Abstract
Objectives
To examine trajectories of adolescent psychosocial risk—drug use, depressive and anxiety symptoms, and violence victimization and observation—and the longitudinal relationship between psychosocial risk trajectories during adolescence and HIV risk behaviors in adulthood.
Methods
The eighteen-year longitudinal study was conducted from September 1994 through May 2013, in Michigan. Eight-hundred and fifty predominantly (80%) African American adolescents completed demographics and measures of drug use, depressive and anxiety symptoms, violence victimization and observation at Times 1-4, sexual risk behaviors at Times 5 and 6, and social conditions (i.e., family, peer, and community-level factors) between 14.9 and 32.0 years of age.
Results
Growth mixture modeling revealed two trajectories of psychosocial risk factors which can be characterized as a syndemic index: High-Frequency and Low-Frequency. The High-Frequency class was more likely to report HIV risk behaviors, including condomless sex at last sexual intercourse with their primary and secondary partner, sexual intercourse with someone they just met, ≥ 4 sexual partners, and licit and illicit drug use prior to sexual intercourse at Time 5 (mean age 23.1). At Time 6 (mean age 32.0), the High-Frequency class was more likely to report sexual intercourse with someone they just met and ≥ 4 sexual partners, relative to the Low-Frequency class. Additionally, the High-Frequency class was linked to peer and family-level indicators of social conditions.
Conclusion
A syndemic index comprised of co-occurring psychosocial risk factors in adolescence seem to have lasting effects on the vulnerability to engage in HIV risk behaviors in emerging adulthood, some of which extend into middle adulthood.
Keywords: Adolescents, HIV syndemics, longitudinal
The human immunodeficiency virus (HIV) remains a significant public health concern in the United States, and African American adolescents and young adults are disproportionately affected [1]. The highest prevalence of new HIV infections is among adolescents and young adults aged 20–29 years [2,3]. African American adolescents accounted for approximately 56.2% (i.e., 5,464) of the estimated 9,731 youth aged 13–24 diagnosed with HIV in 2014—a rate three times that of non-Hispanic white youth [2]. Approximately 90.7% of all new HIV infections among African American females can be attributed to heterosexual contact [1]. Young Black men who have sex with men account for 44.4% of new HIV infections among 13–24-year-olds [2]. Moreover, youth aged 15 and 24 constitute approximately one quarter of the sexually active population, but account for half of the 20 million new sexually transmitted infections (STIs) that occur in the United States each year [4]. African American youth bear disproportionate prevalence of STIs, and the presence of an STI enhances vulnerability to HIV infection [5].
Drug use, mental distress, and violence exposure are prominent psychosocial risk factors among African American youth [6], and may enhance vulnerability to HIV infection. Consequently, comprehensive and timely prevention of these risk factors is essential to improving adolescent health [7]. In fact, federal recommendations [8, 9] underscore the urgent need for clinicians to screen for psychosocial risk factors—including drug use, mental distress, and violence exposure—which are associated with HIV risk behaviors among African American youth such as condomless sex, sexual intercourse with someone just met, multiple sexual partners, and drug use before intercourse [10].
Syndemics, defined as the constellation of multiple risk factors that operate in a synergistic manner, increases vulnerability in disease burden [11,12]. Within this framework, syndemic theory affirms that psychosocial risk factors are interconnected, co-occur in a dynamic and reciprocally influential manner, and unfold in the context of social conditions, thereby enhancing vulnerability for HIV infection [13, 14]. A growing number of researchers have applied syndemic theory to understand how multiple psychosocial risk factors shape HIV risk and vulnerability [15], including condomless sex [16–20], and drug use prior to sex [21]. Longitudinal research also supports the notion that multiple psychosocial risk factors increase HIV vulnerability over time. Mustanski and colleagues [19], for example, demonstrated that a latent syndemic index of psychosocial risk predicted condomless anal sex among men who have sex with men over a six-month period. Few researchers [16–21], however, have employed a longitudinal design over several years or focused on other vulnerable populations other than sexual and gender minorities.
Our eighteen-year longitudinal study uses the syndemic model as a guiding framework [22–25] to address important gaps in the literature by: (1) examining the feasibility of collapsing three psychosocial risk factors onto a latent variable that includes drug use, mental distress, and violence exposure; (2) modeling developmental trajectories of this latent factor syndemic index; (3) examining how these trajectories are associated with HIV vulnerability in emerging and young adulthood; and (4) examining how individual, family, peer, community-level factors predict class membership in a sample of predominantly African American adolescents.
Methods
Participants
We use data from six time points of a longitudinal study of alcohol and other drug (AOD) use and high school dropout among adolescents in Flint, Michigan. To be eligible for this study, participants had to be: (a) enrolled in one of the four Flint public high schools, (b) have a grade point average of 3.0 or lower at the end of eighth grade, and (c) self-identify as African American, non-Hispanic white, or both. Exclusion criteria included adolescents who were diagnosed as emotionally or developmentally impaired by the school. A total of 850 participants enrolled in the study at time 1 and were followed over an eighteen-year period without the replacement of participants. Approximately 50% of the study sample was female, and the mean age of participants at Time 1 was 14.9 years (SD = 0.64; Range 13.9–16.9). Participants were predominately African American (N = 681, or 80%), followed by non-Hispanic white (N = 143, or 17%), and mixed African American and non-Hispanic white (N = 26, or 3%), respectively.
Procedure
Study approval was granted from our Institutional Review Board and from staff at the four participating high schools. Participant consent and passive parental consent for minors were obtained prior to participation in the study. Adolescents were assessed at six time points during adolescence and young adulthood, corresponding to baseline, one, two, three, nine, and eighteen years post-baseline. In Times 1-4 of data collection, participants were interviewed face-to-face in private rooms at their school; participants who had dropped out of school were contacted and interviewed at home or at another location. In Times 5 and 6, participants were interviewed either in their homes or community settings [26]. Interviews lasted approximately 60 minutes. To prevent attrition, participants’ contact information provided as part of the interviews were used for initiating follow-up contact in later time points. The LexisNexis Accurint® service was used to locate individuals. The Accutrint service was used in tracking for the Longitudinal Study of American Youth (LSAY). At each follow-up time point, participants were asked if they would like to continue participating in the study. Participants were given an incentive ($15 for Time 1, $20 for Time 2, $25 for Times 3 and 4, and $35 for Times 5 and 6) for taking time to participate in the study [27–29].
Measures
Demographics (Time 1, mean age= 14.9)
Participants reported their age (birth month & year), gender, race, and grade. Family Socioeconomic Status (SES) score was assessed based on the highest occupational prestige score of either of the participant’s parents [30]. The mean occupational prestige score was 39.92 (SD = 10.4; Range = 29.28–64.38), which represented blue-collar employment.
Psychosocial risk factors (Times 1–4, mean ages= 14.9 - 17.9)
We assessed adolescent psychosocial risk factors, including AOD use, mental distress, and violence exposure. Cronbach’s alphas are provided as a range across Times 1–4.
AOD use (2 items, α = .65–.70) was assessed using items from the Monitoring the Future study [31]. Participants were asked to respond to the frequency with which they used alcohol and marijuana in the past 30 days. Response choices ranged from 1 = never to 7 = 40+ times.
Depressive (6 items, α = .79–.86) and anxiety symptoms (6 items, α =.77–.88) were assessed using the corresponding subscales from the Brief Symptom Inventory [32]. The response choices for both scales ranged from 1 = Not at all to 5 = Extremely. The depressive symptoms subscale measures adolescents’ feelings of sadness and hopelessness. A sample question included, “During the past week, including today, please tell me how uncomfortable you felt because of the following problems: Thoughts of ending your life?” The anxiety symptoms subscale measures adolescents’ feelings of anxiety and restlessness. A sample question included, “During the past week, including today, please tell me how uncomfortable you felt because of the following problems: Nervousness or shakiness inside?”
Violence victimization (3 items, α =.52–.65) assessed how often participants had “someone threaten to hurt me”, “something taken from me by physical force”, and “experienced being physically assaulted or hurt by someone” in the past 12 months. The response choices ranged from 1 = 0 times to 5 = 4+ times. Observed violence (2 items, α =.68–.83) assessed the frequency of seeing someone commit a violent crime where a person was hurt and seeing someone get shot, stabbed or beaten up the past 12 months. The response choices ranged from 1 = 0 times to 5 = 4+ times.
HIV risk behaviors (Times 5 and 6, mean ages 23.1 and 32.0)
Separate binary variables were created to assess each HIV risk behavior. The variables were coded as 1 if the youth had engaged in the behavior and 0 if not.
Adolescents’ STI was measured by one item that asked, “In the last 12 months, have you been newly diagnosed as having a sexually transmitted disease such as syphilis or gonorrhea?” Condomless sex with primary partner at last sexual intercourse was measured by one item that asked, “Did you (or your partner) use a condom the last time you had sexual intercourse (sex) with your primary partner?” Condomless sex with secondary partner at last sexual intercourse was measured by one item that asked, “Did you (or your partner) use a condom the last time you had sexual intercourse (sex) with your secondary partner?” Number of sexual partners was measured with one item that asked, “How many sex partners have you had in the last 12 months?” We coded as 1 if participant reported ≥ 4 sexual partners, and 0 otherwise. Sexual intercourse with someone the participant just met was assessed with one item that asked, “With how many different people that you just met did you have sex in the last 12 months?” Alcohol use prior to last sexual intercourse was measured with one item that asked, “In the last 12 months, when you had sexual intercourse (sex), how often did you use alcohol?” Drug use prior to last sexual intercourse was assessed with one item that asked, “In the last 12 months, when you had sexual intercourse (sex), how often did you use any illegal drugs?”
Social conditions (Time 1, mean age= 14.9)
Family
We assessed adolescents’ parent support, including perceived emotional and instrumental support from parents, and the closeness of the parent-child relationship (5 items, α = .89) [33]. A sample statement included, “I rely on my mother/father for emotional support.” Response choices ranged from 1 =not true to 5 =very true. Adolescents’ negative family environment was assessed using the Family Conflict Scale (5 items, α = .76) [34]. A sample statement included, “We fight in our family.” Response choices ranged from 1=hardly ever to 4 =often.
Peer
We assessed participants’ perceived peer support (5 items, α = .82) [33]. A sample statement included, “My friends enjoy hearing about what I think.” Response choices ranged from 1 =not true to 5 =very true. We assessed negative peer influence (13 items, α = .89) [35,36]. A sample question included, “How many of your friends have been busted for having drugs?” Response choices ranged from 1 = none to 5 = all.
Community
We assessed adolescents’ fear of violence in school (2 items) and community (3 items, α = .45) [37]. Sample statements for school included, “I am afraid I will get hurt by someone in my school,” and community, “I am afraid of the violence in my neighborhood.” Response choices ranged from 1=strongly disagree to 5 =strongly agree.
Analytic Approach
Analyses were conducted using Mplus version 7 [38]. Missing data were handled using full information maximum likelihood (FIML). Good model fit is represented as CFI ≥ .95, RMSEA ≤ .05, and SRMR ≤ .06; and adequate fit is represented as CFI ≥ .90, RMSEA ≤ .08, and SRMR ≤ .08 [39]. The analytic approach proceeded in five steps. First, we conducted a descriptive statistics and attrition analysis. Second, we computed a confirmatory factor analysis to ascertain the feasibility of collapsing the three psychosocial risk factor indicators of a syndemic index (i.e., AOD use, depressive and anxiety symptoms, and violence victimization and observation) onto a single latent variable. Third, we estimated growth mixture models (GMM) with maximum likelihood estimation to examine linear slopes to identify number of class trajectories for our syndemic index [40]. Good model fit is represented by relatively smaller values for the Akaike Information Criteria (AIC), Bayesian Information Criterion (BIC) and sample-adjusted BIC, > .80 entropy, and Vuong-Lo-Mendell-Rubin (VLMR) p<.05 [41–44]. Fourth, we tested if trajectories of a latent psychosocial risk factors variable at Times 1–4 (high school years) are associated with HIV vulnerability at Times 5 and 6. We included covariates to account for baseline levels of HIV risk behaviors and group differences based on gender, age, and race. Finally, we examined individual-level and social condition influences on syndemic index trajectories by regressing individuals’ class membership on individuals’ demographic and social condition predictors.
Results
Attrition Analysis
Retention rates at Times 1-4 were 94% (n = 799), 90.4% (n = 768), and 87.8% (n = 746), respectively. Sample retention was 68.1% (n = 579) at Time 5 and 45.2% (n = 384) at Time 6 (approximately 18 years post-baseline). When we compared participants missing at Time 6 with youth present at 18 years post-baseline we found no differences by race, χ2(2) = 0.14 (p = .93) or socioeconomic status, t(748) = .05 (p = .95). A higher proportion of the 18 years post-baseline sample was female (57.7%) compared to baseline (50%), χ2 (1) = 16.02 (p < .001). Those present at Time 6 were approximately a month younger at baseline than youth who left the study (t(848) = 2.95, p < .01). Participants present at Time 6 did not differ from those who left the study for baseline condomless sex (χ2(1) = 0.13, p = .93) or number of sexual partners (χ2(1) = 1.06, p = .72).
Confirmatory Factor Analysis
We computed a confirmatory factor analysis to ascertain the feasibility of collapsing three psychosocial risk factor indicators of a syndemic index into a latent construct. The model provided a good fit to the data, χ2 (198) = 675.81, p < .001, CFI = .94; RMSEA = .05, SRMR = .076. Standardized loadings ranged from .27 to .86.
Identifying Number of Classes
Growth mixture modeling (GMM) yielded a two-class solution. When compared to a two-class solution (AIC = 2871.05, BIC = 2913.76, sample-adjusted BIC= 2885.17, entropy = .94), the AIC, BIC, and sample-adjusted BIC decreased in the three-class solution (AIC = 1543.59, BIC = 1600.53, sample-adjusted BIC = 1562.42, entropy = .94), suggesting an improvement in model fit. Yet, the VLMR p=. 0.28 criteria indicated a model fit improvement in the two-class solution as compared to the three-class solution. Therefore, we retained the two-class model as the most parsimonious model. Class 1, hereafter referred to as High Frequency of Interaction (intercept = 0.63, p < .001; slope = 0.08, p < .001), consisted of 23.8% (n = 203) of the sample. Approximately 76.1% (n = 647) of adolescents were in class 2, referred to as Low Frequency of Interaction (intercept = –0.20, p < .001; slope = –0.02, p < .001). Whereas the High Frequency of Interaction class was characterized by relatively higher frequency of psychosocial risk factors at Time 1 and increased over time, the Low Frequency of Interaction class was characterized by relatively lower frequency of psychosocial risk factors at Time 1 and decreased over time (Figure 1). Descriptive statistics for the total sample and by class membership on demographics, psychosocial risk factors at Times 1-4, and HIV risk outcomes at Times 5-6 are reported in Tables 1 and 2.
Figure 1.
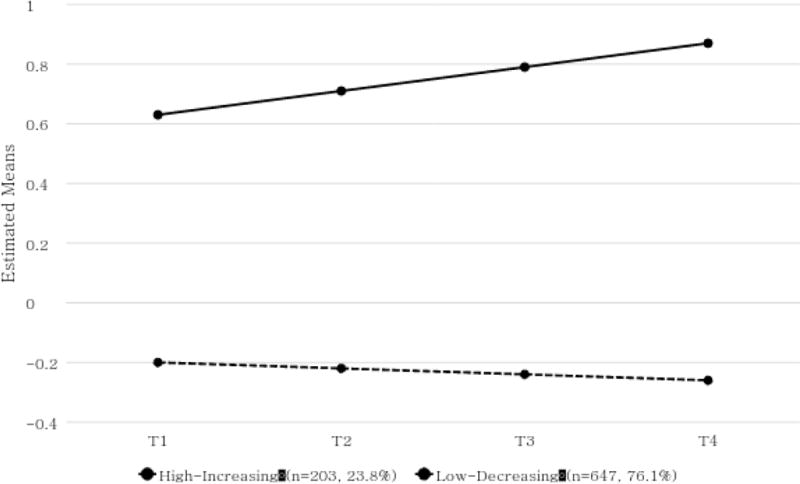
Trajectories of psychosocial risk factor indicators of syndemic index
Table 1.
Baseline demographics and behavioral outcomes at Time 5 and 6 by class
| Variable | N | Low Frequency of Interaction | High Frequency of Interaction | Test Statistic§ |
|---|---|---|---|---|
| Demographic | 850 | |||
| Age | 850 | 14.82 (.03) | 14.96 (.05) | −2.62** |
| Gender (% Female) | 850 | 53.2% | 45.5% | 3.41+ |
| SESǂ | 690 | 40.3 (.26) | 39.0 (.77) | 1.32 |
| Race (%) | 7.02* | |||
| Black | 681 | 81.5% | 73.8% | |
| White | 143 | 15.7% | 24.1% | |
| Mixed Race | 26 | 2.9% | 2.1% | |
| Behavioral outcomes (%) | ||||
| STI (time 5) | 560 | 1.51% | 2.48% | 0.51 |
| STI (time 6) | 365 | 0.40% | 1.11% | 0.59 |
| Condomless sex with primary partner (time 5) | 421 | 58.0% | 70.8% | 4.76* |
| Condomless sex with primary partner (time 6) | 264 | 82.0% | 84.4 | 0.19 |
| Condomless sex with secondary partner (time 5) | 184 | 26.3% | 43.4% | 4.87* |
| Condomless sex with secondary partner (time 6) | 85 | 44.7% | 26.7% | 2.53 |
| ≥ 4 sex partners (time 5) | 501 | 9.7% | 17.9% | 5.50* |
| ≥ 4 sex partners (time 6) | 329 | 3.1% | 10.7% | 7.31** |
| Sex with someone just met (time 5) | 497 | 14.9% | 23.7% | 4.63* |
| Sex with someone just met (time 6) | 330 | 3.5% | 11.9% | 7.90** |
| Drug use during sex (time 5) | 492 | 20.9% | 53.6% | 44.01*** |
| Drug use during sex (time 6) | 324 | 8.5% | 14.5% | 2.38 |
| Alcohol use during sex (time 5) | 492 | 43.4% | 71.2% | 26.01*** |
| Alcohol use during sex (time 6) | 324 | 14.3% | 20.48% | 1.73 |
Note.
T-statistic for mean comparisons, chi-square statistic for categorical associations.
Based on sample of n = 690 due to missing data
Table 2.
Mean scores (standard deviation) of the three psychosocial health problem indicators of HIV syndemics-index
| Licit and illicit drug use | Mental health problems | Violence | ||||
|---|---|---|---|---|---|---|
| Past 30 day alcohol use | Past 30 day marijuana use | Anxiety symptoms | Depressive symptoms | Violence victimization | Observed violence | |
| Time 1 | ||||||
| Low frequency | 1.23 (0.58) | 1.26 (0.81) | 1.50 (0.52) | 1.54 (0.57) | 1.35 (0.54) | 2.02 (1.09) |
| High frequency | 2.33 (1.43) | 2.69 (1.92) | 1.92 (0.79) | 2.00 (0.90) | 1.82 (0.76) | 2.84 (1.26) |
| Total sample | 1.49 (.98) | 1.59 (1.32) | 1.6 (.62) | 1.65 (.69) | 1.47 (.63) | 2.22 (1.18) |
| Time 2 | ||||||
| Low frequency | 1.29 (0.65) | 1.36 (0.93) | 1.69 (0.79) | 1.76 (0.83) | 1.27 (0.44) | 1.91 (1.07) |
| High frequency | 2.50 (1.40) | 3.78 (2.03) | 1.96 (0.90) | 2.12 (0.97) | 1.73 (0.77) | 2.94 (1.32) |
| Total sample | 1.57 (1.02) | 1.93 (1.64) | 1.76 (.82) | 1.84 (.87) | 1.38 (.57) | 2.15 (1.21) |
| Time 3 | ||||||
| Low frequency | 1.28 (0.67) | 1.41 (1.03) | 1.60 (0.74) | 1.69 (0.80) | 1.22 (0.42) | 1.66 (0.91) |
| High frequency | 2.84 (1.65) | 3.78 (2.24) | 2.00 (0.79) | 2.15 (0.91) | 1.70 (0.74) | 2.78 (1.24) |
| Total sample | 1.64 (1.18) | 1.96 (1.73) | 1.69 (.77) | 1.79 (.84) | 1.33 (.55) | 1.92 (1.10) |
| Time 4 | ||||||
| Low frequency | 1.35 (0.76) | 1.51 (1.18) | 1.60 (0.82) | 1.65 (0.83) | 1.21 (0.41) | 1.50 (0.79) |
| High frequency | 2.86 (1.63) | 4.07 (2.33) | 2.05 (0.96) | 2.14 (1.01) | 1.64 (0.74) | 2.59 (1.32) |
| Total sample | 1.79 (1.21) | 2.09 (1.86) | 1.71 (.87) | 1.76 (.72) | 1.30 (.53) | 1.74 (1.04) |
Syndemic Index Classes Predicting HIV Risk Behaviors at Times 5 and 6
While controlling for baseline levels of the HIV risk behaviors, the High-Frequency class was more likely to report condomless sex at last sexual intercourse with their primary (AOR = 1.82, 95% Confidence Interval [CI] = 1.86 – 3.13) and secondary partner (AOR = 2.22, CI = 1.07 – 4.64), as compared to the Low Frequency of Interaction class at Time 5 (Table 3). Furthermore, relative to the Low Frequency of Interaction class, the High Frequency of Interaction class was more likely to report sexual intercourse with someone they just met (AOR= 1.79, CI = 1.04 – 3.08), ≥ 4 sexual partners (AOR= 2.06, CI = 1.10 – 3.84), and alcohol (AOR = 3.57, CI = 2.13 - 5.88) or illicit drug use (AOR = 4.42, CI = 2.73 - 7.14) prior to sexual intercourse at Time 5. Moreover, relative to the Low Frequency of Interaction class, the High Frequency of Interaction class was more likely to report sexual intercourse with someone they just met (AOR= 3.62; CI = 1.34 – 9.80) and ≥ 4 sexual partners (AOR= 3.68; CI = 1.28 – 10.60) at Time 6.
Table 3.
Psychosocial risk factor indicators of syndemic index and links to HIV risk behaviors at Times 5 and 6
| STI | Condomless Sex (Primary Partner) |
Condomless Sex (Secondary Partner) |
≥4 Sex Partners | Sex with Someone Just Met |
Drug Use during Sex |
Alcohol Use during Sex |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | Timepoint | |
| 5 | 6 | 5 | 6 | 5 | 6 | 5 | 6 | 5 | 6 | 5 | 6 | 5 | 6 | |
| Odds Ratio (CI) High Frequency versus Low Frequency | 1.61 (.37, 7.14) | 1.11 (0.51, 2.43) | 1.82 (1.06, 3.13) | 1.11 (0.51, 2.43) | 2.22 (1.07, 4.64) | 0.41 (0.14, 1.18 | 2.06 (1.10, 3.84) | 3.68 (1.28, 10.60) | 1.79 (1.04, 3.08) | 3.62 (1.34, 9.80) | 4.42 (2.73, 7.14) | 0.55 (.24, 1.25) | 3.57 (2.13, 5.88) | 0.63 (0.32, 1.26) |
Social Conditions Predicting Class Membership
Members in the High Frequency of Interaction class were more likely to report higher levels of peer support (OR=1.36, CI = 1.08 – 1.72) and negative peer influence (OR=4.62, CI = 3.00 – 7.11), and lower levels of parent support (OR=0.72, CI = 0.58 – 0.90) compared to members in the Low Frequency of Interaction class (Table 4).
Table 4.
Classes and unadjusted odds ratio [confidence interval] by Individual-level and social condition predictors
| Predictor | High Frequency of Interaction Membership |
|---|---|
| Demographics | |
| Age | 1.31 [0.97, 1.75] |
| Gender | 1.96 [1.27, 3.04] |
| Race | |
| Black | 0.50 [0.29, .085] |
| Mixed | 0.45 [0.11, 1.81] |
| Individual-level | |
| Baseline Condomless Sex | 1.69 [1.08, 2.63] |
| Baseline Number of Partners | 1.85 [1.07, 3.19] |
| Family-level | |
| Parent support | 0.72 [0.58, 0.90] |
| Family conflict | 1.35 [0.85, 2.14] |
| Peer-level | |
| Peer support | 1.36 [1.08, 1.72] |
| Negative peer influence | 4.62 [3.00, 7.11] |
| Community-level | |
| Fear of school violence | 0.95 [0.70, 1.28] |
| Fear of neighborhood violence | 0.95 [0.66, 1.35] |
Discussion
This study is among the first to examine how psychosocial risk factors experienced in adolescence—a developmental period of enhanced vulnerability—shape HIV risk behaviors in emerging and young adulthood. Sexual risk behaviors in emerging adulthood occurred with a relatively high level of frequency among participants in the high frequency class who were also more likely to report sexual risk behaviors in young adulthood relative to the low frequency class. Additionally, findings highlight the social conditions that are predictive of class membership. Findings suggest that comprehensive and timely screening of psychosocial risk factors in adolescents may help reduce HIV vulnerability in adulthood.
Consistent with researchers that have used a latent construct approach [19, 45], our confirmatory factor analysis results revealed the feasibility of collapsing multiple indicators of psychosocial risk factors, including AOD, mental distress, and violence exposure, onto a single latent variable. Researchers [19] have modeled a latent construct of psychosocial risk factors at one timepoint, but our findings expand on this research by modeling a syndemic index across four timepoints that correspond to developmental moments of enhanced vulnerability.
Our growth mixture model approach allowed us to identify two distinct subgroups of psychosocial risk factors; one defined by a relatively higher starting point of a syndemic index that increased overtime, and a second with a relatively lower starting point that decreased overtime. Notably, nearly one in four participants were in the high frequency class. These findings are clinically meaningful and underscore the urgent need to routinely screen for psychosocial risk factors among vulnerable adolescents as recommended by several federal institutions [8,9]. Routine screening of psychosocial risk factors may provide opportunities for preventive services, including linkage to care and the identification of adolescents eligible for Pre-exposure prophylaxis (PrEP) [46].
Our findings also have important theoretical implications. Using the syndemic model [13,14] as a guiding framework, our findings provide evidence that increasing psychosocial risk factors experienced in adolescence may have effects that span nearly two decades. The syndemic model [13,14] also posits that multiple psychosocial risk factors should be considered in the context of social conditions. In this sample, family and peer-level factors were associated with greater risk. This is not surprising given that family and peers are most proximal during adolescent development and often the focus for HIV prevention among adolescents [47,48]. In a recent review of 71 studies in the syndemic literature between 2003-2016, 15 studies have been longitudinal and 3 have focused on adolescents. Thus, our findings contribute to the syndemic literature in new and significant ways. Our study suggests that future research that examines population-level outcomes and the multiplicative effects of psychosocial risk factors would be informative [49,50].
Researchers [16–21] have found that increasing psychosocial risk factors shape HIV risk behaviors among adolescents, but these studies are mostly cross-sectional or relatively short longitudinal studies. Our findings suggest that increasing psychosocial risk factors experienced in adolescence have lasting effects on HIV risk behaviors into emerging and young adulthood. These findings indicate that HIV prevention strategies may be effective if they focused on psychosocial risk factors among vulnerable adolescents. Consistent with syndemic theory [13,14], the additive effects of psychosocial risk indicate a need for intervention strategies that address multiple risk factors [49,50]. Addressing psychosocial risk factors at the individual, interpersonal and socio-ecological level may be particularly useful during adolescence as it may provide primary prevention of HIV risk into young adulthood [51]. This may be an especially useful strategy to reduce disparities in HIV infection between African American and non-Hispanic white adolescents [1].
Limitations
The present study has several limitations. This study was composed of participants from a Midwest urban and economically challenged setting who predominately identified as African American. Thus, study findings may not be generalizable to all adolescents, including sexual and gender minorities. Nevertheless, this is a population at risk for both exposure to risk factors we studied and HIV infection and may be a vital group to study. Additionally, as with much of the work in the psychosocial risk factors literature, we relied on self-report data, the nature of which is subject to recall and social desirability bias, and under- or over-reporting of sexual risk behaviors. Thus, future research that includes biomarker data may be especially useful.
Conclusions
Our findings support the notion that increasing psychosocial risk factors enhance HIV vulnerability among adolescents in important ways, and have effects on HIV risk behaviors decades later. Our results also suggest that screening for psychosocial risk factors during adolescence may have a salutary effect on HIV risk and transmission in emerging and young adulthood. Furthermore, our findings suggest that interventions that focus on the multidimensional nature of psychosocial risk factors may be warranted. Doing so may help reduce HIV disparities and improve health equity in vulnerable populations.
Acknowledgments
DC, JH, and MAZ conceived the study and interpreted the findings. DC, JH, HFH, and RM drafted the manuscript. JH did the statistical analyses with aid from DC, HFH, and MAZ. DC, JH, HFH, RM, CPSW, SC, and MAZ helped with data acquisition, interpretation of the findings, and drafting the manuscript. DC, JH, and MAZ were involved in revising the manuscript for important intellectual content. All authors read and approved the final manuscript.
Source of Funding:This research was funded by the National Institute on Drug Abuse, Grant DA07484 (Principal Investigator: Marc A. Zimmerman). The research reported here does not necessarily reflect the views or policies of the National Institute on Drug Abuse. Preparation of this article was supported, in part, by the National Institute of Mental Health, Grant R25 MH067127, National Institute on Minority Health and Health Disparities Loan Repayment Program, Grant 1L60MD006269-01, and National Institute on Drug Abuse, Grant 1R03DA041891-01A1 awarded to David Córdova.
Footnotes
Conflicts of Interest: All authors declare no competing interests.
References
- 1.Centers for Disease Control and Prevention (CDC) HIV Among Youth. http://www.cdc.gov/hiv/group/age/youth. Updated April 7, 2017. Accessed April 6, 2017.
- 2.Centers for Disease Control and Prevention (CDC) HIV Surveillance Report. 2015;27 https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. Published November 2016. Accessed April 6, 2017. [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Sexually Transmitted Disease Surveillance. 2014 https://www.cdc.gov/std/stats14/surv-2014-print.pdf. Published November 2015. Accessed April 6, 2017.
- 4.Centers for Disease Control and Prevention (CDC) Adolescents and Young Adults. https://www.cdc.gov/std/life-stages-populations/adolescents-youngadults.htm. Updated March 10, 2017. Accessed April 6, 2017.
- 5.Centers for Disease Control and Prevention (CDC) HIV Among African American Youth. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/archive/cdc-youth-aas-508.pdf. Published February 2014. Accessed April 6, 2017.
- 6.Kann L, McManus T, Harris WA, et al. Youth Risk Behavior Surveillance United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 7.Global Burden of Disease Pediatrics Collaboration. Child and adolescent health from 1990 to 2015: Findings from the global burden of diseases, injuries, and risk factors 2015 study. JAMA Pediatr. 2017 doi: 10.1001/jamapediatrics.2017.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Human immunodeficiency virus (HIV) infection: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/human-immunodeficiency-virus-hiv-infection-screening. Published April 2013. Accessed April 6, 2017.
- 9.Centers for Disease Control and Prevention (CDC) HIV Testing in Clinical Settings. https://www.cdc.gov/hiv/testing/clinical/. Updated November 15, 2016. Accessed April 6, 2017.
- 10.Substance Abuse and Mental Health Services Administration and Health Resources and Services Administration. The Case for Behavioral Health Screening in HIV Care Settings. Rockville, MD: 2016. http://store.samhsa.gov/shin/content/SMA16-4999/SMA16-4999.pdf. [Google Scholar]
- 11.Blashill AJ, Bedoya CA, Mayer KH, et al. Psychosocial syndemics are additively associated with worse ART adherence in HIV-infected individuals. AIDS Behav. 2015;19:981–986. doi: 10.1007/s10461-014-0925-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Distefano AS, Cayetano RT. Health care and social service providers’ observations on the intersection of HIV/AIDS and violence among their clients and patients. Qual Health Res. 2011;21(7):884–899. doi: 10.1177/1049732311403501. [DOI] [PubMed] [Google Scholar]
- 13.Singer M, Clair S. Syndemics and public health: Reconceptualizing disease in bio-social context. Med Anthropol Q. 2004;17(4):423–41. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 14.Singer M. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. San Francisco, CA: Jossey-Bass; 2009. [Google Scholar]
- 15.Friedman MR, Stall R, Silvestre AJ, et al. Effects of syndemics on HIV viral load and medication adherence in the multicentre AIDS cohort study. AIDS. 2015;29:1087–1096. doi: 10.1097/QAD.0000000000000657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dyer TP, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to Black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Heal Bull New York Acad Med. 2012;89(4):697–708. doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pitpitan EV, Smith LR. “‘ Outness ’” as a moderator of the association between syndemic conditions and HIV risk-taking behavior among men who have sex with men in Tijuana, Mexico. AIDS Behav. 2016;20(2):431–438. doi: 10.1007/s10461-015-1172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van den Berg JJ, Isabel Fernández M, Fava JL, Operario D, Rudy BJ, Wilson PA. Using syndemics theory to investigate risk and protective factors associated with condomless sex among youth living with HIV in 17 U.S. cities. AIDS Behav. 2017;21(3):833–844. doi: 10.1007/s10461-016-1550-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mustanski B, Phillips G, Ryan DT, Swann G, Kuhns L, Garofalo R. Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS Behav. 2017;21(3):845–857. doi: 10.1007/s10461-016-1607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mimiaga MJ, OʼCleirigh C, Biello KB, et al. The effect of psychosocial syndemic production on 4-Year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. JAIDS J Acquir Immune Defic Syndr. 2015;68(3):329–336. doi: 10.1097/QAI.0000000000000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Friedman MR, Kurtz SP, Buttram ME, Wei C, Silvestre AJ, Stall R. HIV risk among substance-using men who have sex with men and women (MSMW): Findings from South Florida. AIDS Behav. 2014;18(1):111–119. doi: 10.1007/s10461-013-0495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brennan J, Kuhns LM, Johnson AK, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–1757. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. http://www.ncbi.nlm.nih.gov/pubmed/12773359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nehl EJ, Klein H, Sterk CE, Elifson KW. Prediction of HIV sexual risk behaviors among disadvantaged African American adults using a syndemic conceptual framework. AIDS Behav. 2015;20(2):449–460. doi: 10.1007/s10461-015-1134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurd NM, Sánchez B, Zimmerman MA, Caldwell CH. Natural Mentors, Racial Identity, and Educational Attainment Among African American Adolescents: Exploring Pathways to Success. Child Dev. 2012;83(4):1196–1212. doi: 10.1111/j.1467-8624.2012.01769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zimmerman MA, Salem DA, Maton KI. Family structure and psychosocial correlates among urban African-American adolescent males. Child Dev. 1995;66(6):1598–1613. http://www.ncbi.nlm.nih.gov/pubmed/8556888. [PubMed] [Google Scholar]
- 28.Bauermeister JA, Zimmerman M, Xue Y, Gee GC, Caldwell CH. Working, Sex Partner Age Differences, and Sexual Behavior among African American Youth. Arch Sex Behav. 2009;38(5):802–813. doi: 10.1007/s10508-008-9376-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zimmerman MA, Caldwell CH, Bernat DH. Discrepancy between self-report and school-record grade point average: Correlates with psychosocial outcomes among African American adolescents. J Appl Soc Psychol. 2002;32(1):86–109. doi: 10.1111/j.1559-1816.2002.tb01421.x. [DOI] [Google Scholar]
- 30.Nakao K, Treas J. Computing 1989 Occupational Prestige Scores. 1990 Nov Publisher not identified. [Google Scholar]
- 31.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schlenberg JG. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2016. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf. [Google Scholar]
- 32.Derogatis LR, Spencer MS. The Brief Symptom Inventory (BSI): Administration, scoring and procedures manual—1. Baltimore, MD: Johns Hopkins University, School of Medicine, Clinical Psychometrics Research Unit; 1982. [Google Scholar]
- 33.Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol. 1983;11(1):1–24. doi: 10.1007/BF00898416. http://www.ncbi.nlm.nih.gov/pubmed/6837532. [DOI] [PubMed] [Google Scholar]
- 34.Moos R, Moos B. Family environment scale manual: Development, applications, research. Palo Alto, CA: Center for Health Care Evaluation, Department of Veterans Affairs, Stanford Medical Center; 2002. [Google Scholar]
- 35.Doljanac RF, Zimmerman MA. Psychosocial factors and high-risk sexual behavior: race differences among urban adolescents. J Behav Med. 1998;21(5):451–467. doi: 10.1023/a:1018784326191. http://www.ncbi.nlm.nih.gov/pubmed/9836131. [DOI] [PubMed] [Google Scholar]
- 36.Elkington KS, Bauermeister JA, Zimmerman MA. Do Parents and Peers Matter? A Prospective Socio-Ecological Examination of Substance Use and Sexual Risk among African American Youth. Journal of Adolescence. 2011;34:1035–1047. doi: 10.1016/j.adolescence.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brenner AB, Zimmerman MA, Bauermeister JA, Caldwell CH. The physiological expression of living in disadvantaged neighborhoods for youth. J Youth Adolesc. 2013;42(6):792–806. doi: 10.1007/s10964-012-9838-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muthen LK, Muthen B. Mplus: Statistical Analysis with Latent Variables: User’s Guide. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- 39.Little T. Longitudinal Structural Equation Modeling. New York, NY: The Guilford Press; 2013. [Google Scholar]
- 40.Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2(1):302–317. doi: 10.1111/j.1751-9004.2007.00054.x. [DOI] [Google Scholar]
- 41.Li W, Jaroszewski L, Godzik A. Clustering of highly homologous sequences to reduce the size of large protein databases. Bioinformatics. 2001;17(3):282–283. doi: 10.1093/bioinformatics/17.3.282. [DOI] [PubMed] [Google Scholar]
- 42.Muthén B. Latent Variable Analysis: Growth Mixture Modeling and Related Techniques for Longitudinal Data. In: Kaplan D, editor. The SAGE Handbook of Quantitative Methodology for the Social Sciences. Thousand Oaks, CA: SAGE Publications, Inc; 2004. pp. 346–369. [Google Scholar]
- 43.Acock A. Summer Institute on Research Methodology. Corvallis, OR: 2008. Latent growth curve modeling using Mplus. [Google Scholar]
- 44.Tolvanen A. Latent Growth Mixture Modeling: A Simulation Study. Finland: University of Jyväskylä; 2007. https://jyx.jyu.fi/dspace/handle/123456789/22537. Accessed April 6, 2017. [Google Scholar]
- 45.Batchelder AW, Gonzalez JS, Palma A, Schoenbaum E, Lounsbury DW. A social ecological model of syndemic risk affecting women with and at-risk for HIV in impoverished urban communities. Am J Community Psychol. 2015;56(3-4):229–240. doi: 10.1007/s10464-015-9750-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. Pre-Exposure Prophylaxis (PrEP) 2017 Retrieved from https://www.cdc.gov/hiv/risk/prep/index.html on July 19, 2017.
- 47.Sandler I, Ingram A, Wolchik S, Tein J-Y, Winslow E. Long-Term Effects of Parenting-Focused Preventive Interventions to Promote Resilience of Children and Adolescents. Child Dev Perspect. 2015;9(3):164–171. doi: 10.1111/cdep.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maticka Tyndale E, Barnett JP. Peer-led interventions to reduce HIV risk of youth: A review. Eval Program Plann. 2010;33(2):98–112. doi: 10.1016/j.evalprogplan.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 49.Tsai AC, Burns BFO. Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Soc Sci Med. 2015;139:26–35. doi: 10.1016/j.socscimed.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tsai AC, Mendenhall E, Trostle JA, Kawachi I. Co-occurring epidemics, syndemics, and population health. Lancet. 2017;389(10072):978–982. doi: 10.1016/S0140-6736(17)30403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Meyer J, Springer S, Altice F. Substance abuse, violence, and HIV in women: A literature review of the syndemic. J Womens Health. 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]


