The article describes the types of thought processes used during medical decision making; emphasizes the cognitive biases inherent in these ways of thinking, which can lead to diagnostic error; and reviews cognitive and systemic strategies to combat these biases to reduce diagnostic error.
Abstract
Medical errors are a leading cause of morbidity and mortality in the medical field and are substantial contributors to medical costs. Radiologists play an integral role in the diagnosis and care of patients and, given that those in this field interpret millions of examinations annually, may therefore contribute to diagnostic errors. Errors can be categorized as a “miss” when a primary or critical finding is not observed or as a “misinterpretation” when errors in interpretation lead to an incorrect diagnosis. In this article, the authors describe the cognitive causes of such errors in diagnostic medicine, specifically in radiology. Recognizing the cognitive processes that radiologists use while interpreting images should improve one’s awareness of the inherent biases that can impact decision making. The authors review the common biases that impact clinical decisions, as well as strategies to counteract or minimize the potential for misdiagnosis. System-level processes that can be implemented to minimize cognitive errors are reviewed, as well as ways to implement personal changes to minimize cognitive errors in daily practice.
©RSNA, 2017
SA-CME LEARNING OBJECTIVES
After completing this journal-based SA-CME activity, participants will be able to:
■ Discuss the types of cognitive processes radiologists use when interpreting cases.
■ Recognize the types of biases that can affect radiologic interpretation.
■ Describe cognitive and systemic solutions to implement in reading rooms and departments to minimize radiologic misses and misinterpretations.
Introduction
Medical errors are a substantial cause of morbidity and mortality. Estimates of the annual occurrence of medical errors range from 44 000 to 400 000 (1,2), with higher estimates ranking medical errors as the third leading cause of death in the United States (2). In addition, medical errors contribute to unnecessary medical spending, with estimated costs ranging between $17 billion and $29 billion (U.S. dollars) annually (1).
Medical errors can be categorized and can include diagnostic errors, treatment errors, preventive errors, and other errors (eg, communication failures, equipment failures, and other system failures) (1). In radiology, most medical errors are categorized as diagnostic errors or other errors (3). Diagnostic errors can be defined as errors that result in incorrect, delayed, or missed diagnoses (3). In malpractice lawsuits filed against radiologists, approximately 75% of lawsuits relate to diagnostic errors (3), and 38% of money paid in general malpractice lawsuits results from diagnostic errors (4).
Radiologists were first made aware of the high rates of diagnostic errors within the field in 1959, when an article by Garland (5) reported a 32% retrospective error rate in the interpretation of abnormal chest radiographs and an average daily error rate of 3%–4% when negative studies were included; subsequent studies have demonstrated that these high error rates persist, despite decades of intervention (5–7). Thirty percent of these retrospective errors represented misses of positive findings, and 2% represented misinterpretations, specifically false-positive diagnoses of diseases that had not manifested (5). In this article, we describe the cognitive biases that contribute to diagnostic errors to help radiologists accept mistakes and learn from them.
Type 1 and Type 2 Thinking
It is important for a radiologist to understand human decision making and the context in which cognitive biases occur. A 1974 article by psychologists Tversky and Kahneman (8) established the basis for current theories about human decision making and judgment. They theorized that individuals process information and make estimates and choices through the use of heuristics (8). Heuristics, also known as intuitive thought processes, are “highly economical” ways of thinking that allow for rapid—almost reflexive—decision making with limited information (8). Although heuristic techniques are common and are usually effective, they are subject to biases that can lead to diagnostic errors (8).
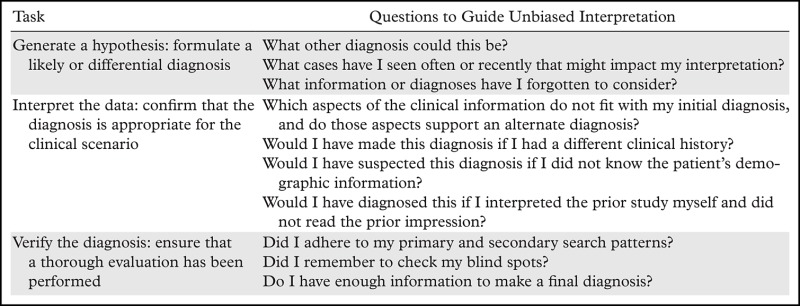
Heuristics, also known as system 1, type 1, or fast thinking, describe the ability of the brain to think and act intuitively (9). Type 1 thinking requires continuous work (8–10) (Table 1), as humans consciously experience less than 1% of the information the senses can process (approximately 400 billion bits of information per second) (11). Experienced radiologists may reach a diagnosis without much conscious deliberation using a variety of heuristic techniques; however, heuristics may fail due to inherent errors called biases (12).
Table 1:
Key Characteristics of the Dual Process Theory of Reasoning
In comparison with type 1 thinking, type 2 thinking, or system 2, is an analytical, slow, deliberate, and effortful approach to decision making (9,10). Type 2 thinking takes over when situations become difficult, and it is more likely than type 1 thinking to help the radiologist determine the correct diagnosis (9,10).
For example, a first-year radiology resident may carefully review an abdominal computed tomography (CT) study and consciously think about each structure in a checklist (lung bases, liver, spleen, etc). Such a review (using type 2 thinking) may take 45 minutes to 1 hour. In contrast, a fourth-year resident on an evening call shift, who has internalized this checklist, may read the same study in 5–10 minutes, using a greater degree of type 1 thinking. Even if type 2 thinking takes over, the fourth-year resident remains influenced by type 1 thinking, which includes heuristics and cognitive biases (9).
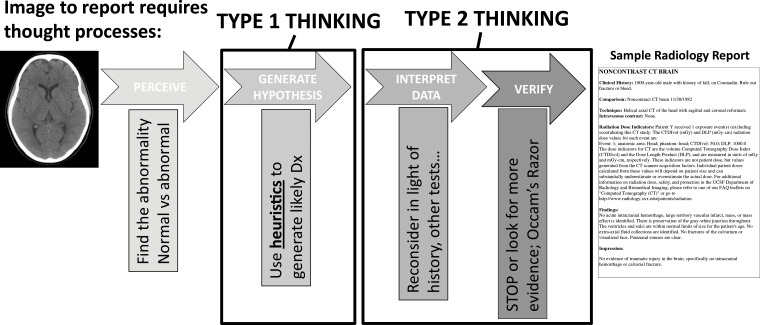
Complex decision making requires a combination of type 1 and type 2 thinking (10). A radiologist must acknowledge his or her susceptibility to cognitive biases, which can result from type 1 thinking, when developing a thought process that incorporates both types of thinking to make diagnoses and generate reports (Fig 1).
Figure 1.
Drawing shows the types of thinking used during each step of the radiologic review process, from image interpretation to radiology report formation. Understanding how one thinks about a case can help a radiologist learn how he or she may think incorrectly. Dx = diagnosis.
Cognitive Biases
Both heuristics and biases are concepts from behavioral decision theory, which can explain errors in diagnostic reasoning and judgment. When engaged in type 1 thinking, radiologists employ heuristics to make decisions quickly, subjecting themselves to cognitive biases. Many biases reflect faulty reasoning that may result from using heuristics. Since the original explanation of heuristics was published, at least 30 biases that impact human decision making have been recognized (13).
An individual can evaluate his or her own thought process, also known as metacognition, which provides an opportunity to combat bias. First introduced in 1979 by Flavell (14), metacognition is described as “thinking about thinking” (15). This multifactorial process involves (a) acknowledging the limitations of memory, (b) seeking perspective while making decisions, (c) being able to self-critique, and (d) choosing strategies to prevent cognitive error (15). Many of the strategies used to avoid bias that we describe are also known as cognitive forcing strategies, which are mental tools used to force unbiased decision making (15).
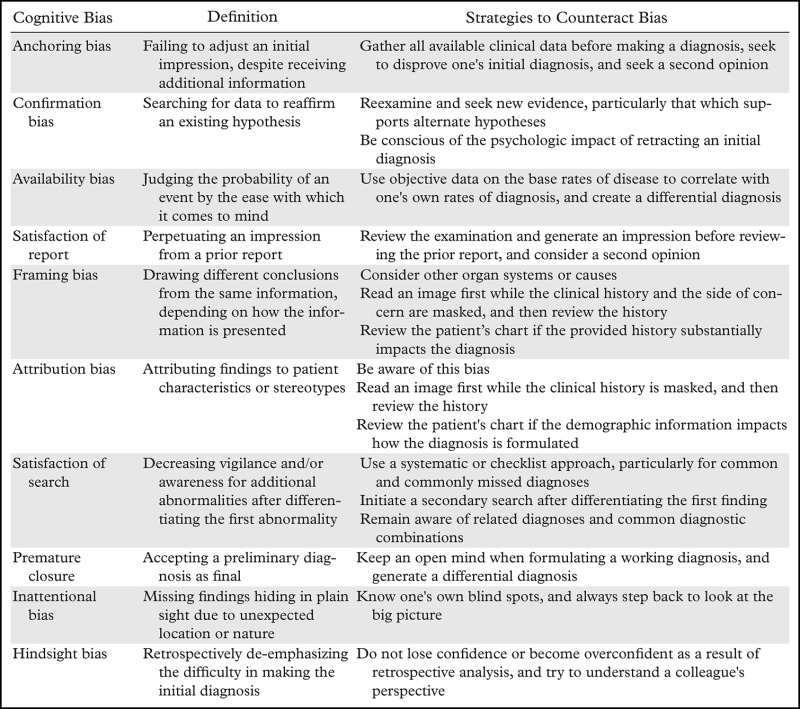
In this article, we describe 10 of the most common biases (Table 2) that impact radiologic decision making and provide illustrative case examples. In addition, we discuss cognitive forcing and metacognitive strategies to avoid bias and provide summary questions for radiologists to consider before signing a report.
Table 2:
Types of Cognitive Biases
Anchoring Bias
Anchoring bias describes a situation in which one remains fixed to his or her initial diagnostic impression, despite being presented with additional subsequent contrary information (3,13,16,17). Information presented early in a case tends to be inappropriately weighted during decision making (16). The failure to change diagnostic probability despite conflicting new information was previously called conservatism. This bias can be particularly damaging when combined with confirmation bias (discussed in the following section) (Fig 2) (13), and it can delay reaching the correct diagnosis.
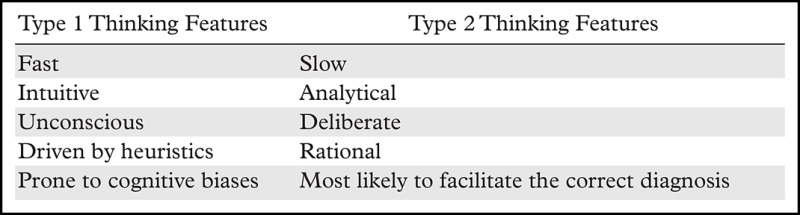
Figure 2a.
Anchoring bias confounded by confirmation bias. A 17-month-old girl presented with 1.5 months of intermittent leg pain and the inability to walk and reversion to crawling during the past month. (a) Frontal radiograph of the proximal left tibial metaphysis shows periosteal reactions (arrows), which were suspicious for malignancy. A calcific fragment (arrowhead) adjacent to the distal left femoral metaphysis was described as a likely developmental variant spur rather than a classic metaphyseal lesion, which would raise concern for nonaccidental trauma. Magnetic resonance (MR) imaging was recommended. (b) Coronal gadolinium-enhanced fat-saturated spoiled gradient-echo T1-weighted MR image shows periosteal enhancement (arrowheads) in the proximal left tibia. Absence of bone marrow edema or enhancement in the distal left femur was reassuring that the finding was a normal variant and not a sequel of trauma. (c) Axial CT image of the proximal left tibia shows a guided biopsy. Results of the biopsy helped confirm a healing fracture. In this case, the radiologist continued to pursue imaging and intervention that would support the initial diagnosis of malignancy.
Figure 2b.
Anchoring bias confounded by confirmation bias. A 17-month-old girl presented with 1.5 months of intermittent leg pain and the inability to walk and reversion to crawling during the past month. (a) Frontal radiograph of the proximal left tibial metaphysis shows periosteal reactions (arrows), which were suspicious for malignancy. A calcific fragment (arrowhead) adjacent to the distal left femoral metaphysis was described as a likely developmental variant spur rather than a classic metaphyseal lesion, which would raise concern for nonaccidental trauma. Magnetic resonance (MR) imaging was recommended. (b) Coronal gadolinium-enhanced fat-saturated spoiled gradient-echo T1-weighted MR image shows periosteal enhancement (arrowheads) in the proximal left tibia. Absence of bone marrow edema or enhancement in the distal left femur was reassuring that the finding was a normal variant and not a sequel of trauma. (c) Axial CT image of the proximal left tibia shows a guided biopsy. Results of the biopsy helped confirm a healing fracture. In this case, the radiologist continued to pursue imaging and intervention that would support the initial diagnosis of malignancy.
Anchoring bias is rooted in anchoring effect, which is the tendency to place undue influence on the information provided when initially faced with a decision (18). For example, if a group is asked if the length of the Golden Gate Bridge is more or less than 2500 m and is then asked to estimate the exact length of the bridge, the group’s answer will be clustered around the provided information of 2500 m, regardless of whether or not this is an accurate measurement (18).
Strategies to Combat Anchoring Bias.—One should avoid formulating a diagnosis before reviewing pending relevant clinical data (13). Radiologists should be aware of the tendency to anchor in an early decision (13) and should always seek to disprove an initial diagnosis (3,16,17). If clinical symptoms progress or otherwise do not fit the diagnosis, one should seek a second opinion (13).
Questions to Ask Yourself.—What else could this be? What have I forgotten to consider?
Confirmation Bias
Confirmation bias describes when one actively searches for data to confirm a specific hypothesis rather than searching for data that facilitate efficient testing of a competing hypothesis (13,16,19). This can include ordering more tests to increase confidence in a diagnosis, even if the new data do not alter the probability of the diagnosis (13). It can also result in a delayed diagnosis, the inappropriate use of medical resources, or potentially unnecessary invasive procedures (Fig 2c). This bias impacts decision making (13), as reaffirming or disproving one’s diagnosis can have a psychologic impact on the provider (13,19).
Figure 2c.
Anchoring bias confounded by confirmation bias. A 17-month-old girl presented with 1.5 months of intermittent leg pain and the inability to walk and reversion to crawling during the past month. (a) Frontal radiograph of the proximal left tibial metaphysis shows periosteal reactions (arrows), which were suspicious for malignancy. A calcific fragment (arrowhead) adjacent to the distal left femoral metaphysis was described as a likely developmental variant spur rather than a classic metaphyseal lesion, which would raise concern for nonaccidental trauma. Magnetic resonance (MR) imaging was recommended. (b) Coronal gadolinium-enhanced fat-saturated spoiled gradient-echo T1-weighted MR image shows periosteal enhancement (arrowheads) in the proximal left tibia. Absence of bone marrow edema or enhancement in the distal left femur was reassuring that the finding was a normal variant and not a sequel of trauma. (c) Axial CT image of the proximal left tibia shows a guided biopsy. Results of the biopsy helped confirm a healing fracture. In this case, the radiologist continued to pursue imaging and intervention that would support the initial diagnosis of malignancy.
Strategies to Combat Confirmation Bias.—When formulating a diagnosis, one should continually reexamine evidence, particularly that which supports alternate hypotheses (19), to avoid confirmation bias. Similar to the methods used to avoid anchoring bias, a radiologist should be aware of the tendency toward confirmation bias (13) and actively pursue evidence to disprove the initial diagnosis. One should not fall subject to pseudodiagnostic effect, which occurs when diagnostic information of no statistical significance is taken into consideration to support a diagnosis (13).
In addition, one should be conscious of the psychologic impact of retracting an initial diagnosis, and he or she should not let that prevent the pursuit of alternate diagnoses if the clinical progression does not fit the initial diagnosis (19).
Questions to Ask Yourself.—What aspects of the clinical information do not fit with my initial diagnosis? Does that support an alternate diagnosis?
Availability Bias
Availability bias is defined as judging the probability of an event by the ease with which examples come to one’s mind (3,13,16,17,19). As eloquently noted in Rhetorica ad Herennium, written in 85 bc, “the striking and the novel stay longer in the mind.”
Availability bias can result in a decreased sensitivity to entities not seen for a while and an increased sensitivity to recently seen entities (Fig 3) (13). This is also true for a diagnosis that may have been a miss, which is colloquially referred to as an "I got burned once (IGBO)" case (3,13,16,17,20). Availability bias can exert inappropriate influence on physicians’ presumed rates of disease prevalence (13). Conversely, nonavailability bias describes diagnoses not recently seen by a physician, such as rare disease entities (colloquially called “zebras”), which are not considered and therefore are underdiagnosed (13).
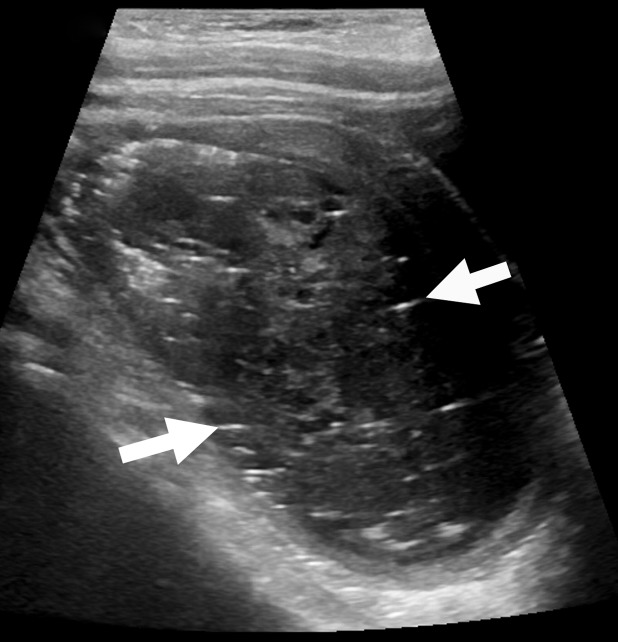
Figure 3a.
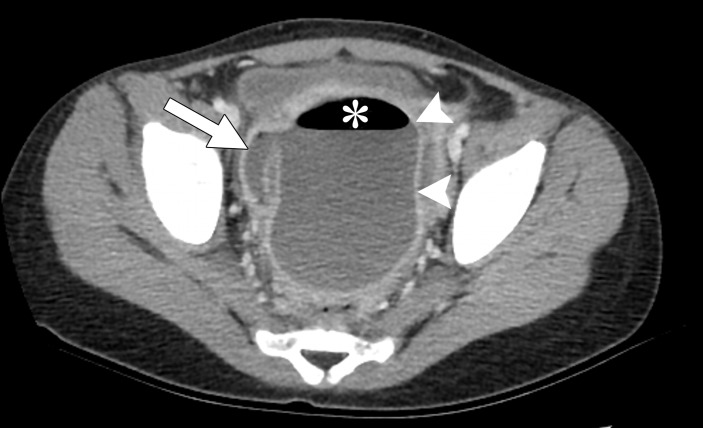
Availability bias. A 6-year-old girl presented with a 10-day history of abdominal pain and mild fever. (a) Sagittal ultrasonographic (US) image of the pelvis shows a lesion with linear echoes (arrows), heterogeneous echotexture, and echogenic foci. The interpreting radiologist, who had recently given a lecture on the imaging features of teratomas, diagnosed a teratoma. The patient’s fever and white blood cell count increased, and the pain persisted. (b) Axial contrast material–enhanced CT image of the pelvis shows a rim-enhancing collection (arrowheads) with air (*), connecting to the appendix (arrow). The patient was diagnosed with ruptured appendicitis with a pelvic abscess.
Figure 3b.
Availability bias. A 6-year-old girl presented with a 10-day history of abdominal pain and mild fever. (a) Sagittal ultrasonographic (US) image of the pelvis shows a lesion with linear echoes (arrows), heterogeneous echotexture, and echogenic foci. The interpreting radiologist, who had recently given a lecture on the imaging features of teratomas, diagnosed a teratoma. The patient’s fever and white blood cell count increased, and the pain persisted. (b) Axial contrast material–enhanced CT image of the pelvis shows a rim-enhancing collection (arrowheads) with air (*), connecting to the appendix (arrow). The patient was diagnosed with ruptured appendicitis with a pelvic abscess.
Strategies to Combat Availability Bias.—The reader should use objective data on the base rates of disease, when available, and correlate them with the frequency with which he or she observes this disease (3,13). One should be aware of this tendency (3,13) and always create a differential diagnosis before diagnosing a patient with an IGBO diagnosis or an otherwise recent or memorable diagnosis.
Question to Ask Yourself.—What cases have I seen often or recently that might impact my interpretation of this study?
Satisfaction of Report
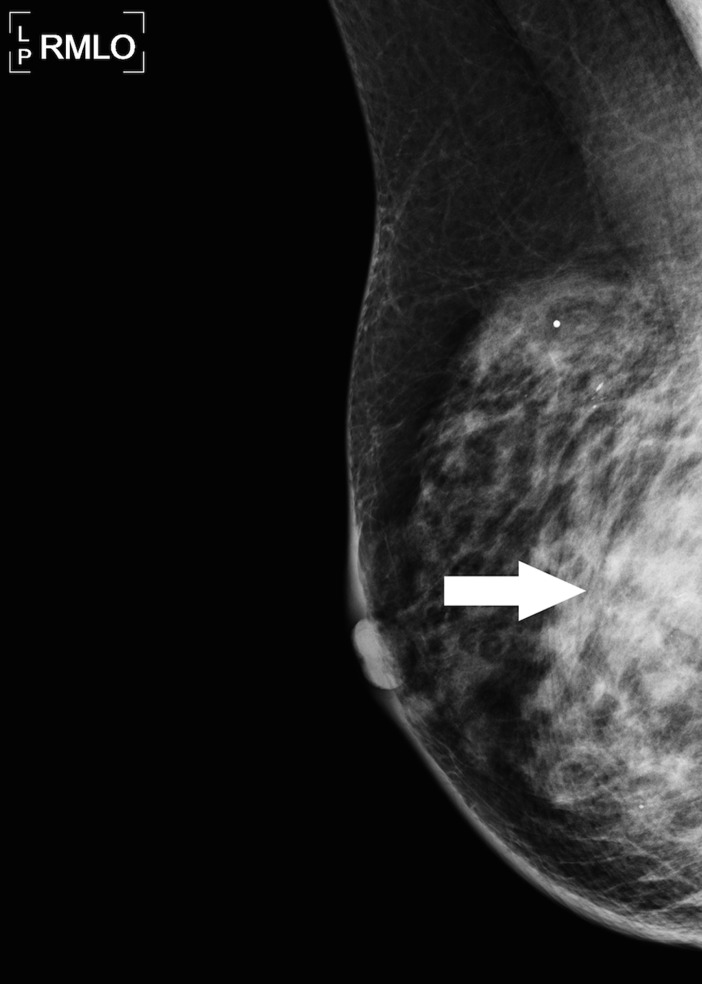
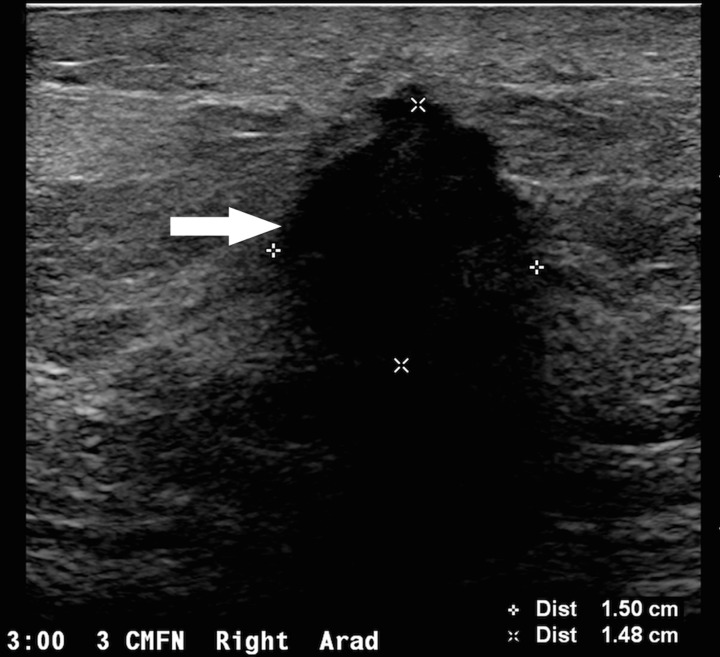
Also referred to as alliterative error, satisfaction of report is the tendency to perpetuate an impression written in a prior report (Fig 4a–4d), whether it is a colleague’s or one’s own report (4,6,17,19). As in any medical specialty, a colleague’s opinion can exert undue influence on a radiologist’s medical decision making (17).
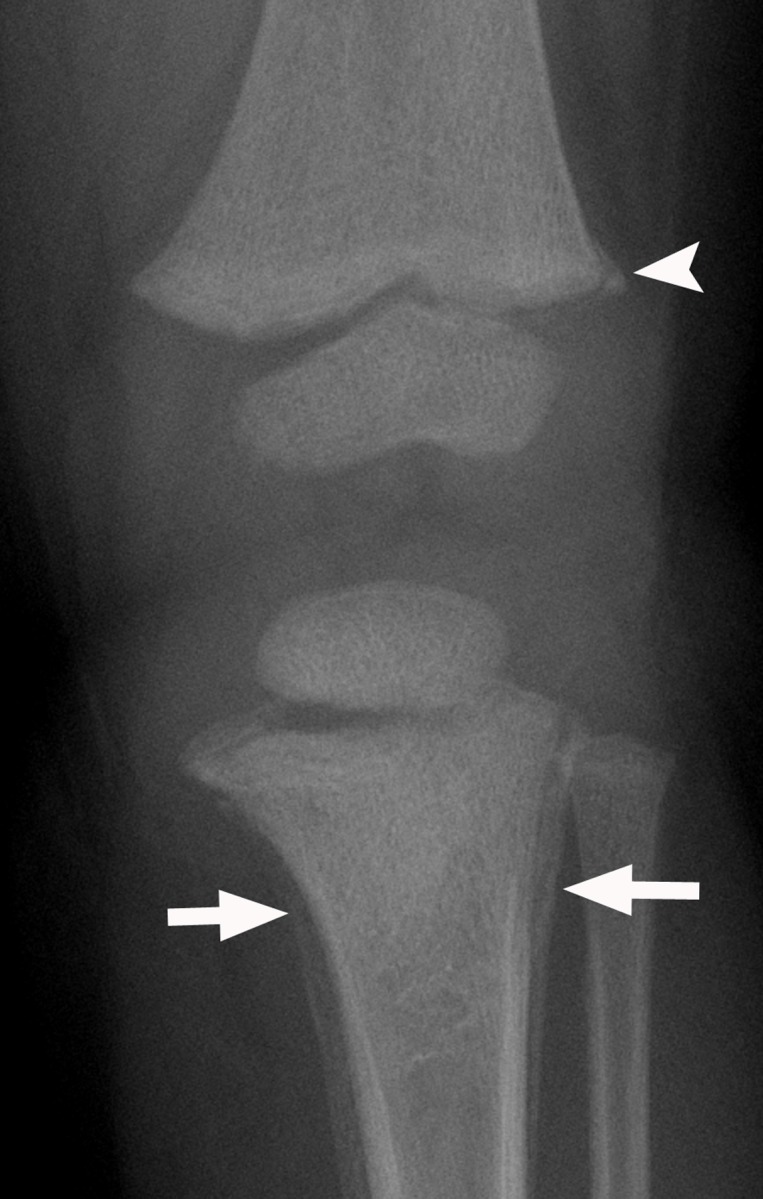
Figure 4a.
Satisfaction of report. A 65-year-old woman, with a history of bilateral lumpectomy followed by left mastectomy for disease recurrence, presented for right diagnostic mammography, per lumpectomy protocol. The patient denied having a palpable lump, pain, or nipple discharge. (a) Right mediolateral oblique (MLO) mammogram shows an area of increased density (arrow) at the lumpectomy site. (b, c) Right MLO mammograms from previous imaging studies from the past 2 years show the area of increased density, which was described in the previous reports as scarring and classified as Breast Imaging Reporting and Data System (BI-RADS) category 2. (d) MLO right mammogram from a remote prior imaging study shows the original lumpectomy scar, which helped confirm that the most recent mammogram (a) represents a developing asymmetry at the lumpectomy site. (e) Antiradial US image shows a shadowing mass (arrow), which was palpable at clinical examination. Pathologic analysis helped confirmed recurrent breast carcinoma.
Figure 4d.
Satisfaction of report. A 65-year-old woman, with a history of bilateral lumpectomy followed by left mastectomy for disease recurrence, presented for right diagnostic mammography, per lumpectomy protocol. The patient denied having a palpable lump, pain, or nipple discharge. (a) Right mediolateral oblique (MLO) mammogram shows an area of increased density (arrow) at the lumpectomy site. (b, c) Right MLO mammograms from previous imaging studies from the past 2 years show the area of increased density, which was described in the previous reports as scarring and classified as Breast Imaging Reporting and Data System (BI-RADS) category 2. (d) MLO right mammogram from a remote prior imaging study shows the original lumpectomy scar, which helped confirm that the most recent mammogram (a) represents a developing asymmetry at the lumpectomy site. (e) Antiradial US image shows a shadowing mass (arrow), which was palpable at clinical examination. Pathologic analysis helped confirmed recurrent breast carcinoma.
Figure 4b.
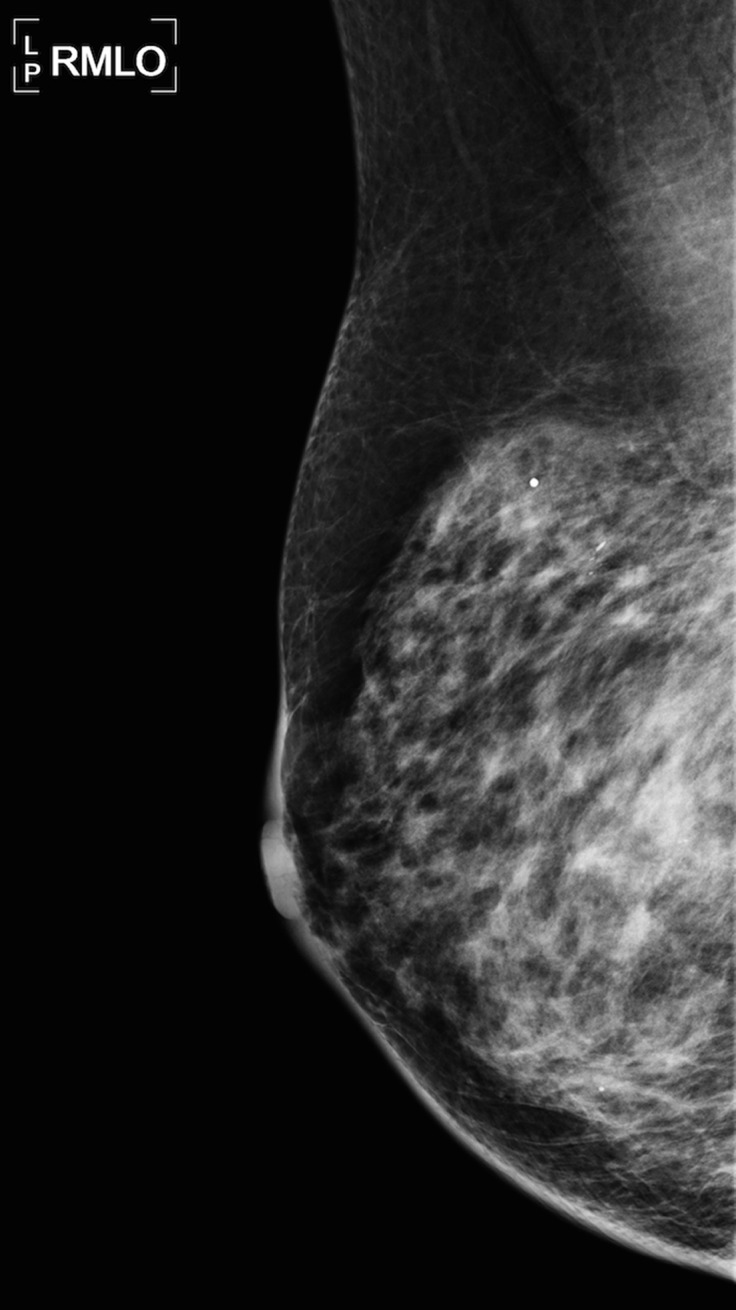
Satisfaction of report. A 65-year-old woman, with a history of bilateral lumpectomy followed by left mastectomy for disease recurrence, presented for right diagnostic mammography, per lumpectomy protocol. The patient denied having a palpable lump, pain, or nipple discharge. (a) Right mediolateral oblique (MLO) mammogram shows an area of increased density (arrow) at the lumpectomy site. (b, c) Right MLO mammograms from previous imaging studies from the past 2 years show the area of increased density, which was described in the previous reports as scarring and classified as Breast Imaging Reporting and Data System (BI-RADS) category 2. (d) MLO right mammogram from a remote prior imaging study shows the original lumpectomy scar, which helped confirm that the most recent mammogram (a) represents a developing asymmetry at the lumpectomy site. (e) Antiradial US image shows a shadowing mass (arrow), which was palpable at clinical examination. Pathologic analysis helped confirmed recurrent breast carcinoma.
Figure 4c.
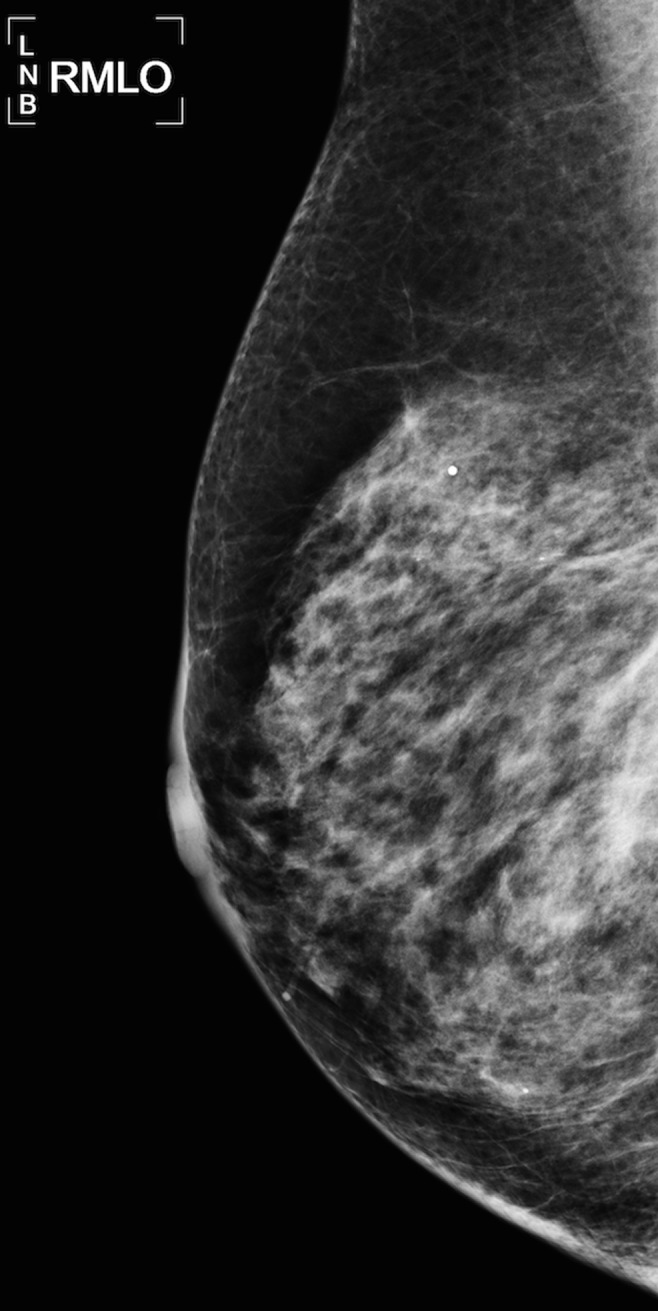
Satisfaction of report. A 65-year-old woman, with a history of bilateral lumpectomy followed by left mastectomy for disease recurrence, presented for right diagnostic mammography, per lumpectomy protocol. The patient denied having a palpable lump, pain, or nipple discharge. (a) Right mediolateral oblique (MLO) mammogram shows an area of increased density (arrow) at the lumpectomy site. (b, c) Right MLO mammograms from previous imaging studies from the past 2 years show the area of increased density, which was described in the previous reports as scarring and classified as Breast Imaging Reporting and Data System (BI-RADS) category 2. (d) MLO right mammogram from a remote prior imaging study shows the original lumpectomy scar, which helped confirm that the most recent mammogram (a) represents a developing asymmetry at the lumpectomy site. (e) Antiradial US image shows a shadowing mass (arrow), which was palpable at clinical examination. Pathologic analysis helped confirmed recurrent breast carcinoma.
Figure 4e.
Satisfaction of report. A 65-year-old woman, with a history of bilateral lumpectomy followed by left mastectomy for disease recurrence, presented for right diagnostic mammography, per lumpectomy protocol. The patient denied having a palpable lump, pain, or nipple discharge. (a) Right mediolateral oblique (MLO) mammogram shows an area of increased density (arrow) at the lumpectomy site. (b, c) Right MLO mammograms from previous imaging studies from the past 2 years show the area of increased density, which was described in the previous reports as scarring and classified as Breast Imaging Reporting and Data System (BI-RADS) category 2. (d) MLO right mammogram from a remote prior imaging study shows the original lumpectomy scar, which helped confirm that the most recent mammogram (a) represents a developing asymmetry at the lumpectomy site. (e) Antiradial US image shows a shadowing mass (arrow), which was palpable at clinical examination. Pathologic analysis helped confirmed recurrent breast carcinoma.
In an review of 656 radiologic examinations with delayed diagnoses, Kim and Mansfield (6) reported that satisfaction of report was the fifth most common cause of diagnostic errors, demonstrating that 6% of errors in diagnostic radiology were related to this bias. However, an additional 5% of errors resulted from readers not reviewing prior studies (6); it has been shown that reviewing prior studies provides diagnostic value in 89% of examinations (21). A radiologist should not discount the benefit of reviewing prior studies in an attempt to reduce this bias.
Strategies to Combat Satisfaction of Report.—In radiology, it is considered standard of care to review relevant prior imaging examinations and reports (4,22). As such, how does a radiologist limit this bias? One should consider reviewing the examination and generating an impression before reviewing a colleague’s prior report (17,19). If, after generating an initial impression, the review of the prior report changes the impression, one should consider a second opinion.
Question to Ask Yourself.—What would I think the diagnosis was if I interpreted the prior study myself and if I hadn’t read the prior impression?
Framing Bias
Framing bias, or framing effect, reflects the phenomenon in which different diagnostic conclusions can be drawn from the same information, depending on how the clinical information is presented (3,16,17,19). Radiologists often interpret a study with limited clinical history (eg, ordering indication: chest pain) and are vulnerable to the way other clinicians present a patient’s clinical history (Fig 5) (3). Clinical information has been shown to improve diagnostic sensitivity without any loss of specificity (22); however, the provided history on radiography requisitions has been shown to be incomplete, inadequate, or, at worst, incorrect or misleading (22–25).
Figure 5a.
Attribution bias confounded by framing bias. A 7-year-old girl, with a history of surgical correction for complex heart disease, presented with acute back pain after running. The clinical differential diagnosis included referred pain from mesenteric ischemia, ovarian torsion, and appendicitis. (a, b) Axial CT images of the pelvis were read as negative for all sources of referred pain by two radiologists. Additional patient history noted a supratherapeutic international normalized ratio. After 2 days in the hospital, the patient experienced weakness in the lower extremities and could no longer void independently. A third radiologist reviewing the CT images noted an area of hyperattenuation (arrows in b) surrounding the thoracic spinal cord. MR imaging was recommended to assess for epidural hematoma. (c) Sagittal T2-weighted MR image of the thoracic spine shows a focal epidural hematoma (arrow). In this case, the back pain was initially framed as a “referred pain” by the other clinicians. Primary causes of back pain are typically attributed to older patients and not children, and as such the radiologist continued the search for sources of referred back pain.
Figure 5b.
Attribution bias confounded by framing bias. A 7-year-old girl, with a history of surgical correction for complex heart disease, presented with acute back pain after running. The clinical differential diagnosis included referred pain from mesenteric ischemia, ovarian torsion, and appendicitis. (a, b) Axial CT images of the pelvis were read as negative for all sources of referred pain by two radiologists. Additional patient history noted a supratherapeutic international normalized ratio. After 2 days in the hospital, the patient experienced weakness in the lower extremities and could no longer void independently. A third radiologist reviewing the CT images noted an area of hyperattenuation (arrows in b) surrounding the thoracic spinal cord. MR imaging was recommended to assess for epidural hematoma. (c) Sagittal T2-weighted MR image of the thoracic spine shows a focal epidural hematoma (arrow). In this case, the back pain was initially framed as a “referred pain” by the other clinicians. Primary causes of back pain are typically attributed to older patients and not children, and as such the radiologist continued the search for sources of referred back pain.
Figure 5c.

Attribution bias confounded by framing bias. A 7-year-old girl, with a history of surgical correction for complex heart disease, presented with acute back pain after running. The clinical differential diagnosis included referred pain from mesenteric ischemia, ovarian torsion, and appendicitis. (a, b) Axial CT images of the pelvis were read as negative for all sources of referred pain by two radiologists. Additional patient history noted a supratherapeutic international normalized ratio. After 2 days in the hospital, the patient experienced weakness in the lower extremities and could no longer void independently. A third radiologist reviewing the CT images noted an area of hyperattenuation (arrows in b) surrounding the thoracic spinal cord. MR imaging was recommended to assess for epidural hematoma. (c) Sagittal T2-weighted MR image of the thoracic spine shows a focal epidural hematoma (arrow). In this case, the back pain was initially framed as a “referred pain” by the other clinicians. Primary causes of back pain are typically attributed to older patients and not children, and as such the radiologist continued the search for sources of referred back pain.
Strategies to Combat Framing Bias.—A radiologist should step outside the clinical framework in which a case is presented and consider different organ systems or causes (19). For example, a cardiologist may not consider noncardiac causes of chest pain (eg, a rib fracture). Radiologists are in a position to interpret an examination outside of the context of a clinical speciality whose specialists may have considered a narrower differential diagnosis (19). The practice advice for radiologists is to read an image first while masking the clinical history or the side of concern before reviewing the clinical history (3,17). If the provided history substantially impacts how the diagnosis is formulated, then one must consider reviewing the patient’s electronic medical record for a more complete and accurate clinical context (3).
Question to Ask Yourself.—Would I still make this diagnosis if I had a different clinical history?
Attribution Bias
Attribution bias occurs when findings are attributed to certain patient characteristics or stereotypes (19), which, in the setting of radiology, are typically obtained from the provided clinical history (Fig 5). A radiologist is frequently divorced from the patient’s initial clinical presentation, which allows a radiologist’s diagnosis to be less influenced by patient stereotypes when compared to the diagnoses of other physicians. However, radiologists are still subject to this bias and can be influenced by the provided patient information, which includes age, name, sex, and ethnicity (19).
A patients’ ethnicity or country of origin can play a critical role in informing a diagnosis. For example, this information is valuable when considering rare genetic diseases or infectious diseases that may be endemic in certain countries or populations. However, as described previously, the provided clinical history can be limited and subject to error (23–26), which could mislead the interpreting radiologist and lead to an incorrect diagnosis (19).
Strategies to Combat Attribution Bias.—When formulating a diagnosis, one should be aware that patient information can impact the rate of diagnosis of disease (19). Other strategies used to combat this type of bias are similar to those used to reduce framing bias; a radiologist should consider reading an imaging study with the clinical history masked, and then he or she should review the provided history. If the provided history substantially impacts the diagnosis, one should review the patient’s chart for more complete and accurate clinical information.
Question to Ask Yourself.—Would I suspect this diagnosis if I did not know the patient’s demographic information?
Satisfaction of Search
Satisfaction of search refers to an individual’s decreased vigilance and/or awareness of additional abnormalities after the first abnormality has been identified (Fig 6) (3,6,13,16,19).This is a bias that plagues radiologists. In a study classifying types of radiologic diagnostic errors, 22% were related to satisfaction of search, which was second only to errors classified as underdiagnoses or misses, making this the most common cognitive bias in diagnostic radiology (6).
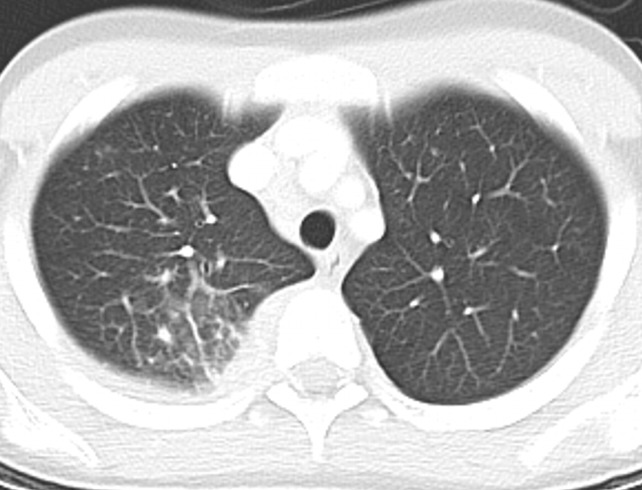
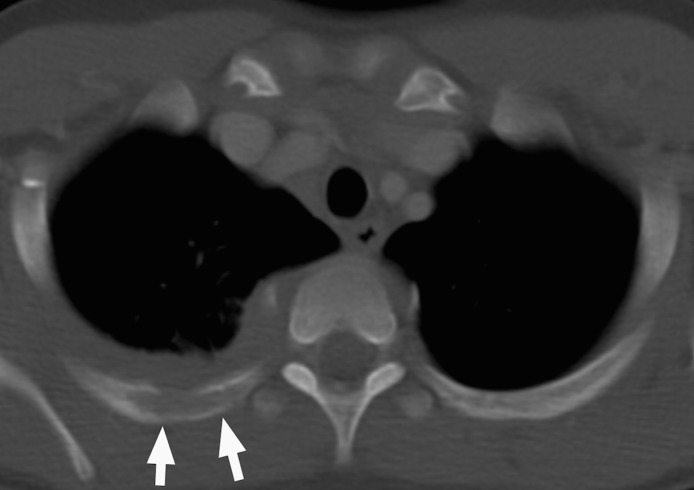
Figure 6a.
Satisfaction of search compounded by premature closure. A 17-year-old boy presented with fever of unknown origin. (a) Axial nonenhanced CT image of the chest demonstrated pneumonia in the posterior segment of the right upper lobe. Antibiotic therapy was started, but the fever persisted. Images were further reviewed at the referred institution. (b) Axial nonenhanced CT image (bone window) shows cortical rib erosions (arrows). Tuberculosis with rib involvement was diagnosed. In this case, the secondary rib findings were missed after the pulmonary findings were identified. In addition, the initial diagnostic evaluation did not consider tuberculosis, although it should have been included as a differential diagnosis for the pulmonary findings.
Figure 6b.
Satisfaction of search compounded by premature closure. A 17-year-old boy presented with fever of unknown origin. (a) Axial nonenhanced CT image of the chest demonstrated pneumonia in the posterior segment of the right upper lobe. Antibiotic therapy was started, but the fever persisted. Images were further reviewed at the referred institution. (b) Axial nonenhanced CT image (bone window) shows cortical rib erosions (arrows). Tuberculosis with rib involvement was diagnosed. In this case, the secondary rib findings were missed after the pulmonary findings were identified. In addition, the initial diagnostic evaluation did not consider tuberculosis, although it should have been included as a differential diagnosis for the pulmonary findings.
Radiologists can be subject to answering only the clinical question asked, but their role is to make a unifying diagnosis (19). For example, the call for a peripherally inserted central catheter line check, which appears to be a straightforward check, primarily asks whether the line is appropriately positioned. Answering only this clinical question obscures the search for possible additional findings, such as pulmonary nodules.
It has been shown that introducing an artificial second finding on a chest radiograph reduces the sensitivity for detection of the initial abnormality (27). Even in the absence of introduced bias, lung cancer on chest radiographs has been shown to be commonly missed (28,29).
Strategies to Combat Satisfaction of Search.—Radiologists can use a systematic approach to ensure all relevant findings are identified, particularly common and commonly missed diagnoses (3,6,19). After completing the primary search and identifying the first finding or responding to the clinical question, one should initiate a secondary search (3,13). Related diagnoses and common diagnostic combinations should be kept in the forefront of the search (3).
Question to Ask Yourself.—Did I adhere to my primary and secondary search patterns?
Premature Closure
Premature closure is defined as the tendency to accept an initial diagnosis as final during the preliminary stages of evaluation (3,13,16,30). This is the most common type of cognitive error in clinical medicine (31). Premature closure can result from convenience or “laziness of thought,” particularly when one is fatigued (13). It has been said that “when the diagnosis is made, the thinking stops” (16). This bias can be compounded by satisfaction of search and satisfaction of report (Fig 6).
Strategies to Combat Premature Closure.—To avoid this bias, a radiologist should initially generate a broad differential diagnosis (3), and then deliberately narrow down the potential diagnoses. One should have an open mind while formulating a working diagnosis. If the diagnosis is unclear, one must consider obtaining pathologic confirmation, if it is feasible (3,13).
Question to Ask Yourself.—Do I really have enough information to make a final diagnosis?
Inattentional Blindness
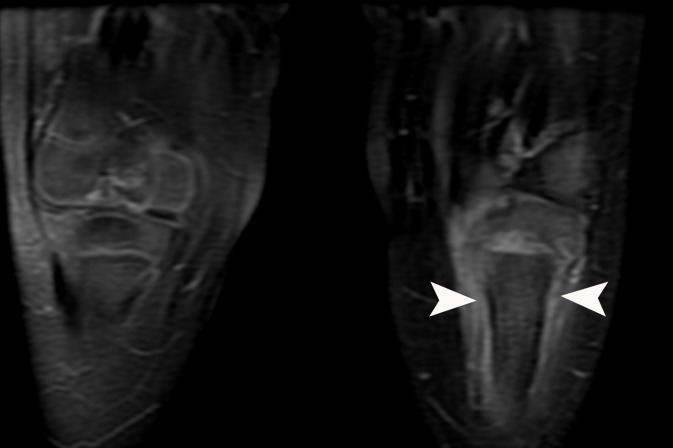
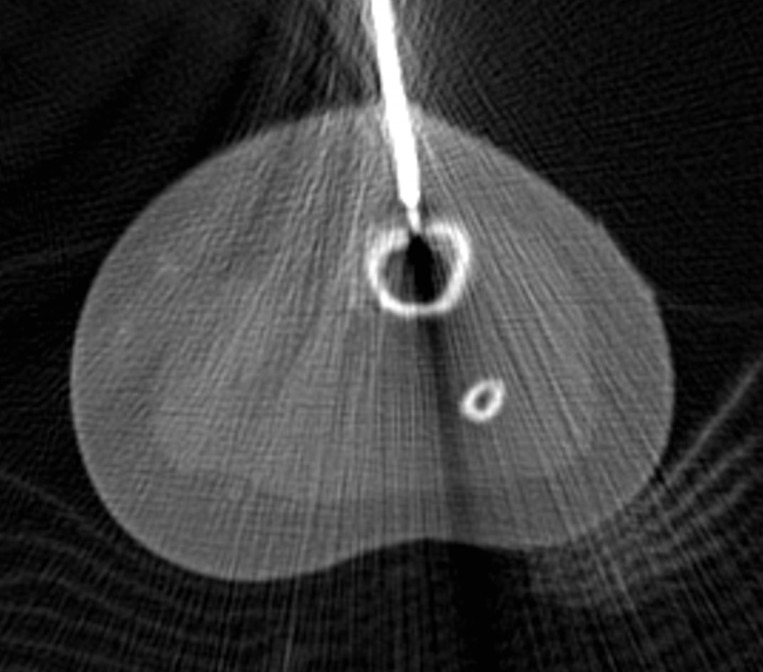
Inattentional blindness, also known as scrolling error or tunnel vision, describes findings that are missed because they are hidden in plain sight. Findings can be missed because of their location (eg, the last sections of the acquisition or the periphery of the field of view) or because of the unexpected nature of the findings (Fig 7) (6,32). A study showed that this is the fourth most common cause of error in diagnostic radiology, as 7% of errors were attributed to the finding being in the periphery of the image (6).
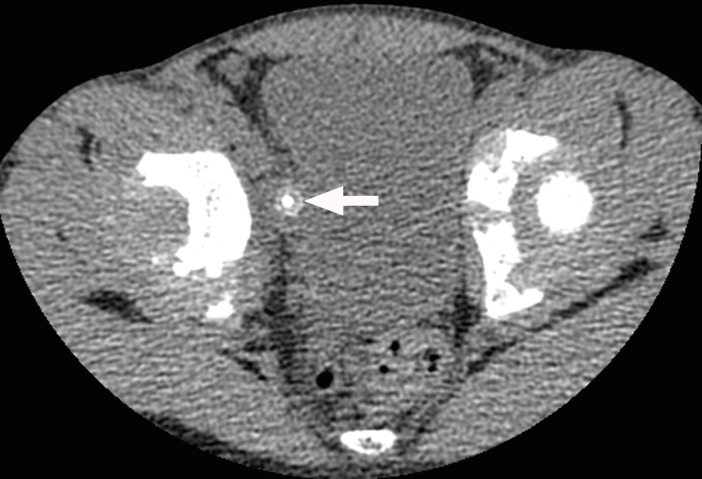
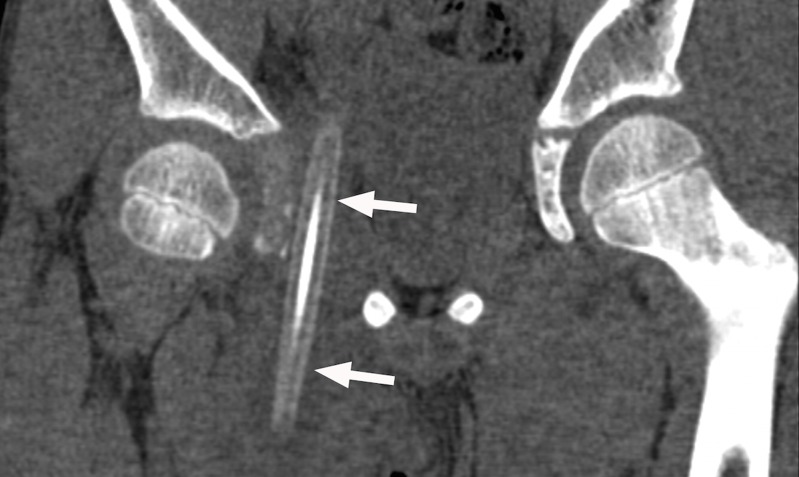
Figure 7a.
Inattentional blindness and hindsight bias. A child presented to the emergency department with a limp and denied a history of trauma. (a, b) Frontal (a) and right frog-leg lateral (b) radiographs show a normal pelvis and right hip, as interpreted by the radiologist. (c, d) Axial (c) and coronal (d) nonenhanced CT images of the pelvis show a pencil (arrows), which was present due to self-inflicted trauma. This finding was outside the traditional search pattern and demonstrates inattentional bias during radiographic review. The radiologist interpreting the CT images (c, d) could not believe the finding was missed during the initial review, which is an example of hindsight bias.
Figure 7b.
Inattentional blindness and hindsight bias. A child presented to the emergency department with a limp and denied a history of trauma. (a, b) Frontal (a) and right frog-leg lateral (b) radiographs show a normal pelvis and right hip, as interpreted by the radiologist. (c, d) Axial (c) and coronal (d) nonenhanced CT images of the pelvis show a pencil (arrows), which was present due to self-inflicted trauma. This finding was outside the traditional search pattern and demonstrates inattentional bias during radiographic review. The radiologist interpreting the CT images (c, d) could not believe the finding was missed during the initial review, which is an example of hindsight bias.
Figure 7c.
Inattentional blindness and hindsight bias. A child presented to the emergency department with a limp and denied a history of trauma. (a, b) Frontal (a) and right frog-leg lateral (b) radiographs show a normal pelvis and right hip, as interpreted by the radiologist. (c, d) Axial (c) and coronal (d) nonenhanced CT images of the pelvis show a pencil (arrows), which was present due to self-inflicted trauma. This finding was outside the traditional search pattern and demonstrates inattentional bias during radiographic review. The radiologist interpreting the CT images (c, d) could not believe the finding was missed during the initial review, which is an example of hindsight bias.
Figure 7d.
Inattentional blindness and hindsight bias. A child presented to the emergency department with a limp and denied a history of trauma. (a, b) Frontal (a) and right frog-leg lateral (b) radiographs show a normal pelvis and right hip, as interpreted by the radiologist. (c, d) Axial (c) and coronal (d) nonenhanced CT images of the pelvis show a pencil (arrows), which was present due to self-inflicted trauma. This finding was outside the traditional search pattern and demonstrates inattentional bias during radiographic review. The radiologist interpreting the CT images (c, d) could not believe the finding was missed during the initial review, which is an example of hindsight bias.
The significant impact tunnel vision can have on radiologists was demonstrated in a study in which a cartoon gorilla was inserted into the lung fields on a chest CT study. It was missed by 83% of radiologists who were asked to search for pulmonary nodules (32).
Strategies to Combat Inattentional Bias.—A radiologist should know his or her blind spots and create a search pattern to review areas that are prone to this bias, including the periphery, first and last images, and scout and localizer sequences (6). One should step back and look at the big picture, as unexpected findings may be outside the traditional search pattern.
Question to Ask Yourself.—Did I remember to check my blind spots?
Hindsight Bias
Prevalent in all medical specialties, hindsight bias is the tendency to retrospectively de-emphasize the difficulty in making the initial diagnosis after it has been confirmed (3,13,16,19), particularly in morbidity and mortality conferences. This bias is also referred to as the “I knew it all along” bias (3,13), retrospectoscope bias, or the “how could he/she miss that?” bias. It is distinct from previously described biases due to its retrospective nature (Fig 7) (13,19).
Hindsight bias prevents the realistic assessment of past events, distorts the evaluation of prior decision making, and discounts the scenario under which the decision making occurred (13,16). This bias is related to self-serving bias in that individuals are more likely to take credit for their correct decisions and discount their mistakes (19).
Strategies to Combat Hindsight Bias.—This bias is difficult to overcome but is important to recognize. It can create an illusion that some radiologists are more intelligent than others (19), and it can compromise learning by setting unrealistic expectations for trainees (16,19). A radiologist should not lose confidence or become overconfident as the result of a retrospective analysis of his or her interpretation (13). A radiologist should try to understand a colleague’s perspective before making judgments about his or her decisions.
Question to Ask Yourself.—How could I have come to the same conclusion as the radiologist who missed this diagnosis?
Reducing Cognitive Errors
There is a wide range of cognitive and systemic strategies for reducing error in clinical decision making (33). In this section, we focus on additional strategies to combat cognitive errors. In addition to the previously described cognitive forcing strategies, metacognition is a described mechanism used to combat bias (34). Systemic strategies to reduce cognitive diagnostic error include reducing interruptions, participating in quality assurance conferences to provide feedback on clinical decision making, and reviewing radiologic-pathologic correlations to establish the base rate of disease.
Improving Metacognition
Systemic factors often contribute to cognitive errors, but metacognitive training and cognitive forcing strategies can be used to combat cognitive bias at an individual level. Medical decision making is a complex process and requires type 1 and type 2 thinking (35). The first step of metacognition is to note whether an individual is using type 1 or type 2 thinking and recognize that type 1 thinking can subject a person to cognitive errors (36,37). Reflective thinking and self-questioning form the basis of metacognitive training, which can be used to identify what cognitive bias an individual’s current thinking process is most susceptible to (36,37).
Once a cognitive error has been identified, cognitive debiasing, or cognitive forcing strategies (Table 3), can be employed to prevent the error from occurring (12). For example, a cognitive forcing strategy to combat satisfaction of search would be to initiate a secondary search once the first finding has been identified (12). Alternately, if a radiologist, on self-questioning, realizes that he or she made a rare diagnosis based on an experience with a recent manifestation, he or she can employ a strategy to avoid this bias by actively including more likely diagnoses.
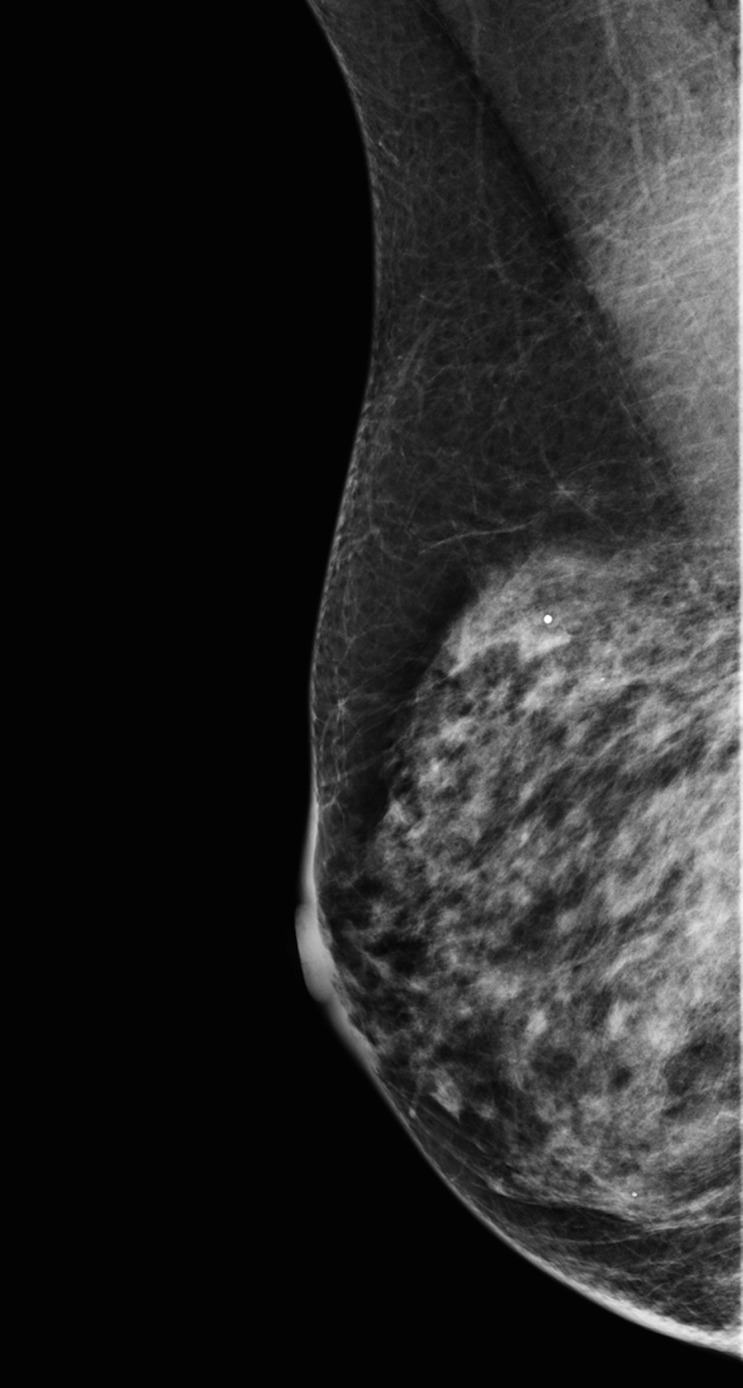
Table 3:
Questions to Guide a Strategic Approach for Unbiased Interpretation
Systemic Sources and Solutions
Systemic processes can contribute to cognitive error in a multitude of ways. In the following section, we describe both the challenges of and solutions for systemic influences on cognition.
Workplace Interruptions.—Common elements in medical workplace errors include interruptions and disruptions (38). Radiologists often multitask, balancing reading studies with noninterpretive tasks such as performing consults, protocoling, and answering calls and pages. In a study of radiology fellows, these tasks constituted 37% of the workday (39). On-call radiologists in particular experience a high volume of disruptions from noninterpretive responsibilities and, at peak hours, can expect to be interrupted an average of 2.5 times while interpreting a CT study (40).
An increase in phone calls before resident generation of a preliminary report has shown significant association with discrepancies (41). Interruptions have been shown to disrupt cognitive processes, and the memory of the original task begins to fade to address the interruption (38). As such, interruptions can contribute to all cognitive biases, particularly satisfaction of search and premature closure. Implementing strategies to reduce workflow disruption, such as designating an individual to manage noninterpretive tasks, has been successful in increasing interpretation time and decreasing disruptions (42).
Quality Assurance and Peer Review.—During radiology training, there is a focus on diagnostic accuracy, although radiologic diagnoses are rarely dichotomous (eg, normal or abnormal) and often require advanced and complex decision making (43). Even among trained specialists, there is significant interreader and intrareader variation in diagnostic interpretation (44), with one study reporting discrepancy rates of 26% and 32%, respectively (45). Understanding, accepting, and forgiving one's cognitive error is an essential component of identifying and correcting cognitive biases.
Creating a peer-review program with a positive culture is essential to correct cognitive bias (3,46). Peer-review programs establish an environment where errors are instructive rather than punitive (46) and support an atmosphere of cognitive debiasing, ensuring that hindsight bias does not overwhelm the retrospective analyses. It is important to acknowledge both hits and misses throughout this process, as sharing and discussing positive calls, in addition to missed findings, helps foster a positive environment for analyzing clinical decisions.
Radiologic-Pathologic Correlation.—Routine radiologic-pathologic correlation is the current standard of care in breast imaging. It has the potential for positive implications on cognitive training for all involved when radiologic diagnoses have pathologic correlates. Radiologic-pathologic correlation gives a diagnostic radiologist accurate feedback on his or her disease detection rates, positive predictive values, and abnormal interpretation rates (3,47). This establishes the radiologist’s knowledge of base rates of disease and therefore helps increase awareness and prevention of availability bias.
Conclusion
Biases can substantially impact radiologic decision making, resulting in medical errors and negative patient outcomes. Maintaining an awareness of how individuals process thoughts and decisions is important, as heuristics are an integral part of human information processing. Understanding heuristics and one's vulnerability to cognitive biases does not prevent the biases' potential effects, but it can help a radiologist identify when he or she may be wrong.
Cognitive forcing strategies and metacognition can help disrupt and reduce the impact of cognitive bias on decision making and decrease rates of diagnostic error. Systemic sources of error that can impact cognitive processes should be addressed through institutional measures, including limiting unnecessary interruptions during imaging interpretation and providing radiologists with diagnostic feedback through peer-review programs, quality improvement, and radiologic-pathologic correlation. Being aware of the limitations in one’s judgment can lead to more thoughtful deliberation of imaging findings and improve the quality of decision making.
Footnotes
Presented as an education exhibit at the 2016 RSNA Annual Meeting.
For this journal-based SA-CME activity, the authors, editor, and reviewers have disclosed no relevant relationships.
L.P.B. supported by a National Institute of Biomedical Imaging and Bioengineering T32 Training Grant (T32EB001631).
References
- 1.Kohn LT, Corrigan JM, Donaldson MS, et al. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000. [PubMed] [Google Scholar]
- 2.Makary MA, Daniel M. Medical error: the third leading cause of death in the US. BMJ 2016;353:i2139. [DOI] [PubMed] [Google Scholar]
- 3.Lee CS, Nagy PG, Weaver SJ, Newman-Toker DE. Cognitive and system factors contributing to diagnostic errors in radiology. AJR Am J Roentgenol 2013;201(3):611–617. [DOI] [PubMed] [Google Scholar]
- 4.Berlin L. Malpractice issues in radiology: perceptual errors. AJR Am J Roentgenol 1996;167(3):587–590. [DOI] [PubMed] [Google Scholar]
- 5.Garland LH. Studies on the accuracy of diagnostic procedures. Am J Roentgenol Radium Ther Nucl Med 1959;82(1):25–38. [PubMed] [Google Scholar]
- 6.Kim YW, Mansfield LT. Fool me twice: delayed diagnoses in radiology with emphasis on perpetuated errors. AJR Am J Roentgenol 2014;202(3):465–470. [DOI] [PubMed] [Google Scholar]
- 7.Berlin L. Accuracy of diagnostic procedures: has it improved over the past five decades? AJR Am J Roentgenol 2007;188(5):1173–1178. [DOI] [PubMed] [Google Scholar]
- 8.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science 1974;185(4157):1124–1131. [DOI] [PubMed] [Google Scholar]
- 9.Kahneman D. Part 1. In: Kahneman D, ed. Thinking, fast and slow. New York, NY: Farrar, Straus & Giroux, 2011; 19–89. [Google Scholar]
- 10.Croskerry P. A universal model of diagnostic reasoning. Acad Med 2009;84(8):1022–1028. [DOI] [PubMed] [Google Scholar]
- 11.Sheth A. Internet of things to smart IoT through semantic, cognitive, and perceptual computing. IEEE Intell Syst 2016;31(2):108–112. [Google Scholar]
- 12.Croskerry P. The cognitive imperative: thinking about how we think. Acad Emerg Med 2000;7(11):1223–1231. [DOI] [PubMed] [Google Scholar]
- 13.Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med 2002;9(11):1184–1204. [DOI] [PubMed] [Google Scholar]
- 14.Flavell JH. Metacognition and cognitive monitoring: a new area of cognitive-developmental inquiry. Am Psychol 1979;34(10):906–911. [Google Scholar]
- 15.Croskerry P. Cognitive forcing strategies in clinical decisionmaking. Ann Emerg Med 2003;41(1):110–120. [DOI] [PubMed] [Google Scholar]
- 16.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 2003;78(8):775–780. [DOI] [PubMed] [Google Scholar]
- 17.Waite S, Scott J, Gale B, Fuchs T, Kolla S, Reede D. Interpretive error in radiology. AJR Am J Roentgenol 2017;208(4):739–749. [DOI] [PubMed] [Google Scholar]
- 18.Strack F, Mussweiler T. Explaining the enigmatic anchoring effect: mechanisms of selective accessibility. J Pers Soc Psychol 1997;73(3):437–446. [Google Scholar]
- 19.Gunderman RB. Biases in radiologic reasoning. AJR Am J Roentgenol 2009;192(3):561–564. [DOI] [PubMed] [Google Scholar]
- 20.Dumitrescu A, Ryan CA. Addressing the taboo of medical error through IGBOs: I got burnt once! Eur J Pediatr 2014; 173(4):503–508. [DOI] [PubMed] [Google Scholar]
- 21.White K, Berbaum K, Smith WL. The role of previous radiographs and reports in the interpretation of current radiographs. Invest Radiol 1994;29(3):263–265. [DOI] [PubMed] [Google Scholar]
- 22.Berlin L. Comparing new radiographs with those obtained previously. AJR Am J Roentgenol 1999;172(1):3–6. [DOI] [PubMed] [Google Scholar]
- 23.Loy CT, Irwig L. Accuracy of diagnostic tests read with and without clinical information: a systematic review. JAMA 2004;292(13):1602–1609. [DOI] [PubMed] [Google Scholar]
- 24.Markert DJ, Haney PJ, Allman RM. Effect of computerized requisition of radiology examinations on the transmission of clinical information. Acad Radiol 1997;4(2):154–156. [DOI] [PubMed] [Google Scholar]
- 25.Gunderman RB, Phillips MD, Cohen MD. Improving clinical histories on radiology requisitions. Acad Radiol 2001;8(4): 299–303. [DOI] [PubMed] [Google Scholar]
- 26.Troude P, Dozol A, Soyer P, et al. Improvement of radiology requisition. Diagn Interv Imaging 2014;95(1):69–75. [DOI] [PubMed] [Google Scholar]
- 27.Berbaum KS, Franken EA, Jr, Dorfman DD, et al. Satisfaction of search in diagnostic radiology. Invest Radiol 1990;25(2): 133–140. [DOI] [PubMed] [Google Scholar]
- 28.Walker A, Murchison J, Beek E, Ritchie G, Sharkey J. Chest radiographs and the elusive lung cancer. Digit Media 2016; 2(3):120. [Google Scholar]
- 29.Berlin L. Defending the “missed” radiographic diagnosis. AJR Am J Roentgenol 2001;176(2):317–322. [DOI] [PubMed] [Google Scholar]
- 30.McSherry D. Avoiding premature closure in sequential diagnosis. Artif Intell Med 1997;10(3):269–283. [DOI] [PubMed] [Google Scholar]
- 31.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med 2005;165(13):1493–1499. [DOI] [PubMed] [Google Scholar]
- 32.Drew T, Võ ML-H, Wolfe JM. The invisible gorilla strikes again: sustained inattentional blindness in expert observers. Psychol Sci 2013;24(9):1848–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graber M, Gordon R, Franklin N. Reducing diagnostic errors in medicine: what’s the goal? Acad Med 2002;77(10):981–992. [DOI] [PubMed] [Google Scholar]
- 34.Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ Theory Pract 2009;14(suppl 1):27–35. [DOI] [PubMed] [Google Scholar]
- 35.Marcum JA. An integrated model of clinical reasoning: dual-process theory of cognition and metacognition. J Eval Clin Pract 2012;18(5):954–961. [DOI] [PubMed] [Google Scholar]
- 36.Hendricks J, Mooney D, Berry C. A practical strategy approach to use of reflective practice in critical care nursing. Intensive Crit Care Nurs 1996;12(2):97–101. [DOI] [PubMed] [Google Scholar]
- 37.Pashler H, Bain PM, Bottge BA, et al. Organizing instruction and study to improve student learning: IES practice guide. Washington, DC: National Center for Education Research, Institute of Education Sciences, U.S. Department of Education. http://files.eric.ed.gov/fulltext/ED498555.pdf. Updated 2007. Accessed April 19, 2017. [Google Scholar]
- 38.Rivera-Rodriguez AJ, Karsh BT. Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care 2010;19(4):304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schemmel A, Lee M, Hanley T, et al. Radiology workflow disruptors: a detailed analysis. J Am Coll Radiol 2016;13(10): 1210–1214. [DOI] [PubMed] [Google Scholar]
- 40.Yu JP, Kansagra AP, Mongan J. The radiologist’s workflow environment: evaluation of disruptors and potential implications. J Am Coll Radiol 2014;11(6):589–593. [DOI] [PubMed] [Google Scholar]
- 41.Balint BJ, Steenburg SD, Lin H, Shen C, Steele JL, Gunderman RB. Do telephone call interruptions have an impact on radiology resident diagnostic accuracy? Acad Radiol 2014;21(12):1623–1628. [DOI] [PubMed] [Google Scholar]
- 42.Lee MH, Schemmel AJ, Pooler BD, et al. Workflow dynamics and the imaging value chain: quantifying the effect of designating a nonimage-interpretive task workflow. Curr Probl Diagn Radiol 2017;46(4):275–281. [DOI] [PubMed] [Google Scholar]
- 43.Gunderman RB, Nyce JM. The tyranny of accuracy in radiologic education. Radiology 2002;222(2):297–300; discussion 301. [DOI] [PubMed] [Google Scholar]
- 44.Strickland NH. Quality assurance in radiology: peer review and peer feedback. Clin Radiol 2015;70(11):1158–1164. [DOI] [PubMed] [Google Scholar]
- 45.Abujudeh HH, Boland GW, Kaewlai R, et al. Abdominal and pelvic computed tomography (CT) interpretation: discrepancy rates among experienced radiologists. Eur Radiol 2010;20(8):1952–1957. [DOI] [PubMed] [Google Scholar]
- 46.Kaewlai R, Abujudeh H. Peer review in clinical radiology practice. AJR Am J Roentgenol 2012;199(2):W158–W162. [DOI] [PubMed] [Google Scholar]
- 47.Lee JK. Quality: a radiology imperative—interpretation accuracy and pertinence. J Am Coll Radiol 2007;4(3):162–165. [DOI] [PubMed] [Google Scholar]