Figure 2C). After the range-of-motion limits had been set for each test, participants were familiarized with the motion and speed and were instructed to stop testing if the motion was too painful. For all tests, participants were stabilized with a lap belt, footrest, and belt across the contralateral shoulder. Participants were instructed to hold onto the handle on the edge of the Biodex seat, contralateral to the side being tested. This increased the trunk stability of participants with higher level injuries, as did positioning the feet at a comfortable position on the footrest. After familiarization repetitions were completed, gravity correction was performed with the arm in a relaxed position. Participants then performed 5 maximal repetitions at 60° per second with verbal encouragement from the principal investigator and study staff. During the maximal isokinetic movements, EMG data from the 2 trapezius parts were collected synchronously with the arm movement.
Table 2.
Test position descriptions
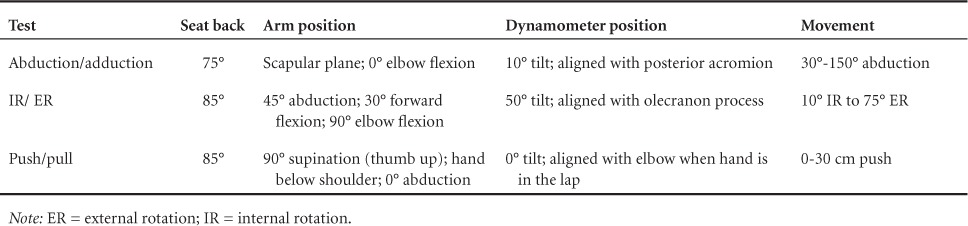
Figure 2.

(A) Positioning and set-up for arm abduction/adduction, (B) positioning and set-up for shoulder internal/external rotation, and (C) positioning and set-up for push and pull.
Isokinetic dynamometry signal processing
Raw isokinetic dynamometer signals were analog/digital converted (16-bit resolution) at 2,000 Hz. Signals were converted to force, position, and velocity following standardized calibrations. Range-of-motion markers were automatically generated to define 60° to 120° of abduction/adduction, 0° to 20° of IR/ER, and 5 to 15 cm of push/pull.
EMG signal processing
Raw EMG signals were analog/digital converted (16-bit resolution) at 2,000 Hz and were low- and high-pass filtered. A 35-ms moving average was used to smooth the signal. The RMS values over 60° to 120° of arm abduction were averaged across the 5 repetitions. The mean amplitude EMG signal, expressed as a percentage of MVICs, was used to assess the activity of the 2 trapezius parts during arm abduction.
Statistical analysis
Means, standard deviations, and ranges were calculated for the dependent variables: UT:LT; average force during specified periods of abduction, adduction, IR, ER, and push and pull; ABD:ADD, IR:ER, and ratio of force for push to pull (PUSH:PULL).
Each shoulder tested was assigned to 1 of 4 groups: NI-SCI (n = 8), I-SCI (n = 9), NI-AB (n = 10), or I-AB (n = 10). If a participant had bilateral shoulder impingement, only his or her more painful shoulder was included in the analysis. Three participants in the SCI group had signs of bilateral impingement, so we added 2 additional people with SCI who did not have impingement in an effort to have a sufficient sample for analyses in the NI-SCI group. One AB participant had bilateral impingement, and one I-AB shoulder was unable to produce sufficient force to register on the dynamometer and was not included in the analysis.
The primary interest was the interaction between impingement and SCI/AB. We first analyzed the data using 2-way multivariate analysis of variance (MANOVA) including independent variables of impingement/nonimpingement and SCI/AB and dependent variables of UT:LT; average force during specified periods of abduction, adduction, IR, ER, and push and pull; ABD:ADD, IR:ER, and PUSH:PULL. The Impingement × SCI/AB interaction was not significant in the 2-way MANOVA model [F(10, 24) = 0.33, P = .96]; therefore, the model was re-fit using a multivariate general linear model (GLM) to determine the influence of the main effects (SCI/AB and impingement/nonimpingement) on the dependent variables.
Groups were similar for height, weight, and age; no adjustments were made in the analyses for these variables. There were 4 women in the AB group and 3 women in the SCI group. When the single-item VAS and SPADI were used for determining level of pain, groups were similar (P > .05); therefore, pain level was not considered a confounding variable. The SCI group performed less physical activity than the AB group; however, the difference was not statistically significant (P = .053) and not adjusted for in the analysis. Hand dominance was not a significant predictor in the GLM model and was not included in the final analysis. Statistical analyses were performed with IBM SPSS, version 21.0 (IBM Corp., Armonk, NY).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Scapular stabilization during maximal isokinetic shoulder abduction
Descriptive results of EMG and isokinetic force data for all motions are summarized in Table 3. The multivariate GLM model containing SCI/AB and impingement/nonimpingement showed a significant difference for UT:LT activity during maximal isokinetic shoulder abduction (F = 4.45, df = 2, P = .019) (Table 3). Post hoc analysis revealed that shoulders with impingement, regardless of SCI/AB status, had significantly higher UT:LT (1.46 ± 0.52) compared with nonimpingement shoulders (0.93 ± 0.45) (P = .006) (Figure 3). There was no significant difference in the ratio between SCI and AB groups (P = .62) (Figure 3).
Table 3.
Scapular stabilization and muscle torque by group
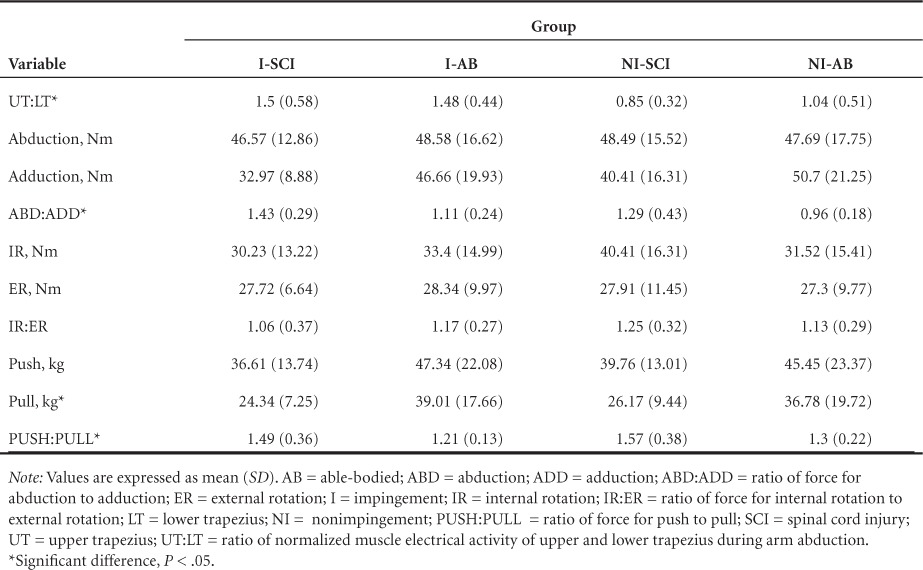
Figure 3.

Main effects (able-bodied/spinal cord injury; impingement/nonimpingement) for all ratio variables. *P < .05.
Muscle imbalance during maximal isokinetic movements
The multivariate GLM model containing SCI/AB and impingement/nonimpingement showed a statistically significant difference for ABD:ADD (F = 6.29, df = 2, P = .005), PUSH:PULL (F = 5.02, df = 2, P = .012), and absolute pull force (F = 3.45, df = 2, P = .043) but not for rotation or any other absolute differences in strength (Table 3). Post hoc tests revealed that shoulders of participants with SCI had a significantly greater ABD:ADD (1.37 ± 0.36) than shoulders of AB participants (1.04 ± 0.22) (P = .002) (Figure 3) and significantly greater PUSH:PULL (1.53 ± 0.36) than that of AB participants (1.26 ± 0.18) (P = .005) (Figure 3). Post hoc analysis revealed that differences were due to decreased strength in adduction (P = .021) and pull (P = .013) in the SCI group (Figure 4).
Figure 4.
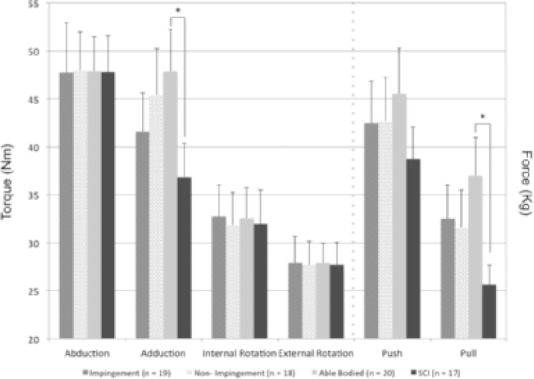
Main effects (able-bodied/spinal cord injury; impingement/nonimpingement) for all torque/force variables. *P < .05.
Discussion
Current rehabilitation for impingement in manual wheelchair users with SCI is based on findings from AB adults, typically overhead athletes or workers. An understanding of muscle imbalance and scapular stabilization in AB adults with shoulder impingement offers clinicians insight into the treatment and prevention of shoulder pain in manual wheelchair users with SCI. Several important observations are made concerning scapular stabilization and muscle imbalance for manual wheelchair users with SCI and impingement. First, poor scapular stabilization (increased UT:LT) during arm abduction occurs in shoulders with impingement and is not greater in shoulders of manual wheelchair users with SCI who have impingement. Second, manual wheelchair users with SCI demonstrate an altered muscle balance (decreased strength in adduction and pulling) compared with AB adults, and this difference is not amplified for those with impingement and SCI. Finally, no differences exist in rotational strength between persons with SCI and AB adults or impingement/nonimpingement.
Manual wheelchair users with SCI and impingement have increased UT:LT activity during maximal isokinetic arm abduction. These results are similar to findings in AB adults in previous studies.5 The combined actions of UT and LT during arm abduction normally cause upward rotation and posterior tilting of the scapula to maintain subacromial height.7 When alteration in the function of these muscles occurs, scapular stabilization is compromised, potentially leading to decreased subacromial space and impingement of the underlying structures. We observed that muscle dysfunction in the trapezius occurs similarly for manual wheelchair users with SCI who have impingement and AB adults with impingement. These results suggest that the altered muscle activity is related to the shoulder pathology, regardless of the type of repetitive activity being performed (overhead activities vs wheelchair use).
In our evaluation of muscle balance (strength ratios of opposing motions), we found that manual wheelchair users with SCI have an increased ABD:ADD. The increased ABD:ADD is in agreement with findings by other investigators who have observed decreased adduction strength in manual wheelchair users with shoulder pain.26 Our results indicate that the increased ratios result primarily from decreased adduction strength in the SCI group. We did not observe any differences in the absolute force for rotational movements or in the IR:ER (see Table 3). The rotator cuff is often cited as a causative factor for shoulder pain and impingement because of its role in humeral head centralization9; however, no differences were observed in our cohort.
Wheelchair propulsion is a push-dominant activity, with forward flexion comprising the majority of the movement at the shoulder joint.27 Previous EMG studies show that the pectoral muscles are a major contributor to the push phase of wheelchair propulsion, without subsequent contraction in the posterior shoulder girdle.28 This is an important observation because other investigators have noted that tightness in the pectoral muscles increases the likelihood for kinematic changes in the scapula, predisposing individuals to shoulder dysfunction.7 Prolonged wheelchair propulsion, along with weight relief maneuvers and wheelchair transfers, may create an imbalance between push/pull strength in manual wheelchair users with SCI, which had not been evaluated previously. We found an increased ratio of push to pull force for the SCI group, indicating that persons with SCI may benefit from prophylactic strengthening of the posterior shoulder muscles.
Adduction strength was also significantly lower in the group with SCI. The combination of decreased pull strength, adduction strength, and LT activity reveals that manual wheelchair users with SCI, specifically those with impingement, lack strength in the posterior shoulder girdle. Previous studies have shown that targeted strengthening activities for the posterior shoulder muscles are effective in relieving pain and improving scapular stabilization.29 Based on our findings, rehabilitation prescriptions that focus on scapular stabilization and posterior shoulder strength like those recommended for AB adults with impingement are appropriate for the SCI population.
We did not observe any differences in rotational strength for manual wheelchair users, indicating that it may be of lesser importance to target rotator cuff strengthening in this population. Manual wheelchair users are predisposed to weakness in the posterior shoulder girdle, potentially resulting from the push-dominant activities of wheelchair use.27 This is important for rehabilitation professionals to note because preventative activities that strengthen the posterior shoulder girdle may help to avoid shoulder impingement.
Limitations
The study was primarily limited in 2 ways. First, because of limitations in our data collection system, the EMG measurements were restricted to 2 muscles, the UT and LT. In future studies, it would be beneficial to examine a greater number of muscle groups to determine their involvement in shoulder impingement. Second, we did not have a direct measurement of scapular kinematics during testing. Direct measurement of scapular kinematics would be beneficial to confirm that the observed pattern of impaired scapular stabilization is associated with the same kinematic changes in manual wheelchair users as in AB adults. Our group of participants had a variety of injury levels and time since injury, which we believe increases the external validity of our results; however, we did not have a sufficient sample size to stratify the results by injury level, which may be beneficial in order to tailor strengthening programs to each individual. We did not have any participants with American Spinal Injury Association Impairment Scale (AIS) grade D impairment, potentially because they do not typically use manual wheelchairs as their primary means of mobility.
Conclusion
Manual wheelchair users present with a pattern of impaired scapular stabilization similar to that of AB adults with impingement. These results indicate that prescription of scapular stabilization exercises is an appropriate therapeutic intervention for manual wheelchair users. Participants with SCI also demonstrated weakness in shoulder adduction and pulling strength, indicating weakness in the posterior shoulder girdle. This should be taken into consideration by rehabilitation professionals for both prophylactic strengthening and therapeutic interventions for the shoulder.
Future work is warranted to evaluate the effects of injury level on scapular stabilization and the contribution of rotator cuff strength to impingement, as we did not observe any differences between shoulders with and without impingement. Although protocols including rotator cuff strengthening have reduced pain caused by impingement, the mechanism for their effectiveness may not be uniquely dependent on increased strength of the cuff. Going forward, it may also be beneficial to evaluate these differences during daily tasks such as pressure relief and transfers.
Acknowledgments
The contents of this publication were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant no. 90RE5009). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this article do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. Additional funding was provided by the UAB Department of Physical Medicine and Rehabilitation.
The authors declare no conflict of interest. The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
The authors thank all of the study participants.
REFERENCES
- 1. Subbarao J, Klopfstein J, Turpin R.. Prevalence and impact of wrist and shoulder pain in patients with spinal cord injury. J Spinal Cord Med. 1994; 18: 9– 13. [DOI] [PubMed] [Google Scholar]
- 2. Kemp BJ, Bateham AL, Mulroy SJ, Thompson L, Adkins RH, Kahan JS.. Effects of reduction in shoulder pain on quality of life and community activities among people living long-term with SCI paraplegia: A randomized control trial. J Spinal Cord Med. 2011; 34 3: 278– 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dyson-Hudson T, Kirshblum S.. Shoulder pain in chronic spinal cord injury, part I: Epidemiology, etiology and pathomechanics. J Spinal Cord Med. 2004; 27 1: 4– 17. [DOI] [PubMed] [Google Scholar]
- 4. Bayley J, Cochran T, Sledge C.. The weight-bearing shoulder. The impingement syndrome in paraplegics. J Bone Joint Surg Am. 1987; 69 5: 676– 678. [PubMed] [Google Scholar]
- 5. Cools AM, Declercq GA, Cambier DC, Mahieu NN, Witvrouw EE.. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007; 17 1: 25– 33. [DOI] [PubMed] [Google Scholar]
- 6. Ludewig PM, Cook TM.. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000; 80 3: 276– 291. [PubMed] [Google Scholar]
- 7. Ludewig PA, Reynolds JF.. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009; 39 2: 90– 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Timmons MK, Thigpen CA, Seitz A, Karduna AR, Arnold BL, Michener LA.. Scapular kinematics and subacromial-impingement syndrome: A meta-analysis. J Sport Rehabil. 2012; 21: 354– 370. [DOI] [PubMed] [Google Scholar]
- 9. Matsen F, Fu F, Hawkins R.. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1993. [Google Scholar]
- 10. Smith M, Sparkes V, Busse M, Enright S.. Upper and lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Phys Ther Sport. 2009; 10: 45– 50. [DOI] [PubMed] [Google Scholar]
- 11. Moraes G, Faria C, Teixeira-Salmela L.. Scapular muscle recruitment patterns and isokinetic strength ratios of the shoulder rotator muscles in individuals with and without impingement syndrome. J Shoulder Elbow Surg. 2008; 17: 48– 53. [DOI] [PubMed] [Google Scholar]
- 12. Burnham R, May L, Nelson E, Steadward R, Reid D.. Shoulder pain in wheelchair athletes: The role of muscle imbalance. Am J Sports Med. 1993; 21 2: 238– 242. [DOI] [PubMed] [Google Scholar]
- 13. Curtis KA, Tyner TM, Zachary L, . et al. Effect of a standard exercise protocol on shoulder pain in long-term wheelchair users. Spinal Cord. 1999; 37 6: 421– 429. [DOI] [PubMed] [Google Scholar]
- 14. Mulroy SJ, Thompson L, Kemp B, . et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: A randomized controlled trial. Phys Ther. 2011; 91 3: 305– 324. [DOI] [PubMed] [Google Scholar]
- 15. Nawoczenski DA, Ritter-Soronen JM, Wilson CM, Howe BA, Ludewig PM.. Clinical trial of exercise for shoulder pain in chronic spinal cord injury. Phys Ther. 2006; 86 12: 1604– 1618. [DOI] [PubMed] [Google Scholar]
- 16. Van Stratten MG, Cloud BA, Morrow MM, Ludewig PM, Zhao KD.. Effectiveness of home exercise on pain, function, and strength of manual wheelchair users with spinal cord injury: A high-dose shoulder program with telerehabilitation. Arch Phys Med Rehabil. 2014; 95 10: 1810– 1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Riek L, Ludewig P, Nawoczenski D.. Comparative shoulder kinematics during free standing, standing depression lifts and daily functional activities in persons with paraplegia: Considerations for shoulder health. Spinal Cord. 2008; 46: 335– 343. [DOI] [PubMed] [Google Scholar]
- 18. Nawoczenski D, Riek L, Greco L, Staiti K.. Effect of shoulder pain on shoulder kinematics during weight-bearing tasks in persons with spinal cord injury. Arch Phys Med Rehabil. 2012; 93 8: 1421– 1430. [DOI] [PubMed] [Google Scholar]
- 19. Finley M, McQuade K, Rodgers M.. Scapular kinematics during transfers in manual wheelchair users with and without shoulder impingement. Clin Biomech (Bristol, Avon). 2005; 20 1: 32– 40. [DOI] [PubMed] [Google Scholar]
- 20. Goldstein B, Young J, Escobedo EM.. Rotator cuff repairs in individuals with paraplegia. Am J Phys Med Rehabil. 1997; 76 4: 316– 322. [DOI] [PubMed] [Google Scholar]
- 21. Michener LA, Walsworth MK, Doukas WC, Murphy KP.. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009; 90 11: 1898– 1903. [DOI] [PubMed] [Google Scholar]
- 22. Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y.. Development of a shoulder pain and disability index. Arthritis Care Res. 1991; 4 4: 143– 149. [PubMed] [Google Scholar]
- 23. Curtis KA, Roach KE, Applegate EB, . et al. Reliability and validity of the Wheelchair User's Shoulder Pain Index (WUSPI). Paraplegia. 1995; 33 10: 595– 601. [DOI] [PubMed] [Google Scholar]
- 24. Craig CL, Marshall AL, Sjöström M, . et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35 8: 1381– 1395. [DOI] [PubMed] [Google Scholar]
- 25. Washburn R, Zhu W, McAuley E, Frogley M, Figoni SF.. The physical activity scale for individuals with physical disabilities: Development and evaluation. Arch Phys Med Rehabil. 2002; 83 2: 193– 200. [DOI] [PubMed] [Google Scholar]
- 26. Sinnott K, Milburn P, McNaughton H.. Factors associated with thoracic spinal cord injury, lesion level and rotator cuff disorders. Spinal Cord. 2000; 38: 748– 753. [DOI] [PubMed] [Google Scholar]
- 27. Shimada S, Robertson R, Bonninger M, Cooper R.. Kinematic characterization of wheelchair propulsion. J Rehabil Res Dev. 1998; 35 2: 210– 218. [PubMed] [Google Scholar]
- 28. Mulroy S, Gronley J, Newsam C, Perry J.. Electromyograpic activity of shoulder muscles during wheelchair propulsion by paraplegic persons. Arch Phys Med Rehabil. 1996; 77: 187– 193. [DOI] [PubMed] [Google Scholar]
- 29. De Mey K, Danneels L, Cagnie B, Cools AM.. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: Effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med. 2012; 40 8: 1906– 1915. [DOI] [PubMed] [Google Scholar]


