Abstract
Podocytes contain an intricate actin cytoskeleton that is essential for the specialized function of this cell type in renal filtration. Serum response factor (SRF) is a master transcription factor for the actin cytoskeleton, but the in vivo expression and function of SRF in podocytes are unknown. We found that SRF protein colocalizes with podocyte markers in human and mouse kidneys. Compared with littermate controls, mice in which the Srf gene was conditionally inactivated with NPHS2-Cre exhibited early postnatal proteinuria, hypoalbuminemia, and azotemia. Histologic changes in the mutant mice included glomerular capillary dilation and mild glomerulosclerosis, with reduced expression of multiple canonical podocyte markers. We also noted tubular dilation, cell proliferation, and protein casts as well as reactive changes in mesangial cells and interstitial inflammation. Ultrastructure analysis disclosed foot process effacement with loss of slit diaphragms. To ascertain the importance of SRF cofactors in podocyte function, we disabled the myocardin-related transcription factor A and B genes. Although loss of either SRF cofactor alone had no observable effect in the kidney, deficiency of both recapitulated the Srf-null phenotype. These results establish a vital role for SRF and two SRF cofactors in the maintenance of podocyte structure and function.
Keywords: serum response factor, glomerulopathy, podocyte, renal failure, knockout
Podocytes are terminally differentiated cells of the glomerulus with elaborate extensions of the cell body that terminate as interdigitating foot processes separated by slit diaphragms essential for selective filtration at the glomerular filtration barrier.
Maintenance of podocyte structure and function is dependent on a complex actin cytoskeleton.1 Serum response factor (SRF) is a transcription factor that binds a DNA cis-acting element known as a CArG box.2 Conserved CArG boxes are adjacent to thousands of genes, including numerous cytoskeletal genes.3–5 Podocyte-specific knockout (KO) of SRF-dependent cytoskeletal-associated genes, such as Tln1,6 Cfl1,7 Itgb1,8 and Tjp1,9 results in defective glomerular function. SRF is regulated by PRKDC,10 a kinase that has been implicated as a susceptibility gene for adriamycin-induced nephropathy,11 and INF2, which has mutations that contribute to FSGS.12 However, the specific role of SRF in the kidney and particularly, within podocytes is ill defined. Here, evidence is provided in support of an essential role of SRF and two of its cofactors in maintaining the structure and function of podocytes in mice.
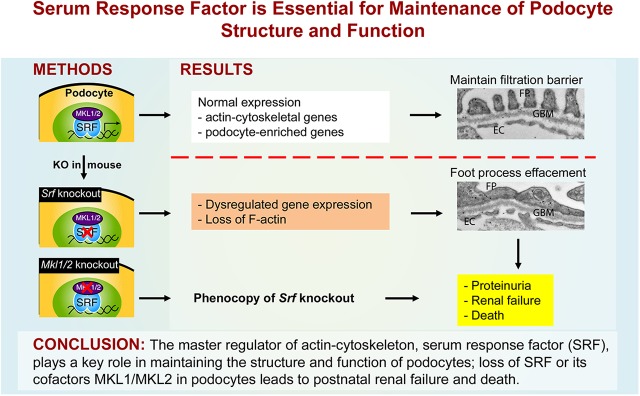
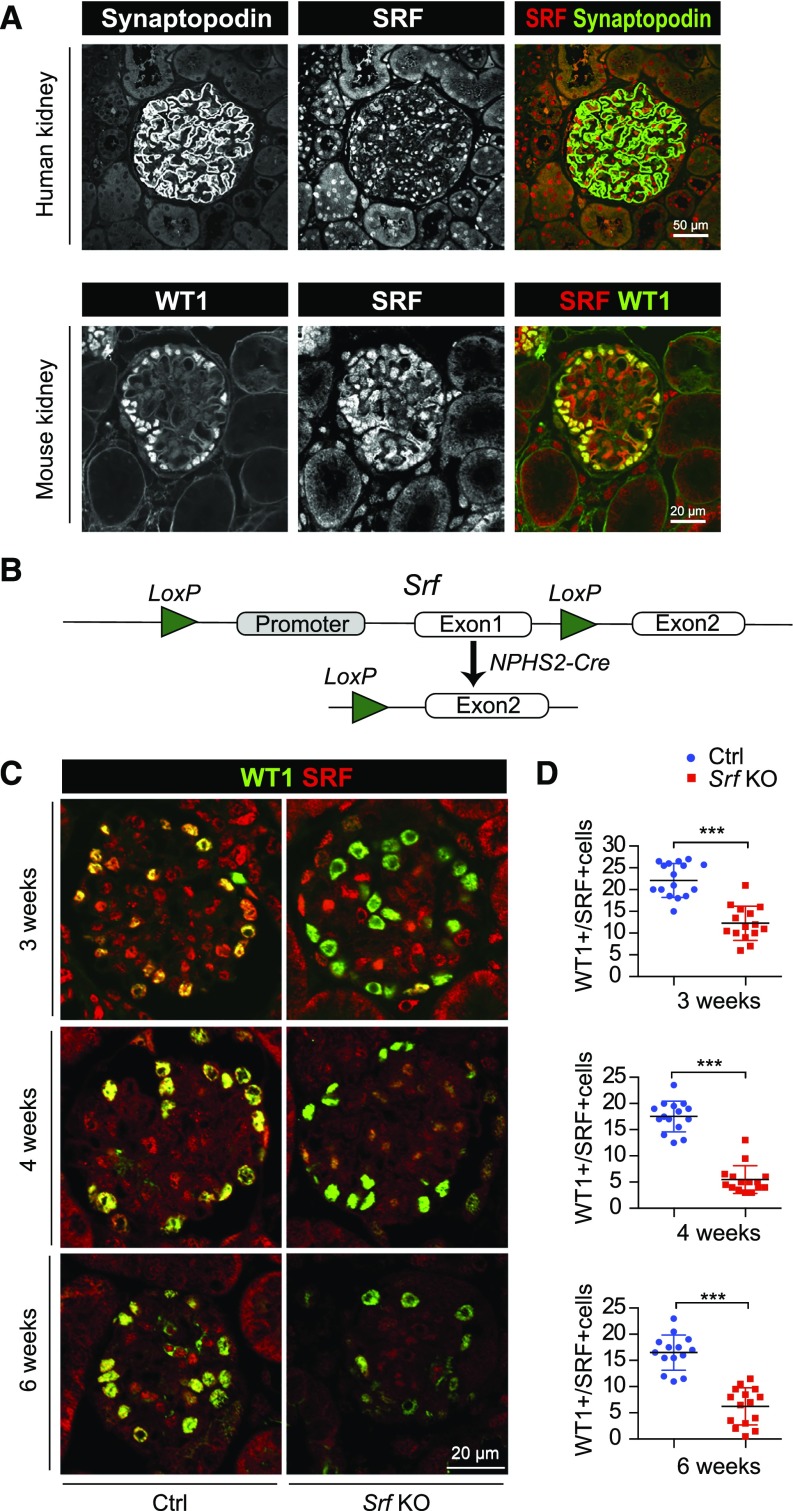
SRF is expressed in podocytes of the adult mouse and human kidney (Figure 1A), with onset of expression in mice occurring between embryonic day 18.5 and postnatal day 0 (Supplemental Figure 1A). A genetic cross to inactivate Srf in podocytes (Figure 1B) yielded an expected Mendelian ratio of pups (Supplemental Figure 1B) with normal glomerular structure (Supplemental Figure 1C). Furthermore, quantitative immunofluorescence microscopy (IFM) showed no change in the expression of SRF in podocytes of newborn, podocyte-specific Srf KO mice (Supplemental Figure 1, D and E). Together, these results suggest that SRF plays little, if any, role in glomerulogenesis during embryonic development.
Figure 1.
Generation of podocyte-specific Srf KO mice. (A) IFM of sections of human and mouse kidney shows SRF expression in both podocytes and nonpodocytes. Podocytes were identified by immunolabeling of Synaptopodin or WT1. Note that efforts to reliably show WT1 in human podocytes were unsuccessful. (B) General strategy for generating podocyte-specific Srf KO mice. (C) Representative images of control and mutant glomeruli immunolabeled with anti-WT1 (podocyte marker) and anti-SRF antibodies (Supplemental Figure 2 shows single-channel images). (D) Quantitative IFM of control and mutant glomeruli (n=15) shows 44.5%, 68.8%, and 62.2% reductions of SRF+/WT1+ podocytes at 3, 4, and 6 weeks, respectively. Scale bars, 50 μm in A, upper panel; 20 μm in A, lower panel and C. ***P<0.001.
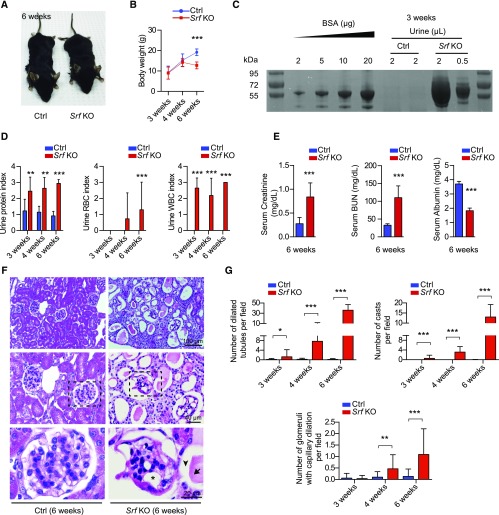
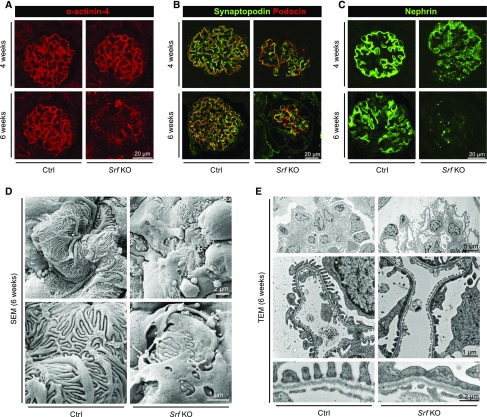
A significant reduction of SRF/WT1-positive cells was observed in Srf KO mice between 3 and 6 weeks after birth (Figure 1, C and D, Supplemental Figure 2). Although Srf KO mice were indistinguishable from littermate controls at birth, they exhibited a notable decrease in body size (Figure 2A) and body weight (Figure 2B) at 6 weeks of age. Srf KOs also displayed increased urinary protein, hematuria, and leukocyturia (Figure 2, C and D) as well as elevated serum creatinine and BUN, with concomitant hypoalbuminemia (Figure 2E). Death occurred by 7 weeks of age in both male and female Srf KO mice. Quantitative histopathology established progressive tubular dilation, protein cast formation, and glomerular capillary dilation in Srf KO mice (Figure 2, F and G). Lotus tetragonolobus lectin staining indicated dilation of both proximal and distal tubules (Supplemental Figure 3). Occasional instances of glomerulosclerosis were observed at 6 weeks of age with little to no interstitial fibrosis (Supplemental Figure 4), likely due to the rapid onset of kidney failure. IFM of Srf KO mice showed lower expression and irregular distribution of several podocyte markers, including α–Actinin-4, Synaptopodin, Podocin, and Nephrin (Figure 3, A–C). Furthermore, upregulation of smooth muscle α-actin and vWF was seen in Srf KO glomeruli (Supplemental Figure 5, A and B), suggestive of reactive changes in mesangial cells and glomerular capillary endothelial cells, respectively. Srf KO mice also exhibited an infiltration of CD45-positive inflammatory cells within the tubulointerstitium and Ki67 staining in tubular epithelial cells; no such findings were evident in control mice or within the glomerulus of Srf KO mice (Supplemental Figure 5, C–E). The presence of inflammatory cells and proliferative tubular epithelial cells of Srf KO mice likely represents a secondary response to the glomerulopathy-induced accumulation of tubular urinary casts. Ultrastructure analysis by scanning and transmission electron microscopy revealed occasional foot process effacement in 3-week-old Srf KO mice (data not shown); this phenotype was more pronounced at 6 weeks of age (Figure 3, D and E). Higher magnification showed loss of slit diaphragms between adjacent foot processes, with little evidence of alterations in glomerular basement membrane thickness or fenestrated endothelial cells (Figure 3E). Collectively, these results suggest that SRF plays an important role in maintaining postnatal podocyte structure and function.
Figure 2.
Postnatal nephropathy and renal failure in podocyte-specific Srf KO mice. (A and B) Decreased body size and body weight in Srf KO mice compared with control mice at 6 weeks of age (n≥5 age-matched male mice). (C) Coomassie Blue staining of urine samples shows massive proteinuria in 3-week-old mutant mice. (D) Dipstick analysis indicates increased urinary protein (left panel), red blood cells (RBCs; center panel), and white blood cells (WBCs; right panel) of mutant mice between 3 and 6 weeks of age (n≥7). (E) Serum analysis reveals elevated creatinine (left panel) and BUN (center panel) and decreased albumin (right panel) in 6-week-old Srf KO mice (n≥5). (F) Hematoxylin and Eosin staining of kidneys at 6 weeks of age. Note dilated tubules (arrowhead), glomerular capillary dilation (asterisk), and cast formation (arrow) in Srf KO kidneys (n≥3). (G) Quantitative measures of dilated tubules, protein casts, and glomerular capillary dilation in control versus Srf KO kidneys at 3, 4, and 6 weeks of age (n≥30 fields of view in three or more mice per condition). Scale bars, 100 μm in F, top panel; 40 μm in F, middle panel; 20 μm in F, bottom panel. *P<0.05; **P<0.01; ***P<0.001.
Figure 3.
Podocyte marker expression and ultrastructural abnormalities in Srf KO mice. (A–C) IFM shows diminished and punctate staining of (A) α–Actinin-4, (B) Synaptopodin and Podocin, and (C) Nephrin in mutant mice (n=3) at 4 and 6 weeks of age. (D and E) Representative (D) scanning electron microscopy (SEM) and (E) transmission electron microscopy (TEM) of control and Srf KO kidneys (n=2 each for control and mutant). Note (D, lower panel) foot process effacement and (E, bottom panel) loss of slit diaphragms in Srf KO. Scale bars, 20 μm in A–C; 2 μm in D, upper panel; 5 μm in E, top panel; 1 μm in D, lower panel and E, middle panel; 0.2 μm, E bottom panel.
To verify the regulatory role of SRF on podocyte actin cytoskeleton, we evaluated F-actin by phalloidin staining in a conditional immortalized podocyte cell line.13 siRNA-induced Srf knockdown attenuated phalloidin staining in differentiated podocytes, suggesting that low SRF in podocytes results in dysregulation of the actin cytoskeleton. Quantitative RT-PCR revealed dysregulated expression of podocyte-enriched genes,14 including Acta2, Fgfr1, and Actn4 (Supplemental Figure 6). The upregulation of Fgfr1 is of particular relevance in this context given its association with experimental membranous nephropathy15 and regulation by microRNA-16,16 a known SRF-dependent target gene.17
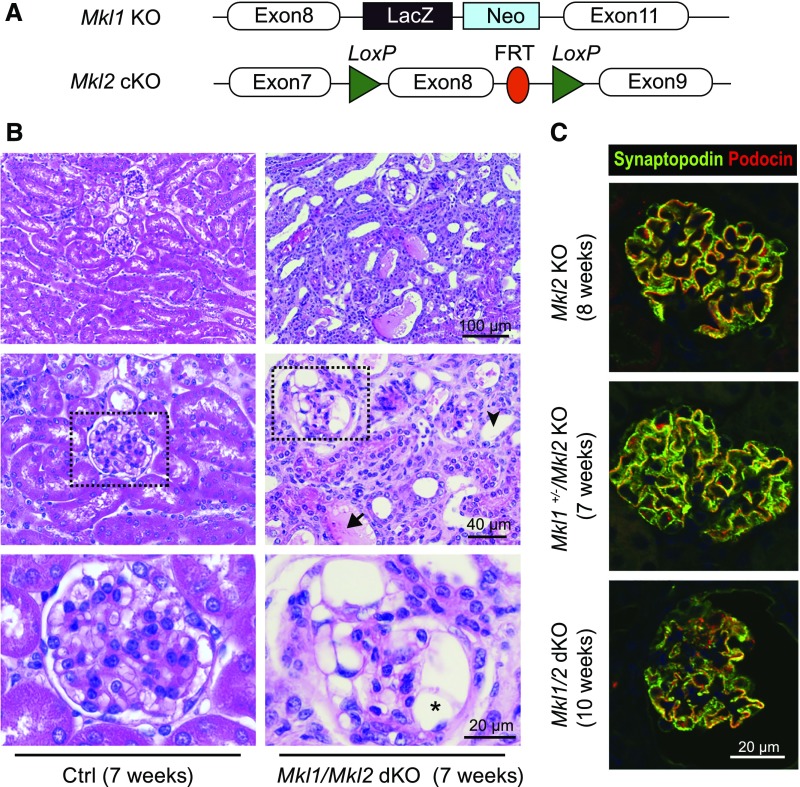
Because the myocardin family of transcriptional cofactors controls expression of contractile and actin cytoskeletal–related genes,18–20 we hypothesized these factors were key SRF cofactors mediating the observed phenotype. We first determined the relative mRNA expression of myocardin-related transcription factor A (Mkl1) and B (Mkl2) with another family member, Myocardin. Both Mkl1 and Mkl2 mRNA were more abundant in the glomerular-rich cortex than Myocardin (Supplemental Figure 7). Accordingly, we inactivated Mkl1 as a conventional KO,21 floxed Mkl222 using the NPHS2-Cre driver, or both Mkl1 and Mkl2 (Figure 4A). Unlike Srf KO mice, loss of either Mkl1 or Mkl2 showed no evidence of glomerular or renal tubular abnormalities (Supplemental Figure 8A). Furthermore, the histology of the kidney in three-allele Mkl KO mice (i.e., mice with only one wild-type allele of Mkl1 or Mkl2) up to 1 year of age was unremarkable (Supplemental Figure 8B), and there was no indication of proteinuria (Supplemental Figure 8C). In contrast, the Mkl1/Mkl2 double knockout (dKO) exhibited dilated tubules with numerous urinary casts and enlarged glomerular capillary loops as well as proteinuria at 7 weeks (Supplemental Figure 8, A and D), all of which are consistent with the histopathologic features of the podocyte-specific Srf KO (Figure 4B versus Figure 2F). Thus, a single allele from either Mkl cofactor seems to compensate for the loss of the other three alleles, a finding that contrasts with a prior Mkl KO study.23
Figure 4.
Recapitulation of the Srf KO phenotype in Mkl1/Mkl2 dKO mice. (A) Schematic of Mkl1 (conventional) and Mkl2 (conditional) KOs in podocytes (the NPHS2-Cre cross is not shown). Based on references 21 and 22. (B) Hematoxylin and Eosin staining of kidneys from control (wild-type) and Mkl1/Mkl2 dKO mice at 7 weeks of age. The asterisk, arrow, and arrowhead indicate the dilated glomerular capillary, the protein cast, and the dilated renal tubule, respectively. (C) IFM showing decreased and punctate expression of Synaptopodin and Podocin in dKO mice but not in Mkl2 KO and three-allele KOs at 7–10 weeks of age. Scale bars, 100 μm in B, top panel; 40 μm, B, middle panel; 20 μm in B, bottom panel and C.
We were unsuccessful in reliably detecting MKL cofactors in podocytes, likely because of technical limitations of available antibodies. However, the strong phenotype observed in the Mkl1/Mkl2 dKO but not observed in individual Mkl KOs implies the presence of both within podocytes. Of note, Mkl1/Mkl2 dKO mice, but not three-allele KO mice, showed somewhat lower expression of SRF in podocytes (Supplemental Figure 9); a similar reduction in Srf mRNA was seen in skeletal muscle lacking these cofactors.24 IFM disclosed reduced expression of Synaptopodin and Podocin in glomeruli of Mkl1/Mkl2 dKO mice but not in Mkl2 KO or three-allele KOs, which were comparable with wild-type mice (Figure 4C versus Figure 3B). The lifespan of Mkl1/Mkl2 dKO mice was over 10 weeks, slightly longer than Srf KO mice. Previous studies showed an injury-promoting role of SRF/MKL in kidney disease25–28; in contrast, data here support SRF and MKL1/MKL2 in the maintenance of normal podocyte structure and function.
Continued expression of WT1 in podocytes of the Srf KO and Mkl1/Mkl2 dKO suggests that Wt1 transcription is SRF/MKL independent. The absence of conserved SRF binding CArG boxes within proximal regulatory regions of the WT1 locus further supports this concept (J.M. Miano, unpublished observations). We propose that WT1 and other complementary transcription factors29 specify and direct the initial differentiation of podocytes, including the onset of cytoskeletal gene expression. Subsequently, SRF and MKL1/MKL2 direct a later program of gene expression necessary to augment and maintain the complex actin cytoskeleton, which is essential for the increasing demand on postnatal kidney filtration.
Transcriptomic data suggest that altered SRF expression may play a role in human kidney disease. For example, SRF mRNA is reduced in human diabetic glomeruli,30 and several SRF target genes are upregulated in human podocytes treated with glucocorticoids.31 Moreover, human mutations exist in different cytoskeletal genes, such as ACTN4, that are probable SRF targets on the basis of the presence of conserved CArG boxes and ChIP-seq data (J.M. Miano, unpublished observations). Of note, we previously reported the existence of CArG SNPs in the human genome, with such variants exhibiting defective SRF binding and target promoter activity.3 Given the abundant expression of SRF in human podocytes as reported here, it will be important to determine if levels of SRF protein change in podocytopathies and whether CArG SNPs exist that portend kidney disease. In contrast to SRF, several mutations in MKL1 and MKL2 are associated with human diseases, although none have been linked to kidney disease (https://www.ebi.ac.uk/gwas/).
In conclusion, SRF and MKL1/MKL2 are essential for postnatal podocyte structure and function, likely through the maintenance of a normal actin cytoskeleton. Future work should interrogate SRF and MKL1/MKL2 target genes within podocytes through integrative computational, RNA-seq, and ChIP-seq studies. Such information could shed new light on the pathogenesis of some podocytopathies and open up new opportunities for therapeutic interventions in CKD.
Concise Methods
Animals and Human Subjects
Srffl/fl, Mkl1−/−, Mkl2fl/fl, and NPHS2-Cre mice21,22,32,33 were used to produce podocyte-specific Srf KO mice (Srffl/fl/NPHS2-Cre) and Mkl1/Mkl2 single-KO, three-allele, and dKO mice. Supplemental Table 1 lists genotyping primers. Animals were treated in accordance with the National Institutes of Health animal care guidelines, and all animal experiments were approved by the Institutional Animal Care and Use Committee of the University of Rochester School of Medicine and Dentistry. Sections of deidentified human kidney biopsies were obtained with approval from the University of Rochester School of Medicine and Dentistry Research Subjects Review Board (RSRB00062813).
Urine, Serum, and Body Weight Analyses
Urine from control and Srf KO mice was collected for albumin and blood cell analysis by dipstick assay (Fisher Scientific, Hampton, NH) and Coomassie Blue staining. For quantification of dipstick data, different indices were assigned to corresponding ranges of protein, white blood cell, and red blood cell readings. Urine was resolved by SDS-PAGE gel and stained by SimplyBlue SafeStain (Invitrogen, Waltham, MA) according to the manufacture’s protocol. Blood samples were harvested via heart puncture and submitted to the Cobas 6000 Analyzer to measure serum levels of BUN, creatinine, and albumin. Body weight data were obtained from age-matched male control and Srf KO mice.
Histopathology and IFM
Kidney tissues were formalin fixed, paraffin embedded, and sectioned at 5-μm thickness. Slides were deparaffinized and rehydrated in PBS. Hematoxylin and Eosin staining, Masson trichrome staining (American MasterTech, Lodi, CA), and immunofluorescence staining were conducted according to standard procedures. Immunofluorescence images were taken on a confocal microscope (Olympus FV 1000). The primary antibodies and detailed procedures for immunostaining are provided in Supplemental Material and Supplemental Table 2. Quantitation of kidney histology and WT1+/SRF+ cells was conducted by two independent observers blind to genotype.
Electron Microscopy
For scanning electron microscopy, the kidneys were fixed in 0.1 M sodium cacodylate–buffered 2.5% glutaraldehyde/4.0% paraformaldehyde fixative, postfixed in buffered 1.0% osmium tetroxide, dehydrated, and sputter coated with gold. A Zeiss Auriga Supra Field Emission Microscope was used to photograph the fractured glomeruli. For transmission electron microscopy, the kidneys were osmicated, dehydrated, and embedded in EPON/Araldite resin. Thin sections (70 nm) on grids were stained with aqueous uranyl acetate and lead citrate and photographed using a Hitachi 7650 Microscope with an attached Gatan Erlangshen 11-megapixel digital camera.
Quantitative Real-Time PCR
Total RNA was extracted from the aorta and kidney cortex of wild-type adult mice and cultured podocytes using the RNAeasy Kit (Qiagen, Hiden, Germany), treated with DNAase I (Invitrogen), and reverse transcribed into cDNA with iScript Reverse Transcription Supermix (Bio-Rad, Hercules, CA). SYBR Green Supermix (Bio-Rad) was used for quantitative PCR; relative mRNA levels to Gapdh or Rhoa were normalized to the control sample using the 2−∆∆Ct method. Sequences of real-time primers are provided in Supplemental Table 3.
Cell culture, Srf knockdown, and phallodin staining are described in Supplemental Material.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank Karen L. De Mesy Bentley and the University of Rochester Medical Center Electron Microscopy Core for generating the electron microscopic images.
B.G. is supported by a grant from Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. A.G.G. is supported by Department of Defense Peer Reviewed Medical Investigator-Initiated Research award PR151419, and E.M.S. is supported by National Institutes of Health (NIH) grants HL120919 and HL133761. J.M.M. is supported by NIH grants HL112793 and HL117907.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2017050473/-/DCSupplemental.
References
- 1.Faul C, Asanuma K, Yanagida-Asanuma E, Kim K, Mundel P: Actin up: Regulation of podocyte structure and function by components of the actin cytoskeleton. Trends Cell Biol 17: 428–437, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Minty A, Kedes L: Upstream regions of the human cardiac actin gene that modulate its transcription in muscle cells: Presence of an evolutionarily conserved repeated motif. Mol Cell Biol 6: 2125–2136, 1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benson CC, Zhou Q, Long X, Miano JM: Identifying functional single nucleotide polymorphisms in the human CArGome. Physiol Genomics 43: 1038–1048, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olson EN, Nordheim A: Linking actin dynamics and gene transcription to drive cellular motile functions. Nat Rev Mol Cell Biol 11: 353–365, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee MY, Park C, Berent RM, Park PJ, Fuchs R, Syn H, Chin A, Townsend J, Benson CC, Redelman D, Shen TW, Park JK, Miano JM, Sanders KM, Ro S: Smooth muscle cell genome browser: Enabling the identification of novel serum response factor target genes. PLoS One 10: e0133751, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian X, Kim JJ, Monkley SM, Gotoh N, Nandez R, Soda K, Inoue K, Balkin DM, Hassan H, Son SH, Lee Y, Moeckel G, Calderwood DA, Holzman LB, Critchley DR, Zent R, Reiser J, Ishibe S: Podocyte-associated talin1 is critical for glomerular filtration barrier maintenance. J Clin Invest 124: 1098–1113, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garg P, Verma R, Cook L, Soofi A, Venkatareddy M, George B, Mizuno K, Gurniak C, Witke W, Holzman LB: Actin-depolymerizing factor cofilin-1 is necessary in maintaining mature podocyte architecture. J Biol Chem 285: 22676–22688, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pozzi A, Jarad G, Moeckel GW, Coffa S, Zhang X, Gewin L, Eremina V, Hudson BG, Borza DB, Harris RC, Holzman LB, Phillips CL, Fassler R, Quaggin SE, Miner JH, Zent R: Beta1 integrin expression by podocytes is required to maintain glomerular structural integrity. Dev Biol 316: 288–301, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Itoh M, Nakadate K, Horibata Y, Matsusaka T, Xu J, Hunziker W, Sugimoto H: The structural and functional organization of the podocyte filtration slits is regulated by Tjp1/ZO-1. PLoS One 9: e106621, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu SH, Ma JT, Yueh AY, Lees-Miller SP, Anderson CW, Ng SY: The carboxyl-terminal transactivation domain of human serum response factor contains DNA-activated protein kinase phosphorylation sites. J Biol Chem 268: 21147–21154, 1993 [PubMed] [Google Scholar]
- 11.Papeta N, Zheng Z, Schon EA, Brosel S, Altintas MM, Nasr SH, Reiser J, D’Agati VD, Gharavi AG: Prkdc participates in mitochondrial genome maintenance and prevents Adriamycin-induced nephropathy in mice. J Clin Invest 120: 4055–4064, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie J, Hao X, Azeloglu EU, Ren H, Wang Z, Ma J, Liu J, Ma X, Wang W, Pan X, Zhang W, Zhong F, Li Y, Meng G, Kiryluk K, He JC, Gharavi AG, Chen N: Novel mutations in the inverted formin 2 gene of Chinese families contribute to focal segmental glomerulosclerosis. Kidney Int 88: 593–604, 2015 [DOI] [PubMed] [Google Scholar]
- 13.Mundel P, Reiser J, Zúñiga Mejía Borja A, Pavenstädt H, Davidson GR, Kriz W, Zeller R: Rearrangements of the cytoskeleton and cell contacts induce process formation during differentiation of conditionally immortalized mouse podocyte cell lines. Exp Cell Res 236: 248–258, 1997 [DOI] [PubMed] [Google Scholar]
- 14.Lu Y, Ye Y, Bao W, Yang Q, Wang J, Liu Z, Shi S: Genome-wide identification of genes essential for podocyte cytoskeletons based on single-cell RNA sequencing. Kidney Int 92: 1119–1129, 2017 [DOI] [PubMed] [Google Scholar]
- 15.Floege J, Kriz W, Schulze M, Susani M, Kerjaschki D, Mooney A, Couser WG, Koch KM: Basic fibroblast growth factor augments podocyte injury and induces glomerulosclerosis in rats with experimental membranous nephropathy. J Clin Invest 96: 2809–2819, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chamorro-Jorganes A, Araldi E, Penalva LO, Sandhu D, Fernández-Hernando C, Suárez Y: MicroRNA-16 and microRNA-424 regulate cell-autonomous angiogenic functions in endothelial cells via targeting vascular endothelial growth factor receptor-2 and fibroblast growth factor receptor-1. Arterioscler Thromb Vasc Biol 31: 2595–2606, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park C, Hennig GW, Sanders KM, Cho JH, Hatton WJ, Redelman D, Park JK, Ward SM, Miano JM, Yan W, Ro S: Serum response factor-dependent MicroRNAs regulate gastrointestinal smooth muscle cell phenotypes. Gastroenterology 141: 164–175, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pipes GC, Creemers EE, Olson EN: The myocardin family of transcriptional coactivators: Versatile regulators of cell growth, migration, and myogenesis. Genes Dev 20: 1545–1556, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Parmacek MS: Myocardin-related transcription factors: Critical coactivators regulating cardiovascular development and adaptation. Circ Res 100: 633–644, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Miano JM: Myocardin in biology and disease. J Biomed Res 29: 3–19, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li S, Chang S, Qi X, Richardson JA, Olson EN: Requirement of a myocardin-related transcription factor for development of mammary myoepithelial cells. Mol Cell Biol 26: 5797–5808, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mokalled MH, Johnson A, Kim Y, Oh J, Olson EN: Myocardin-related transcription factors regulate the Cdk5/Pctaire1 kinase cascade to control neurite outgrowth, neuronal migration and brain development. Development 137: 2365–2374, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith EC, Thon JN, Devine MT, Lin S, Schulz VP, Guo Y, Massaro SA, Halene S, Gallagher P, Italiano JE Jr., Krause DS: MKL1 and MKL2 play redundant and crucial roles in megakaryocyte maturation and platelet formation. Blood 120: 2317–2329, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cenik BK, Liu N, Chen B, Bezprozvannaya S, Olson EN, Bassel-Duby R: Myocardin-related transcription factors are required for skeletal muscle development. Development 143: 2853–2861, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao L, Wang X, Sun L, Nie H, Liu X, Chen Z, Guan G: Critical role of serum response factor in podocyte epithelial-mesenchymal transition of diabetic nephropathy. Diab Vasc Dis Res 13: 81–92, 2016 [DOI] [PubMed] [Google Scholar]
- 26.Zhao L, Chi L, Zhao J, Wang X, Chen Z, Meng L, Liu G, Guan G, Wang F: Serum response factor provokes epithelial-mesenchymal transition in renal tubular epithelial cells of diabetic nephropathy. Physiol Genomics 48: 580–588, 2016 [DOI] [PubMed] [Google Scholar]
- 27.Sakai N, Chun J, Duffield JS, Lagares D, Wada T, Luster AD, Tager AM: Lysophosphatidic acid signaling through its receptor initiates profibrotic epithelial cell fibroblast communication mediated by epithelial cell derived connective tissue growth factor. Kidney Int 91: 628–641, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu H, Wu X, Qin H, Tian W, Chen J, Sun L, Fang M, Xu Y: Myocardin-related transcription factor a epigenetically regulates renal fibrosis in diabetic nephropathy. J Am Soc Nephrol 26: 1648–1660, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rascle A, Suleiman H, Neumann T, Witzgall R: Role of transcription factors in podocytes. Nephron, Exp Nephrol 106: e60–e66, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Woroniecka KI, Park AS, Mohtat D, Thomas DB, Pullman JM, Susztak K: Transcriptome analysis of human diabetic kidney disease. Diabetes 60: 2354–2369, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiang L, Hindmarch CC, Rogers M, Campbell C, Waterfall C, Coghill J, Mathieson PW, Welsh GI: RNA sequencing analysis of human podocytes reveals glucocorticoid regulated gene networks targeting non-immune pathways. Sci Rep 6: 35671, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moeller MJ, Sanden SK, Soofi A, Wiggins RC, Holzman LB: Podocyte-specific expression of cre recombinase in transgenic mice. Genesis 35: 39–42, 2003 [DOI] [PubMed] [Google Scholar]
- 33.Miano JM, Ramanan N, Georger MA, de Mesy Bentley KL, Emerson RL, Balza RO Jr., Xiao Q, Weiler H, Ginty DD, Misra RP: Restricted inactivation of serum response factor to the cardiovascular system. Proc Natl Acad Sci U S A 101: 17132–17137, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.