Abstract
The science of mental life is critical for understanding both how we function, and impairments in our functioning. However, understanding the causal mechanisms underlying mental health disorders and developing new treatments are challenges too great to be solved by any individual approach. There is a growing awareness that translational research—from laboratory to patient and back again to animal models—will be critical for the improved understanding and treatment of mental health disorders. The motivation and intention to pursue translational approaches is therefore strong in mental health research, but critically, opportunities for interaction between basic scientists and clinicians are relatively limited, and vary depending on the institution in which researchers are working. This has promoted the development of a ‘culture gap’ between basic and clinical scientists that limits interaction and sharing of knowledge. Here, we provide 14 examples of contemporary translational research and call for an increased collaborative approach to mental health research that spans clinical diagnoses, levels of analysis and bridges between basic to clinical mental health sciences, including, but not limited to, psychology and neuroscience. What is needed is an inclusive and integrated approach, bringing together scientists working at all levels of enquiry with clinicians providing insights on what works (and what does not). To stimulate the much-needed innovation in therapeutic techniques, an analysis of component parts is critical. Our approach suggests simplifying complex behaviours into distinct psychological components. Asking collaboratively driven scientific questions about dysfunction will also benefit our fundamental understanding of mental life.
This article is part of a discussion meeting issue ‘Of mice and mental health: facilitating dialogue between basic and clinical neuroscientists'.
Keywords: mental health science, translation, backtranslation, psychological treatment, pharmacological treatment
1. Introduction
Coming together is a beginning; keeping together is progress; working together is success.
—Henry Ford
In putting together the meeting, ‘Of Mice and Mental Health: Facilitating Dialogue between Basic and Clinical Neuroscientists' at the Royal Society, we aimed not only to showcase how different approaches can be transformative in understanding and treating mental health disorders, but also to highlight areas where more discussion would produce fruitful research in both basic and clinical disciplines. The 14 papers presented in this issue by contributors to the meeting provide reviews, perspectives and primary data showing the power of transdiagnostic, translational and backtranslational approaches to understanding mental health. Dame Professor Uta Frith has graciously put them into a wider historical and scientific context in her preface to this special issue. The interdisciplinary meeting included researchers who range from basic scientists to clinicians—yet who brought together their different methods to a shared goal. The common approach is to understand and improve treatments for mental health disorders via mental health science.
Why encourage clinicians and scientists of various disciplines to work together to better understand and improve mental health treatments? Mental health disorders now account for more than 15% of the disease burden in developed countries, more than all forms of cancer. Even our best mental health treatments demand improvement—for example to increase the proportion of patients who achieve a clinically meaningful reduction in symptoms or full remission [1]. Mental health science has an important role to play in improving treatments of all types, whether psychological, pharmacological or their combination [2,3].
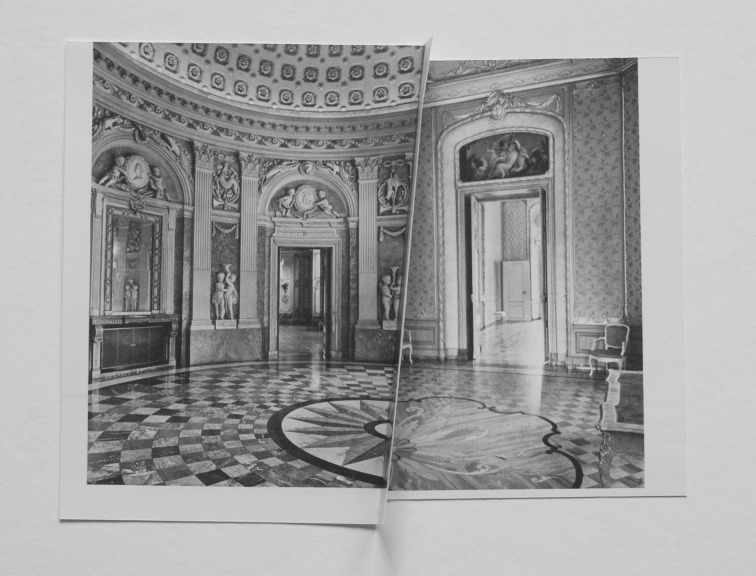
Basic and clinical scientists pioneering research into mental health disorders have much to learn from each other, but critically, opportunities for interaction are limited and vary depending on the institution in which researchers are working. A culture gap means both sides are often unaware of what the other is doing, which limits interaction and sharing of knowledge. An aim of this meeting, ‘Of Mice and Mental Health’, was to facilitate dialogue—ultimately to aid in the development of translational models for mental health. As illustrated on the cover of this special issue and in figure 1 below, there is a need for our salons of discussion to more closely intersect.
Figure 1.
Abigail Reynolds ‘Mirror (Benrath)’. Image courtesy of the artist. Reproduced with permission from the artist.
Our hope is that asking collaboratively driven scientific questions about dysfunction will also benefit our fundamental understanding of the fascinating science of mental life. As scientists, we explore the biological and physical sciences, from the planet Earth and animals, to space and numbers—psychology is still a relatively young science and we have an expanse of knowledge to be gained about the functioning of our own minds. Psychology has had a long tradition of understanding mental life through studies of dysfunction and function, and of studying both human and non-human animals. The papers in this issue explore both.
We start with an elegant example of how behavioural work with non-human animals has led to one of the most efficacious treatments we have to date for anxiety disorders. Anxiety disorders comprise a group of mental health disorders including specific phobias and panic disorder. They are typically characterized by intense emotional states of anxiety (about future events) or fear (about current events) and associated psychophysiological responses (e.g. increased heart rate) which together impair an individual's functioning [4]. Craske et al. [5] review how discoveries in fundamental animal learning theory led to major advances in the treatment of anxiety disorders in the middle part of the twentieth century. This close relationship between the basic study of pavlovian extinction learning and the development of cue exposure therapy has continued over an extended period of time, with progressive refinements—with many examples by Craske herself—enhancing and optimizing the efficacy of treatment for anxiety disorders based on fundamental learning principles. Cue exposure therapy can be considered as an outstanding example of the fruitfulness of translating animal behavioural research for human patients. Psychological treatments incorporating variations of exposure therapy have a strong clinical evidence base for patients. This success is the result of clinical and basic scientists in close communication—taking observations concerning clinical need, testing, and refining procedures to improve anxiety within this theoretical framework and by using experimental models, while applying results to benefit patients.
This translation should not be one way, however. It is also critically important to backtranslate clinical findings into animal models to ensure that, when basic scientists claim that they are studying a phenomenon of clinical relevance, they really are answering the right question. As described by Monfils and colleagues [6], although pavlovian fear conditioning in rats has been a very useful model of some aspects of anxiety disorders in humans, what has tended to be measured in animal studies is a reduction in fear produced by particular interventions. However, the clinically relevant behavioural outcome in patients is not necessarily any reduction in fear; rather, clinicians would consider a treatment successful when a patient is functionally healthy—i.e. they behave no differently to individuals without the disorder. These are subtly different, but important, criteria for recovery. What Monfils and colleagues elegantly provide here is an example of how a more clinically oriented approach can be applied to basic behavioural data, to allow ‘remission’ from conditioned fear to be identified in animals and also to account for individual differences in treatment response. This illustrates how even highly successful animal models can benefit from a reappraisal of assumptions—ensuring that we are asking the right questions—on a regular basis.
Another area in which there has been productive dialogue between basic and clinical mental health researchers has been in the fields of memory consolidation and reconsolidation. Since its rediscovery in 2000 [7], reconsolidation—the process by which memories become destabilized under certain conditions of retrieval, and require the recruitment of specific neurochemical and molecular ‘restabilization’ mechanisms in order to persist in the brain—has been promoted by basic researchers as a potential target for treating mental health disorders, including post-traumatic stress disorder (PTSD) and drug addiction. While the phenomenon holds promise—and has been used to inform small-scale, experimental medicine studies with both patients with PTSD [8] and patients with substance use disorder (addiction) [9]—there are inevitably challenges and subtleties in translating rodent research to the clinic. One challenge is that some aspects of mental health disorders—such as the experience of involuntary intrusive memories of a traumatic experience, or ‘flashbacks’ in post-traumatic stress—may not be readily amenable to study in rodents. However, as described by Visser et al. [10], inspiration from the basic literature does not always need to rely on directly analogous processes in the form of trauma memory expression, and it is possible to develop procedures for humans based on fundamental psychological principles taken from both rodents and humans, i.e. to use theory-driven innovations in treatment. For example, informed in part by memory reconsolidation work in animals, a behavioural method (task interference after a memory reactivation task) was derived to reduce the frequency of intrusive memories of experimental trauma in humans [11]. A second example, informed in part by memory consolidation theory, uses an earlier time window during which memory is assumed to be malleable. Here, a behavioural method (computer task after a reminder cue) was tested with patients after a real trauma in a hospital [12,13] within the first few hours after trauma. Both lines of enquiry are as yet early and further work is needed.
In such ways, combining ideas from rodent behavioural neuroscience and cognitive psychology, it is possible to design new interventions for use in humans that are yet to be backtranslated into animals. However, even when the same psychological process is targeted in animals and humans—for example, a pavlovian fear memory—the translation of this from healthy human populations to the clinic presents its own challenges, as described by Kindt [14]. Even though she has seen remarkable treatment outcomes from applying reconsolidation-based therapies to patients with anxiety disorders (see ref. [15] for her groundbreaking work on phobia), she relates the challenges that are associated with getting old, pathological memories to reconsolidate in the clinic. Combining insights from the basic literature with clinical experience allows some of these challenges to be overcome; and for those aspects of treatment that are still problematic, careful backtranslation into animals should allow more parametric studies to be conducted, revealing the methods that would be most promising in clinical practice and helping to delineate precise mechanisms underlying effects.
The importance of psychological principles, translation and backtranslation is also relevant to the more fundamental understanding of memory. As discussed by Albo & Gräff [16], the study of memory has been heavily influenced by research with patients—most notably, a patient called Henry Molaison (known by his initials, HM, until his death in 2008) who was diagnosed with amnesia after medial temporal lobe damage. This work, conducted over decades by Brenda Milner, Suzanne Corkin and colleagues, has led to the development of our key psychological theories regarding the nature of remote memory. Albo & Gräff describe how these patient-derived observations can be complemented by cutting-edge molecular neuroscience techniques to provide further levels of insight into the nature of remote memory. This fundamental, basic research informs new understanding of long-term memory, regardless of any potential clinical impact, emphasizing the importance of translation and backtranslation even if there are no immediately obvious therapeutic implications (though, of course, it may lead to benefit ultimately). Basic research without doubt has its own value, independent of clinical impact. However, at the same time, it may be that advances in basic understanding one day provide new avenues for clinical research. Familiarity and reference to both the basic and clinical literature should not be limited to those who feel that they are conducting ‘translational’ research. Psychology and neuroscience remain relatively young fields in the greater scheme of science, and we need the best research at all levels. Psychology—the science of mental life—has benefited from a long tradition of understanding function through dysfunction. Thus, basic science-informed questions can benefit from an improved dialogue with clinical scientists. And, clinical questions benefit from understanding more fundamental issues. Translation per se does not have to involve only a middle zone—pioneering translation of the future may well benefit from input from both extremes of clinical to basic perspectives.
The importance of understanding psychological processes and of developing analogue behavioural tasks to model mental disorders is a key message from the review from Everitt et al. [17]. Substance abuse disorder [4], or drug addiction, is the result of a number of dysfunctional psychological processes, some of which predate drug use and others which are the result of drug toxicity. While it is possible to encapsulate many of these within a single behavioural model—for example, the ‘3-criteria’ or ‘resistance to punishment’ models [18,19]—insights into fundamental changes in psychological processing often do not require these ‘full’ models of drug addiction. One of the key values of animal models lies in their simplification of complex phenomena into underlying components that can be more readily understood [20]. This is not necessarily the limitation that it might at first seem: ‘deconstruction’ of complex behaviour can subsequently be reconstructed into more translationally relevant models, as required. Everitt et al. [17] discuss the ways in which animal models of specific psychological dysfunction in drug addiction have led to better understanding of the neural circuitry underlying the disorder (through causal manipulations that are simply not possible in humans) and to the identification of potential avenues for treatment.
This close attention to translation of psychological processes is mirrored by the focus on backtranslation in the work of Goldstein and colleagues [21]. Focusing on different but complementary aspects of dysfunctional psychological processing in drug addiction—those of response inhibition and salience attribution—they highlight the conservation of dysfunction in the thalamic circuitry in addicted patients and animal models of the disorder, providing future directions for human and animal translational research.
A core psychological dysfunction in addiction—compulsive behaviour—is also seen in other mental health disorders, such as compulsive eating, and obsessive–compulsive disorder (OCD). As reviewed by Cottone and colleagues [22], there is significant overlap in the neuropharmacological mechanisms underlying drug addiction and compulsive eating, indicating the potential therapeutic value of studying underlying psychological processes that may be transdiagnostic across disorders. Although the concept of ‘food addiction’ is controversial, there may be pharmacological, psychological or combined treatments that can be administered to patients whether their maladaptive consumption is of drugs or food. This transdiagnostic approach is also supported by the work of Ahmari and colleagues [23], in which they demonstrate that an animal analogue of compulsive grooming in OCD, the SAPAP3 knockout mouse (in which the gene for the post-synaptic density protein SAPAP3, strongly expressed in excitatory synapses of the striatum, is not functional) shows monoaminergic changes in the post-mortem brain that are analogous to those observed in OCD patients. In addition to providing insights into the mechanisms by which monoaminergic medications work both in patients and the model, this neurochemical research indicates the complex interplay of different neurobiological circuits supporting psychological processes. Ahmari and colleagues conclude by providing future directions for animal research, taking advantage of circuit-selective, neuronal-selective and temporally specific optogenetic technology to map the neurobiological underpinnings of compulsive behaviour.
Some readers may be sceptical of the utility of animal models for disorders in which subjective states are a key diagnostic criterion. Indeed, it is true that animals may be induced to seek and take drugs compulsively through the profound chemical effects that these substances inflict on the nervous system, but is it really possible to model mood states such as anhedonia and dysphoria in non-human animals? Perhaps, our ‘models’ of disorders like major depressive disorder (MDD) are limited to those with predictive validity for the effects of antidepressants, such as the forced swim test? The elegant translational research and theorizing of Robinson and colleagues [24] should reassure the sceptical reader. By examining the effect of more subjective processes on psychological functioning that can be readily assessed in animals—such as memory and decision-making—they have produced validated behavioural tasks that model psychological dysfunction in mood disorders like MDD. Furthermore, in doing so they have highlighted how MDD develops from a set of conserved neuropsychological processes that become dysfunctional, despite the numerous biological causes that contribute to the disorder.
The value of this approach is clear from the research reported by Harmer and colleagues [25], who demonstrate that the use of a translational probabilistic response bias task within a wider test battery, assessing other emotional and cognitive deficits in patients with MDD, can reveal subtle deficits in reward processing that appear to be orthogonal to other dysfunctional psychological processes. Furthermore, they use this more selective psychological assessment to reveal an intriguing time course of the antidepressant action of bupropion, providing valuable information for subsequent clinical trials of this drug.
The challenges of translational research are perhaps most striking when considering disorders such as schizophrenia, where it seems difficult—though perhaps not impossible—to imagine how the aberrant psychological processing that gives rise to hallucinations and delusions could be modelled in non-human animals. This question is tackled directly by Canetta & Kellendonk [26], who assert that the historical limitations of animal models of mental health disorders in providing treatment leads have arisen because of a focus on developing models with face validity of behavioural symptoms, rather than models with construct validity of the underlying neurobiological differences contributing to altered psychological processing. By modelling potential causes of schizophrenia—genetic and environmental, including early-life experiences—and measuring specific psychological processes, such as working memory, that have been shown to be impaired in patients with schizophrenia using translational tasks, it is possible to use the array of circuit-mapping and causal manipulations in rodents to provide insights into the clinical condition. St Clair & Johnstone [27] review the advantages of taking this modelling further, to the level of stem cells and brain organoids, to identify potential treatments for schizophrenia and autism at the pharmacological and molecular levels.
The potential impact of translational research is transformative, but the challenges facing it are far from trivial, argues Hyman [28]. Mental health disorders are inarguably complex and heterogeneous. Hyman takes a genetic perspective, arguing that many different genes contribute in a small way to the development of abnormal psychological function. It is possible to model specific genetic variants in mutant mice but, as noted by Hyman, the use of models to simplify disorders may also limit their generalizability. He argues for a map, by which multiple genetic variants might be associated with the risk of a specific mental health disorder in large human populations, and models generated that allow for the combinatorial effects of these genes to be assessed. He is sceptical that this will be in mouse models, instead favouring a ‘brain organoid’ approach.
We agree with Hyman's assertion that mental health disorders are complex and heterogeneous, and that individual animal models should not be ‘reified’ as fully encapsulating a mental health disorder. We need to be honest about what our favoured models really are, and are not, modelling. Furthermore, we would argue that the diagnostic system for mental disorders and the way we define them may impede research progress: we need to be open to the thought that our diagnostic criteria for specific disorders are fluid and evolving, and that alterations in psychological processes do not necessarily respect today's diagnostic boundaries. However, we have a different—and perhaps more optimistic—perspective on the problem than Hyman. We too think that a combinatorial, deconstructive then reconstructive approach will be fruitful in understanding mental health disorders—but we would promote strongly the notion that modelling should go beyond genetics. Genetics alone is not enough to be the key determinant of mental health. Indeed, modelling should go beyond any one subdiscipline of neuroscience; the questions are too great and span too many different levels of analysis to be solved only by neurogeneticists, or behavioural neuroscientists, or psychologists alone. What is needed is an inclusive and integrated approach, bringing together scientists working on basic genetic, molecular, neurochemical, anatomical and behavioural levels with clinicians and patients on the frontline, providing insights on what is, and is not, most useful, effective and acceptable for particular groups of patients, and describing alterations in psychological processing in terms that are readily backtranslatable.
There is a way forward for understanding mental health disorders and critically for understanding them in a way that can improve treatment. We need both top-down and bottom-up approaches if we are to get a full picture of mental health and its driving mechanisms. We would suggest that psychology can act as a bridge between these approaches. As the final common output of essentially all mental activity is behaviour in some form or another, we can organize our thinking on basic psychological processing, how it generates behaviour, and how top-down and bottom-up mechanisms modulate this behaviour.
Our approach suggests that this will probably mean simplifying complex behaviours into distinct psychological components so that they can be studied in isolation, or designing behavioural tasks that allow factorial analysis of different psychological components. These tasks should be translatable between animals and humans, and ideally would be transdiagnostic. They probably will not model a mental health disorder in its entirety—but simplification can be a virtue. Understanding the psychological routes to a specific behaviour will allow us to identify the neuronal circuits contributing to those psychological processes, in turn facilitating approaches focusing on specific neuron types, and molecular and genetic approaches. We need to study mechanisms at all levels from the behavioural and social to the molecular and cellular.
Psychological processes can be studied in patient populations—including across disorder types—and healthy individuals. The power of this approach is illustrated by work from Gillan & Robbins [29], in which large numbers of participants—a sample size potentially amenable to complementary genetic approaches—were recruited online to complete DSM-inspired [4] questionnaires assessing whether they had a mental health disorder, and behavioural tasks inspired by basic animal learning theory. This study identified three psychological processes that could account for behavioural performance across a range of tasks, and showed that the propensity of participants to develop habit-based associations was more predictive of obsessive–compulsive symptom severity than the DSM questionnaires. Coupled with information from animal behavioural studies, including genetic models, this gives potential for major insights into the development of compulsion in OCD—and potentially transdiagnostically for other disorders with an element of compulsion.
To conclude, we are of the opinion that the greatest advances in understanding mental health disorders will be made by the collaboration of scientists from many different fields, spanning levels of analysis, clinicians to basic scientists, all seeking common threads of research and speaking the same language. It is critical that basic scientists better understand current treatments and know which questions are important now. It is critical that clinical scientists understand fundamental insights and harvest benefits. The call for improved dialogue in research is being heard across mental health treatment modalities including pharmacological treatments [2] and psychological treatments [3]. What is needed is an inclusive and integrated approach, bringing together scientists working across all levels of enquiry with clinicians, providing insights on what works (and what does not) with patients, and describing alterations in psychological processing in terms that are readily backtranslatable.
To stimulate the much-needed innovation in therapeutic techniques, an analysis of component parts is critical. Our approach suggests value in simplifying complex behaviours into distinct psychological components, so that they can be studied in isolation. We have argued that one of the key values of animal models lies in their simplification of complex phenomena into underlying components that can be more readily understood. The use of animal models in the twentieth century contributed to innovations such as exposure therapy which provide among the most effective treatments for anxiety disorders we have to date. We do not just need new treatments per se, but ones that are more scalable to meet the global mental health need. Simplicity may also be an asset not only for understanding mechanisms of action, but also for delivering treatments at scale. The papers in this issue illustrate the power of translational approaches and highlight some of the challenges to be overcome. We also hope that this collection of papers illustrates the value of engaging with literature outside of our own immediate fields—seeing further in the pursuit of an improved scientific understanding of mental health.
Data accessibility
This article has no additional data.
Author contributions
All authors contributed actively to the writing of the paper and have approved the final version of the manuscript.
Competing interests
A.L.M. has no competing interests to declare. E.A.H. is an Honorary Professor of Clinical Psychology in the Department of Psychiatry at the University of Oxford, holds an honorary contract at the Medical Research Council Cognition and Brain Sciences Unit at the University of Cambridge and serves on the board of the charity ‘MQ: Transforming Mental Health’; she receives no renumeration for these roles.
Funding
We are grateful to the Royal Society for their support in convening the meeting ‘Of mice and mental health: facilitating dialogue between basic and clinical neuroscientists'. A.L.M. receives research support from the Medical Research Council (MR/N02530X/1) and the Wellcome Trust (200710/Z/16/Z), and is the Ferreras-Willetts Fellow in Neuroscience at Downing College, Cambridge. E.A.H. receives support from the Karolinska Institutet and the Lupina Foundation.
References
- 1.Holmes EA, Craske MG, Graybiel AM. 2014. A call for mental-health science. Nature 511, 287–289. ( 10.1038/511287a) [DOI] [PubMed] [Google Scholar]
- 2.Goodwin GM, et al. In press From neuroscience to evidence based psychological treatments – the promise and the challenge. Eur. Neuropsychopharmacol. ( 10.1016/j.euroneuro.2017.1010.1036) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holmes EA, et al. In press. Psychological treatments research in tomorrow's science: seeing further. Lancet Psychiatry. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. 2013. The diagnostic and statistical manual of mental disorders, 5th edn Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- 5.Craske MG, Hermans D, Vervliet B. 2018. State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Phil. Trans. R. Soc. B 373, 20170025 ( 10.1098/rstb.2017.0025) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shumake J, Jones C, Auchter A, Monfils M-H. 2018. Data-driven criteria to assess fear remission and phenotypic variability of extinction in rats. Phil. Trans. R. Soc. B 373, 20170035 ( 10.1098/rstb.2017.0035) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nader K, Schafe GE, LeDoux JE. 2000. Fear memories require protein synthesis in the amygdala for reconsolidation after retrieval. Nature 406, 722–726. ( 10.1038/35021052) [DOI] [PubMed] [Google Scholar]
- 8.Kindt M, van Emmerik A. 2016. New avenues for treating emotional memory disorders: towards a reconsolidation intervention for posttraumatic stress disorder. Therapeutic Adv. Psychopharmacol. 6, 283–295. ( 10.1177/2045125316644541) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xue Y-X, et al. 2012. A memory retrieval-extinction procedure to prevent drug craving and relapse. Science 336, 241–245. ( 10.1126/science.1215070) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Visser RM, Lau-Zhu A, Henson RN, Holmes EA. 2018. Multiple memory systems, multiple time points: how science can inform treatment to control the expression of unwanted emotional memories. Phil. Trans. R. Soc. B 373, 20170209 ( 10.1098/rstb.2017.0209) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.James EL, Bonsall MB, Hoppitt L, Tunbridge EM, Geddes JR, Milton AL, Holmes EA. 2015. Computer game play reduces intrusive memories of experimental trauma via reconsolidation-update mechanisms. Psychol. Sci. 26, 1201–1215. ( 10.1177/0956797615583071) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iyadurai L, Blackwell SE, Meiser-Stedman R, Watson PC, Bonsall MB, Geddes JR, Nobre AC, Holmes EA. In press. Preventing intrusive memories after trauma via a brief intervention involving Tetris computer game play in the emergency department: a proof-of-concept randomized controlled trial. Mol. Psychiatry. ( 10.1038/mp.2017.23) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horsch A, Vial Y, Fayrod C, Harari MM, Blackwell SE, Watson P, Iyadurai L, Bonsall MB, Holmes EA. 2017. Reducing intrusive traumatic memories after emergency caesarean section: a proof-of-principle randomized controlled study. Behav. Res. Ther. 94, 36–47. ( 10.1016/j.brat.2017.03.018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kindt M. 2018. The surprising subtleties of changing fear memory: a challenge for translational science. Phil. Trans. R. Soc. B 373, 20170033 ( 10.1098/rstb.2017.0033) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soeter M, Kindt M. 2015. An abrupt transformation of phobic behavior after a post-retrieval amnestic agent. Biol. Psychiatry. 78, 880–886. ( 10.1016/j.biopsych.2015.04.006) [DOI] [PubMed] [Google Scholar]
- 16.Albo Z, Gräff J. 2018. The mysteries of remote memory. Phil. Trans. R. Soc. B 373, 20170029 ( 10.1098/rstb.2017.0029) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Everitt BJ, Giuliano C, Belin D. 2018. Addictive behaviour in experimental animals: prospects for translation. Phil. Trans. R. Soc. B 373, 20170027 ( 10.1098/rstb.2017.0027) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deroche-Gamonet V, Belin D, Piazza PV. 2004. Evidence for addiction-like behavior in the rat. Science 305, 1014–1017. ( 10.1126/science.1099020) [DOI] [PubMed] [Google Scholar]
- 19.Pelloux Y, Everitt BJ, Dickinson A. 2007. Compulsive drug seeking by rats under punishment: effects of drug taking history. Psychopharmacology (Berl) 194, 127–137. ( 10.1007/s00213-007-0805-0) [DOI] [PubMed] [Google Scholar]
- 20.Milton AL, Everitt BJ. 2010. The psychological and neurochemical mechanisms of drug memory reconsolidation: implications for the treatment of addiction. Eur. J. Neurosci. 31, 2308–2319. ( 10.1111/j.1460-9568.2010.07249.x) [DOI] [PubMed] [Google Scholar]
- 21.Huang AS, Mitchell JA, Haber SN, Alia-Klein N, Goldstein RZ. 2018. The thalamus in drug addiction: from rodents to humans. Phil. Trans. R. Soc. B 373, 20170028 ( 10.1098/rstb.2017.0028) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore CF, Panciera JI, Sabino V, Cottone P. 2018. Neuropharmacology of compulsive eating. Phil. Trans. R. Soc. B 373, 20170024 ( 10.1098/rstb.2017.0024) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wood J, LaPalombara Z, Ahmari SE. 2018. Monoamine abnormalities in the SAPAP3 knockout model of obsessive-compulsive disorder-related behaviour. Phil. Trans. R. Soc. B 373, 20170023 (doi:10.1098.rstb.2017.0023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robinson ESJ. 2018. Translational new approaches for investigating mood disorders in rodents and what they may reveal about the underlying neurobiology of major depressive disorder. Phil. Trans. R. Soc. B 373, 20170036 ( 10.1098/rstb.2017.0036) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walsh AEL, Browning M, Drevets WC, Furey M, Harmer CJ. 2018. Dissociable temporal effects of bupropion on behavioural measures of emotional and reward processing in depression. Phil. Trans. R. Soc. B 373, 20170030 ( 10.1098/rstb.2017.0030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Canetta S, Kellendonk C. 2018. Can we use mice to study schizophrenia? Phil. Trans. R. Soc. B 373, 20170032 ( 10.1098/rstb.2017.0032) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.St. Clair D, Johnstone M. 2018. Using mouse transgenic and human stem cell technologies to model genetic mutations associated with schizophrenia and autism. Phil. Trans. R. Soc. B 373, 20170037 ( 10.1098/rstb.2017.0037) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hyman SE. 2018. The daunting polygenicity of mental illness: making a new map. Phil. Trans. R. Soc. B 373, 20170031 ( 10.1098/rstb.2017.0031) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gillan CM, Robbins TW. 2014. Goal-directed learning and obsessive-compulsive disorder. Phil. Trans. R. Soc. B 369, 20130475 ( 10.1098/rstb.2013.0475) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This article has no additional data.