Abstract
We developed a loop-mediated isothermal amplification (LAMP) assay for the detection of Y. pestis by targeting the 3a sequence on chromosome. All 11 species of the genus Yersinia were used to evaluate the specificity of LAMP and PCR, demonstrating that the primers had a high level of specificity. The sensitivity of LAMP or PCR was 2.3 or 23 CFU for pure culture, whereas 2.3 × 104 or 2.3 × 106 CFU for simulated spleen and lung samples. For simulated liver samples, the sensitivity of LAMP was 2.3 × 106 CFU, but PCR was negative at the level of 2.3 × 107 CFU. After simulated spleen and lung samples were treated with magnetic beads, the sensitivity of LAMP or PCR was 2.3 × 103 or 2.3 × 106 CFU, whereas 2.3 × 105 or 2.3 × 107 CFU for magnetic bead-treated liver samples. These results indicated that some components in the tissues could inhibit LAMP and PCR, and liver tissue samples had a stronger inhibition to LAMP and PCR than spleen and lung tissue samples. LAMP has a higher sensitivity than PCR, and magnetic bead capture of DNAs could remarkably increase the sensitivity of LAMP. LAMP is a simple, rapid and sensitive assay suitable for application in the field or poverty areas.
Keywords: Plague, Yersinia pestis, Loop-mediated isothermal amplification, Magnetic beads
Introduction
Plague is a zoonotic disease caused by Gram-negative bacterium Yersinia pestis, which is occasionally transmitted to humans from Y. pestis-infected rodents via the bites of infected fleas.1 Y. pestis is thought to have evolved from a serotype O: 1b strain of Y. pseudotuberculosis about 6000–10,000 years ago although these two species cause remarkably different diseases.2, 3 Y. pestis is a highly virulent and infectious pathogen, and was classified as a Category A pathogen by the U. S. Centers for Disease Control and Prevention.4 Historically, Y. pestis has given rise to three major plague pandemics, leading to millions of human deaths. Recently, the increased outbreak of plague around the world is reported annually to the World Health Organization (WHO), and plague was classified as a re-emerging infectious disease by the WHO.5, 6 In addition, plague has been attracting a considerable attention because its causative agent has always been recognized as one of the classical biological warfare or bioterrorism agents.7, 8 To minimize these threats, development of a rapid method for the detection of Y. pestis is essential.
Y. pestis was often detected by bacterial isolation and microscopy observation,9 phage lysis assay,10, 11 ELISA assays based on the detection of F1 antigen and antibodies against Y. pestis,12, 13, 14, 15 conventional PCR assays,16, 17, 18 real-time quantitative PCR assays,19, 20, 21, 22, 23, 24, 25, 26, 27, 28 biosensors based on fiber-optic or upconverting phosphor technology,29, 30, 31 solid-phase radioimmunoassay based on radiolabeled monoclonal antibody for the detection of plague antigen.32 All these methods are playing an important role in the diagnosis of plague, but these methods either are time-consuming and laborious, or require expensive equipment and personnel with a high level of technical expertise. However, permanent surveillance of the foci of plague located in the poor regions to predict future epizootics in rodents and exposure risk for humans or investigation of samples suspected of bioterrorism on site requires a simple, rapid and efficient diagnostic method. A colloidal gold particles-based lateral-flow (LF) strip detection method for Y. pestis has been developed based on antibodies to F1 and LcrV proteins.33, 34 This dipstick test is a low-cost, easy-to-use and rapid screening method in the surveillance of plague or investigation of samples suspected of bioterrorism on site, but nucleic acid-based rapid detection technology could be a more powerful alternative for detecting Y. pestis.
Loop-mediated isothermal amplification (LAMP) technology has received considerable attention because it allows efficiently amplification of DNA with high specificity and sensitivity under isothermal conditions of 60–65 °C. The LAMP reaction can be accomplished within less than 1 h based on a set of four to six primers and the Bst DNA polymerase with strand displacement activity.35 The method is more suitable for field applications, especially in poverty areas, because it does not require specialized or expensive equipment, and only a simple and inexpensive water bath or heating block can satisfy LAMP assay.36, 37 In addition, LAMP results can be read by the naked eye, or the lateral flow dipstick (LFD) under natural light, which makes the detection results easy to be judged in the field. Currently, the LAMP technique has been widely used in the diagnosis of infectious diseases,38 and it is more sensitive in detecting bacteria compared to the conventional polymerase chain reaction (PCR) method.39, 40 In this study, we construct a simple and rapid LAMP method for detection of Y. pestis based on the specific sequence 3a (GenBank accession no. AF350075) that is a specific fragment located on Y. pestis chromosome found by using a comparative genomic method.41 The specificity of the method was evaluated by using all 11 species of the genus Yersinia. The sensitivity was evaluated by using Y. pestis pure culture, and simulated tissue samples, and magnetic bead-treated simulated tissue samples.
Materials and methods
Bacterial strains, reagents, instruments and animals
Y. pestis EV vaccine strain, Y. pseudotuberculosis, Y. enterocolitica, Y. frederiksenii, Y. intermedia, Y. kristensenii, Y. bercovieri, Y. mollaretii, Y. rohdei, Y. ruckeri, and Y. aldovae were used to evaluate the specificity of LAMP and PCR; 10× thermopol buffer, MgSO4 (100 mM), and Bst DNA Polymerase, Large Fragment (8000 U/ml) were purchased from NEB (Beijing, China); Calcein and real-time turbidity meter LA-320c were purchased from Eiken China CO., LTD.; Taq DNA polymerase (5 U) and dNTPs (2.5 mM) were purchased from TaKaRa (Dalian, China); SM3-P100, amino-modified silica-coated magnetic beads, was purchased form Shanghai Allrun Nano Science & Technology CO., LTD. BALB/c were obtained from Laboratory Animal Research Center, Academy of Military Medical Science, China (licensed from the Ministry of Health in General Logistics Department of Chinese People's Liberation Army, Permit No. SCXK-2007-004). The protocols were approved by Committee of the Welfare and Ethics of Laboratory Animals, Beijing Institute of Microbiology and Epidemiology. The experiments were conducted strictly in compliance with the Regulations of Good Laboratory Practice for nonclinical laboratory studies of drug issued by the National Scientific and Technologic Committee of People's Republic of China.
LAMP and PCR assays
For LAMP reaction, a set of five primers was designed according to the published sequence of 3a in Y. pestis KIM D46 (GenBank accession no.: AF350075) using Primer Explorer version 4. A forward inner primer (FIP), a backward inner primer (BIP), two outer primers (F3 and B3), and a loop forward primer (LF) were used for LAMP amplification. The sequences of the primers are shown in Table 1. LAMP reaction was performed in a total volume of 25 μL mixture containing 10× Thermopol buffer (2.5 μL), 100 mM MgSO4 (1.5 μL), 2.5 mM dNTP Mix (14 μL), 100 mM 3a-FIP (0.4 μL), 100 mM 3a-BIP (0.4 μL), 10 mM 3a-F3 (0.5 μL), 10 mM 3a-B3 (0.5 μL), 10 mM 3a-LF (0.2 μL), 8000 U/mL of Bst DNA Polymerase, Large Fragment (1 μL), water (3 μL), template DNA (1 μL). The LAMP reaction was carried out at 65 °C for 60 min and inactivated at 80 °C for 5 min in water bath. For direct visual detection of DNA amplification, 1 μL of Fluorescent Detection Reagent containing calcein (EIKEN CHINA CO., LTD.) was added to the reaction tube before the LAMP reaction. For a positive reaction, a color change from orange to green was observed through the naked eye under natural light, whereas a negative reaction mixture remained orange. Alternatively, specific DNA amplification was monitored spectrophotometrically by a real-time turbidity meter. To confirm that color change in reaction tubes is a result of DNA amplification, LAMP product was also detected by 0.8% agarose gel electrophoresis and ethidium bromide staining.
Table 1.
Sequence of the primers for LAMP and PCR reactions.
| Primer names | Type | Sequence (5′–3′) | Primer length (bp) |
|---|---|---|---|
| 3a-F3 | Forward outer primer | ACTACCATCCCCTCAAGGTT | 20 |
| 3a-B3 | Backward outer primer | GAGGGCGTTTTGGTAGAGAA | 20 |
| 3a-FIP | Forward inner primer | CACCCGCGTTATCTCATCCCG- TTTTCGAGTAGGGTTAGGTGGGC |
44 |
| 3a-BIP | Backward inner primer | CATGGACGTATGGCGGGTCA- TTTTGTGATGCCGTCCAATGCA |
42 |
| 3a-LF | Forward loop primer | ACCGCCATGAAATGGACAATG | 21 |
Conventional PCR reaction was performed in a total volume of 25 μL mixture containing 10 × buffer (3 μL), 2.5 mM dNTPs (0.6 μL), 10 mM 3a-F3 (0.5 μL), 10 mM 3a-B3 (0.5 μL), 5 U of Taq DNA polymerase (0.1 μL), deionized water (15.3 μL) and template DNA (5 μL). F3 and B3 primers were used for the conventional PCR amplification (Table 1). The reaction was subjected to an initial denaturation at 95 °C for 5 min, followed by 35 cycles of denaturation at 95 °C for 30 s, annealing at 56 °C for 30 s, extension at 72 °C for 1 min and a final extension at 72 °C for 5 min. The PCR products were analyzed by 1.5% agarose gel electrophoresis and stained with ethidium bromide.
Extraction of bacterial genomic DNA
For preparation of high-quality genomic DNA, Y. pestis EV vaccine strain and other bacteria were cultured in Luria broth (LB) at 26 °C and 37 °C, respectively, and then collected by centrifugation. The collected bacterial pellet was resuspended in SE buffer (0.15 M NaCl, 0.1 M EDTA-2Na·2H2O, adjusted to pH 8.0 by 10 M HCl), added to a final concentration of 2% SDS, and then placed in a water bath at 60 °C for 10 min. Then, an equal volume of phenol, chloroform and isoamyl alcohol mixture (25:4:1) was added and the solution was mixed by slowly inverting or rotating to denature proteins, then to remove proteins. The aqueous phase was added a final concentration of 50–100 μg/ml of RNase to degrade RNAs at 37 °C for 30–60 min. Then, an equal volume of chloroform was added, shaking vigorously. The aqueous phase was precipitated with two times volume of ethanol, and then the DNA was spooled out with a glass rod, rinsed with 70% ethanol, and dried in air. Finally, the DNA was dissolved into TE buffer (10 mM Tris–HCl, 1 mM EDTA-2Na·2H2O, adjusted to pH 8.0 by 10 M HCl) for use.
For simple and rapid isolation of bacterial DNA, the bacterial cells were resuspended in deionized water, and then genomic DNA was released by boiling the bacterial suspension at 100 °C for 10 min. The supernatant was collected and used as the DNA template in both LAMP and conventional PCR reactions.
Capture of bacterial genomic DNA by magnetic beads
Bacterial genomic DNA was released by boiling bacterial suspension at 100 °C for 10 min, 300 μL of the supernatant was mixed with the same volume of binding buffer [4 M NaCl and 20% polyethylene glycol (PEG) 8000], followed by addition of 0.2 mg magnetic nanoparticles SM3-P100. The suspension was vibrated vigorously for 15 s, followed by standing at room temperature for 5 min. The magnetic beads were collected by using an external magnet, and the supernatant was discarded. The magnetic pellet was washed two times with 200 μL of 70% ethanol, and then dried completely at room temperature. Finally, the magnetic pellet was resuspended in 100 μL of deionized water to elute bound DNA at room temperature for 5 min with continuous agitation. The supernatant containing the genomic DNA was used as the DNA template in both LAMP and conventional PCR assays.
Preparation of simulated samples and magnetic bead capture of DNA
The spleen, liver and lungs were collected aseptically from pathogen-free BALB/c mice, and then blended with the appropriate volume of PBS buffer to prepare tissue homogenates. Y. pestis was cultured in LB, collected by centrifugation, and then resuspended in deionized water to prepare serial 10-fold dilutions of bacterial suspension. The spleen, liver and lung tissue homogenates were respectively inoculated with the same volume of serial 10-fold dilutions of bacterial suspension to obtain different concentrations of artificially contaminated samples (2.3 × 107–2.3 × 10−1 CFU). Noninoculated tissue homogenates were mixed with the same volume of deionized water to be used as a negative control. Artificially contaminated samples for each tissue were boiled at 100 °C for 10 min, and then centrifugated at 10,000 × g for 2 min. The supernatants can be directly used as the DNA template in both LAMP and conventional PCR assays. The supernatants can be further used to isolate bacterial DNA by magnetic beads according to the protocol described above, and then used in both LAMP and conventional PCR assays.
Determination of LAMP or PCR sensitivity
The sensitivity of LAMP or PCR for the detection of Y. pestis was evaluated with the high-quality genomic DNA. Serial 10-fold dilutions of DNA were made in sterile deionized water, and used as the DNA templates to perform LAMP and PCR assays. The sensitivity of LAMP or PCR was evaluated with Y. pestis pure culture. Serial 10-fold dilutions of Y. pestis cells were made in sterile deionized water, boiled at 100 °C for 10 min, and the supernatants were used for LAMP and conventional PCR reactions. The sensitivity of LAMP or PCR was evaluated with the simulated samples prepared by using mouse spleen, liver and lungs. Serial 10-fold dilutions of Y. pestis cells were respectively spiked into the same volume of tissue homogenates, and boiled at 100 °C for 10 min. The supernatants were directly used for LAMP and PCR assays. In addition, the bacterial DNA was captured from the supernatants by magnetic beads, and then used to determine the sensitivity of LAMP and PCR assays.
Evaluation of specificity of LAMP or PCR
The specificity of LAMP or PCR for the detection of Y. pestis was evaluated by using the high-quality bacterial DNAs (20 ng) from 11 species of bacteria in the genus Yersinia. The specificity of the LAMP or PCR was also evaluated with pure cultures from 11 species of bacteria in the genus Yersinia. Each bacterium was diluted to 107 CFU in sterile deionized water, boiled at 100 °C for 10 min, and the supernatants were used for LAMP and PCR reactions.
Results
The sensitivity of detection of Y. pestis by LAMP and PCR assays
To determine the sensitivity of LAMP or PCR assay, serial 10-fold dilutions of high-purity Y. pestis DNAs were tested. The results showed that the lowest detection limit for LAMP was 0.02 ng of Y. pestis DNA when the product was detected by the naked eye, a real-time turbidity meter or agarose gel electrophoresis and ethidium bromide staining, whereas the sensitivity for PCR was 0.2 ng of Y. pestis DNA (Fig. 1A–D). These results indicated that LAMP had a higher sensitivity than PCR for the detection of Y. pestis DNA, and two LAMP detection methods had the same sensitivity. When Y. pestis was determined by using serial 10-fold dilutions of bacterial solution, the sensitivity for LAMP was 2.3 CFU of Y. pestis when the product was detected by a real-time turbidity meter, the naked eye under natural light or agarose gel electrophoresis, whereas the sensitivity for PCR was 23 CFU of Y. pestis (Fig. 2A–D). Three LAMP detection methods also had the same sensitivity, and had a higher sensitivity than PCR.
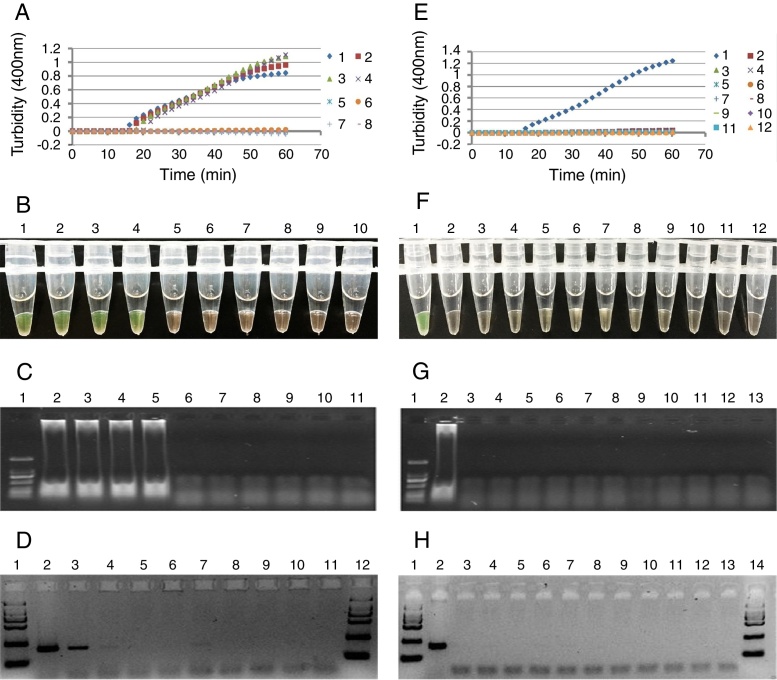
Fig. 1.
The sensitivity (A–D) of the LAMP or PCR for the detection of Y. pestis using serial dilutions of extracted DNA, and the specificity (E–H) of the LAMP or PCR for the detection of Y. pestis using 20 ng DNA from each bacterium of the genus Yersinia. (A) Detection of LAMP products with a real-time turbidity meter. 1–8: 20 ng–0.002 pg; 10: negative control. (B) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–9: 20 ng–0.0002 pg; 10: negative control. (C) Detection of LAMP products with agarose gel electrophoresis. Lane 1: marker; 2–10: 20 ng–0.0002 pg; 11: negative control. (D) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; 2–10: 20 ng–0.0002 pg; 11: negative control; 12: marker. (E) Detection of the LAMP products with a real-time turbidity meter. 1: Y. pestis; 2: Y. pseudotuberculosis; 3: Y. enterocolitica; 4: Y. frederiksenii; 5: Y. intermedia; 6: Y. kristensenii; 7: Y. bercovieri; 8: Y. mollaretii; 9: Y. rohdei; 10: Y. ruckeri; 11: Y. aldovae; 12: negative control. (F) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1: Y. pestis; 2: Y. pseudotuberculosis; 3: Y. enterocolitica; 4: Y. frederiksenii; 5: Y. intermedia; 6: Y. kristensenii; 7: Y. bercovieri; 8: Y. mollaretii; 9: Y. rohdei; 10: Y. ruckeri; 11: Y. aldovae; 12: negative control. (G) Detection of LAMP products with agarose gel electrophoresis. Lane 1: marker; 2: Y. pestis; 3: Y. pseudotuberculosis; 4: Y. enterocolitica; 5: Y. frederiksenii; 6: Y. intermedia; 7: Y. kristensenii; 8: Y. bercovieri; 9: Y. mollaretii; 10: Y. rohdei; 11: Y. ruckeri; 12: Y. aldovae; 13: negative control. (H) Electrophoretic analysis of PCR products with 1.5% agarose gel. Lane 1: marker; 2: Y. pestis; 3: Y. pseudotuberculosis; 4: Y. enterocolitica; 5: Y. frederiksenii; 6: Y. intermedia; 7: Y. kristensenii; 8: Y. bercovieri; 9: Y. mollaretii; 10: Y. rohdei; 11: Y. ruckeri; 12: Y. aldovae; 13: negative control; 14: marker.
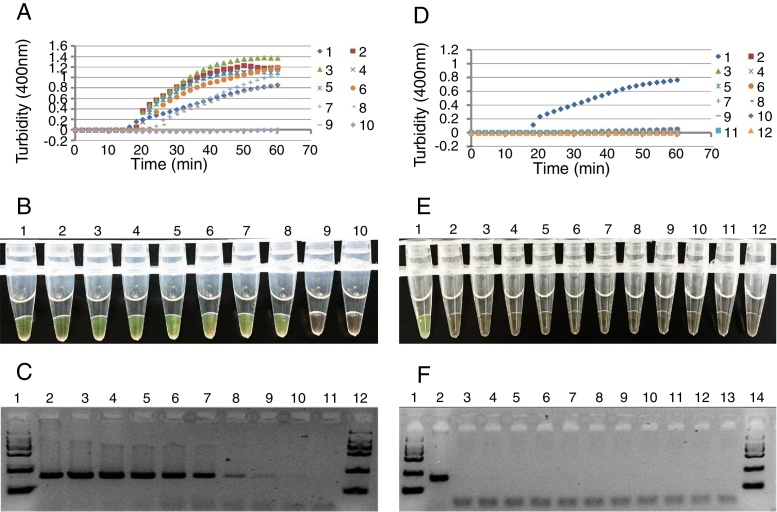
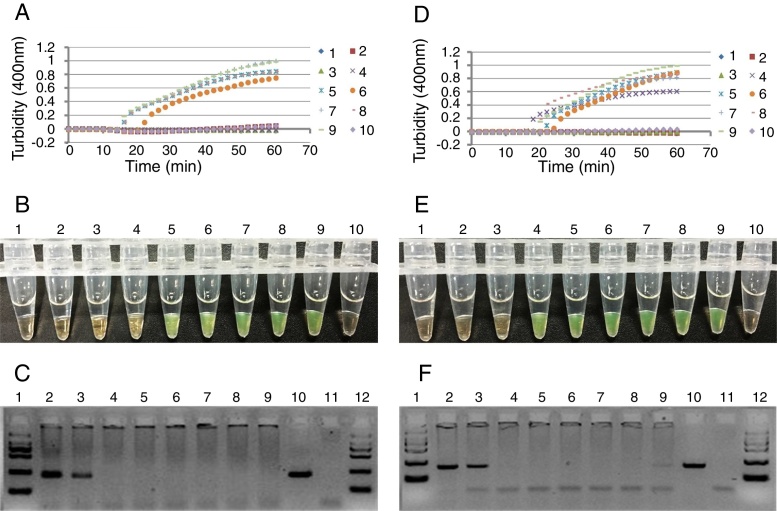
Fig. 2.
The sensitivity (A–C) of the LAMP and PCR for the detection of Y. pestis by using the DNA extracted crudely from serial dilutions of bacterial solutions, and the specificity (D–F) of the LAMP and PCR for the detection of Y. pestis using crudely extracted DNA from each bacterium (2.3 × 107 CFU) of the genus Yersinia. (A) Detection of the LAMP products with a real-time turbidity meter. 1–9: 2.3 × 107–2.3 × 10−1 CFU of Y. pestis; 10: negative control. (B) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–9: 2.3 × 107–2.3 × 10−1 CFU of Y. pestis; 10: negative control. (C) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–10: 2.3 × 107–2.3 × 10−1 CFU of Y. pestis; 11: negative control; 12: marker. (D) Detection of LAMP products with a real-time turbidity meter. 1: Y. pestis; 2: Y. pseudotuberculosis; 3: Y. enterocolitica; 4: Y. frederiksenii; 5: Y. intermedia; 6: Y. kristensenii; 7: Y. bercovieri; 8: Y. mollaretii; 9: Y. rohdei; 10: Y. ruckeri; 11: Y. aldovae; 12: negative control. (E) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1: Y. pestis; 2: Y. pseudotuberculosis; 3: Y. enterocolitica; 4: Y. frederiksenii; 5: Y. intermedia; 6: Y. kristensenii; 7: Y. bercovieri; 8: Y. mollaretii; 9: Y. rohdei; 10: Y. ruckeri; 11: Y. aldovae; 12: negative control. (F) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; 2: Y. pestis; 3: Y. pseudotuberculosis; 4: Y. enterocolitica; 5: Y. frederiksenii; 6: Y. intermedia; 7: Y. kristensenii; 8: Y. bercovieri; 9: Y. mollaretii; 10: Y. rohdei; 11: Y. ruckeri; 12: Y. aldovae; 13: negative control; 14: marker.
The specificity of detection of Y. pestis by LAMP and PCR assays
To determine the specificity for the detection of Y. pestis by LAMP or PCR assay, 11 species of the genus Yersinia were tested. When the high-purity DNAs extracted from 11 species of the genus Yersinia were used for the detection of Y. pestis, respectively, the LAMP product was only detected in the reaction tube of Y. pestis, and no LAMP amplicons appeared in the reaction tubes of other Yersinia strains. Similarly, when the high-purity DNAs extracted from 11 species of the genus Yersinia were respectively used to detect Y. pestis by PCR, specific band was only observed in Y. pestis EV vaccine strain (Fig. 1D–F). When Y. pestis was determined by using 107 CFU of pure culture from 11 species of the genus Yersinia, LAMP product was only detected in the reaction tube of Y. pestis, and no LAMP amplicons appeared in the reaction tubes of other Yersinia strains. Similarly, when 11 species of the genus Yersinia were used to detect Y. pestis by PCR, specific band was only observed in Y. pestis EV vaccine strain (Fig. 2D–F).
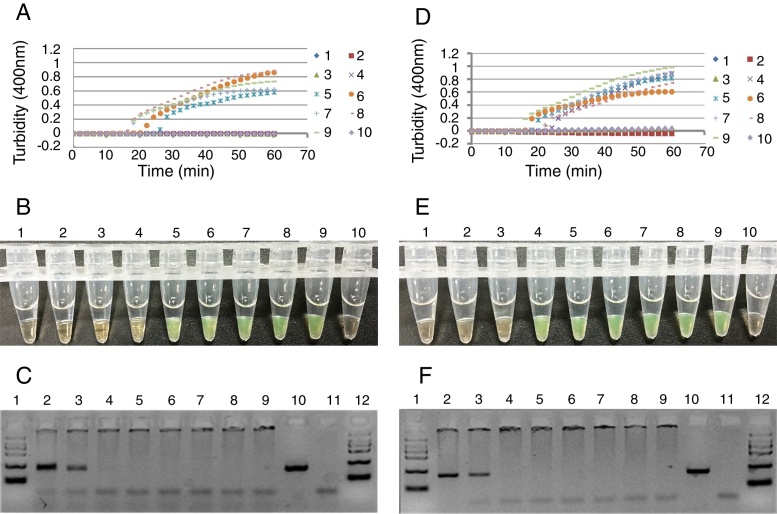
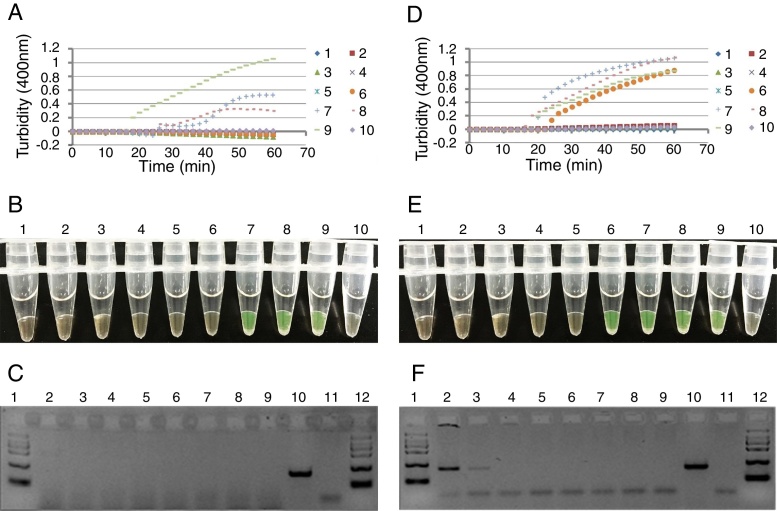
Detection of Y. pestis in simulated samples by LAMP and PCR assays
To determine the sensitivity for the detection of Y. pestis in simulated spleen, liver and lung samples by LAMP or PCR. Artificially contaminated spleen, liver and lung samples containing different concentrations of Y. pestis were prepared by mixing spleen, liver and lung tissue homogenates with the same volume of serial 10-fold dilutions of Y. pestis suspension. Artificially contaminated spleen, liver and lung samples were boiled for 10 min, and then the supernatants were directly determined by LAMP and PCR assays, respectively. The sensitivity for the artificially contaminated spleen by LAMP or PCR assay was 2.3 × 104 or 2.3 × 106 CFU of Y. pestis, respectively. The LAMP assay was 100-fold more sensitive than PCR assay (Fig. 3A–C). The lowest detection limit for the artificially contaminated liver samples by LAMP was 2.3 × 106 CFU of Y. pestis, but PCR assay didn’t detect 2.3 × 107 CFU of Y. pestis in the simulated liver samples (Fig. 4A–C). The lowest detection limit for the artificially contaminated lung samples by LAMP and PCR assay was 2.3 × 104 and 2.3 × 106 CFU of Y. pestis, respectively. The LAMP assay was 100-fold more sensitive than PCR assay (Fig. 5A–C). To increase the sensitivity for the detection of Y. pestis in the simulated samples, the supernatants obtained by boiling the artificially contaminated spleen, liver and lung samples were respectively mixed with the magnetic beads to capture the DNAs for LAMP and PCR assays. After the DNAs in the simulated spleen samples were captured by magnetic beads, the sensitivity for LAMP or PCR assay was 103 or 106 CFU of Y. pestis, respectively. LAMP assay was 1000-fold more sensitive than PCR assay (Fig. 3E and F). The lowest detection limit for the artificially contaminated liver by LAMP or PCR was 2.3 × 105 or 2.3 × 107 CFU of Y. pestis. LAMP assay was 100-fold more sensitive than PCR assay (Fig. 4E and F). The sensitivity for the artificially contaminated lungs by LAMP or PCR assay was 103 or 106 CFU of Y. pestis. LAMP assay was 1000-fold more sensitive than PCR assay (Fig. 5E and F).
Fig. 3.
Detection of Y. pestis in simulated spleen samples by LAMP and PCR. The sensitivity of LAMP or PCR was determined by using the DNA extracted by boiling simulated spleen sample for 10 min (A–C) or by using the DNA captured by magnetic beads (D–F). (A) Detection of LAMP products with a real-time turbidity meter. 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (B) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (C) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–9: 2.3 × 107–2.3 × 100 CFU of Y. pestis; 10: positive control; 11: negative control; 12: marker. (D) Detection of LAMP products with a real-time turbidity meter. 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (E) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (F) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–9: 2.3 × 107–2.3 × 100 CFU of Y. pestis; 10: positive control (20 ng DNA); 11: negative control; 12: marker.
Fig. 4.
Detection of Y. pestis in simulated liver samples by LAMP and PCR. The sensitivity of LAMP or PCR was determined by using the DNA extracted by boiling simulated liver sample for 10 min (A-C) or by using the DNA captured by magnetic beads (D–F). (A) Detection of LAMP products with a real-time turbidity meter. 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (B) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (C) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–9: 2.3 × 107–2.3 × 100 CFU of Y. pestis; 10: positive control (20 ng DNA); 11: negative control; 12: marker. (D) Detection of LAMP products with a real-time turbidity meter. 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (E) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (F) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–9: 2.3 × 107–2.3 × 100 CFU of Y. pestis; 10: positive control (20 ng DNA); 11: negative control; 12: marker.
Fig. 5.
Detection of Y. pestis in simulated lung samples by LAMP and PCR. The sensitivity of LAMP or PCR was determined by using the DNA extracted by boiling simulated lung samples for 10 min (A–C) or by using the DNA captured by magnetic beads (D–F). (A) Detection of LAMP products with a real-time turbidity meter. 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (B) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (C) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–9: 2.3 × 107–2.3 × 100 CFU of Y. pestis; 10: positive control (20 ng DNA); 11: negative control; 12: marker. (D) Detection of LAMP products with a real-time turbidity meter. 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (E) Visualization of LAMP products stained with calcein and inspected under natural light. Tube 1–8: 2.3 × 100–2.3 × 107 CFU of Y. pestis; 9: positive control; 10: negative control. (F) Electrophoretic analysis of PCR products with agarose gel. Lane 1: marker; Lane 2–9: 2.3 × 107–2.3 × 100 CFU of Y. pestis; 10: positive control (20 ng DNA); 11: negative control; 12: marker.
Discussion
Y. pestis strains usually contain three virulence plasmids pCD1, pMT1 and pPCP1, of which pCD1 was inherited from its ancestor Y. pseudotuberculosis. The plasmid pCD1 mainly encodes type three secretion system (T3SS), which plays an essential role in the pathogenesis of Y. pestis.42, 43 The newly acquired pPCP1 encodes a surface proteinase, plasminogen activator (Pla), that is responsible for the increase of the pathogen's invasive ability in bubonic plague and the replication of Y. pestis rapidly in the lungs.44, 45 Another plasmid pMT1 encodes F1 antigen, one of the major protective antigens in Y. pestis, and the murine toxin (Ymt) required for survival of Y. pestis in the midgut of flea.46 Immunological diagnosis of Y. pestis was mainly based on F1 antigen or its antibodies, but this method could not detect the virulent Y. pestis strains lacking F1 antigen.47 In addition, our recent studies found some natural isolates of Y. pestis with one or two plasmids. By contrast, the target genes on chromosome might be more stable. In this study, we constructed a LAMP method to detect Y. pestis based on the 3a sequence on chromosome, which might recognize a greater amount of samples than previous studies. Currently, there have been two reports that described the detection of Y. pestis by LAMP.48, 49 Compared with these two reports, our method had a similar sensitivity with Nune's method for the detection of Y. pestis DNA, but showed a higher sensitivity than Dong's method for the detection of Y. pestis pure culture. All these three methods had a higher specificity. However, the two previous reports are based on the target of F1 antigen gene encoded on the pMT1 for the detection of Y. pestis pure culture and high-quality genomic DNA. Evidently, these two methods cannot detect Y. pestis strains lacking F1 antigen on the plasmid pMT1, and a LAMP method is also needed to detect Y. pestis in actual samples. Based on the LAMP method we constructed in this study, we determined simulated spleen, liver and lung tissue samples combined with magnetic bead capture of Y. pestis DNA.
The genus Yersinia contains 11 species, of which Yersinia enterocolitica, Yersinia pseudotuberculosis and Y. pestis are pathogenic for humans and animals, whereas other eight species, formerly called Y. enterocolitica-like isolates, Yersinia frederiksenii, Yersinia intermedia, Yersinia kristensenii, Yersinia bercovieri, Yersinia mollaretii, Yersinia rohdei, Yersinia ruckeri, and Yersinia aldovae are opportunistic pathogens mostly found in the environment.1 To evaluate the specificity of the primers based on the 3a sequence for the detection of Y. pestis, all 11 species of the genus Yersinia, closely related organisms, were tested in the experiments. The results showed that the primers designed in this study had a high level of specificity for Y. pestis by LAMP or PCR. However, in our recent study, 3a-negative natural isolates of Y. pestis were found in Dingbian County, Shaanxi Province, China,50 indicating that a 3a-based LAMP or PCR method is also not reliable for the detection of Y. pestis. Therefore, a multi-target LAMP or PCR detection method should be developed for the reliable identification of Y. pestis in the future.
To determine the sensitivity for the detection of Y. pestis, we first use serial 10-fold dilutions of high-quality DNA to perform LAMP or PCR assay. The results showed that the lowest detection limit of LAMP or PCR assay was 0.02 or 0.2 ng of Y. pestis DNA, indicating that LAMP assay was 10-fold more sensitive than conventional PCR assay. Then, serial 10-fold dilutions of Y. pestis pure culture were used to crudely extract DNA by boiling, and then detected by LAMP and PCR. The results showed that the sensitivity of LAMP or PCR assay was 2.3 or 23 CFU of Y. pestis, indicating that LAMP assay was 10-fold more sensitive than PCR assay. In addition, the results also showed that the detection of LAMP products by the naked eye was as sensitive as that by a real-time turbidity meter. LAMP amplification can be accomplished within 60 min at an isothermal temperature of 65 °C. Therefore, LAMP assay is a simple, rapid and sensitive method suitable for application in the field, especially in poverty areas.
To evaluate the reliability for the determination of Y. pestis by LAMP and PCR assays in actual samples, we determined Y. pestis in the simulated spleen, liver and lung samples. The results showed that the sensitivity of three simulated samples were much lower than that of Y. pestis pure culture and DNA, indicating that some components in the spleen, liver and lung tissues might inhibit LAMP and PCR reactions. This result was similar to the previous studies in which clinical samples, such as serum, plasma and urine, had an inhibition to both LAMP and PCR assay.51, 52 In addition, our results also showed that the simulated liver sample had a lower sensitivity than the simulated spleen and lung samples for the detection of Y. pestis by LAMP and PCR. This result indicated that there might be more bioactive components in liver tissue that could inhibit LAMP and PCR reactions. Compared with PCR for the detection of three simulated samples, LAMP assay was 100-fold more sensitive than PCR assay, indicating that LAMP was less affected by inhibitory substances present in mouse spleen, liver and lung tissue samples than PCR. LAMP is not only more simple, rapid and sensitive than PCR, but also more suitable to detect spleen, liver and lung tissue samples than PCR.
To further enhance the sensitivity for the detection of actual samples, magnetic beads were used to capture Y. pestis DNAs from three simulated samples. After the DNAs were captured from the simulated spleen and lung samples with magnetic beads, the sensitivity of these two samples were increased for the detection of Y. pestis by LAMP, but the sensitivity of these two samples were unchanged for the detection of Y. pestis by PCR, and LAMP was 1000-fold more sensitive than PCR. After the DNAs were captured from simulated liver samples with magnetic beads, the sensitivity of LAMP and PCR were equally increased, and the sensitivity of LAMP was 100-fold more sensitive than that of PCR. These results indicated that magnetic bead capture of DNAs could remarkably increase the sensitivity of LAMP for the detection of Y. pestis in spleen, liver and lung tissue samples.
Conflicts of interest
The authors declare that they have no competing interests.
Acknowledgement
Financial support for this study came from the National Natural Science Foundation of China (31430006, 81171529).
Associate Editor: Roxane Piazza
Contributor Information
Yusen Zhou, Email: yszhou@bmi.ac.cn.
Xiaoyi Wang, Email: wgenome@163.com.
References
- 1.Perry R.D., Fetherston J.D. Yersinia pestis-etiologic agent of plague. Clin Microbiol Rev. 1997;10:35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cui Y., Yu C., Yan Y. Historical variations in mutation rate in an epidemic pathogen, Yersinia pestis. Proc Natl Acad Sci U S A. 2013;110:577–582. doi: 10.1073/pnas.1205750110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Achtman M., Zurth K., Morelli G., Torrea G., Guiyoule A., Carniel E. Yersinia pestis, the cause of plague, is a recently emerged clone of Yersinia pseudotuberculosis. Proc Natl Acad Sci U S A. 1999;96:14043–14048. doi: 10.1073/pnas.96.24.14043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenfield R.A., Bronze M.S. Prevention and treatment of bacterial diseases caused by bacterial bioterrorism threat agents. Drug Discov Today. 2003;8:881–888. doi: 10.1016/s1359-6446(03)02847-2. [DOI] [PubMed] [Google Scholar]
- 5.Human plague. Review of regional morbidity and mortality 2004–2009. Wkly Epidemiol Rec. 2009;85:40–45. [PubMed] [Google Scholar]
- 6.Stenseth N.C., Atshabar B.B., Begon M. Plague: past, present, and future. PLoS Med. 2008;5:e3. doi: 10.1371/journal.pmed.0050003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riedel S. Plague: from natural disease to bioterrorism. Proc (Bayl Univ Med Cent) 2005;18:116–124. doi: 10.1080/08998280.2005.11928049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inglesby T.V., Dennis D.T., Henderson D.A. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA. 2000;283:2281–2290. doi: 10.1001/jama.283.17.2281. [DOI] [PubMed] [Google Scholar]
- 9.Gaval S.R., Shrikhande S.N., Makhija S.K., Tankhiwale N.S., Pathak A.A., Saoji A.M. Study of suspected plague cases for isolation and identification of Yersinia pestis. Indian J Med Sci. 1996;50:335–338. [PubMed] [Google Scholar]
- 10.Nunes M.P., Suassuna I. Bacteriophage specificity in the identification of Yersinia pestis as compared with other enterobacteria. Rev Bras Pesqui Med Biol. 1978;11:359–363. [PubMed] [Google Scholar]
- 11.Sergueev K.V., He Y., Borschel R.H., Nikolich M.P., Filippov A.A. Rapid and sensitive detection of Yersinia pestis using amplification of plague diagnostic bacteriophages monitored by real-time PCR. PLoS ONE. 2010;5:e11337. doi: 10.1371/journal.pone.0011337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chanteau S., Rahalison L., Ratsitorahina M. Early diagnosis of bubonic plague using F1 antigen capture ELISA assay and rapid immunogold dipstick. Int J Med Microbiol. 2000;290:279–283. doi: 10.1016/S1438-4221(00)80126-5. [DOI] [PubMed] [Google Scholar]
- 13.Chanteau S., Rahalison L., Ralafiarisoa L. Development and testing of a rapid diagnostic test for bubonic and pneumonic plague. Lancet. 2003;361:211–216. doi: 10.1016/S0140-6736(03)12270-2. [DOI] [PubMed] [Google Scholar]
- 14.Splettstoesser W.D., Rahalison L., Grunow R., Neubauer H., Chanteau S. Evaluation of a standardized F1 capsular antigen capture ELISA test kit for the rapid diagnosis of plague. FEMS Immunol Med Microbiol. 2004;41:149–155. doi: 10.1016/j.femsim.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Gomes-Solecki M.J., Savitt A.G., Rowehl R., Glass J.D., Bliska J.B., Dattwyler R.J. LcrV capture enzyme-linked immunosorbent assay for detection of Yersinia pestis from human samples. Clin Diagn Lab Immunol. 2005;12:339–346. doi: 10.1128/CDLI.12.2.339-346.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinnebusch J., Schwan T.G. New method for plague surveillance using polymerase chain reaction to detect Yersinia pestis in fleas. J Clin Microbiol. 1993;31:1511–1514. doi: 10.1128/jcm.31.6.1511-1514.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norkina O.V., Kulichenko A.N., Gintsburg A.L. Development of a diagnostic test for Yersinia pestis by the polymerase chain reaction. J Appl Bacteriol. 1994;76:240–245. doi: 10.1111/j.1365-2672.1994.tb01622.x. [DOI] [PubMed] [Google Scholar]
- 18.Tsukano H., Itoh K., Suzuki S., Watanabe H. Detection and identification of Yersinia pestis by polymerase chain reaction (PCR) using multiplex primers. Microbiol Immunol. 1996;40:773–775. doi: 10.1111/j.1348-0421.1996.tb01140.x. [DOI] [PubMed] [Google Scholar]
- 19.Higgins J.A., Ezzell J., Hinnebusch B.J., Shipley M., Henchal E.A., Ibrahim M.S. 5′ nuclease PCR assay to detect Yersinia pestis. J Clin Microbiol. 1998;36:2284–2288. doi: 10.1128/jcm.36.8.2284-2288.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iqbal S.S., Chambers J.P., Goode M.T., Valdes J.J., Brubaker R.R. Detection of Yersinia pestis by pesticin fluorogenic probe-coupled PCR. Mol Cell Probes. 2000;14:109–114. doi: 10.1006/mcpr.2000.0295. [DOI] [PubMed] [Google Scholar]
- 21.Lindler L.E., Fan W., Jahan N. Detection of ciprofloxacin-resistant Yersinia pestis by fluorogenic PCR using the LightCycler. J Clin Microbiol. 2001;39:3649–3655. doi: 10.1128/JCM.39.10.3649-3655.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loiez C., Herwegh S., Wallet F., Armand S., Guinet F., Courcol R.J. Detection of Yersinia pestis in sputum by real-time PCR. J Clin Microbiol. 2003;41:4873–4875. doi: 10.1128/JCM.41.10.4873-4875.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tomaso H., Reisinger E.C., Al Dahouk S. Rapid detection of Yersinia pestis with multiplex real-time PCR assays using fluorescent hybridisation probes. FEMS Immunol Med Microbiol. 2003;38:117–126. doi: 10.1016/S0928-8244(03)00184-6. [DOI] [PubMed] [Google Scholar]
- 24.Chase C.J., Ulrich M.P., Wasieloski L.P. Real-time PCR assays targeting a unique chromosomal sequence of Yersinia pestis. Clin Chem. 2005;51:1778–1785. doi: 10.1373/clinchem.2005.051839. [DOI] [PubMed] [Google Scholar]
- 25.Woron A.M., Nazarian E.J., Egan C. Development and evaluation of a 4-target multiplex real-time polymerase chain reaction assay for the detection and characterization of Yersinia pestis. Diagn Microbiol Infect Dis. 2006;56:261–268. doi: 10.1016/j.diagmicrobio.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 26.Skottman T., Piiparinen H., Hyytiainen H., Myllys V., Skurnik M., Nikkari S. Simultaneous real-time PCR detection of Bacillus anthracis, Francisella tularensis and Yersinia pestis. Eur J Clin Microbiol Infect Dis. 2007;26:207–211. doi: 10.1007/s10096-007-0262-z. [DOI] [PubMed] [Google Scholar]
- 27.Tomaso H., Jacob D., Eickhoff M. Preliminary validation of real-time PCR assays for the identification of Yersinia pestis. Clin Chem Lab Med. 2008;46:1239–1244. doi: 10.1515/CCLM.2008.251. [DOI] [PubMed] [Google Scholar]
- 28.Qu S., Shi Q., Zhou L. Ambient stable quantitative PCR reagents for the detection of Yersinia pestis. PLoS Negl Trop Dis. 2010;4:e629. doi: 10.1371/journal.pntd.0000629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson G.P., King K.D., Cao L.K., Jacoby M., Ligler F.S., Ezzell J. Quantifying serum antiplague antibody with a fiber-optic biosensor. Clin Diagn Lab Immunol. 1998;5:609–612. doi: 10.1128/cdli.5.5.609-612.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yan Z., Zhou L., Zhao Y. Rapid quantitative detection of Yersinia pestis by lateral-flow immunoassay and up-converting phosphor technology-based biosensor. Sens Actuators B. 2006;119:656–663. doi: 10.1016/j.snb.2006.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wei H., Zhao Y., Bi Y. Direct detection of Yersinia pestis from the infected animal specimens by a fiber optic biosensor. Sens Actuators B. 2007;123:204–210. [Google Scholar]
- 32.Soergel M.E., Schaffer F.L., Blank H.F. Solid-phase radioimmunoassay for detection of plague antigen in animal tissue. J Clin Microbiol. 1982;16:953–956. doi: 10.1128/jcm.16.5.953-956.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thullier P., Guglielmo V., Rajerison M., Chanteau S. Short report: Serodiagnosis of plague in humans and rats using a rapid test. Am J Trop Med Hyg. 2003;69:450–451. [PubMed] [Google Scholar]
- 34.Abbott R.C., Hudak R., Mondesire R., Baeten L.A., Russell R.E., Rocke T.E. A rapid field test for sylvatic plague exposure in wild animals. J Wildl Dis. 2014;50:384–388. doi: 10.7589/2013-07-174. [DOI] [PubMed] [Google Scholar]
- 35.Notomi T., Okayama H., Masubuchi H. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000;28:E63. doi: 10.1093/nar/28.12.e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parida M., Posadas G., Inoue S., Hasebe F., Morita K. Real-time reverse transcription loop-mediated isothermal amplification for rapid detection of West Nile virus. J Clin Microbiol. 2004;42:257–263. doi: 10.1128/JCM.42.1.257-263.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Savan R., Kono T., Itami T., Sakai M. Loop-mediated isothermal amplification: an emerging technology for detection of fish and shellfish pathogens. J Fish Dis. 2005;28:573–581. doi: 10.1111/j.1365-2761.2005.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mori Y., Notomi T. Loop-mediated isothermal amplification (LAMP): a rapid, accurate, and cost-effective diagnostic method for infectious diseases. J Infect Chemother. 2009;15:62–69. doi: 10.1007/s10156-009-0669-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horisaka T., Fujita K., Iwata T. Sensitive and specific detection of Yersinia pseudotuberculosis by loop-mediated isothermal amplification. J Clin Microbiol. 2004;42:5349–5352. doi: 10.1128/JCM.42.11.5349-5352.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ranjbar R., Afshar D. Development of a loop-mediated isothermal amplification assay for rapid detection of Yersinia enterocolitica via targeting a conserved locus. Iran J Microbiol. 2015;7:185–190. [PMC free article] [PubMed] [Google Scholar]
- 41.Radnedge L., Gamez-Chin S., McCready P.M., Worsham P.L., Andersen G.L. Identification of nucleotide sequences for the specific and rapid detection of Yersinia pestis. Appl Environ Microbiol. 2001;67:3759–3762. doi: 10.1128/AEM.67.8.3759-3762.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cornelis G.R. Yersinia type III secretion: send in the effectors. J Cell Biol. 2002;158:401–408. doi: 10.1083/jcb.200205077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang H., Tan Y., Zhang T. Identification of novel protein–protein interactions of Yersinia pestis type III secretion system by yeast two hybrid system. PLOS ONE. 2013;8:e54121. doi: 10.1371/journal.pone.0054121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lathem W.W., Price P.A., Miller V.L., Goldman W.E. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science. 2007;315:509–513. doi: 10.1126/science.1137195. [DOI] [PubMed] [Google Scholar]
- 45.Zimbler D.L., Schroeder J.A., Eddy J.L., Lathem W.W. Early emergence of Yersinia pestis as a severe respiratory pathogen. Nat Commun. 2015:1–10. doi: 10.1038/ncomms8487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Felek S., Muszynski A., Carlson R.W., Tsang T.M., Hinnebusch B.J., Krukonis E.S. Phosphoglucomutase of Yersinia pestis is required for autoaggregation and polymyxin B resistance. Infect Immun. 2010;78:1163–1175. doi: 10.1128/IAI.00997-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Friedlander A.M., Welkos S.L., Worsham P.L. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin Infect Dis. 1995;21(Suppl. 2):S178–S181. doi: 10.1093/clinids/21.supplement_2.s178. [DOI] [PubMed] [Google Scholar]
- 48.Dong W., Jieying W., Guozhi W. Development of loop-mediated isothermal amplification method for detection of Yersinia pestis. Chin J Health Lab Technol. 2012;22:2074–2077. [Google Scholar]
- 49.Nunes M.L., Mendes-Marques C.L., Almeida A.M.P., Leal N.C. The development of a loop-mediated isothermal amplification (LAMP) procedure for plague diagnostic. Am J Anal Chem. 2014;5:1069–1077. [Google Scholar]
- 50.Qi Z., Wu Y., Li Y. 3a-Negative Yersinia Pestis, China. Infect Dis Transl Med. 2015;1:61–62. [Google Scholar]
- 51.Kaneko H., Kawana T., Fukushima E., Suzutani T. Tolerance of loop-mediated isothermal amplification to a culture medium and biological substances. J Biochem Biophys Methods. 2007;70:499–501. doi: 10.1016/j.jbbm.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 52.Nkouawa A., Sako Y., Li T. Evaluation of a loop-mediated isothermal amplification method using fecal specimens for differential detection of Taenia species from humans. J Clin Microbiol. 2010;48:3350–3352. doi: 10.1128/JCM.00697-10. [DOI] [PMC free article] [PubMed] [Google Scholar]