Abstract
A 40-year-old female dental technician visited our hospital for the investigation of a chest X-ray abnormality. Chest computed tomography demonstrated centrilobular nodules and lung volume reduction, and her serum KL-6 level was elevated. A histological analysis of the specimens obtained on a surgical lung biopsy showed peribronchiolar fibrosis with pigmented macrophages and cholesterol clefts. An energy-dispersive X-ray analysis showed that these lung tissues contained some metals, including indium. The serum indium level was also elevated. We diagnosed this patient with pneumoconiosis caused by exposure to sandblasting certain dental metals. This is the first reported case of pneumoconiosis in a dental technician associated with exposure to indium.
Keywords: dental technician, pneumoconiosis, indium
Introduction
Pneumoconiosis is a fibrotic pulmonary disease caused by the accumulation of inhaled particles in the lungs. It is an important occupational disease because it leads to chronic respiratory failure with a high risk of complicating tuberculosis and lung cancer (1). Dental technicians are exposed to various airborne particles because their work includes the sandblasting of dental metals. Therefore, their working conditions carry a risk of pneumoconiosis (2-14). Indium is a rare element included in indium-tin oxide (ITO), a material in flat-panel displays or plasma display panels for television screens, and has been reported as a risk factor for occupational lung disease (15-19). We herein report for the first time a case of pneumoconiosis in a dental technician associated with exposure to dental metals including indium.
Case Report
A 40-year-old woman visited our hospital in October 2015 because of an abnormality on a chest X-ray film taken during a health checkup. She had no symptoms, such as coughing or shortness of breath. She had never smoked and had no history of respiratory disease. She had worked as a dental technician since 20 years of age and had been engaged in the sandblasting of dental metals for 20 years. She had no occupational history of exposure except as a dental technician.
Her vital signs on admission were as follows: respiratory rate, 20/min; heart rate, 84/min; blood pressure, 91/50 mmHg; and body temperature, 36.3°C. A physical examination and blood hematology gave normal results. She had no fine crackles or clubbed fingers. Hematology and laboratory examinations revealed elevation of the erythrocyte sedimentation rate (ESR 40 mm/h) and the serum levels of lactate dehydrogenase (LDH 302 IU/L) and KL-6 (1,797 IU/mL) as biomarkers of interstitial lung disease (ILD). Diagnostic biomarkers of connective tissue diseases, such as rheumatoid factor and antinuclear antibody, were negative. An arterial blood gas analysis indicated no abnormalities, such as hypoxemia or hypercapnia (PaO2 95.4 Torr, PaCO2 38.4 Torr). Chest X-ray and high-resolution computed tomography (HRCT) demonstrated parenchymal linear lesions, centrilobular nodules, subpleural fibrosis, and lung volume reduction, predominantly in both upper lobes (Fig. 1). Pulmonary function tests demonstrated restrictive ventilatory impairment (forced vital capacity 67.9% of that predicted, total lung capacity 68.0% of that predicted, forced expiratory volume 1.0% 86.7%, residual volume 128% of that predicted). A six-minute walking test yielded a distance of 519.2 m and a minimum SpO2 of 95%. No bacterial or fast-acid bacillus bodies or atypical cells were found in bronchoalveolar lavage fluid. Transbronchial lung biopsy specimens showed only non-specific inflammation of the alveolar septa. The differential diagnosis included pneumoconiosis, chronic hypersensitivity pneumonia, and pleuroparenchymal fibroelastosis (PPFE).
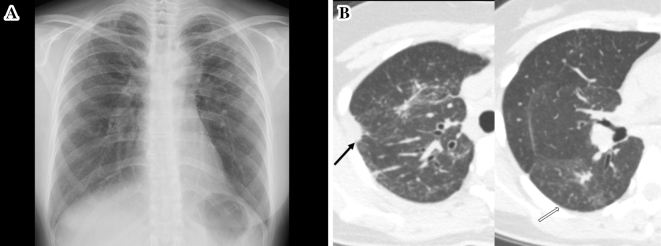
Figure 1.
Chest X-ray film (A) showing parenchymal linear lesions and lung volume reduction predominantly in both upper lobes. Chest high-resolution computed tomography images (B) showing subpleural pulmonary opacity (black arrow) in the right upper lobe and centrilobular nodules (white arrow), parenchymal linear lesions, and ground-glass attenuation predominantly in both upper lobes.
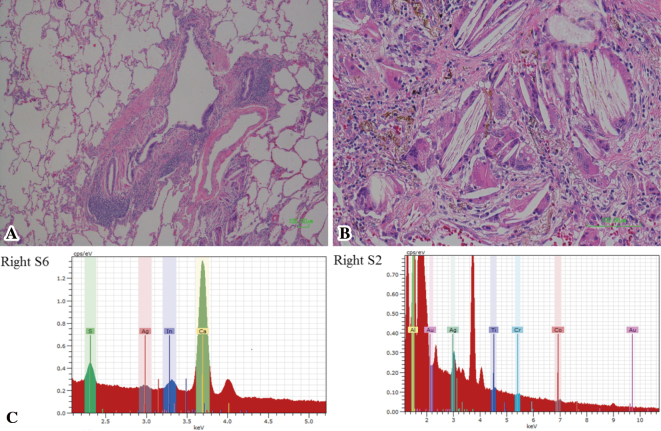
We performed a surgical lung biopsy using video-assisted thoracoscopy to establish a diagnosis. A histological examination revealed patchy and peribronchiolar fibrosis and fibroelastosis with pigmented macrophages and marked foreign body granuloma with cholesterol clefts in both the alveolar spaces and interstitium in specimens from the right S2 and S6 segments (Fig. 2A, B). The peribronchiolar distribution of fibroelastosis was inconsistent with the histological pattern of PPFE. These findings were consistent with pneumoconiosis, particularly indium-associated lung disease. A microanalysis using an energy-dispersive X-ray analytical spectrometer (TM3000+Quantax70; HITACHI, Tokyo, Japan) showed that the affected lung tissues contained metallic particles, such as aluminum (Al), silver (Ag), titanium (Ti), cobalt (Co), nickel (Ni), chromium (Cr), and indium (In) (Fig. 2C). An inductively coupled plasma mass spectrometry analysis showed a high serum indium level at 34 μg/L (cut-off level 0.1 μg/L). Therefore, we diagnosed this patient as having dental technicians' pneumoconiosis caused by exposure to dental metals. We classified the case as 1/2 of the PR classification of pneumoconiosis. We advised her to use a protective face mask to avoid regular dust exposure at her job and requested that the person responsible in her workplace improve the environment of the dental laboratory. The patient's disease activity is now being monitored by periodic examinations in our hospital, and she is currently stable.
Figure 2.
Histological findings in the specimen obtained by a surgical lung biopsy. Hematoxylin and Eosin staining showing patchy peribronchiolar fibrosis and fibroelastosis with pigmented macrophages and marked foreign body granuloma with cholesterol clefts in both the alveolar spaces and interstitium (A, B: right S6). A microanalysis using an energy-dispersive X-ray analytical spectrometer revealed peaks for several metallic elements used in dental devices (C).
Discussion
It has been reported that the prevalence of pneumoconiosis among dental technicians is 4.5-23.6% after a mean exposure duration of 12.8-28.4 years (2-14). Ergün et al. suggested that exposure to sandblasting is a major risk factor that carries a 77-fold-increased risk of pneumoconiosis (2). Patients with pneumoconiosis have micronodular and reticular lesions predominantly in both upper lobes of the lung and restrictive and/or obstructive pulmonary function impairment (2). Previous studies have shown that dental technicians have more respiratory symptoms and lower pulmonary function than controls in other lines of work (3,6-9). Employment duration is positively correlated with the extent of radiological abnormalities and negatively correlated with the pulmonary function (3,10-12). In addition, Dogan et al. reported that the prevalence of pneumoconiosis among 36 dental technicians increased from 13.8% to 47% and that the radiologic findings and pulmonary function worsened significantly during 7 years of continuous work in the same place (13). These results suggest that exposure to dental metals is an obvious risk factor for the development of pneumoconiosis in dental technicians. Preventive measures against exposure to dental metals may be insufficient. Choudat et al. investigated 105 self-employed dental technicians living in Paris and found that they often worked alone (43.7%) or in small laboratories without adequate dust control (3). Seldén et al. suggested that local exhaust ventilation might reduce the risk of exposure to dental metals (14). Various measures are therefore needed to protect the health and hygiene of dental technicians.
Previous reports have suggested that the substances that cause pneumoconiosis include silica, nickel-chromium, asbestos, beryllium, cobalt, and other components of dental metals (2). We described the first case of dental technicians' pneumoconiosis caused by exposure to indium in the present case report. Several cases of lung disease have been reported in plant workers exposed to indium (15-19). Cummings et al. reported 10 clinical cases of lung disease in indium workers (15). Histologically, indium lung disease is characterized by peribronchiolar fibrosis with the accumulation of macrophages and numerous cholesterol clefts (16). The present case also showed histological findings similar to those associated with indium lung disease. Some cases of pneumoconiosis might have been diagnosed as indium lung disease. Nogami et al. reported that the serum level of KL-6 as a biomarker of ILD was elevated in patients with indium lung disease and was correlated with the serum indium level (19). The histological findings in the lung and elevation of the KL-6 serum level in the present case were compatible with indium lung disease. The clinical course of indium lung disease is progressive (15,17). Cummings et al. reported that 2 of their 10 cases were fatal (15). The present case report is important because it draws attention to the possible development of progressive indium lung disease in dental technicians.
Recent improvements in dental medical technology and increases in the demand for dental materials will make it more important to adopt protective measures against dust exposure in dental technicians.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Pelucchi C, Pira E, Piolatto G, Coggiola M, Carta P, La Vecchia C. Occupational silica exposure and lung cancer risk: a review of epidemiological studies 1996-2005. Ann Oncol 17: 1039-1050, 2006. [DOI] [PubMed] [Google Scholar]
- 2.Ergün D, Ergün R, Ozdemir C, Oziş TN, Yilmaz H, Akkurt I. Pneumoconiosis and respiratory problems in dental laboratory technicians: analysis of 893 dental technicians. Int J Occup Med Environ Health 27: 785-796, 2014. [DOI] [PubMed] [Google Scholar]
- 3.Choudat D, Triem S, Weill B, Vicrey C, Ameille J, Brochard P, Letourneux M, Rossignol C. Respiratory symptoms, lung function, and pneumoconiosis among self employed dental technicians. Br J Ind Med 50: 443-449, 1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Vuyst P, Vande Weyer R, De Coster A, et al. . Dental technician's pneumoconiosis. A report of two cases. Am Rev Respir Dis 133: 316-320, 1986. [DOI] [PubMed] [Google Scholar]
- 5.Cimrin A, Komus N, Karaman C, Tertemiz KC. Pneumoconiosis and work-related health complaints in Turkish dental laboratory workers. Tuberk Toraks 57: 282-288, 2009. [PubMed] [Google Scholar]
- 6.Froudarakis ME, Voloudaki A, Bouros D, Drakonakis G, Hatzakis K, Siafakas NM. Pneumoconiosis among Cretan dental technicians. Respiration 66: 338-342, 1999. [DOI] [PubMed] [Google Scholar]
- 7.Rom WN, Lockey JE, Lee JS, et al. . Pneumoconiosis and exposure of dental laboratory technicians. Am J Public Health 74: 1252-1257, 1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doğan DÖ, Ozdemir AK, Polat NT, Dal U, Gümüş C, Akkurt I. Prevalence of respiratory abnormalities and pneumoconiosis in dental laboratory technicians. Tuberk Toraks 58: 135-141, 2010. [PubMed] [Google Scholar]
- 9.Sherson D, Maltbaek N, Olsen O. Small opacities among dental laboratory technicians in Copenhagen. Br J Ind Med 45: 320-324, 1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radi S, Dalphin JC, Manzoni P, Pernet D, Leboube MP, Viel JF. Respiratory morbidity in a population of French dental technicians. Occup Environ Med 59: 398-404, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berk S, Dogan DO, Gumus C, Akkurt I. Relationship between radiological (X-ray/HRCT), spirometric and clinical findings in dental technicians' pneumoconiosis. Clin Respir J 10: 67-73, 2016. [DOI] [PubMed] [Google Scholar]
- 12.Kahraman H, Koksal N, Cinkara M, Ozkan F, Sucakli MH, Ekerbicer H. Pneumoconiosis in dental technicians: HRCT and pulmonary function findings. Occup Med (Lond) 64: 442-447, 2014. [DOI] [PubMed] [Google Scholar]
- 13.Dogan DÖ, Berk S, Gumus C, Ozdemır AK, Akkurt I. A longitudinal study on lung disease in dental technicians: what has changed after seven years? Int J Occup Med Environ Health 26: 693-701, 2013. [DOI] [PubMed] [Google Scholar]
- 14.Seldén AI, Persson B, Bornberger-Dankvardt S, Winström LE, Bodin LS. Exposure to cobalt chromium dust and lung disorders in dental technicians. Thorax 50: 769-772, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cummings KJ, Nakano M, Omae K, et al. . Indium lung disease. Chest 141: 1512-1521, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Homma S, Miyamoto A, Sakamoto S, Kishi K, Motoi N, Yoshimura K. Pulmonary fibrosis in an individual occupationally exposed to inhaled indium-tin oxide. Eur Respir J 25: 200-204, 2005. [DOI] [PubMed] [Google Scholar]
- 17.Homma T, Ueno T, Sekizawa K, Tanaka A, Hirata M. Interstitial pneumonia developed in a worker dealing with particles containing indium-tin-oxide. J Occup Health 45: 137-139, 2003. [DOI] [PubMed] [Google Scholar]
- 18.Chonan T, Taguchi O, Omae K. Interstitial pulmonary disorders in indium-processing workers. Eur Respir J 29: 317-324, 2007. [DOI] [PubMed] [Google Scholar]
- 19.Nogami H, Shimoda T, Shoji S, Nishima S. Pulmonary disorders in indium-processing workers. Nihon Kokyuki Gakkai Zasshi (J Jpn Respir Soc) 46: 60-64, 2008. (in Japanese, Abstract in English). [PubMed] [Google Scholar]