Abstract
Several studies have documented a protective association between social trust and mental and physical health, but gaps in knowledge remain. Debates regarding the contextual versus individual nature of social trust are ongoing; research from low- and middle-income countries is lacking, and study designs have been limited for causal inference. To address these gaps, we examined the association between social trust and depressive symptoms using three waves of the National Income Dynamics Study, a longitudinal South African survey. We used individual fixed-effects models to assess the association between changes in scores on the Center for Epidemiological Studies Depression Scale Short Form (CES-D-10) and in individual-level and district-level personalized and generalized trust among 15,670 individuals completing at least two waves of the NIDS adult questionnaire. High individual-level generalized trust was unexpectedly associated with increased depressive symptoms scores while district generalized trust did not show an association. We also found a cross-level interaction between individual and district-level personalized trust. High individual trust was associated with increased depressive symptoms scores when district trust was low; however, as district-level trust increased, higher individual trust was associated with reduced depressive symptoms. Our unexpected results suggest that trust may not always be beneficial for depressive symptoms, but rather, that its effects may depend on context. In the South African setting where social trust is low, being very likely to trust may be associated with worse depressive symptoms in some circumstances.
Keywords: trust, depression, South Africa, social capital, longitudinal, fixed effects
Introduction
The role of trust and other psychosocial resources in health promotion has been a topic of increasing interest in social epidemiology (Kawachi, 2017). Trust can be conceptualized as a type of “moral resource” which facilitates reciprocity exchanges within networks, and it is viewed as a critical component of social capital (Giordano & Lindstrom, 2011; Kawachi & Berkman, 2014; Mckenzie, 2008). A growing body of research has linked social trust to health outcomes such as mental and self-rated health, and health is often more strongly associated with trust than with other dimensions of social capital (Feng, Vlachantoni, Liu, & Jones, 2016; Giordano & Lindstrom, 2010, 2011, 2016; D. Kim, Baum, Ganz, Subramanian, & Kawachi, 2011; Meng & Chen, 2014). For example, in a recent study in China, Meng and Chen (2014) found that trust was associated with better self-rated health even though other aspects of social capital such as social participation and group membership were not.
At the individual level, several studies have examined the association between health and social trust, using responses to survey questions about individuals’ perceptions of trust as the exposure of interest. However, trust is also viewed as a contextual phenomenon, a collective characteristic of groups that may independently influence health (Kawachi, Kim, Coutts, & Subramanian, 2004; Kawachi, Takao, & Subramanian, 2013). As a contextual measure, social trust is traditionally operationalized by aggregating individual responses to the group level (e.g., community or workplace), and this has also been linked to health (Feng et al., 2016; D. Kim et al., 2011). For instance, in a cross-country study using instrumental variables, Daniel Kim and colleagues (2011) found that higher country-level trust was associated with better self-rated health, controlling for individual-level trust and other variables.
One class of health outcomes whose burden has been on the increase globally, and for which trust is hypothesized to have an effect is mental illness, particularly depression. Major depressive disorder is the 15th leading cause of global disability-adjusted life years according to the Global Burden of Disease 2015, and depressive disorders contribute more than any other mental or behavioral condition to years lived with disability (Kassebaum et al., 2016). In addition to being a major cause of disability, depression contributes to mortality through suicide, and has been tied to other physical health conditions, including poor cardiovascular health (Hare, Toukhsati, Johansson, & Jaarsma, 2014; Rumsfeld & Ho, 2005). Thus, efforts to understand the etiology of and potential mitigating factors against depression are of great importance to public health.
Social trust at the individual level has been linked to reduced levels of depressive symptoms and improved psychological well-being (Bassett & Moore, 2013; Fujiwara & Kawachi, 2008a; Giordano & Lindstrom, 2011; S. S. Kim, Chung, Perry, Kawachi, & Subramanian, 2012; Riumallo-Herl, Kawachi, & Avendano, 2014;; Yip et al., 2007). In a 2013 study among adults from Montreal, Basset and Moore found generalized trust and trust in neighbors to be associated with a lower likelihood of depressive symptoms. At the contextual level, some studies have also found support for a positive association between social trust and better mental health, though these are less consistent when controlling for individual-level factors or individual-level trust (Hamano et al., 2010; Kawachi, Takao, et al., 2013; Murayama, Fujiwara, & Kawachi, 2012).
The proposed mechanisms connecting social trust to depression and mental illness include the observation that communities with high levels of social trust provide members with social support and other resources that may reduce the effects of stressors on mental health (Kessler, 1997; Mckenzie, 2008). Furthermore, high social trust may facilitate health-promoting behaviors such as outdoor exercise and social interactions which may lower rates of depression (Frank, Davis, & Elgar, 2014; Giordano & Lindstrom, 2010, 2011; Kawachi & Berkman, 2014; Subramanian, Kim, & Kawachi, 2002).
In general, research on social trust and mental health from low- and middle-income countries (LMICs) is lacking (De Silva, McKenzie, Harpham, and Huttly, 2005; De Silva, Huttly, Harpham, & Kenward, 2007; Nyqvist, Forsman, Giuntoli, & Cattan, 2013). A recent study from Chile reported inverse associations between individual-level measures of trust and depressive symptoms, similar to associations observed in high-income countries (Riumallo-Herl et al., 2014). However, it should not be assumed that relationships observed in high-income countries apply or are transferable to other settings. The effects of social trust and social capital may depend on location and setting. For this reason, it is important to examine these questions in LMICs so that appropriate interventions can be designed. Moreover, many LMICs are undergoing societal changes, including rapid urbanization, industrialization, and increasing income inequality, which may affect social structures and, in turn, social capital and trust in those societies (Mckenzie, 2008). To the extent that social trust is associated with mental health, such changes may have consequences for mental health and further highlight the need for research on social trust and health in these contexts.
The region of sub-Saharan Africa has seldom been the focus of research examining relationships between mental health and trust or other aspects of social capital (Ramlagan, Peltzer, and Phaswana-Mafuya, 2013; Hall, Tol, Jordans, Bass, & de Jong, 2014; Verduin, Smid, Wind, and Scholte, 2014). In South Africa, a few recent studies using the National Income Dynamics Study (NIDS) have found associations between trust and reduced depressive symptoms or improved self-rated health. (Lau & Ataguba, 2015; Tomita & Burns, 2013). However, these studies have so far used cross-sectional or lagged models and have not yet exploited the panel design of the NIDS to control for time-constant confounding, such as by employing fixed-effects methods. Such methodologies are needed to enhance causal inference in studies of the effects of social trust on health (De Silva et al., 2005; Fujiwara & Kawachi, 2008b; Kawachi, Ichida, Tampubolon, and Fujiwara, 2013).
Objectives
The present study seeks to address the above gaps and extend previous analyses by drawing on three waves of the NIDS to examine longitudinally whether social trust at both a contextual (district) and individual level is associated with depressive symptoms in South Africa. By directly examining the relationship between intra-individual changes in both social trust and depressive symptoms in our sample over time, we can estimate the effect of social trust on depressive symptoms, controlling for between-individual (and between-district) differences.
Hypothesis
We hypothesized that higher individual- and district-level social trust would be independently associated with lower rates of depressive symptoms.
Methods
Setting
South Africa is an upper middle-income country. However, it has consistently high levels of income inequality, crime, violence, and racial disparities (United Nations Office on Drugs and Crime, 2014; van der Berg, 2011; World Bank, 2015; World Bank, 2016), which may be indicative of low social cohesion or the presence of latent social conflict (Kawachi & Berkman, 2014; Kawachi et al., 2004). Previous data also suggest low levels of trust in South Africa (D. Kim et al., 2011). Thus, South Africa is an apt location to study the relationship between social trust and health.
The prevalence of depression in South Africa is not well established, but studies have estimated between 4% and 10% for major depression (Rai, Zitko, Jones, Lynch, & Araya, 2013; Tomlinson, Grimsrud, Stein, Williams, & Myer, 2009; Williams et al., 2008), with about one-fifth to one-third of women and one-eighth to one-quarter of men having depressive symptomatology in various South African samples (Ardington & Case, 2009; Nduna, Jewkes, Dunkle, Shai, & Colman, 2010; Tomlinson et al., 2009).
Administratively, South Africa is divided into nine provinces and 53 districts as of the 2001 census. (These were reduced to 52 districts in the 2011 census). The following study examines indicators of social trust at the level of both individuals and districts.
Sample
Data were drawn from the adult survey of the NIDS Waves 1 (2008), 2 (2010–11), and 3 (2012). The NIDS is a nationally-representative, household panel study, and sampling was done in a stratified, two-stage cluster design. In Wave 1, the household response rate was 69%, and 16,871 individuals were included in the adult survey, with panel members being added in subsequent waves (De Villiers, Brown, Woolard, Daniels, & Leibbrandt, 2014; Southern Africa Labour and Development Research Unit, 2014a, 2014b, 2014c).
Our sample excluded respondents who: 1) were not successfully interviewed in two or more waves (due to death, non-response or refusal, inability to be located, or moving outside of South Africa); 2) did not have a depressive symptoms score [Center for Epidemiology Studies of Depression Short Form (CES-D-10)] or responses to the trust items in two or more waves; 3) were not aged 15 years or over by Wave 2; or 4) had no district information when joining the sample. In Wave 2, a non-response follow-up phase was conducted which contained a shortened version of the survey that excluded the CES-D-10 among other items. Seven hundred thirty-four individuals were excluded due to being surveyed in Phase 2 of Wave 2. Our final sample contained 15,670 individuals interviewed in at least two of three waves, 12,868 of whom were members of the original Wave 1 sample.
Variables
Depressive symptoms
Depressive symptoms were measured using CES-D-10 scores, as described in previous studies (Adjaye-Gbewonyo, Avendano, Subramanian, & Kawachi, 2016; Tomita, Labys, & Burns, 2015a; Tomita, Labys, & Burns, 2015b). Internal consistency measures for the CES-D-10 scale in this sample yielded standardized Cronbach’s alpha values of 0.75 in Wave 1; 0.71 in Wave 2; and 0.74 in Wave 3.
Trust
The survey asked the following questions regarding personalized and generalized trust (Lau & Ataguba, 2015), respectively. Response options were ordinal, in a Likert scale with three options ranging from very likely to not likely (see below):
“Imagine you lost a wallet or purse that contained R200 and it was found by someone who lives close by. Is it very likely, somewhat likely or not likely at all to be returned with the money in it?”
“Imagine you lost a wallet or purse that contained R200 and it was found by a complete stranger. Is it very likely, somewhat likely or not likely at all to be returned with the money in it?”1
These variables were analyzed as dichotomous variables at the individual level comparing those responding very likely to those who responded somewhat or not likely.
For district-level trust, we aggregated responses to each question by district for the full NIDS samples using the 2001 administrative district boundaries for all 53 South African districts. The percentage of respondents in each district responding that it was very likely for the wallet to be returned was calculated applying the NIDS cross-sectional post-stratification weights (Wittenberg, 2009), and this was used as an indicator of high district social trust in the models.
Covariates
Age, race/population group (African, Coloured, Asian/Indian, or White), highest education level attained (no education, some general education & training, completed general education & training, some further education & training, completed further education & training, higher education), sex, marital status (currently married/living with partner, currently single), employment status (employed, unemployed, not economically active), household size, and the log of monthly household income2 were included as covariates. At the district level, covariates constructed from the NIDS survey included mean age; the percent of the district population that was female, rural, and African; percent of the adult population that was unemployed, not economically active, having no formal education, having completed further education, and having tertiary education; the percent of households receiving government grants; and the district Gini coefficient.
Analysis
Data were analyzed in Stata version 13. The analysis was conducted using an “intention-to-treat” (ITT) method, in which individuals who moved from their original Wave 1 or Wave 2 district or who had missing district information in a subsequent wave were treated as if they remained in their original district. This was to avoid potential endogeneity if moving or having missing district information was a result of the outcomes of interest. In our sample, 1,640 people (578 in Wave 2 and 1,219 in Wave 3) or 10.5% of the sample had missing district information in a subsequent wave, and 1,359 people (or 8.7% of the sample) had moved to a different district by Wave 2 or Wave 3. These were assigned to their original district.
For all models, responses of missing, don’t know, or not applicable on all other variables were excluded, and complete-case analyses were conducted. Pooled cross-sectional analyses and longitudinal models with individual fixed-effects were conducted using linear regression with standard errors clustered by district. CES-D-10 scores were mildly skewed, but due to the sample size, the central limit theorem was invoked to run linear regression models on the untransformed CES-D-10 scores. Models presented here are as follows: a model including only individual-level personalized and generalized trust and dummies for wave (wave-adjusted); a model adding individual and household covariates (Model 2); and models adding levels of district high trust and district covariates (Model 3);
The statistical models were of the following form:
where t represents wave, i represents individuals, h represents households, and j represents districts. CESDtihj represents individuals’ CES-D-10 scores in each wave. β0 is the intercept. Social Trusttihj is a vector of individual-level personalized and generalized trust at each wave. Social Trusttj is a vector of district-level personalized and generalized trust at each wave. Covariatestihj, Covariatesthj, and Covariatestj are vectors of individual-level, household, and district covariates, respectively. Individuali represents individual fixed effects. Wavet represents time fixed effects, and e0tihj represents random error. The study employs an individual fixed-effects design to reduce the influence of observed and unobserved time-invariant confounding. All covariates and unmeasured confounders that are constant over time drop out of the models due to the inclusion of individual fixed effects. The associations of interest are expressed in coefficients β1 and β2.
Results
Sample Characteristics
In all waves, over 60% of the sample was female, over 80% was of African race/population group, and mean household size was over four individuals (See Table 1). Sample members were two years older on average in Wave 3 than in Wave 1, and mean deflated monthly household incomes increased by nearly 500 Rand during the study period. The proportion of households living in rural areas decreased from half to 47.4% by Wave 3. Over one-third of sample members were married or living with a partner.
Table 1.
Sample characteristics, NIDS Waves 1, 2, and 3
| Wave 1 | Wave 2 | Wave 3 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Sample Size | Proportion/Mean (SD) | Sample Size | Proportion/Mean (SD) | Sample Size | Proportion/Mean (SD) | |
|
| ||||||
| Total | 12,868 | 15,351 | 14,567 | |||
|
| ||||||
| Female | 7,887 | 61.3% | 9,226 | 60.1% | 8,817 | 60.5% |
|
| ||||||
| Race/population group | ||||||
| African | 10,347 | 80.4% | 12,541 | 81.7% | 11,882 | 81.6% |
| Coloured | 1,831 | 14.2% | 2,070 | 13.5% | 1,997 | 13.7% |
| Asian/Indian | 160 | 1.2% | 179 | 1.2% | 163 | 1.1% |
| White | 530 | 4.1% | 561 | 3.7% | 525 | 3.6% |
|
| ||||||
| Age in years | 12,868 | 37.5 (17.4) | 15,351 | 37.9 (17.7) | 14,567 | 39.5 (17.4) |
|
| ||||||
| Highest Education level | ||||||
| No Education | 1,658 | 12.9% | 1,772 | 11.7% | 1,621 | 11.2% |
| Some General Ed & Training | 4,291 | 33.4% | 4,913 | 32.5% | 4,168 | 28.8% |
| General Ed & Training | 1,200 | 9.4% | 1,459 | 9.7% | 1,267 | 8.8% |
| Some Further Ed & Training | 2,884 | 22.5% | 3,533 | 23.4% | 3,688 | 25.5% |
| Further Ed & Training | 1,968 | 15.3% | 2,359 | 15.6% | 2,281 | 15.8% |
| Higher Education | 831 | 6.5% | 1,063 | 7.0% | 1,447 | 10.0% |
|
| ||||||
| Monthly household income, Rand | 6,227 | 5,248.9 (9,373.1) | 6,442 | 5,479.2 (11,173.7) | 7,317 | 5,719.8 (9,387.9) |
|
| ||||||
| Household size | 6,227 | 4.1 (2.6) | 6,442 | 4.4 (2.9) | 7,317 | 4.2 (2.8) |
|
| ||||||
| Rural household | 3,116 | 50.0% | 3,393 | 49.4% | 3,654 | 47.4% |
|
| ||||||
| Household receipt of government grants | 3,604 | 58.1% | 3,727 | 58.1% | 4,334 | 59.3% |
|
| ||||||
| CES-D-10 score | 12,438 | 8.1 (4.8) | 13,817 | 7.1 (4.2) | 13,625 | 7.0 (4.4) |
|
| ||||||
| Employment status | ||||||
| Employed | 4,683 | 38.1% | 4,302 | 30.5% | 4,982 | 36.6% |
| Unemployed | 2,315 | 18.8% | 1,981 | 14.1% | 2,312 | 17.0% |
| Not economically active | 5,297 | 43.1% | 7,815 | 55.4% | 6,316 | 46.4% |
|
| ||||||
| Marital Status | ||||||
| Currently Married/Cohabiting | 4,573 | 36.8% | 4,699 | 33.2% | 4,659 | 34.2% |
| Currently single | 7,858 | 63.2% | 9,451 | 66.8% | 8,974 | 65.8% |
|
| ||||||
| Trust of neighbors | ||||||
| Very likely | 1,210 | 10.2% | 2,327 | 17.6% | 1,736 | 13.1% |
| Somewhat or not likely | 10,650 | 89.8% | 10,909 | 82.4% | 11,525 | 86.9% |
|
| ||||||
| Trust of strangers | ||||||
| Very likely | 547 | 4.7% | 1,322 | 10.2% | 1,018 | 7.8% |
| Somewhat or not likely | 11,208 | 95.3% | 11,659 | 89.8% | 11,989 | 92.2% |
From Wave 1 to Wave 3, mean CES-D-10 scores decreased from 8.1 to 7.0. Mean CES-D-10 scores varied across districts (see Figure 1). The percentages of sample members believing that it was very likely for their neighbor (high personalized trust) or stranger (high generalized trust) to return their lost wallet increased significantly between Waves 1 and 2 and subsequently declined.
Figure 1.
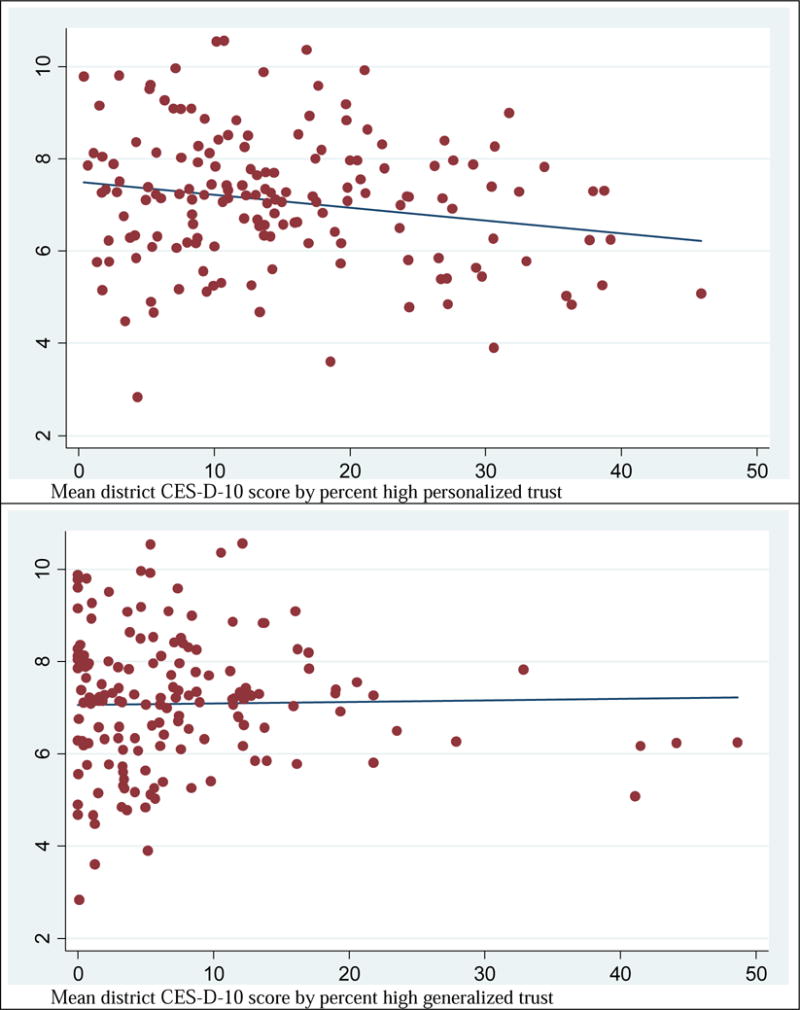
Scatter plots of mean district-level depressive symptoms (y-axis) by district-level high personalized trust (top panel) or high generalized trust (bottom panel) (x-axis), pooled Waves 1, 2, and 3.
At the district level, the mean level of high personalized trust was 11.6% (range: 0.4%-31.7%) at baseline. The corresponding mean level of high district generalized trust was 4.5% (range: 0% to 21.8%) in Wave 1. District trust increased in Wave 2 and decreased again slightly in Wave 3 (See Appendix A). Figure 1 shows scatter plots of district trust by mean district depressive symptoms pooled across all waves.
Model Results
In pooled cross-sectional models adjusting for covariates, personalized trust was not significantly associated with depressive symptoms at the individual or district level. However, individual-level generalized trust was positively associated with depressive symptoms; those who were very likely to trust a stranger had CES-D-10 scores that were more than one point higher than those who were somewhat or not likely to trust a stranger. District-level generalized trust indicators were not associated with CES-D-10 scores (Table 2).
Table 2.
Pooled cross-sectional model estimates and 95% confidence intervals for associations between CES-D-10 scores and personalized and generalized trust
| Wave-adjusted | Model 2 | Model 3 | Model 3+ | |
|---|---|---|---|---|
| Personalized trust (Trust of neighbors) | ||||
| Individual-level | ||||
| Very likely | −0.30 (−0.76, 0.16) | −0.10 (−0.52, 0.32) | −0.10 (−0.50, 0.30) | 0.80* (0.12, 1.47) |
| Somewhat or not likely | Ref | |||
| District-level | ||||
| % Very likely | 0.01 (−0.02, 0.03) | 0.01 (−0.01, 0.04) | ||
| Cross-level interaction | ||||
| % Very likely* very likely | −0.05* (−0.08, −0.01) | |||
| % Very likely* Somewhat or not likely | Ref | |||
| Generalized trust (Trust of strangers) | ||||
| Individual-level | ||||
| Very likely | 1.30*** (0.77, 1.82) | 1 07*** (0.62, 1.52) | 1.15*** (0.73, 1.57) | 1.14*** (0.61, 1.66) |
| Somewhat or not likely | Ref | |||
| District-level | ||||
| % Very likely | −0.01 (−0.04, 0.01) | −0.01 (−0.04, 0.02) | ||
| Cross-level interaction | ||||
| % Very likely* Very likely | 0.00 (−0.04, 0.04) | |||
| % Very likely* Somewhat or not likely | Ref |
Notes: Standard errors are clustered by district. Wave-adjusted model controls for wave. Model 2 adds household and individual factors: log household income, household size, rural/urban location, household receipt of government grants, age, population group, sex, education level, marital status, and employment status. Model 3 adds district variables percent very likely to trust, mean age, percent female, percent rural, percent African, percent unemployed, percent not economically active, percent with no formal education, percent with completed further education, percent with tertiary education, percent of households receiving government grants, and Gini coefficient to Model 2. Model 3+ adds an interaction between district percent very likely to trust and individual-level trust to Model 3. Bold indicates significance at the p<0.05 level.
indicates p<0.05.
indicates p<0.01.
indicates p<0.001.
Longitudinal, fixed-effects models accounting for time-constant confounding and controlling for time-varying covariates mirrored the findings observed in pooled cross-sectional models. Shifting from being somewhat/not trusting to being highly trusting of strangers was associated with an increase in CES-D-10 scores of over one point (95% CI: 0.62–1.53). Changes in levels of high personalized and generalized trust at the district level were not associated with changes in depressive symptoms, however.
To further examine these unexpected results, we added cross-level interaction terms between the indicators of district-level and individual-level trust (Tables 2 & 3, Model 3+). A significant interaction was observed for personalized trust both in the pooled cross-sectional models as well as in longitudinal models of change over time. This revealed that when the percent of district members feeling that a neighbor was very likely to return a lost wallet approached zero, being very trusting (compared to somewhat or not trusting) was associated with worsened mental health. However, this increase in CES-D-10 scores among the very trusting diminished and reversed as the percent of district members who were very trusting of neighbors increased towards 100%. Increases in personalized trust at the district level were associated with improvements in depressive symptoms only among those who were very trusting but were not associated among those who were somewhat or not trusting.
Table 3.
Fixed-effects model estimates and 95% confidence intervals for associations between changes in CES-D-10 scores and changes in personalized and generalized trust
| Wave-adjusted | Model 2 | Model 3 | Model 3+ | |
|---|---|---|---|---|
| Personalized trust (Trust of neighbors) | ||||
| Individual level | ||||
| Very likely | 0.03 (−0.45, 0.51) | 0.03 (−0.45, 0.52) | −0.02 (−0.47, 0.44) | 1.13** (0.37, 1.90) |
| Somewhat or not likely | Ref | |||
| District level | ||||
| % Very likely | −0.01 (−0.05, 0.02) | −0.00 (−0.04, 0.03) | ||
| Cross-level interaction | ||||
| % Very likely * Very likely | −0.06** (−0.10, −0.02) | |||
| % Very likely* Somewhat or not likely | Ref | |||
| Generalized trust (Trust of strangers) | ||||
| Individual level | ||||
| Very likely | 0 99*** (0.49, 1.48) | 0 97*** (0.47, 1.47) | 1.07*** (0.62, 1.53) | 0.89** (0.27, 1.50) |
| Somewhat or not likely | Ref | |||
| District level | ||||
| % Very likely | −0.00 (−0.04, 0.03) | −0.01 (−0.04, 0.03) | ||
| Cross-level interaction | ||||
| % Very likely* Very likely | 0.01 (−0.02, 0.05) | |||
| % Very likely* Somewhat or not likely | Ref |
Notes: Models use individual fixed effects and adjust for clustering by district. Wave-adjusted model controls for wave. Model 2 adds employment status, log household income, household size, receipt of government grants, and marital status. Model 3 adds district variables percent very likely to trust, mean age, percent female, percent rural, percent African, percent unemployed, percent not economically active, percent with no formal education, percent with completed further education, percent with tertiary education, percent of households receiving government grants, and Gini coefficient to Model 2. Model 3+ adds an interaction between district percent very likely to trust and individual-level trust to Model 3. Bold indicates significance at the p<0.05 level.
indicates p<0.05.
indicates p<0.01.
indicates p<0.001.
For generalized trust, being very trusting remained consistently associated with elevated CES-D-10 scores as the percent of district members very likely to trust strangers approached zero. No significant interaction was observed, and changes in district generalized social trust were not associated with changes in depressive symptoms among either the very trusting or those less trusting.
Figure 2 graphically displays the predicted relationship between district trust and CES-D-10 scores for those who were very likely, and somewhat or not likely to trust others, showing the interaction between individual and district personalized trust based on the fixed-effects results in Table 3; high individual personalized trust was protective in districts with high levels of personalized trust, but detrimental in districts with low percentages of highly trusting individuals. Several covariates were consistently associated with depressive symptoms in the expected directions (see Appendix B).
Figure 2.
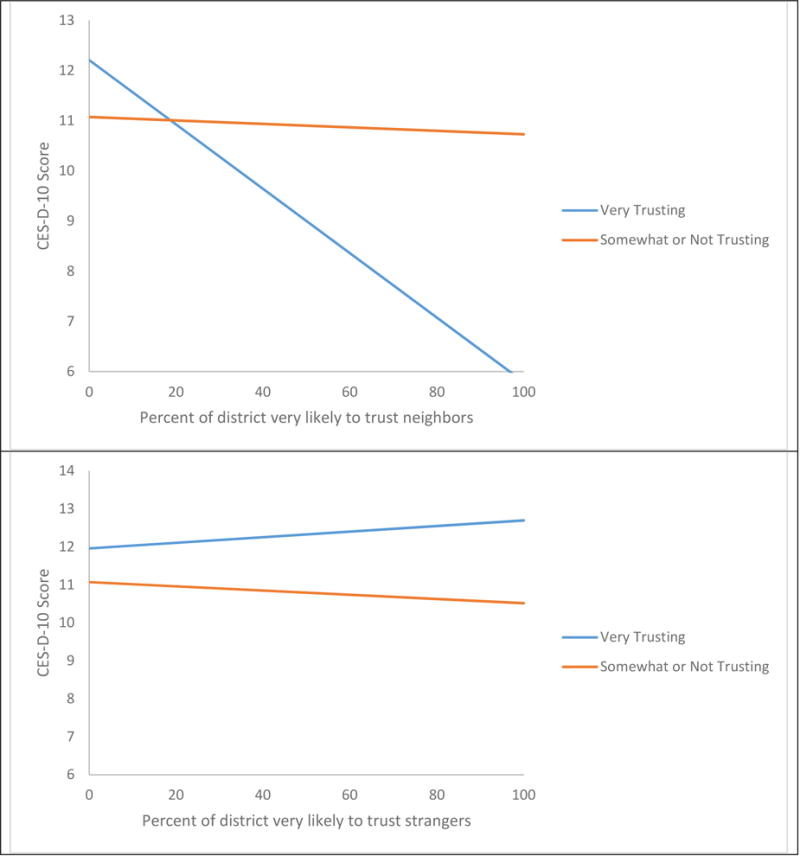
Predicted Relationship between District Trust and CES-1 D-10 Scores for Very Trusting Compared to Somewhat/Not Trusting Individuals in the Reference Population
Discussion
In this South African sample, we found that high individual-level generalized trust was unexpectedly associated with worse depressive symptoms while district-level trust measures and individual-level personalized trust did not show associations in main effects models. However, for personalized trust, a cross-level interaction revealed that high individual-level trust was associated with worse mental health in districts lacking high trust but with increasingly better mental health as district trust levels increased. Moreover, the expected inverse association between district-level personalized trust and depressive symptoms was observed only among individuals with high trust of others in their community but not among those who were less trusting.
These unexpected findings regarding trust deserve further exploration. Although a few studies have observed negative associations between structural components of social capital— such as network participation—and mental health (Bertotti et al., 2013; Croezen, Avendano, Burdorf, & van Lenthe, 2015; Murayama et al., 2013), most research on cognitive components of social capital, such as trust, has found these to be health-preserving or promoting.
There may be a number of explanations for our unexpected results. One possibility is that trust in others is mainly beneficial (for mental health) in societies in which levels of social trust and social capital are already high. By contrast, trusting others may be detrimental in societies that have low social trust. In other words, individuals who blindly trust others in a context where everyone else is mistrusting may get taken advantage of. This could make them more likely to be exposed to stressful life events such as victimization by crime or fraud, thereby increasing risk for depression (Kessler, 1997); or, the psychological impact of such experiences could be higher among those with unwarranted levels of trust compared to others, enhancing risk of depressive symptoms. Our cross-level interaction for personalized trust seems to support this hypothesis. Although for generalized trust, our models appeared to suggest that high individual-level trust would be consistently associated with worse depressive symptoms even as district trust levels increased, these estimates are nevertheless based on a sample with very low levels of generalized trust. On average, districts had under 12% of respondents endorsing high trust of strangers at any point in time. This corroborates data from the World Values Survey which similarly estimated that fewer than 20%, and in some waves as few as 12% of South Africans endorsed that most people can be trusted (D. Kim et al., 2011; Scheffler et al., 2010). Thus, estimates under scenarios of high district trust would be based on extrapolations, and it is still plausible that if generalized trust in fact increased to high levels across districts in South Africa, being a highly trusting individual may no longer appear to be associated with greater depressive symptoms.
Contrasting our results, a couple of studies from South Africa observed positive associations between trust and depressive symptoms. In a 2008 sample of older South African adults, and in an analysis of NIDS data, Ramlagan et al. (2013) and Tomita and Burns (2013), respectively, found that higher levels of trust at the individual level were associated with lower depressive symptoms. Yet, this could be attributed to the fact that the studies were cross-sectional, utilizing data from only the year 2008. When we examined each NIDS wave separately (see Appendix B), our 2008 Wave 1 cross-section similarly found that being very likely as opposed to somewhat or not likely to trust neighbors was associated with lower depressive symptoms, though in the following waves, this was not the case. Therefore, it is possible that some cross-sectional studies are confounded by unobserved factors.
Reflecting some of the literature on the “dark side” or negative consequences of social capital (Kawachi, Takao, et al., 2013), another potential explanation may be that those individuals who are highly trusting or who perceive greater social trust in their communities may feel an undue sense of obligation or be overburdened by norms of reciprocity to others in their communities, and this may account for the higher level of depressive symptoms. Alternatively, the results may reflect confounding by some time-varying factors that cause individuals to both become highly trusting of others and to have more depressive symptoms.
The complex interaction we observed for personalized trust suggests that when district personalized trust was low, less trusting individuals had better mental health, whereas when district personalized trust was high, highly trusting individuals had better mental health. There is little literature analyzing cross-level interactions between contextual- and individual-level measures of trust in relation to mental health to which we can compare our results. The authors noted a couple of studies examining cross-level interactions between other aspects of social capital in relation to mental health (Bertotti et al., 2013; Murayama et al., 2013), but studies examining cross-level interactions between individual and contextual trust in relation to health have often examined self-rated health as the outcome. The findings by Subramanian, Kim, and Kawachi (2002) and Mansyur et al. (2008) seem to lend some credence to the interaction we observed in our study. In a U.S. sample, Subramanian and colleagues (2002) observed that the positive effect of community social trust on self-rated health was greater for individuals with high trust, but was in the opposite direction for individuals with low trust. In a multi-country study, Mansyur and colleagues (2008) found a significant interaction between individual and societal trust among non-former Communist countries, indicating that the positive effect of trust on self-rated health was even stronger in countries with high societal trust.
A South African study using Wave 1 of the NIDS did not examine cross-level interactions, but stratified analyses by province. The authors observed that in stratified analyses, the relationship between self-rated health and individual trust (as well as other elements of individual and neighborhood social capital) varied by province, being positive in some cases and inverse in others (Chola & Alaba, 2013). Taken together with our results, the above studies suggest that the nature of the relationship between trust and health may be more complicated than has previously been recognized.
We also observed that depressive symptoms decreased in our sample between 2008 and 2012. Because age was associated with worse depressive symptoms in this sample, the trend is not likely due to aging. Potential causes could include improvements in the economic situation or health status and services over time, such as the expansion of anti-retroviral therapy (Bor, Herbst, Newell, & Barnighausen, 2013). Another factor that may have influenced some of the changes observed in the sample could be South Africa’s hosting of the World Cup in 2010 around the time of Wave 2. Depressive symptoms dropped most between Waves 1 and 2 while trust levels increased between Waves 1 and 2 before decreasing again in Wave 3. It is possible that, as is sometimes observed with mega-events, and as suggested by results from a study by Kaplanidou et al. (2013), the hosting and anticipation of the 2010 World Cup temporarily increased positive sentiments, expectations, and a sense of togetherness among South Africans.
Strengths and Limitations
Limitations of this study include the fact that, although the NIDS was nationally-representative, our results may not be generalizable outside our sample. There may also be a risk for selection bias because those excluded from the sample due to missingness, attrition, non-response, and the shortened survey for Phase 2 of Wave 2 may not have been randomly excluded (De Villiers et al., 2014; Southern Africa Labour and Development Research Unit, 2014b). Also, the NIDS is not representative at sub-national levels. Therefore, estimates of district social capital and other district characteristics may not completely reflect true district levels or may be more highly influenced by certain types of respondents.
Because of the ITT analysis, district-level trust values for individuals who moved to new districts after Wave 1 may differ from the levels of district trust to which they were later exposed. Nevertheless, ITT is beneficial for reducing endogeneity, and the misspecification due to using ITT would tend to bias our results toward the null, leading to more conservative estimates.
Data on trust and depression in this study are self-reported, so there is potential for self-report bias or detection of an association due to common method bias. However, these might be expected to induce an inverse association between trust and depressive symptoms; yet, in our case, the association between trust and depressive symptoms was generally in the opposite direction to that expected, suggesting that this bias may not have had strong influence on our results. It is also possible that the CES-D-10 scale may not adequately capture depressive symptoms in this sample; however, the CES-D-10 has been validated and used in various populations (Folb et al., 2015; Wong, Na, Tze, & Tian, 2015; Zhang et al., 2012), including recently in South Africa where it performed well in terms of internal consistency and validity in Zulu, Xhosa, and Afrikaans samples (Baron, Davies, & Lund, 2017).
The issue of relevant units of analysis and the modifiable areal unit problem remains in research on social trust or social capital more generally (Kawachi, Takao, et al., 2013). It is therefore unclear whether administrative units such as districts are a meaningful unit for evaluating contextual effects of trust on health. Also, it should be noted that the measure of trust used in the NIDS may not necessarily capture the same aspects of trust as other measures used in research on social trust. Finally, despite including fixed-effects and controlling for other time-varying confounding, the observational nature of this study means that the possibility of residual time-varying confounding remains.
Strengths of our study include its large sample size and the use of a scale rather than physician diagnosis to measure depression, providing an outcome that is not biased due to healthcare access and utilization. Furthermore, we used data at multiple levels in order to examine potential contextual effects of social trust without falling prey to the ecological fallacy. This also allowed for another strength of the study which was the addition of cross-level interactions between district- and individual-level trust to examine specifically for whom and in which contexts social trust is associated with depressive symptoms. Finally, while many previous studies using multilevel data have used random-effects models, the longitudinal nature of the NIDS allowed us to employ a fixed-effects design. Although fixed-effects models are conservative because they look at only a small portion of the overall variation (namely, where the exposure changes over time), they reduce confounding by allowing individuals and units to serve as their own controls, comparing individuals to themselves under different levels of exposure. This eliminates the effects of all stable, time-constant between-person and between-unit differences. Fixed-effects models also explicitly test the question of whether a change in exposure is associated with changes in outcomes, thereby helping to enhance causal inference in observational data.
Conclusion
The results of this analysis contribute to our understanding of the relationship between social trust and mental health by examining the question of whether trust at individual and community levels protects mental health in a region that has to date had relatively limited research on this topic. It examines the question in a country in which levels of social trust are very low, therefore expanding the range of contexts in which social trust and health research has been conducted. Our results suggest exciting avenues for further research and potential clarifications on the hypotheses regarding social trust and its impacts on mental health. Such knowledge may aid in the development and tailoring of effective interventions for social trust and health in different communities. In summary, our study suggests that whether trust is helpful or harmful for depressive symptoms may depend on one’s context. In a society with very high levels of distrust, having high trust in others, where perhaps such trust is not warranted, may, in fact, be associated with worse mental health.
Supplementary Material
Highlights.
We linked social trust with depressive symptoms in a South African panel
Fixed-effects models controlling for unobserved time-constant factors were employed
Individual generalized trust was positively associated with depressive symptoms
An interaction was noted between individual- and district-level personalized trust
Acknowledgments
The primary author received funding support from the Initiative for Maximizing Student Diversity GM055353-13 and the National Research Service Award T32 HL 098048I CVD Epidemiology Training Program in Behavior, the Environment and Global Health, through the National Institutes of Health. MA received support from the European Research Council (ERC grant No 263684), and the European Union’s Horizon2020 research and innovation programme under grant agreements 633666 (Lifepath) and 667661 (MINDMAP). The authors would also like to acknowledge the NIDS team for support with data questions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
In Wave 3, the questions specified that the wallet or purse “contained R200 and your contact details.” R200 corresponded to between $20 and $30 US during the years of the survey.
In Wave 2, one woman had an erroneous or outlying household income value (over 600,000 Rand) (correspondence with Michelle Chinhema), and this was excluded from all analyses.
References
- Adjaye-Gbewonyo K, Avendano M, Subramanian SV, Kawachi I. Income inequality and depressive symptoms in South Africa: A longitudinal analysis of the National Income Dynamics Study. Health Place. 2016;42:37–46. doi: 10.1016/j.healthplace.2016.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardington C, Case A. Health: Analysis of the NIDS Wave 1 Dataset: National Income Dynamics Study 2009 [Google Scholar]
- Baron EC, Davies T, Lund C. Validation of the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) in Zulu, Xhosa and Afrikaans populations in South Africa. BMC Psychiatry. 2017;17(1):6. doi: 10.1186/s12888-016-1178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett E, Moore S. Social capital and depressive symptoms: the association of psychosocial and network dimensions of social capital with depressive symptoms in Montreal, Canada. Social Science and Medicine. 2013;86:96–102. doi: 10.1016/j.socscimed.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Bertotti M, Watts P, Netuveli G, Yu G, Schmidt E, Tobi P, Renton A. Types of social capital and mental disorder in deprived urban areas: a multilevel study of 40 disadvantaged London neighbourhoods. PLoS One. 2013;8(12):e80127. doi: 10.1371/journal.pone.0080127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J, Herbst AJ, Newell ML, Barnighausen T. Increases in Adult Life Expectancy in Rural South Africa: Valuing the Scale-Up of HIV Treatment. Science. 2013 Feb 22;339 doi: 10.1126/science.1230413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chola L, Alaba O. Associaion of neighborhood and individual social capital, neighbourhood economic deprivation and self-rated health in South Africa—a multi-level analysis. PLoS One. 2013;8(7):e71085. doi: 10.1371/journal.pone.0071085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croezen S, Avendano M, Burdorf A, van Lenthe FJ. Social participation and depression in old age: a fixed-effects analysis in 10 European countries. American Journal of Epidemiology. 2015;182(2):168–176. doi: 10.1093/aje/kwv015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva MJ, Huttly SR, Harpham T, Kenward MG. Social capital and mental health: a comparative analysis of four low income countries. Social Science and Medicine. 2007;64(1):5–20. doi: 10.1016/j.socscimed.2006.08.044. [DOI] [PubMed] [Google Scholar]
- De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. Journal of Epidemiology and Community Health. 2005;59(8):619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVilliers L, Brown M, Woolard I, Daniels R, Leibbrandt M. National Income Dynamics Study Wave 3 User Manual. Cape Town: Southern Africa Labour and Development Research Unit; 2014. [Google Scholar]
- Feng Z, Vlachantoni A, Liu X, Jones K. Social trust, interpersonal trust and self-rated health in China: a multi-level study. Int J Equity Health. 2016;15(1):180. doi: 10.1186/s12939-016-0469-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folb N, Lund C, Fairall LR, Timmerman V, Levitt NS, Steyn K, Bachmann MO. Socioeconomic predictors and consequences of depression among primary care attenders with non-communicable diseases in the Western Cape, South Africa: cohort study within a randomised trial. BMC Public Health. 2015;15:1194. doi: 10.1186/s12889-015-2509-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank C, Davis CG, Elgar FJ. Financial strain, social capital, and perceived health during economic recession: a longitudinal survey in rural Canada. Anxiety Stress Coping. 2014;27(4):422–438. doi: 10.1080/10615806.2013.864389. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Kawachi I. A prospective study of individual-level social capital and major depression in the United States. Journal of Epidemiology and Community Health. 2008a;62(7):627–633. doi: 10.1136/jech.2007.064261. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Kawachi I. Social capital and health. A study of adult twins in the U.S. American Journal of Preventive Medicine. 2008b;35(2):139–144. doi: 10.1016/j.amepre.2008.04.015. [DOI] [PubMed] [Google Scholar]
- Giordano GN, Lindstrom M. The impact of changes in different aspects of social capital and material conditions on self-rated health over time: a longitudinal cohort study. Social Science and Medicine. 2010;70(5):700–710. doi: 10.1016/j.socscimed.2009.10.044. [DOI] [PubMed] [Google Scholar]
- Giordano GN, Lindstrom M. Social capital and change in psychological health over time. Social Science and Medicine. 2011;72(8):1219–1227. doi: 10.1016/j.socscimed.2011.02.029. [DOI] [PubMed] [Google Scholar]
- Giordano GN, Lindstrom M. Trust and health: testing the reverse causality hypothesis. Journal of Epidemiology and Community Health. 2016;70(1):10–16. doi: 10.1136/jech-2015-205822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall BJ, Tol WA, Jordans MJ, Bass J, de Jong JT. Understanding resilience in armed conflict: social resources and mental health of children in Burundi. Social Science and Medicine. 2014;114:121–128. doi: 10.1016/j.socscimed.2014.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamano T, Fujisawa Y, Ishida Y, Subramanian SV, Kawachi I, Shiwaku K. Social capital and mental health in Japan: a multilevel analysis. PLoS One. 2010;5(10):e13214. doi: 10.1371/journal.pone.0013214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. European Heart Journal. 2014;35(21):1365–1372. doi: 10.1093/eurheartj/eht462. [DOI] [PubMed] [Google Scholar]
- Kaplanidou K, Karadakis K, Gibson H, Thapa B, Walker M, Geldenhuys S, Coetzee W. Quality of Life, Event Impacts, and Mega-Event Support among South African Residents before and after the 2010 FIFA World Cup. Journal of Travel Research. 2013;52(5):631–645. [Google Scholar]
- Kassebaum NJ, Arora M, Barber RM, Bhutta ZA, Brown J, Carter A, Murray CJL. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I. Trust and population health. In: Uslaner E, editor. The Oxford handbook of social and political trust. New York: Oxford University Press; 2017. [Google Scholar]
- Kawachi I, Berkman LF. Social capital, social cohesion, and health. In: Berkman LF, Kawachi I, Glymour MM, editors. Social epidemiology. Second. New York: Oxford University Press; 2014. pp. 290–319. [Google Scholar]
- Kawachi I, Ichida Y, Tampubolon G, Fujiwara T. Causal inference in social capital research. In: Kawachi I, Takao S, Subramanian SV, editors. Global perspectives on social capital and health. New York, NY: Springer; 2013. pp. 87–121. [Google Scholar]
- Kawachi I, Kim D, Coutts A, Subramanian SV. Commentary: Reconciling the three accounts of social capital. International Journal of Epidemiology. 2004;33(4):682–690. doi: 10.1093/ije/dyh177. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Takao S, Subramanian SV, editors. Global perspectives on social capital and health. New York: Springer; 2013. [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kim D, Baum CF, Ganz ML, Subramanian SV, Kawachi I. The contextual effects of social capital on health: a cross-national instrumental variable analysis. Social Science and Medicine. 2011;73(12):1689–1697. doi: 10.1016/j.socscimed.2011.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SS, Chung Y, Perry MJ, Kawachi I, Subramanian SV. Association between interpersonal trust, reciprocity, and depression in South Korea: a prospective analysis. PLoS One. 2012;7(1):e30602. doi: 10.1371/journal.pone.0030602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau YK, Ataguba JE. Investigating the relationship between self-rated health and social capital in South Africa: a multilevel panel data analysis. BMC Public Health. 2015;15:266. doi: 10.1186/s12889-015-1601-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansyur C, Amick BC, Harrist RB, Franzini L. Social capital, income inequality, and self-rated health in 45 countries. Social Science and Medicine. 2008;66(1):43–56. doi: 10.1016/j.socscimed.2007.08.015. [DOI] [PubMed] [Google Scholar]
- Mckenzie K. Urbanization, social capital and mental health. Global Social Policy. 2008;8(3):359–377. [Google Scholar]
- Meng T, Chen H. A multilevel analysis of social capital and self-rated health: evidence from China. Health Place. 2014;27:38–44. doi: 10.1016/j.healthplace.2014.01.009. [DOI] [PubMed] [Google Scholar]
- Miller M. Principles of suicide prevention Lecture given at Harvard T H Chan School of Public Health. Boston, MA: 2011. [Google Scholar]
- Murayama H, Fujiwara Y, Kawachi I. Social Capital and Health: A Review of Prospective Multilevel Studies. Journal of Epidemiology. 2012 doi: 10.2188/jea.JE20110128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murayama H, Nishi M, Matsuo E, Nofuji Y, Shimizu Y, Taniguchi Y, Shinkai S. Do bonding and bridging social capital affect self-rated health, depressive mood and cognitive decline in older Japanese? A prospective cohort study. Social Science and Medicine. 2013;98:247–252. doi: 10.1016/j.socscimed.2013.09.026. [DOI] [PubMed] [Google Scholar]
- Murayama H, Nofuji Y, Matsuo E, Nishi M, Taniguchi Y, Fujiwara Y, Shinkai S. Are neighborhood bonding and bridging social capital protective against depressive mood in old age? A multilevel analysis in Japan. Social Science and Medicine. 2015;124:171–179. doi: 10.1016/j.socscimed.2014.11.042. [DOI] [PubMed] [Google Scholar]
- Nduna M, Jewkes RK, Dunkle KL, Shai NP, Colman I. Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. Journal of the International AIDS Society. 2010;13:44. doi: 10.1186/1758-2652-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyqvist F, Forsman AK, Giuntoli G, Cattan M. Social capital as a resource for mental well-being in older people: a systematic review. Aging and Mental Health. 2013;17(4):394–410. doi: 10.1080/13607863.2012.742490. [DOI] [PubMed] [Google Scholar]
- Rai D, Zitko P, Jones K, Lynch J, Araya R. Country- and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. British Journal of Psychiatry. 2013;202(3):195–203. doi: 10.1192/bjp.bp.112.112482. [DOI] [PubMed] [Google Scholar]
- Ramlagan S, Peltzer K, Phaswana-Mafuya N. Social capital and health among older adults in South Africa. BMC Geriatrics. 2013;13(1):100. doi: 10.1186/1471-2318-13-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riumallo-Herl CJ, Kawachi I, Avendano M. Social capital, mental health and biomarkers in Chile: Assessing the effects of social capital in a middle-income country. Social Science and Medicine. 2014;105:47–58. doi: 10.1016/j.socscimed.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumsfeld JS, Ho PM. Depression and cardiovascular disease: a call for recognition. Circulation. 2005;111(3):250–253. doi: 10.1161/01.CIR.0000154573.62822.89. [DOI] [PubMed] [Google Scholar]
- Sampson RJ. Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Scheffler RM, Petris NC, Borgonovi F, Brown TT, Sassi F, Dourgnon P, Sirven N. Social Capital, Human Capital and Health: What Is the Evidence? OECD; 2010. [Google Scholar]
- Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2008, Wave 1 [dataset]. Version 5.2. 2014a Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2010–2011, Wave 2 [dataset]. Version 2.2. 2014b Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2012, Wave 3 [dataset]. Version 1.2. 2014c Retrieved from: http://www.datafirst.uct.ac.za/dataportal/index.php.
- Subramanian SV, Glymour MM, Kawachi I. Identifying causal ecologic effects on health: a methodological assessment. In: Galea S, editor. Macrosocial determinants of population health. New York, N.Y: Springer; 2007. pp. 301–331. [Google Scholar]
- Subramanian SV, Kim DJ, Kawachi I. Social trust and self-rated health in US communities: a multilevel analysis. Journal of Urban Health. 2002;79(4 Suppl 1):S21–34. doi: 10.1093/jurban/79.suppl_1.S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Burns JK. A multilevel analysis of association between neighborhood social capital and depression: evidence from the first South African National Income Dynamics Study. Journal of Affective Disorders. 2013;144(1–2):101–105. doi: 10.1016/j.jad.2012.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Labys CA, Burns JK. Depressive Symptoms Prior to Pregnancy and Infant Low Birth Weight in South Africa. Maternal and Child Health Journal. 2015a doi: 10.1007/s10995-015-1732-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Labys CA, Burns JK. A multilevel analysis of the relationship between neighborhood social disorder and depressive symptoms: evidence from the South African National Income Dynamics Study. American Journal of Orthopsychiatry. 2015b;85(1):56–62. doi: 10.1037/ort0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Grimsrud AT, Stein DJ, Williams DR, Myer L. The epidemiology of major depression in South Africa: Results from the South African Stress and Health study. South African Medical Journal. 2009;99(5):368–373. [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. Global Study on Homicide 2013. Vienna: United Nations; 2014. [Google Scholar]
- van der Berg S. Current poverty and income distribution in the context of South African history. Economic History of Developing Regions. 2011;26(1):120–140. [Google Scholar]
- Verduin F, Smid GE, Wind TR, Scholte WF. In search of links between social capital, mental health and sociotherapy: A longitudinal study in Rwanda. Social Science and Medicine. 2014;121:1–9. doi: 10.1016/j.socscimed.2014.09.054. [DOI] [PubMed] [Google Scholar]
- Williams DR, Herman A, Stein DJ, Heeringa SG, Jackson PB, Moomal H, Kessler RC. Twelve-month mental disorders in South Africa: prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychological Medicine. 2008;38(2):211–220. doi: 10.1017/S0033291707001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittenberg M. Weights: Report on NIDS Wave 1. Cape Town: National Income Dynamics Study; 2009. [Google Scholar]
- Wong JHC, Na LL, Tze MK, Tian CZ. Long Term Prevalence of Depressive Symptoms among Victims of the Sichuan Earthquake. Annals of Depression and Anxiety. 2015;2(6):1067. [Google Scholar]
- World Bank. World Development Indicators: Distribution of Income or Consumption. 2015 Retrieved from http://wdi.worldbank.org/table/2.9#.
- World Bank. World Development Indicators. 2016 Retrieved from http://data.worldbank.org/indicator/VC.IHR.PSRC.P5.
- Yip W, Subramanian SV, Mitchell AD, Lee DT, Wang J, Kawachi I. Does social capital enhance health and well-being? Evidence from rural China. Social Science and Medicine. 2007;64(1):35–49. doi: 10.1016/j.socscimed.2006.08.027. [DOI] [PubMed] [Google Scholar]
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, Lima VD. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


