ABSTRACT
Pleuroparenchymal fibroelastosis (PPFE) is a rare lung disease. It can be idiopathic or associated with any one of various conditions. To our knowledge, this is the first report of two cases of PPFE in Brazil. Our first patient presented with pleural and subpleural fibrosis in the upper lobes; a spiculated nodule in the left upper lobe; and a mild reticular pattern in the lower lobes. Surgical lung biopsy revealed PPFE in the upper lobes, including the nodule, and unclassified interstitial pneumonia in the left lower lobe. Our second patient had a history of exposure to domestic birds, indicating a risk of hypersensitivity pneumonitis, and presented with advanced lung disease, predominantly in the upper lobes, together with subpleural fibrosis.That patient underwent lung transplantation. In the explant specimen, PPFE and granulomas were identified, suggesting hypersensitivity pneumonitis as an associated cause.
Keywords: Lung diseases, interstitial/diagnosis; Lung diseases, interstitial/etiology; Alveolitis, extrinsic allergic
RESUMO
A fibroelastose pleuroparenquimatosa (FEPP) é uma doença pulmonar rara, podendo ser idiopática ou associada a diversas condições. Pelo que sabemos, este é o primeiro relato de dois casos de FEPP no Brasil. Nosso primeiro paciente apresentava fibrose pleural e subpleural nos lobos superiores, um nódulo espiculado no lobo superior esquerdo e um padrão reticular discreto nos lobos inferiores. A biópsia pulmonar cirúrgica demonstrou FEPP nos lobos superiores, incluindo no nódulo, e pneumonia intersticial não classificada no lobo inferior esquerdo. Nosso segundo paciente tinha história de exposição a aves domésticas, indicando um risco de pneumonite de hipersensibilidade, e doença pulmonar avançada predominando em lobos superiores, com fibrose subpleural. Esse paciente foi submetido a transplante pulmonar. No espécime do explante, FEPP e granulomas foram identificados, sugerindo pneumonite de hipersensibilidade como causa associada.
Descritores: Doenças pulmonares intersticiais/diagnóstico, Doenças pulmonares intersticiais/etiologia, Alveolite alérgica extrínseca
INTRODUCTION
Fibroelastosis is a rare interstitial pneumonia. 1 In Brazil, there have been no published reports of diagnosed cases of fibroelastosis. In the present report, we describe two cases of pleuroparenchymal fibroelastosis (PPFE). We provide a brief review of the literature and point out the findings of interest in the cases described.
CASE 1
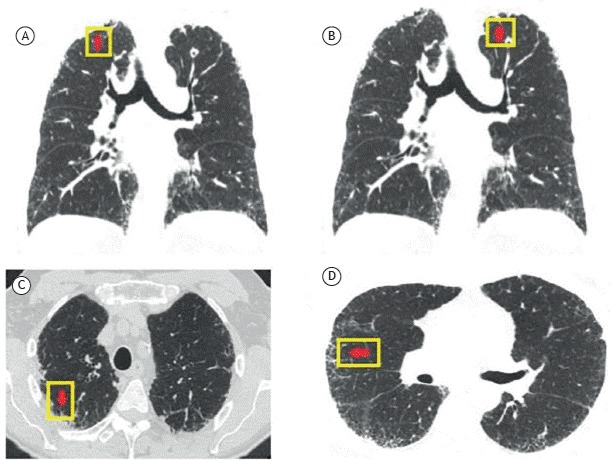
A 67-year-old male patient reported occasional cough and chest X-ray abnormalities detected many years ago. He was an 11-pack-year former smoker and had a history of exposure to mold. The initial tests showed an SpO2 of 95% on room air, fine rales at the left lung base, and squawks on the anterior surface of the left hemithorax. No other changes were observed. Pulmonary function testing revealed an FVC of 4.28 L (87% of predicted); an FEV1 of 3.42 L (92% of predicted); an FEV1/FVC ratio of 0.80; a TLC of 6.34 L (84% of predicted), and a DLCO of 19.0 mL/min/mmHg (54% of predicted). Chest CT scans showed intense pleural and subpleural fibrosis, as well as septal thickening, predominantly located in the upper lobes (Figure 1). There was a spiculated nodule in the left upper lobe and a mild reticular pattern in the lower lobes.
Figure 1. Coronal (A) and axial (B, C, and D) CT scans of the chest showing intense pleural and subpleural fibrosis, as well as septal thickening, predominantly located in the upper lobes and a spiculated nodule in the left upper lobe.
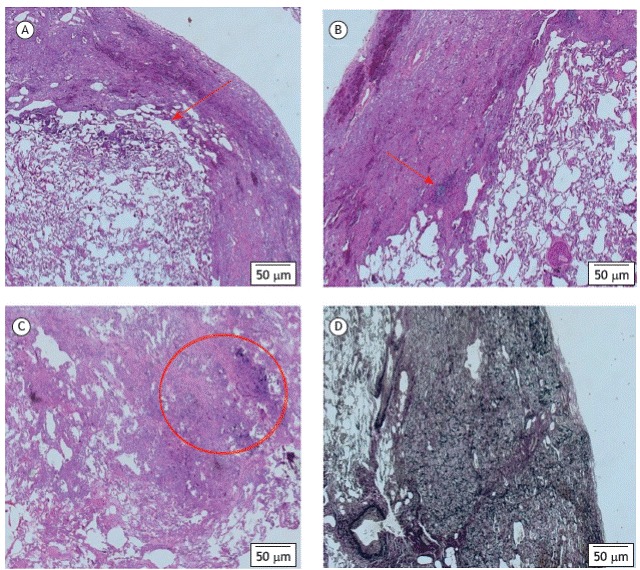
A surgical lung biopsy was performed, with sampling of the left upper and lower lobes. Microscopic examination revealed compact fibrosis with elastosis, with no evidence of malignancy in the resected nodule, as well as clearly delineated areas of pleural/subpleural fibrosis in nonfibrotic parenchyma and little scarce mononuclear cell infiltrate (Figure 2). A biopsy of the lower lobe showed unclassified interstitial fibrosis (image not shown).
Figure 2. Photomicrographs of a surgical lung biopsy specimen from the left upper lobe. In A, clearly delineated areas of pleural/subpleural fibrosis in nonfibrotic parenchyma (arrow; H&E, magnification: ×28). In B, pleural/subpleural fibrosis and scarce mononuclear cell infiltrate (arrow; H&E, magnification: ×28). In C, compact fibrosis with elastosis, with no evidence of malignancy (arrow; H&E, magnification: ×40). In D, an increase in elastic fibers in the areas of pleural fibrosis (arrow; Verhoeff staining for elastic fibers, magnification: ×28).
CASE 2
A 29-year-old male nonsmoker experiencing dyspnea presented with a one-year history of dyspnea on minimal exertion and dry cough. The patient had lost 12 kg in weight during that period. He had a 10-year history of exposure to parakeets and worked cutting plastic. Physical examination revealed emaciation; tachycardia (HR = 130 bpm); and an SpO2 of 79% on room air. Auscultation revealed fine rales bilaterally. Arterial blood gas analysis showed a pH of 7.33; a PaCO2 of 69 mmHg; a PaO2 of 43 mmHg; a bicarbonate level of 36.1 mmol/L; a base excess of 7.7 mmol/L; and an SaO2 of 74.9%. Spirometry showed an FVC of 0.76 L (15% of predicted); an FEV1 of 0.74 L (17% of predicted); and an FEV1/FVC of 0.97. Chest CT showed intense pleural and subpleural fibrosis, as well as septal thickening, predominantly located in the as well as septal thickening, predominantly located in the upper lobes. The diagnosis was chronic hypersensitivity pneumonitis, and lung transplantation was indicated.
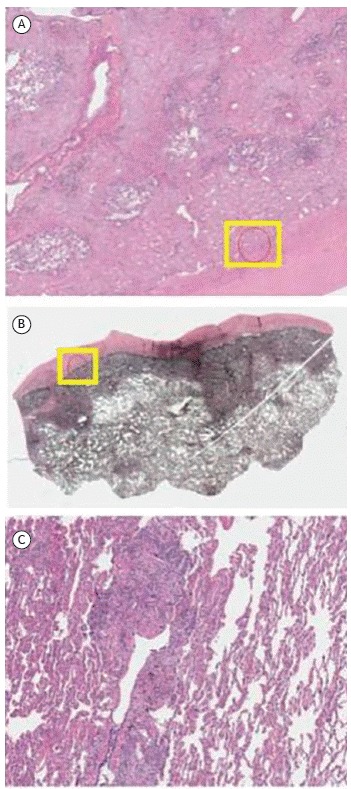
The lung explant histopathological findings are shown in Figure 3.
Figure 3. Upper lobe explant histological findings. In A and B, presence of fibrous thickening of the visceral pleura and subpleural lung parenchyma, with little dense collagen deposition and abundant elastic fibers that are evident on Verhoeff staining. In C, signs of small airways disease, either by obliteration or by distortion of the bronchial wall, accompanied by malformed granulomas and multinucleated giant cells containing cholesterol crystals, located interstitially or intra-alveolarly.
DISCUSSION
PPFE is classified as belonging to the group of rare idiopathic interstitial pneumonias. 1 Approximately 100 cases have been reported. 2
In 1975, Davies et al. reported the cases of 5 patients with pulmonary fibrosis confined to the upper parts of the lungs, similar to the lesions observed in ankylosing spondylitis. 3 In 1992, Amitani et al. reported the cases of 13 patients with fibrosis of unknown etiology, located in the upper lobes. 4 Histopathological examination was performed in nine cases. Various cases were subsequently described in Japan, being reviewed by Kwabata et al. in 2003. 5 In 2004, Frankel et al. reported the cases of 5 patients with upper lobe-predominant fibrosis characterized by intense fibrosis of the visceral pleura and intense subpleural fibrosis, with a mixture of elastic fibers and dense collagen. 6 In that study, the disease was called pulmonary PPFE, a term that has persisted to the present day. 6
Radiologically, PPFE is characterized by pleural and subpleural fibrotic thickening in the upper lobes, with consequent reduction in volume and retraction of the hilum toward the apices. 7 In Brazil, it is likely that many of such cases are diagnosed as tuberculosis cases. Although PPFE was originally considered to be restricted to the upper lobes, it was subsequently shown to be able to involve other lobes, in its initial stage or during its progression, often extending from the upper lobes toward the lower lobes. Reticular opacities in the lower lobes, similar to those seen in nonspecific interstitial pneumonia or with a usual interstitial pneumonia pattern, can be observed. 8
Dyspnea on exertion and dry cough are the major symptoms. Recurrent lower respiratory tract infections and spontaneous pneumothorax can also occur.(8 , 9)
The age distribution is bimodal, with peaks between 21 and 30 years of age and between 51 and 60 years of age. 10 There is no gender predominance. 10
Smoking does not appear to be a risk factor. 2 PPFE can progress slowly or rapidly. Its etiology can be unknown (idiopathic) or be associated with various causes, such as occupational exposures to asbestos and aluminum; bone marrow and/or lung transplantation (the most common cause); history of chemotherapy; history of radiotherapy; autoimmune diseases (such as ankylosing spondylitis and ulcerative colitis); hypersensitivity pneumonitis; and family history of PPFE. 2 , 9 - 13
Physical examination can reveal anteroposterior flattening of the chest (platythorax). 13 Crackles are audible in half of the cases. 8 The usual functional pattern is a restrictive pattern, with decreased DLCO. 7
There is no specific treatment. Patients have been empirically treated with corticosteroids and other immunosuppressants, with no proven evidence of improvement. 2 , 12
The cases reported here have some points of interest. In Case 1, the patient was a former smoker and, in addition to presenting with apical nodular thickening and interlobular septal thickening, he presented with a spiculated nodule in the left upper lobe. The nodule was hypermetabolic on positron emission tomography.
Histological analysis of the resected specimen revealed that the nodule represented a focus of fibroelastosis. A similar case was reported in 2011. 14 Recently, three cases of lung cancer (non-small cell carcinoma) superimposed on fibroelastosis have been described. 15 Fibrosis centered on small airways and bronchiolitis obliterans have been described, 16 , 17 and that explains the squawks heard on auscultation in Case 1.
Case 2 is an example of secondary fibroelastosis. In that case, fibroelastosis was secondary to hypersensitivity, which was confirmed by the finding of granulomas in the lung explant, in addition to the classic findings suggestive of fibroelastosis. Cases with concomitant findings of hypersensitivity pneumonitis have been described. 2 , 16 Lung transplantation in occasional cases of PPFE has been reported. 18
Financial support: None.
Study carried out at the Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) Brasil.
REFERENCES
- 1.Travis WD, Costabel U, Hansell DM, King TE, Jr, Lynch DA, Nicholson AG. An official American Thoracic Society/European Respiratory Society statement Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188(6):733–748. doi: 10.1164/rccm.201308-1483ST. http://dx.doi.org/10.1164/rccm.201308-1483ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Portillo K, Guasch Arriaga I, Ruiz-Manzano J. Pleuroparenchymal fibroelastosis is it also an idiopathic entity? Arch Bronconeumol. 2015;51(10):509–514. doi: 10.1016/j.arbres.2015.05.002. http://dx.doi.org/10.1016/j.arbres.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 3.Davies D, Crowther JS, MacFarlane A. Idiopathic progressive pulmonary fibrosis. Thorax. 1975;30(3):316–325. doi: 10.1136/thx.30.3.316. http://dx.doi.org/10.1136/thx.30.3.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amitani R, Niimi A, Kuze F. Idiopathic pulmonary upper lobe fibrosis. Kokyu. 1992;11:693–699. [Google Scholar]
- 5.Kawabata Y, Matsuoka R. Pathology of idiopathic pulmonary upper lobe fibrosis. Nihon Kyobu Rinsho. 2003;62:S161–S202. [Google Scholar]
- 6.Frankel SK, Cool CD, Lynch DA, Brown KK. Idiopathic pleuroparenchymal fibroelastosis Description of a novel clinicopathologic entity. Chest. 2004;126(6):2007–2013. doi: 10.1378/chest.126.6.2007. http://dx.doi.org/10.1378/chest.126.6.2007 [DOI] [PubMed] [Google Scholar]
- 7.Watanabe K. Pleuroparenchymal fibroelastosis its clinical characteristics. Curr Respir Med Rev. 2013;9:299–237. doi: 10.2174/1573398X0904140129125307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oda T, Ogura T, Kitamura H, Hagiwara E, Baba T, Enomoto Y. Distinct characteristics of pleuroparenchymal fibroelastosis with usual interstitial pneumonia compared with idiopathic pulmonary fibrosis. Chest. 2014;146(5):1248–1255. doi: 10.1378/chest.13-2866. http://dx.doi.org/10.1378/chest.13-2866 [DOI] [PubMed] [Google Scholar]
- 9.Cuppens K, Verbeken E, Coolen J, Verschakelen J, Wuyts W. Idiopathic pleuroparenchymatous fibroelastosis A case report and brief review of the literature. Respir Med Case Rep. 2014;12:7–9. doi: 10.1016/j.rmcr.2013.12.005. http://dx.doi.org/10.1016/j.rmcr.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von der Thüsen JH, Hansell DM, Tominaga M, Veys PA, Ashworth MT, Owens CM. Pleuroparenchymal fibroelastosis in patients with pulmonary disease secondary to bone marrow transplantation. Mod Pathol. 2011;24(12):1633–1639. doi: 10.1038/modpathol.2011.114. http://dx.doi.org/10.1038/modpathol.2011.114 [DOI] [PubMed] [Google Scholar]
- 11.Beynat-Mouterde C, Beltramo G, Lezmi G, Pernet D, Camus C, Fanton A. Pleuroparenchymal fibroelastosis as a late complication of chemotherapy agents. Eur Respir J. 2014;44(2):523–527. doi: 10.1183/09031936.00214713. http://dx.doi.org/10.1183/09031936.00214713 [DOI] [PubMed] [Google Scholar]
- 12.Nakatani T, Arai T, Kitaichi M, Akira M, Tachibana K, Sugimoto C. Pleuroparenchymal fibroelastosis from a consecutive database a rare disease entity? Eur Respir J. 2015;45(4):1183–1186. doi: 10.1183/09031936.00214714. http://dx.doi.org/10.1183/09031936.00214714 [DOI] [PubMed] [Google Scholar]
- 13.Camus P, von der Thüsen J, Hansell DM, Colby TV. Pleuroparenchymal fibroelastosis one more walk on the wild side of drugs? Eur Respir J. 2014;44(2):289–296. doi: 10.1183/09031936.00088414. http://dx.doi.org/10.1183/09031936.00088414 [DOI] [PubMed] [Google Scholar]
- 14.Machuca JS, Niazi M, Diaz-Fuentes G. Pleuroparenchymal fibroelastosis presenting as a hypermetabolic lung nodule. J Bronchology Interv Pulmonol. 2011;18(1):65–68. doi: 10.1097/LBR.0b013e318207b396. http://dx.doi.org/10.1097/LBR.0b013e318207b396 [DOI] [PubMed] [Google Scholar]
- 15.Baroke E, Heussel CP, Warth A, Eichinger M, Oltmanns U, Palmowski K. Pleuroparenchymal fibroelastosis in association with carcinomas. Respirology. 2016;21(1):191–194. doi: 10.1111/resp.12654. http://dx.doi.org/10.1111/resp.12654 [DOI] [PubMed] [Google Scholar]
- 16.Reddy TL, Tominaga M, Hansell DM, von der Thusen J, Rassl D, Parfrey H. Pleuroparenchymal fibroelastosis a spectrum of histopathological and imaging phenotypes. Eur Respir J. 2012;40(2):377–385. doi: 10.1183/09031936.00165111. http://dx.doi.org/10.1183/09031936.00165111 [DOI] [PubMed] [Google Scholar]
- 17.Hirota T, Fujita M, Matsumoto T, Higuchi T, Shiraishi T, Minami M, Okumura M. Pleuroparenchymal fibroelastosis as a manifestation of chronic lung rejection. Eur Respir J. 2013;41(1):243–245. doi: 10.1183/09031936.00103912. http://dx.doi.org/10.1183/09031936.00103912 [DOI] [PubMed] [Google Scholar]
- 18.Chen F, Matsubara K, Miyagawa-Hayashino A, Tada K, Handa T, Yamada T. Lung transplantation for pleuroparenchymal fibroelastosis after chemotherapy. Ann Thorac Surg. 2014;98(5):e115–e117. doi: 10.1016/j.athoracsur.2014.07.045. http://dx.doi.org/10.1016/j.athoracsur.2014.07.045 [DOI] [PubMed] [Google Scholar]


