Abstract
Background
Interventions to impact on the burden of chronic non-communicable diseases, such as hypertension and diabetes, include screening of asymptomatic adults, but little is known about the subsequent course of clinical care. We report on the uptake of referral for clinical assessment and retention in care following a large urban/rural population screening programme in Malawi.
Methods
Adult residents were screened for raised blood pressure and raised fasting blood glucose at a demographic surveillance site in rural Karonga District and in urban Area 25, Lilongwe with well-supported chronic care clinics. Successful uptake was defined as presenting for clinical assessment within 6 weeks of referral, and non-attenders were followed at home. Logistic regression was used to examine association of uptake with demographic and clinical factors. Retention was assessed using survival analysis techniques.
Findings
27,305 participants were screened for hypertension and diabetes between May 2013 and September 2015. Of these, 4,075 (14.9%) were referred for suspected hypertension (3,640), diabetes (172) or both (263). Among those referred, 2,480 (60.9%), reported for clinical assessment. Factors associated with uptake of care included being female (adjusted odds ratio (aOR):1.40; 95%CI:1.20-1.63), rural residency (aOR:2.24; 95%CI:1.93-2.61), increasing age, unemployment (aOR:1.43; 95%CI:1.18-1.74), prior medication, and diabetes. Factors associated with better retention in care included final diagnosis with hypertension and/or diabetes following clinical assessment, rural residency and older age.
Conclusions
Screening for hypertension and diabetes identifies large numbers of individuals who need further clinical assessment, but strategies are needed to ensure better linkage and retention into care.
Funding
The Wellcome Trust
Keywords: Hypertension, diabetes, referral, uptake, retention
Introduction
Non-communicable diseases (NCDs) account for 38 million deaths per year globally, representing 35.6% of all deaths in adults less than 70 years of age. A large part of this burden is in the developing world, including countries in sub-Saharan Africa (SSA), where 85% of the deaths from NCDs years occur.1, 2 Demographic changes, increasing urbanization and lifestyle changes are amongst the contributors to the increasing burden of cardio-metabolic risk factors such as diabetes and hypertension.
Combating the massive burden of NCDs, and their complications, in low-income settings will require increased and sustained efforts to improve awareness among the public and health personnel to enhance detection, access to, and retention in care.3, 4 While health systems in SSA have developed mechanisms to manage infectious diseases, there are few data on the effect of the increased burden of chronic NCDs on their fragile health systems. In Tanzania, as in many SSA countries, outpatient services for NCDs continue to be provided at main hospitals, although new policies encourage decentralisation of care to primary level health centres and dispensaries.5 In Kenya, management of hypertension and diabetes was achievable at the primary care level within an informal setting.6 However, the challenges/weaknesses in public health systems are evident even in emerging economies, such as South Africa.7 Some governments such as Ghana have drafted policies for the prevention and control of chronic NCDs although low funding and weak governance have remained hindrances.8
Reliable data on the burden of NCDs are lacking from Africa, but some settings have reported rates of hypertension and diabetes among adults exceeding 25% and 5%, respectively, with little difference between rural and urban settings.9, 10 These disorders, whose prevalence are already similar to those in developed countries, and rapidly increasing, contribute to at least half of strokes, heart failure and renal failure in SSA.11–15 Importantly, in these settings, hypertension and diabetes are undetected in the majority of subjects, presenting a major impediment to management and necessitating a drive towards appropriate screening programmes. However, it will be crucial that screening is coupled with an effective route to care, and even less is known about the uptake of care following population screening for NCDs in these settings.16
Malawi, like many countries in SSA, needs detailed data to inform the public health response to NCDs, with NCDs now the second leading cause of deaths in Malawian adults, after HIV/AIDS.17 Cardio-metabolic risk factors, including diabetes and hypertension, have been found to be very common in adults following sample surveys. 18, 19 We have recently established a research programme to accurately describe the prevalence and risk factors of NCDs among adults in both urban and rural areas20 with preliminary analysis showing crude prevalence of diabetes and hypertension of 1.5% and 17.2% respectively in the rural area and 2.5% and 20.7% in the urban settings respectively.21, 22 In partnership with the Ministry of Health, chronic care clinics (CCCs) have been established in the two areas, where individuals suspected to have hypertension and/or diagnosed with diabetes, are referred and managed. This has provided a unique opportunity to carefully examine the effect of a mass screening programme on uptake and retention in care among patients with suspected NCDs. Here, we discuss the enrolment process and factors associated with uptake and retention in care, relevant to the SSA setting.
Methods
This work was undertaken at the Malawi Epidemiology and Intervention Research Unit (MEIRU), a research partnership between the London School of Hygiene and Tropical Medicine (LSHTM), the Malawi College of Medicine and the Ministry of Health (MoH). As Karonga Prevention Study, MEIRU has been conducting infectious disease research in rural Karonga for over 30 years, and, with the start of the NCD research programme in 2012, has established an urban study site in Lilongwe. The NCD work includes large cross-sectional studies, at both sites, on the prevalence and risk factors of selected NCDs, including hypertension and diabetes, targeting individuals aged 18 years or more. The urban Lilongwe site, Area 25, had a population of 54,692 with 34,754 (53.8%) adults aged 18 and above following the 2008 population census 23 and was enumerated prior to surveying. In rural Karonga, the participants were drawn from the well characterised Demographic Surveillance Site (DSS) first set-up in 2002 with a population of over 35,000, 40% of whom, were adults.24 Before the start of data collection, we undertook active community sensitization campaigns. Participants were recruited following a household listing of all eligible residents. A questionnaire on lifestyle, physical activity, dietary and economic activities was administered to individuals who consented to participate. Anthropometric measurements were taken with repeat measurements for weight, height, waist and hip circumference, and mid-upper arm circumference (MUAC) among other key physical measurements. Body mass index (BMI) was calculated for all participants except pregnant women, and was categorized as underweight (<18.5-30 kg/m2), normal (18.5-25), overweight (25-30 kg/m2) and obese (> 30 kg/m2).
Blood pressure (BP) was measured three times using an Omron automated device with a five minute interval between measurements and the average of the last two readings was used.25 Fasting blood samples were collected by a team of nurses the following morning for laboratory measurement of glucose and other metabolic markers (including lipid profiles) using Beckman Coulter AU480 Chemistry analysers.
Referral mechanisms
Participants who, on screening, were found to have raised BP (systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg) or those on medication for hypertension were referred. Individuals with a fasting blood glucose (FBG) ≥7mmol/L (≥126mg/dL) or with a self-report of prior diagnosis of diabetes from a health professional were also referred. Referred participants were given a paper referral slip to present at clinic and advised to present within two weeks (or sooner for severe hypertension – see below for definition). The referral CCCs were at primary health care facilities; Area 25 Health Centre in Lilongwe, and Chilumba Rural Hospital (CRH) in Karonga, where clinical assessment and confirmation of diagnosis and subsequent management was provided. Standard MoH clinical management guidelines were followed, and additional drugs were provided (through a donation from CIPLA, India) to ensure a stable supply.
Clinic procedures
At the CCC, participants were received by a study clerk, who cross-checked referral slips and conducted identity checks against a database for those that had forgotten the slip. A clinical assessment was conducted by a clinical officer and included repeat BP measurements and screening for complications of hypertension or diabetes. Those found to have persisting raised BP were managed according to the MoH protocol with lifestyle advice only or lifestyle advice plus medication, based on BP severity. BP readings were classed in three categories; mild (SBP 140-159 mmHG or DBP 90-99 mmHg), moderate (SBP 160-179 mmHG or DBP 100-109 mmHg) and severe hypertension (SBP>180 or DBP>110 mmHg). Participants who, on repeat measurement, no longer met the definition of raised BP, were reviewed on three more monthly visits, to determine if the BP remained below 140/90mmHg. Monthly follow-up appointments were given to all participants enrolled at the clinic, with appointment dates recorded in the patient held record (“Health Passport”). Individuals failing to respond to lifestyle advice would be started on medication on subsequent visits. Management of confirmed diabetic patients also followed MoH guidelines on lifestyle management and, where indicated oral medication. Regular checks of FBG were done at each visit using point of care glucometers to inform clinical management.
Data linkage
Study identifiers assigned during the initial screening at home, and recorded on referral slips, were recorded at the clinic on each visit. The study identifiers were added to the clinical review forms completed by the study clinician and study clerk, allowing linkage to survey data. On each clinic visit a standardised clinical data slip (including study identifiers) was completed and inserted in to the Health Passport, and scanned before departure from the clinic.
Uptake of care
Successful uptake was defined as attending clinic for a full clinical assessment within six weeks of the date of referral. Those who had not taken up the referral for more than six weeks were visited at home and interviewed for reasons for failure to attend.
Retention in care
Retention in care amongst those who attended for the clinical assessment, was defined as coming for scheduled clinic appointments until discharge from the clinic or remaining in care for the entire follow-up period, whichever was earlier. Participants referred with suspected hypertension but whose BP readings did not meet the definition of hypertension on three consecutive clinic attendances were excluded from follow-up but still advised to have regular BP checks in future. As all patients referred for diabetic care met the case definition, there were no circumstances stopping clinical attendance. Retention in care was analysed separately for a) all those with diabetes b) those who still met the definition of raised BP on clinical assessment (excluding those with diabetes), and c) those with low, normal or only slightly raised BP on the clinical assessment (excluding those with diabetes).
Clinic case load
Clinic case-load of those on anti-hypertensive medication was defined as the number of people started on treatment who would still be expected to be attending (expected) and those who were still in contact with health services (actual). Still in contact with health services was defined as attending the clinic at any time following enrolment regardless of missing any appointments in between. This included participants given lifestyle advice only based on their BP readings < 140/90 mmHG for the first 3 clinical visits who were subsequently started on anti-hypertensive medication later if BP failed to normalise in the subsequent visits.
Data management and analysis
Survey data were collected electronically using tablet computers with entry templates programmed in the open data kit (ODK) platform. All data were transferred into a database at the end of each day. Scans of clinical review forms were double-entered in MS Access.
Logistic regression models were used to assess associations of uptake of care and socio-demographic factors such as age, sex, study site, occupation, whether they were on medication or not, reason for referral, BMI and BP level at screening. Univariate odds ratios (ORs) were calculated for the urban and rural sites separately. Adjusted odds ratios (aORs) were obtained from a multivariable logistic regression model that included site, sex, age-group, hypertension/diabetes medication at time of screening, employment (as a surrogate for educational status), BMI category (underweight, normal, overweight, obese), referral reason and BP level at the time of screening.
Factors influencing retention were explored using Cox proportional hazards regression models with Kaplan-Meier plots used to compare retention between sites and within the three groups. The multivariable analysis model included group and the other socio-demographics factors. A participants’ follow-up time was censored at the time of discharge from clinic or at the end of the follow-up period whichever was sooner. Failure (drop-out) was defined as not attending a scheduled clinical appointment for more than 30 days after the appointment date.
Variables where the odds ratios (ORs), hazard ratios (HRs), p-values and 95% confidence intervals (CIs) were found significant (p<0.10) in univariate models were included in multivariable logistic and Cox models to estimate adjusted odds and hazard ratios respectively. Likelihood ratio tests were used in model selection in the multivariable analyses. All analyses were done using Stata version 12 (StataCorp Limited, College Station, TX).
Ethics
The study was approved by the Malawi National Health Sciences Research Committee protocol number #1072 and the LSHTM ethics committee, protocol number #6303.
Results
Between May 2013 and September 2015, 27,305 adults were screened for hypertension and diabetes in Karonga (13,458) and in Lilongwe (13,847). Participation rates are described elsewhere [19]. The median age of participants was 31.6 years (inter-quartile range (IQR): 24.1 – 42.8). 4,075 (14.9%) of all screened participants were referred to the CCCs (14.2% and 15.6% for rural and urban, respectively).
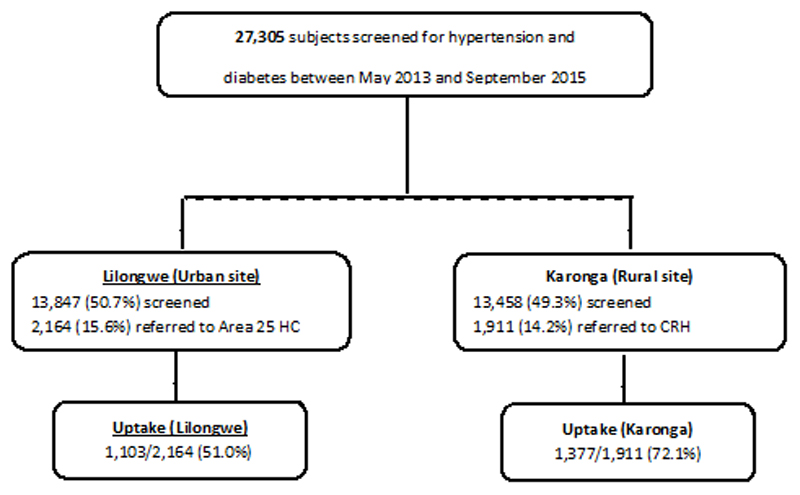
Of the individuals referred, 2,480/4,075 (60.9%) reported to the clinic, 1,377 (72.1%) in the rural, and 1,103 (51.0%) in the urban site (Figure 1). Around 30% of all referred participants were already on hypertension and/or diabetes medication at the time of screening across both sites. The majority of those screened and more likely to be referred were female (59.6%). At both sites, raised BP and diabetes were much more common in individuals aged over 45 years (Table 1).
Figure 1.
Consort diagram showing those screened, identified with hypertension or diabetes, referred for care, and attending for care.
Table 1. Unadjusted Odds Ratios (ORs) by site and adjusted Odds Ratios (aORs) for factors associated with uptake of care following referral for hypertension and/or diabetes.
| Lilongwe (urban) | Karonga (rural) | Both sites | ||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Number (%) | Uptake, n %) | OR (95% CI) | Number (%) | Uptake, n (%) | OR (95% CI) | aOR | p-value |
| Site Lilongwe | 2,164 (53.1) | 1,103 (51.0) | 1 | - | ||||
| Karonga | 1,911 (46.9) | 1,377 (72.1) | 2.24 (1.93-2.61) | <0.001 | ||||
| Sex | ||||||||
| Male | 848 (39.2) | 378 (44.6) | 1 | 795 (41.6) | 523 (65.8) | 1 | 1 | - |
| Female | 1,316 (60.8) | 725 (55.1) | 1.53 (1.28-1.81) | 1,116 (58.4) | 854 (76.5) | 1.70 (1.39-2.07) | 1.40 (1.20-1.63) | <0.001 |
| Age group | ||||||||
| < 25 | 150 (6.9) | 42 (28.0) | 0.52 (0.36-0.76) | 85 (4.5) | 43 (50.6) | 0.77 (0.48-1.24) | 0.69 (0.51-0.94) | 0.020 |
| 25 to 45 | 891 (41.2) | 380 (42.7) | 1 | 404 (21.1) | 230 (56.9) | 1 | 1 | - |
| 45 to 65 | 791 (36.6) | 454 (57.4) | 1.81 (1.49-2.20) | 747 (39.1) | 592 (79.3) | 2.89 (2.22-3.76) | 1.77 (1.50-2.09) | <0.001 |
| 65+ | 332 (15.3) | 227 (68.3) | 2.91 (2.23-3.80) | 675 (35.3) | 512 (75.9) | 2.38 (1.82-3.10) | 1.89 (1.53-2.32) | <0.001 |
| Prior HT/Diabetes meds | ||||||||
| Yes | 692 (32.0) | 411 (59.4) | 1.65 (1.37-1.98) | 530 (27.7) | 448 (84.5) | 2.66 (2.05-3.45) | 1.68 (1.37-2.06) | <0.001 |
| No | 1,472 (68.0) | 692 (47.0) | 1 | 1,381 (72.3) | 929 (67.3) | 1 | 1 | - |
| Paid employment | ||||||||
| Yes | 562 (26.0) | 221 (39.3) | 1 | 109 (5.7) | 79 (72.5) | 1 | 1 | - |
| No | 1,602 (74.0) | 882 (80.0) | 1.89 (1.55-2.30) | 1,802 (94.3) | 1,298 (72.0) | 0.98 (0.63-1.51) | 1.43 (1.18-1.74) | <0.001 |
| BMI (kg/m2) | ||||||||
| Below 18 | 37 (1.7) | 25 (67.6) | 2.38 (1.18-4.81) | 108 (5.8) | 79 (73.2) | 1.18 (0.76-1.85) | 1.29 (0.87-1.92) | 0.210 |
| 18 to 25 | 845 (39.4) | 394 (46.6) | 1 | 1,089 (58.1) | 759 (69.7) | 1 | 1 | - |
| 25 to 30 | 668 (31.2) | 376 (56.3) | 1.47 (1.20-1.81) | 426 (22.7) | 342 (80.3) | 1.77 (1.35-2.32) | 1.28 (1.07-1.52) | 0.005 |
| Above 30 | 594 (27.7) | 299 (50.3) | 1.16 (0.94-1.43) | 253 (13.5) | 182 (71.9) | 1.11 (0.82-1.51) | 0.76 (0.62-0.92) | 0.006 |
| Referral reason | ||||||||
| Hypertension only | 1,899 (87.8) | 922 (48.6) | 1 | 1,741 (91.1) | 1,219 (70.0) | 1 | 1 | - |
| Diabetes only | 92 (4.3) | 55 (59.8) | 1.58 (1.03-2.41) | 80 (4.2) | 70 (87.5) | 3.00 (1.53-5.86) | 3.39 (2.20-5.21) | <0.001 |
| Both | 173 (8.0) | 126 (72.8) | 2.84 (2.01-4.02) | 90 (4.7) | 88 (97.8) | 18.84 (4.62-76.81) | 2.78 (1.97-3.94) | <0.001 |
| BP category | ||||||||
| Normal (diabetics) | 327 (15.2) | 161 (49.2) | 1.16 (0.91-1.49) | 264 (13.9) | 222 (84.1) | 2.68 (1.88-3.81) | 0.63 (0.47-0.83) | 0.001 |
| Mild | 1,243 (57.7) | 565 (45.5) | 1 | 1,094 (57.5) | 726 (66.4) | 1 | - | - |
| Moderate | 341 (15.8) | 196 (57.5) | 1.62 (1.27-2.07) | 346 (18.2) | 262 (75.7) | 1.58 (1.20-2.08) | 1.17 (0.96-1.43) | 0.111 |
| Severe | 243 (11.3) | 179 (73.7) | 3.56 (2.47-4.56) | 200 (10.5) | 162 (81.0) | 2.16 (1.49-3.14) | 1.93 (1.49-2.50) | <0.001 |
Factors associated with uptake of clinical services
Rural participants had twice the odds of attending for clinical assessment compared to urban participants after adjusting for all other factors (aOR: 2.24; 95% CI: 1.93-2.61). From both the site specific univariate analyses and the adjusted model across both sites, female sex was also strongly associated with attendance for clinical assessment (aOR: 1.40; 95% CI: 1.20-1.63). Uptake of care was also higher in older participants. Being already on hypertension or diabetes medication was also strongly associated with attendance for care (aOR: 1.68; 95% CI: 1.37-2.06) irrespective of site, as was not being in paid employment (including unemployed and subsistence farmers) (aOR: 1.43; 95%CI: 1.18-1.74) in the adjusted analysis. Within the disease categories, patients referred with diabetes or a combination of diabetes and suspected hypertension had significantly greater odds of reporting at the clinic than those with suspected hypertension alone (Table 1).
Reasons for non-attendance for clinical assessment
In the rural area 22/170 (12.9%) diabetic patients and 550/1,741 (31.6%) participants with suspected hypertension were interviewed at home after non-attendance (572 in total). 96/265 (36.2%) and 944/1,899 (49.7%) participants with diabetes and suspected hypertension respectively in the urban area were also visited (1,040 in total).
Main reasons for not taking up services at the rural site were lack of transport or distance, being too busy with work (field activities) and being away from home. At the urban site, the main reasons were accessing care at other facilities, being at work (busy) and being away from home (Table 2). Of those visited, 214/570 (37%) at the rural site and 258 (25%) at the urban did attend for clinical assessment following the home visit.
Table 2. Main reasons for non-attendance by site.
| Reason for non-attendance | Lilongwe (1,040† participants) | Karonga (572† participants) |
|---|---|---|
| Attend other facility | 149 (14.3%) | 47 (8.2%) |
| Plan to go later | 82 (7.9%) | 68 (11.9) |
| Busy at work | 220 (21.2%) | 67 (11.7%) |
| Transport costs/distance | 0 (0%) | 118 (20.6%) |
| Away for some time | 109 (10.5%) | 74 (12.9%) |
| Feeling healthy | 39 (3.8%) | 29 (5.1%) |
| Too sick/old | 18 (1.7%) | 34 (5.9%) |
| Other (e.g. feeling healthy) | 280 (26.9%) | 126 (22.0%) |
| Missing | 338 (32.5%) | 137 (24.0%) |
Participants could give more than one reason for non-attendance resulting in total percentages above 100
Retention in care
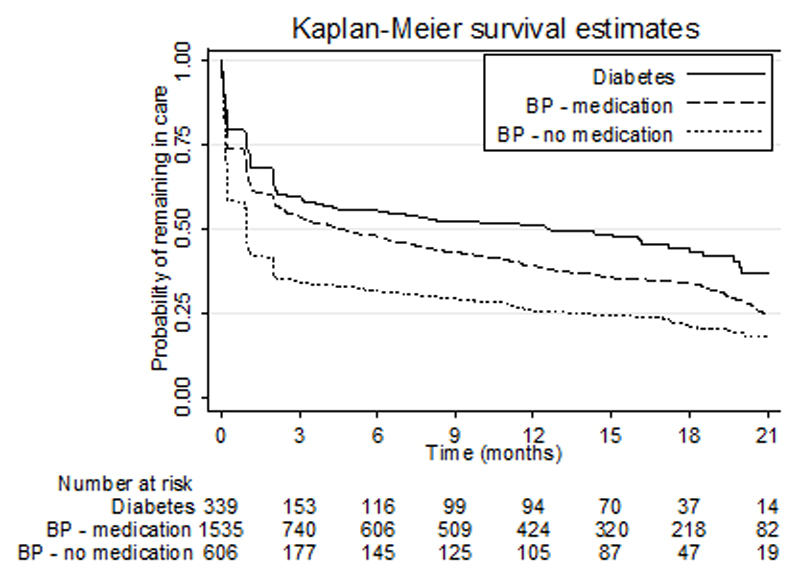
Of the 2,480 attending for clinical assessment, based on observations at the clinics 1,551 (62.5%) were started on medication for diabetes and/or hypertension on the first visit, based on survey FBG or repeat BP measurement at clinic. The remaining 929 (37.5%) were given lifestyle advice and asked to return for repeat measurements according to treatment guidelines. 501/929 (53.9%) of those on lifestyle advice did not have BP above 140/90 mmHg when repeat measurements were made at the clinic.
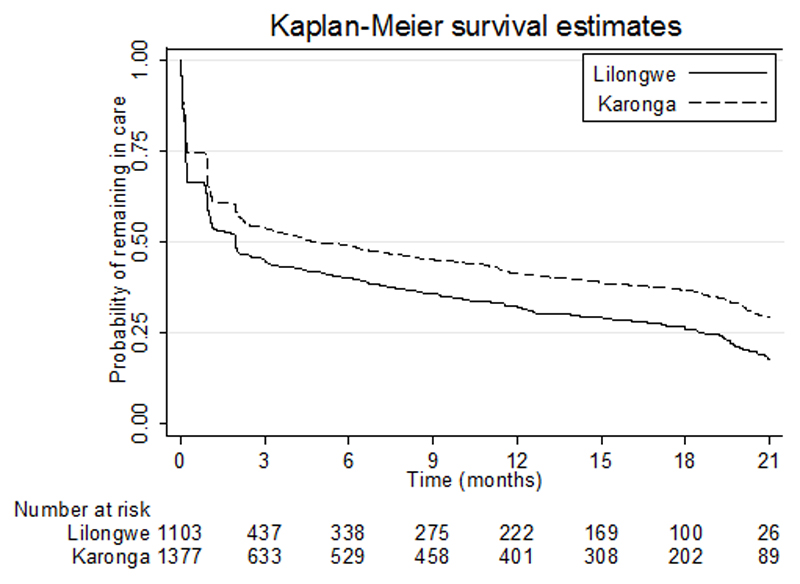
At both sites, more than 25% of all participants expected still to be in care were retained (and were no more than 30 days late for any scheduled appointment) by 18 months after the initial assessment and enrolment in care at the rural and urban sites, Figure 2. The retention patterns differed among the three groups; highest among those with diabetes; followed by participants with raised BP on clinical assessment (excluding those with diabetes), and those with only slightly raised BP on the clinical assessment (excluding those with diabetes) (Figure 3). Factors associated with drop-out (failure to be retained in care) included area of residency (rural compared to urban, aHR: 0.76; 95% CI: 0.68-0.84), younger age and not being on medication prior to screening and referral, Table 3. Unlike with the uptake, sex, employment and BMI were all not associated with failure to be retained in care. The rural urban differences were only apparent before 3 months, thereafter the drop-out was equal across sites (Figure 2)
Figure 2.
Retention in care by site over time
Figure 3.
Retention in care following clinical assessment by reason for continuing care
Table 3. Hazard Ratios (HRs) for factors associated with drop-out after clinical assessment and adjusted Odds Ratios (aHRs) for both sites.
| Diabetes (+/− hypertension) | Hypertension | BP not raised on repeat measurement at clinic | Overall drop-out | ||
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | aHR (95% CI) | p-value | |
| Diagnosis | |||||
| Diabetes | 1 | - | |||
| BP medication | 1.08 (0.91-1.28) | 0.374 | |||
| BP no medication | 1.65 (1.38-1.98) | <0.001 | |||
| Site | |||||
| Lilongwe | 1 | 1 | 1 | 1 | - |
| Karonga | 0.72 (0.53-0.99) | 0.77 (0.68-0.87) | 0.72 (0.60-0.87) | 0.76 (0.68-0.84) | <0.001 |
| Sex | |||||
| Male | 1 | 1 | 1 | 1 | - |
| Female | 1.11 (0.80-1.54) | 0.80 (0.70-0.91) | 0.79 (0.65-0.95) | 0.92 (0.83-1.01) | 0.092 |
| Age group | |||||
| < 25 | 0.87 (0.21-3.55) | 1.85 (1.30-2.62) | 1.05 (0.72-1.53) | 1.19 (0.92-1.53) | 0.182 |
| 25 to 45 | 1 | 1 | 1 | 1 | - |
| 45 to 65 | 0.55 (0.39-0.78) | 0.67 (0.57-0.79) | 0.66 (0.53-0.81) | 0.74 (0.65-0.84) | <0.001 |
| 65+ | 0.44 (0.28-0.69) | 0.60 (0.50-0.71) | 0.49 (0.38-0.65) | 0.69 (0.60-0.80) | <0.001 |
| Prior HT/Diabetes meds | |||||
| Yes | 0.49 (0.36-0.67) | 0.53 (0.46-0.61) | 0.36 (0.28-0.45) | 0.49 (0.43-0.55) | <0.001 |
| No | 1 | 1 | 1 | 1 | - |
| BMI (kg/m2) | |||||
| Below 18 | 2.20 (0.79-6.10) | 1.01 (0.75-1.37) | 1.03 (0.66-1.61) | ||
| 18 to 25 | 1 | 1 | 1 | ||
| 25 to 30 | 1.03 (0.71-1.50) | 0.84 (0.72-0.97) | 1.03 (0.83-1.28) | ||
| Above 30 | 0.80 (0.54-1.18) | 0.87 (0.73-1.04) | 0.82 (0.63-1.07) | ||
| Paid employment | |||||
| Yes | 1 | 1 | 1 | ||
| No | 0.85 (0.57-1.29) | 0.75 (0.62-0.91) | 0.82 (0.63-1.08) | ||
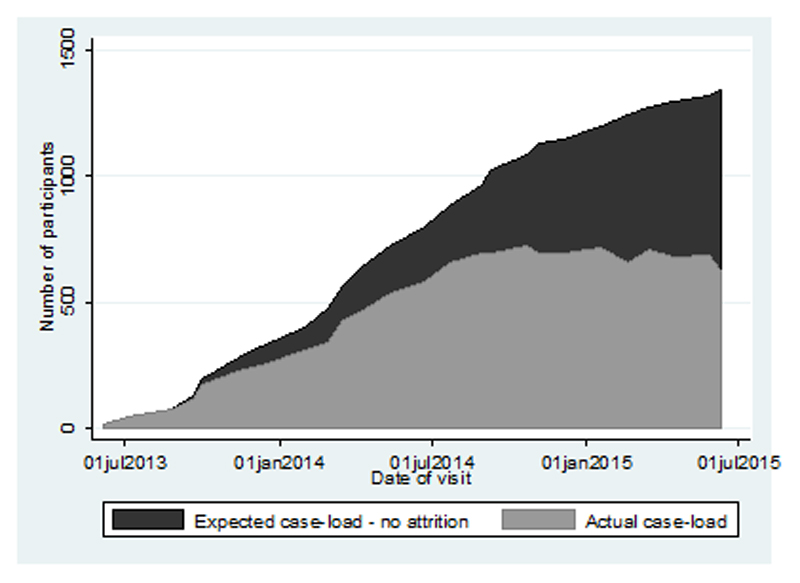
Examining those in contact with the clinic 24 months into the chronic care programme, 631 (47.0%) of individuals started on antihypertensive medication were still in contact with the CCC out of a cumulative 1,343 (Figure 4), and thus still able to be screened for complications and monitored for outcomes, and contributing to clinic case-load. However, some would have missed appointments or been absent from clinic for up to six months.
Figure 4.
Clinic case-load over time, expected and actual, for patients started on anti-hypertensive medication
Over the duration of the study, the median number of participants enrolled each month was 51 (IQR: 32 – 77) while the median monthly clinic attendance including assessment and follow-up visits was 512 (IQR: 205 – 650).
Discussion
Efforts at implementing mass screening programmes and care interventions in SSA have yielded mixed results. We discuss our own experiences from setting up a large screening and care programme for NCDs with comparisons made in uptake and retention of services in urban and rural settings.
The uptake of care following the screening was higher at the rural site compared to the urban site. The reasons for this discrepancy may include the urban population having more options for accessing care (besides the facility they were referred to) than in the rural site. The CRH is the only health facility equipped to manage hypertensive and diabetic patients in Karonga apart from the district hospital which is 80 kilometres away. Other studies have highlighted ease of access to care as one of the challenges to uptake of care. In addition, urban dwellers, especially men, were hard to screen and even when screened and enrolled in care would miss appointments due to work commitments or other behavioural traits.20 Comparatively, uptake of clinical services for hypertension in rural Uganda was 83% – higher than that in our setting at both sites – with older age, female gender and hypertension family history as the associated factors. This, was however, after participants were given travel vouchers for a clinic appointment.25
More females than males were screened and referred for further management at both sites, due to lower participation rates in men. However, even on adjustment women were more likely to take up referrals than men.
With respect to age, there were similar patterns in uptake in both rural and urban settings. The reasons for this are again unclear in this setting but could include the older participants being more concerned about the health consequence of their condition, less able to afford alternative care or having more time to travel to appointments.
Participants already on medication may have found the screening programme as an opportunity to access care for these conditions within their communities and at a clinic where drug supply was guaranteed.
There were contrasting results in uptake with respect to employment. In Lilongwe, uptake was lower among those in salaried employment, while in Karonga employment status was not associated with uptake of care. The salaried are in a financial position to access care in other private health facilities (though health insurance or self-funding) than the unemployed in the urban setting. For the rural setting, with CRH being the only place where management of such conditions is possible, participants would have little choice but to go to this facility regardless of their economic standing.
The perceived seriousness of a health condition influences care-seeking behaviour. This can be seen in the better attendance associated with higher levels of BP on screening. The survey team explained the meaning of category of screened BP (mild, moderate and severe hypertension) and were asked to refer those with severe hypertension urgently. Those referred to care for diabetes or diabetes and hypertension showed better uptake of care at both sites than those with hypertension only (even after adjusting for age and sex). This could also be a result of the perceived seriousness of diabetes as a condition.
Drop-out was lower at the rural site regardless of enrolment reason. We did not investigate reasons for attrition among the rural and urban populations although these may be similar to the reasons for failure in uptake i.e. distance/transport costs in the rural and other care facilities at the urban site. It is interesting that in the rural area there was better retention, despite, the cost of repeated visits to the health facility (at a much greater distance than in the urban area) in a predominantly subsistence economy which makes long-term attendance challenging. This might reflect the fact that CRH was the only site providing such care and the rural community being more compliant in general and having a longer and more trusting relationship with the research organisation. The urban population would also have other treatment options (other nearer/more accessible clinics) if they wished to continue care.
Similar challenges have been reported in setting up NCDs care services in urban Africa, with data from slum dwellers of Nairobi in Kenya showing high dropout and non-compliance rates.26 Even in rural Cameroon, integrating hypertension and diabetes care in non-physician clinics proved feasible but was hampered by low case-detection rates and high attrition among patients enrolled into care.27 As with uptake of care, older people were more likely to remain in care than younger participants following enrolment. Similarly, people who were already on medication prior to screening had higher retention rates regardless of the final diagnosis at enrolment, which may reflect self-selection of those already willing to take long-term medication.
The management of hypertension and diabetes in a primary care setting within an informal settlement showed good retention (68% alive and in care) in Nairobi, Kenya 6. Our findings here show that while the retention was lower than that reported by in Kenya, as the majority of those started on medication were retained, it may yet have an important clinical impact. Already, some interventions to improve retention rates for cardiovascular disease in Cameroon via task-shifting in nurse-led rural facilities have seen improved retention rates in cardiovascular disease. This was, however, after sending out reminder letters following missed appointments.28 A newly rolled out study aims to investigate use of smartphone technology among community health workers as a strategy to optimize linkage and retention to hypertension care in rural Kenya, and thus, NCD management in low- and middle-income countries.29 This, along with other efforts within SSA will provide more insight and lessons on possible strategies that might be employed in future to ensure the success of screening and care programmes for NCDs.
Previous studies have given inconsistent results about the benefits of mass screening for NCDs like hypertension and/or diabetes, and a recent systematic review concluded that untargeted screening had no benefits in resource-limited settings.30 However, the reasons for this lack of success are unclear, but likely to be complex. One element might relate to barriers in linking individuals identified to have high risk or overt disease to care services. Our data show that it is feasible to link a screening programme and a clinical service system in poor resource country settings, with a reasonable uptake of the services. We will continue to explore whether this translates into improved outcomes at a population level.
Perspectives.
We designed and implemented a large screening and care programme for hypertension and diabetes in urban and rural Malawi. Screening for hypertension and diabetes identified large numbers of individuals requiring further clinical assessment, although a large proportion will not take up, or continue to access, care. Uptake of services and retention in care were better at the rural compared to the urban site and amongst women and older people. Services may need to be made more accessible to employed urban men. The longer term clinical outcomes and cost-effectiveness of this programme remain to be examined.
Novelty and Significance.
What Is New?
Little little is known about the long-term outcomes among adults diagnosed with hypertension and/or diabetes following screening and enrolled in care in SSA.
What Is Relevant?
The effectiveness of screening and care programmes and including observed patterns between rural and urban settings.
Summary.
Our findings highlight better uptake and retention of services at the rural site compared to the urban population which can access care at other facilities.
Acknowledgments
We thank the Karonga and Lilongwe participants including traditional leaders for welcoming and taking part in this research programme. We are also grateful for the support from our partners at MoH headquarters at the Karonga and Lilongwe District Health Offices.
Sources of funding
The study was funded by the Wellcome Trust supplemented by CIPLA who provided oral drugs for both hypertension and diabetes at the CCCs.
Footnotes
Conflicts of Interest/Disclosures
All the authors report no conflicts of interest or disclosures.
References
- 1.Streatfield PK, Khan WA, Bhuiya A, et al. Adult non-communicable disease mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014;7:25365. doi: 10.3402/gha.v7.25365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Noncommunicable Diseases Country Profiles 2014. [Accessed 09 February 2016]; [ONLINE] Available at: http://www.who.int/nmh/publications/ncd-profiles-2014/en/.
- 3.Duboz P, Boëtsch G, Gueye L, Macia E. Hypertension prevalence, awareness, treatment and control in Dakar (Senegal) J Hum Hypertens. 2014;28:489–493. doi: 10.1038/jhh.2013.142. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014;43:116–128. doi: 10.1093/ije/dyt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peck R, Mghamba J, Vanobberghen F, Kavishe B, Rugarabamu V, Smeeth L, Hayes R, Grosskurth H, Kapiga S. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. Lancet Glob Health. 2014;2:e285–92. doi: 10.1016/S2214-109X(14)70033-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sobry A, Kizito W, Van den Bergh R, Tayler-Smith K, Isaakidis P, Cheti E, Kosgei RJ, Vandenbulcke A, Ndegwa Z, Reid T. Caseload, management and treatment outcomes of patients with hypertension and/or diabetes mellitus in a primary health care programme in an informal setting. Trop Med Int Health. 2014;19:47–57. doi: 10.1111/tmi.12210. [DOI] [PubMed] [Google Scholar]
- 7.Peltzer K, Phaswana-Mafuya N. Hypertension and associated factors in older adults in South Africa. Cardiovasc J Afr. 2013;24:67–71. doi: 10.5830/CVJA-2013-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bosu WK. A comprehensive review of the policy and programmatic response to chronic non-communicable disease in Ghana. Ghana Med J. 2012;46:69–78. [PMC free article] [PubMed] [Google Scholar]
- 9.Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. The Lancet. 2010;375:2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 10.Adebayo RA, Balogun MO, Adedoyin RA, Obashoro-John OA, Bisiriyu LA, Abiodun OO. Prevalence of hypertension in three rural communities of Ife North Local Government Area of Osun State, South West Nigeria. Int J Gen Med. 2013;6:863–8. doi: 10.2147/IJGM.S51906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akinyemi RO, Izzeldin IM, Dotchin C, et al. Contribution of noncommunicable diseases to medical admissions of elderly adults in Africa: a prospective, cross-sectional study in Nigeria, Sudan, and Tanzania. J Am Geriatr Soc. 2014;62:1460–1466. doi: 10.1111/jgs.12940. [DOI] [PubMed] [Google Scholar]
- 12.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–975. doi: 10.1097/hjh.0b013e3283282f65. [DOI] [PubMed] [Google Scholar]
- 13.Tibazarwa KB, Damasceno AA. Hypetension in developing countries. Can J Cardiol. 2014;30:527–533. doi: 10.1016/j.cjca.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Iwelunmor J, Airhihenbuwa CO, Cooper R, Tayo B, Plange-Rhule J, Adanu R, Ogedegbe G. Prevalence, determinants and systems-thinking approaches to optimal hypertension control in West Africa. Global Health. 2014;10:42. doi: 10.1186/1744-8603-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62:18–26. doi: 10.1161/HYPERTENSIONAHA.113.01374. [DOI] [PubMed] [Google Scholar]
- 16.Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, Hsu J, Martiniuk A, Celletti F, Patel K, Adshead F, et al. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376:1785–1797. doi: 10.1016/S0140-6736(10)61353-0. [DOI] [PubMed] [Google Scholar]
- 17.Bowie C. The burden of diseases in Malawi. Malawi Medical Journal. 2006;18:103–110. [PMC free article] [PubMed] [Google Scholar]
- 18.Msyamboza KP, Kathyola D, Dzowela T, Bowie C. The burden of hypertension and its risk factors in Malawi: nationwide population-based STEPS survey. Int Health. 2012;4:246–252. doi: 10.1016/j.inhe.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Msyamboza KP, Ngwira B, Dzowela T, Mvula C, Kathyola D, Harries AD, Bowie C. The burden of selected chronic non-communicable diseases and their risk factors in Malawi: nationwide STEPS survey. PLoS One. 2011;6:e20316. doi: 10.1371/journal.pone.0020316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crampin AC, Kayuni N, Amberbir A, et al. Hypertension and diabetes in Africa: design and implementation of a large population-based study of burden and risk factors in rural and urban Malawi. Emerg Themes Epidemiol. 2016;13:3. doi: 10.1186/s12982-015-0039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amberbir A, Kayuni N, Tafatatha T, Musicha C, Chirwa V, Mwagomba B, Price A, Koole O, Crampin AC, Jaffar S, Nyirenda MJ. High blood pressure in Africa: findings from a large cross-sectional study in urban and rural Malawi. Journal of Hypertension e-Supplement 1. 2014;32:25.41. [Google Scholar]
- 22.Amberbir A, Kayuni N, Tafatatha T, Musicha C, Chirwa V, Mwagomba B, Price A, Koole O, Crampin AC, Jaffar S, Nyirenda MJ. Prevalence and metabolic risk factors of diabetes and pre-diabetes in Malawi. Journal of Hypertension e-Supplement 1. 2014:32. [Google Scholar]
- 23.National Statistical Office. Population and Housing Census Preliminary Report, 2008. [Accessed 09 February 2016]; [ONLINE] Available at: http://www.malawihighcommission.co.uk/MWCensus08.pdf.
- 24.Crampin AC, Dube A, Mboma S, et al. Profile: the Karonga Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:676–685. doi: 10.1093/ije/dys088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotwani P, Balzer L, Kwarisiima D, et al. Evaluating linkage to care for hypertension after community-based screening in rural Uganda. Trop Med Int Health. 2014;19:459–468. doi: 10.1111/tmi.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Werner ME, van de Vijver S, Adhiambo M, Egondi T, Oti SO, Kyobutungi C. Results of a hypertension and diabetes treatment program in the slums of Nairobi: a retrospective cohort study. BMC Health Serv Res. 2015;15:512. doi: 10.1186/s12913-015-1167-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Labhardt ND, Balo JR, Ndam M, Grimm JJ, Manga E. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Serv Res. 2010;10:339. doi: 10.1186/1472-6963-10-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Labhardt ND, Balo JR, Ndam M, Manga E, Stoll B. Improved retention rates with low-cost interventions in hypertension and diabetes management in a rural African environment of nurse-led care: a cluster-randomised trial. Trop Med Int Health. 2011;16:1276–84. doi: 10.1111/j.1365-3156.2011.02827.x. [DOI] [PubMed] [Google Scholar]
- 29.Vedanthan R, Kamano JH, Naanyu V, et al. Optimizing linkage and retention to hypertension care in rural Kenya (LARK hypertension study): study protocol for a randomized controlled trial. Trials. 2014;15:143. doi: 10.1186/1745-6215-15-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Durão S, Ajumobi O, Kredo T, Naude C, Levitt NS, Steyn K, Bradshaw D, Young T. Evidence insufficient to confirm the value of population screening for diabetes and hypertension in low- and-middle-income settings. S Afr Med J. 2015;105:98–102. doi: 10.7196/samj.8819. [DOI] [PubMed] [Google Scholar]