Abstract
Background:
Osteosarcoma (OS) is the most common primary malignant tumor of bone. The survival of OS patients has steadily improved from <20% in the early 20th century to around 70% with current treatment. There are very few studies in pediatric OS from India analyzing various aspects of the disease. This study focuses on the clinical profile, treatment options, and their complications and survival outcomes in pediatric osteosarcoma (OS) patients.
Materials and Methods:
This was a retrospective observational study which included pediatric patients <14 years of age, with newly diagnosed OS confirmed by histological diagnosis. Medical records of all patients were reviewed for clinical profile, treatment data, surgical management, and treatment complications. Patients alive at the end of treatment were followed up and overall (OAS) and disease-free survival (DFS) were analyzed.
Results:
Sixty-two patients were diagnosed with OS during the study of whom 55 opted for treatment. Cisplatin, adriamycin, and ifosfamide (PAI) was offered as chemotherapy and was completed as planned in the majority of patients. Limb salvage surgery was performed in most patients (87%, n = 40). The local recurrence occurred in 7 patients. The 3 years overall survival for the cohort was 54.6% ± 7.8% and DFS was 43.4% ± 7.9%, with females and those with the localized disease having a significantly better DFS.
Conclusions:
High dose methotrexate free chemotherapy can give good OAS in localized disease and LSS is feasible in most of the pediatric OS patients. However the modest DFS even for localized disease with PAI chemotherapy and extremely poor outcomes in the metastatic OS, demand further research and innovations in systemic therapy to improve outcomes.
Keywords: Limb salvage, Cisplatin, Adriamycin, Ifosfamide chemotherapy, pediatric osteosarcoma
MeSH terms: Cancer chemotherapy protocols, paediatrics, retrospective studies, methotrexate
Introduction
Osteosarcoma (OS) the most common primary malignant tumor of bone, has an incidence worldwide of approximately one to three cases per million annually.1 The survival of OS patients has steadily improved from <20% in the early 20th century to around 70% with current treatment. In developing nations like India, the survival rates are still low compared to the developed nations.2 Patients generally tend to present late, and the disease is more advanced at presentation. This along with the use of less intense chemotherapy, delayed or inadequate surgery and limited supportive care facilities contribute to the poorer outcomes. There are very few studies in pediatric OS from India analyzing various aspects of the disease such as clinical presentation, treatment modalities, and outcome of treatment. In this study, we present the experience from a tertiary level pediatric oncology center in India.
Materials and Methods
This was a retrospective observational study. The permission of the Institutional Review Board was obtained. All newly diagnosed cases of OS in children ≤14 years, registered at the Pediatric Oncology division of our center from January 2008 to December 2013 were included. The treatment given was neoadjuvant chemotherapy with a combination of cisplatin (CDDP), adriamycin, ifosfamide – Cisplatin, Adriamycin, Ifosfamide (PAI) regimen, followed by surgery and further adjuvant chemotherapy. Surgery was planned after three cycles of chemotherapy. For patients undergoing endoprosthetic replacement a 3 cm marrow clear margin was taken based on preoperative magnetic resonance imaging findings and reconfirmed on intraoperative frozen section study. In those patients in whom intercalary resections were performed, the open physis was also considered as sufficient margin. One layer of normal muscle was retained over the extraosseous tumor component to get adequate wide margins.
The patients who were treated elsewhere, relapsed OS and those from whom consent was not obtained were excluded from study.
The medical records of all patients included in the study were analyzed for the clinical profile, investigations, imaging, surgical details, and followup data.
Statistical methods
The data analysis was performed with the help of Division of Epidemiology and Cancer Research of the Institute. Frequency tables for descriptive data were made for different variables. Mean and median values were calculated as appropriate. Kaplan–Meier survival analysis was used for calculating the overall and disease-free survival (DFS). The impact of selected variables on the survival was calculated by univariate analysis. For variables with significant impact on survival multivariate analysis was performed.
Results
Sixty-two patients were newly diagnosed as OS during the study. Six patients with advanced disease and one patient with extraosseous OS opted out of treatment and were excluded from the analysis of treatment details and survival analysis. Mean age of presentation was 10.9 years with a male to female ratio of 0.94:1. The mean duration of symptoms was 7. 5 weeks (range 1–28 weeks).
The main symptoms at presentation were pain and swelling in 48% of patients (n = 30), swelling in 21% (n = 13), or pain alone in19% (n = 12). Uncommon symptoms included Bell's palsy (n = 1), anorexia (n = 1), weight loss (n = 2), fever (n = 2), and limping (n = 1).
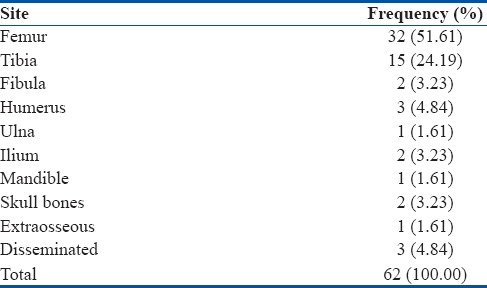
The most common site of involvement was the femur in 32 children (51%) followed by tibia in 15 children (24%). Less commonly involved sites were the humerus (n = 3), fibula (n = 2), ilium (n = 2), mandible (n = 1), ulna (n = 1), and skull bones (n = 2). Three children presented with disseminated disease affecting multiple bones. There was one patient with extraosseous OS in the popliteal fossa [Table 1]. Pathological fracture at the primary site was observed in 13 patients (21%) at the time of presentation.
Table 1.
Sites of involvement
Patients were evaluated for metastasis using bone scan, chest X-ray, and computed tomography scan of thorax. The disease was staged as localized and advanced based on the metastatic status. 71% of patients (n = 44) had localized disease confined to the primary site. One-third (n = 18) presented with advanced disease with metastasis in lungs alone (n = 8) or bones alone (n = 4) or both lungs and bones (n = 6).
The number of preoperative chemotherapy cycles planned were three, but the actual number of cycles administered varied based on the time to surgery. The timing of surgery varied due to logistic reasons, chemotherapy complications and patient preference. The median number of preoperative cycles of chemotherapy administered was four. Six patients received six cycles of PAI before surgery. These were patients with advanced disease, and five of these patients refused surgery. Mean duration between surgery and restarting chemotherapy was 20 days (range 14–40 days).
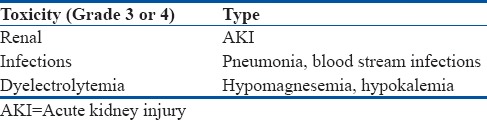
Major toxicities noted were infections, dyselectrolytemias, and acute kidney injury (AKI). Forty percent of patients experienced Grade 3 or 4 toxicities. Thirty-three patients did not have any grade 3 or 4 toxicity. AKI developed in 6 patients. In four patients, AKI occurred after completing the planned six cycles of chemotherapy and so further treatment modification was not required. In one patient, AKI occurred after four cycles of chemotherapy and treatment protocol were modified substituting carboplatin for CDDP, which was well tolerated. There was one case of treatment related mortality due to renal failure [Table 2].
Table 2.
Chemotherapy related toxicity
Of the 55 patients, 50 patients (90%) completed the planned six cycles of chemotherapy. Four patients defaulted and one patient expired after four cycles of chemotherapy. In this cohort of 55 patients, 46 (83.6%) patients underwent surgery. Nine patients refused surgery due to advanced disease, defaulted or died during chemotherapy.
Data regarding the histologic response to preoperative chemotherapy was available in 29 patients out of 46 who underwent surgery. Of these 29 patients, 72% had a good response to chemotherapy as defined by >90% tumor necrosis in the resected specimen and 28% had a poor response to chemotherapy.
Limb salvage surgery (LSS) was done in the majority of patients, n = 40 (87%), including patients with advanced disease. Amputation (AK/BK) was required only in 6% of cases (n = 3). One patient underwent internal hemipelviectomy. Two patients underwent fibulectomy. One patient with lesion in mandible underwent wide excision with reconstruction with fibular graft [Table 3].
Table 3.
Types of surgery
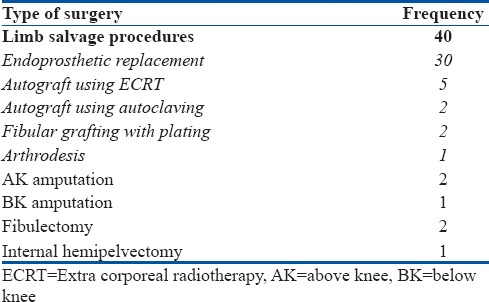
Different procedures were used for limb salvage depending on the primary site and extent of the tumor. Most commonly employed technique was wide excision of the tumor with adequate margin and endoprosthetic replacement. Replacement was with metallic endoprosthesis in 30 patients. Two patients had a fibular graft with plating. One patient had resection of the distal femur tumor with knee joint arthrodesis. Autograft with extra corporeal radiotherapy (ECRT) (n = 5) or bone autoclaving (n = 2) were done in seven patients.
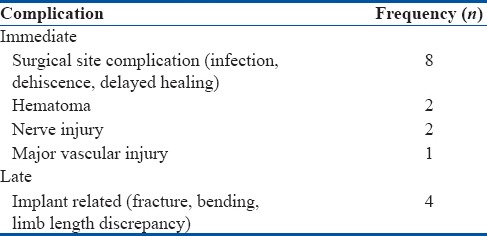
30% (n = 13) of the patients undergoing LSS had intraoperative or immediate postoperative complications. Four patients developed implant related complications [Table 4].
Table 4.
Surgery related complications
There were 19 recurrences including two recurrences in the same patient-seven local and 12 metastatic (pulmonary metastasis in 7 and bone metastasis in 5). Most of the recurrences occurred within the 1st year. Median time to relapse was 4 months (range 1–29 months). Of the seven patients in whom bone which has been sterilized by ECRT or autoclaving used only one had a local recurrence. Six recurrences received further treatment in the form of local radiotherapy (n = 2), repeat wide excision of the local recurrence (n = 2) and metastasectomy of the pulmonary lesion (n = 2). Of the 18 patients with recurrence, all expired, except one patient who was still alive with disease at the time of the study.
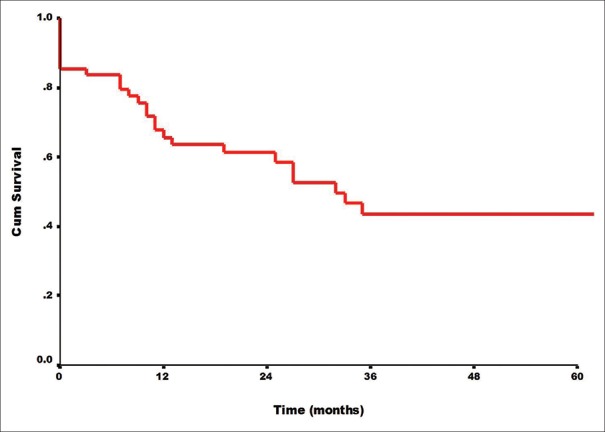
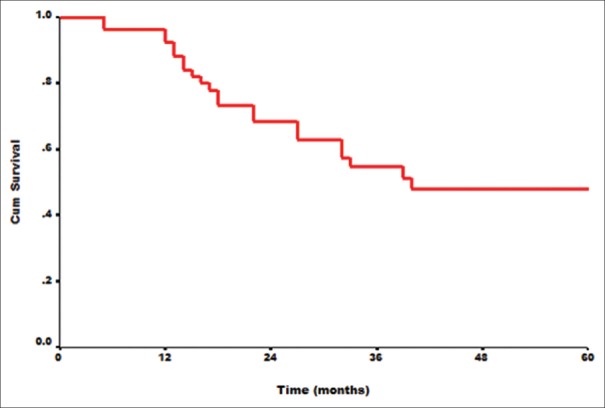
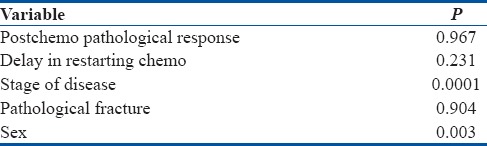
At a median followup of 25 months, the 3 years overall survival (OAS) for all patients who received treatment (n = 55) was 54.6% ±7.8% and DFS was 43.4% ± 7.9% [Figures 1 and 2]. The stage of disease was found to be the most significant factor influencing DFS and OAS. For localized disease OAS and DFS at 3 years were 88.2% and 54.9%, respectively, whereas for advanced disease OAS and DFS were only 9.3% and 0% at 3 years. This was highly significant with a P = 0.00001. Female sex was associated with better DFS (P = 0.0032), though OAS was not significantly better (P = 0.122). Other factors analyzed such as age, pathological fracture at presentation, post-chemotherapy tumor necrosis, site of primary tumor, and delay in restarting chemotherapy (>14 days) after surgery were not found to have a significant impact on the survival [Table 5].
Figure 1.
Kaplan–Meir disease free survival
Figure 2.
Kaplan–Meir overall survival
Table 5.
P values of tested variables for disease free survival for the entire cohort
Discussion
This study has been done on a cohort of patients receiving a rather uniform treatment protocol. Almost 1/3 of our patients had metastatic disease at presentation, which probably is one of the reasons for poor OAS in our series. At the time of OS diagnosis, about 10%–20% of patients present with macroscopic evidence of metastatic disease, most commonly in the lungs (90%), but metastasis can also develop in bone (8%–10%) and rarely in lymph nodes.3,4,5
Our chemotherapy regimen was devoid of high dose methotrexate (HDMtx), which is a standard component in most chemotherapy protocols around the world.6 The role of HDMtx has been established by various randomized and nonrandomized trials. However, some groups have tried regimens without HDMtx and achieved similar results. Daw et al. conducted a multi-institutional trial (OS99) that evaluated the efficacy of carboplatin, ifosfamide, and doxorubicin in 72 patients with newly diagnosed, localized, resectable OS. The regimen produced outcomes comparable to those of CDDP-containing or HDMTx-containing regimens.7 Carboplatin, ifosfamide, and doxorubicin given without HDMTX resulted in 5-year event free survival (EFS) and survival estimates of 66.7% and 78.9%, respectively.8
In developing countries like India, administration of HDMtx at doses of 8–12 g/m2 entails a lot of resource consumption and management of drug toxicities which is not always feasible. Many oncology centers use PAI regimen, but the data regarding the survival in pediatric patients is scarce. This is to the best of our knowledge, the first single center study in India giving the treatment and survival data in pediatric OS patients managed uniformly with a comparatively less intense regimen. Compliance to chemotherapy was good, with 90% of the patients completing the planned six cycles of chemotherapy and local therapy. There were a few defaulters (4 out of 55) and one treatment-related mortality.
The mainstay for successful treatment of OS is surgery.9 Surgical techniques have evolved over the past few decades, and limb salvage strategies have become standard of care. Data are limited regarding outcomes of children undergoing LSS in India.2 Amputation would be considered only when the tumor cannot be excised with a safe margin.10 We opted for limb salvage procedures for all patients including those with advanced disease if they showed regression of metastasis during preoperative assessment. Autografts were used, wherever feasible, using ECRT for bone sterilization. Data support the use of this technique with excellent results.2,11 Only one out of the seven patients in our series had local recurrence. ECRT is, therefore, a safe procedure with low rates of local recurrence and permits early mobilization and bone growth.11,12
The local recurrence in patients undergoing LSS in our series was 15%. The slightly higher rate may be because of the inclusion of patients with the extensive local disease. Most studies suggest that LSS may offer a better quality of life for such patients even though the OS may not be improved.13 However, some have not demonstrated a clear benefit.14,15 Hence, patient selection criteria should be clear, and patients who may require multiple revision surgery or may have poor functional outcomes should not be offered LSS, especially in a resource-limited setting. The incidence of local recurrence is closely related to the achieved surgical margins (intralesional, marginal, wide, and radical), with only a wide margin being considered appropriate.16 All the patients who underwent LSS in our series had a wide margin of resection. However, there is lack of consensus regarding the ideal surgical margin.17 Surgery related complications, although it occurred in 28% of cases, were mostly minor, [Table 5] primarily due to wound site infection and healing and this rate is comparable to others at around 25%. A few like implant-related complications required surgical intervention.
Renard et al. have reported that complications were more common after limb-salvage surgery than after amputation.18 On the other hand, Mavrogenis et al. reported a similar rate of complications, survival and recurrence rates after limb-salvage surgery or amputation for distal tibia OS, but functional outcomes were better with LSS.19 The rates of secondary amputation after limb-salvage surgery ranged from 7.7% to 21.2%.18 In our series, implant revision were required in four patients (8%).
The 3 years OAS for all patients included for final analysis in our study was 54%. This is lower than reported by most of the major pediatric OS trials which have 5 years OAS of over 60%. The lower OAS in our series perhaps reflects the inadequate therapy for an advanced disease which was also treated with the same three drug PAI protocol.
A total of 30%–40% of patients with localized OS will develop a local or distant recurrence.20 Approximately 90% of relapses are lung metastasis, which usually occur in the first 2–3 years.
In this study, we have assessed the impact of various demographic, clinical and investigation parameters on OAS and DFS by univariate and multivariate analysis. The only two factors which had a significant impact on survival were gender and stage at presentation, with males and advanced disease at presentation having poor outcomes. In our series, both OAS and DFS were better for females. However, only DFS, not OAS achieved statistically significant difference. Female gender had significantly improved OAS among all adequately treated patients as reported in a study by Berner et al.21 In another study from Rizzoli Institute of 300 patients, gender was not a significant risk factor.22 However in our series, the difference in survival was striking, with females having a DFS twice that of males. The reason for this disparity cannot be explained. The second significant factor affecting survival was the stage at presentation. Patients with advanced disease had a very dismal outcome. Children with advanced OS at presentation have a poor outcome universally. OAS at 5 years has remained <30% in most studies. In the study by COSS 96 published in 2001, the 15 patients out of 122 who had advanced disease at presentation, the OAS was only 16.6%. This was despite a more intense regimen containing five drugs.23 Intensified treatment for these patients with regimens including HDMtx and an attempt to do metastasectomy for patients with pulmonary metastasis may improve survival in these patients.24
Histological response of the resected tumor to preoperative chemotherapy represents the most important prognostic factor, with patients who achieve a good histological response having a better prognosis.25 Studies have consistently demonstrated 5-year EFS rates of 35%–45% for poor responders and 70%–80% for good responders.12 However, some studies suggest that although intensified chemotherapeutic regimens increases tumor necrosis, the OAS remains unchanged.4 The degree of tumor necrosis was assessed in around half the patients in our study, but this was not found to have an impact on survival, may be due to a smaller sample size of the study.
In our series, delay in resumption of chemotherapy after surgery did not have a significantly worse outcome than others, whereas other studies have shown decreased EFS and increased mortality with a delay of >3 weeks.26,27 Pathological fracture was also not associated with any significant effect on the outcome. It was not used as a selection criterion for LSS in our series. Some series have associated pathological fracture with a higher rate of local recurrence and a lower rate of OAS.28 However, Salunke et al. in a meta analysis of eight studies did not find a significant impact on outcome.29
The strength of this study is that we have a single institution series of patients treated with a uniform approach, including chemotherapy and surgical management. This series also has a reasonable followup period with surgical details that could be analyzed for impact on survival.
Conclusions
OS in children presents with advanced disease in a significant number of patients. LSS was feasible in the majority of pediatric patients with OS. However, local recurrence occurred in 17% of patients. Careful selection of patients may give better results. Stage of the disease was the single most important prognostic factor predicting survival. Although with PAI chemotherapy, OAS appears good, the low DFS even for localized disease calls for much improvement in treatment and alternate chemotherapy regimens may have to be explored.
Patient declaration statement
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ottaviani G, Jaffe N. The epidemiology of osteosarcoma. Cancer Treat Res. 2009;152:3–13. doi: 10.1007/978-1-4419-0284-9_1. [DOI] [PubMed] [Google Scholar]
- 2.Tiwari A, Jain S, Mehta S, Kumar R, Kapoor G, Kumar K, et al. Limb salvage surgery for osteosarcoma: Early results in Indian patients. Indian J Orthop. 2014;48:266–72. doi: 10.4103/0019-5413.132511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bielack SS, Kempf-Bielack B, Delling G, Exner GU, Flege S, Helmke K, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: An analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002;20:776–90. doi: 10.1200/JCO.2002.20.3.776. [DOI] [PubMed] [Google Scholar]
- 4.Bacci G, Longhi A, Versari M, Mercuri M, Briccoli A, Picci P, et al. Prognostic factors for osteosarcoma of the extremity treated with neoadjuvant chemotherapy: 15-year experience in 789 patients treated at a single institution. Cancer. 2006;106:1154–61. doi: 10.1002/cncr.21724. [DOI] [PubMed] [Google Scholar]
- 5.Kager L, Zoubek A, Pötschger U, Kastner U, Flege S, Kempf-Bielack B, et al. Primary metastatic osteosarcoma: Presentation and outcome of patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2003;21:2011–8. doi: 10.1200/JCO.2003.08.132. [DOI] [PubMed] [Google Scholar]
- 6.Luetke A, Meyers PA, Lewis I, Juergens H. Osteosarcoma treatment – Where do we stand? A state of the art review. Cancer Treat Rev. 2014;40:523–32. doi: 10.1016/j.ctrv.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Daw NC, Neel MD, Rao BN, Billups CA, Wu J, Jenkins JJ, et al. Frontline treatment of localized osteosarcoma without methotrexate: Results of the St. Jude children's research hospital OS99 trial. Cancer. 2011;117:2770–8. doi: 10.1002/cncr.25715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Machak GN, Tkachev SI, Solovyev YN, Sinyukov PA, Ivanov SM, Kochergina NV, et al. Neoadjuvant chemotherapy and local radiotherapy for high-grade osteosarcoma of the extremities. Mayo Clin Proc. 2003;78:147–55. doi: 10.4065/78.2.147. [DOI] [PubMed] [Google Scholar]
- 9.Geller DS, Gorlick R. Osteosarcoma: A review of diagnosis, management, and treatment strategies. Clin Adv Hematol Oncol. 2010;8:705–18. [PubMed] [Google Scholar]
- 10.Simon MA, Aschliman MA, Thomas N, Mankin HJ. Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur 1986. J Bone Joint Surg Am. 2005;87:2822. doi: 10.2106/JBJS.8712.cl. [DOI] [PubMed] [Google Scholar]
- 11.Davidson AW, Hong A, McCarthy SW, Stalley PD. En-bloc resection, extracorporeal irradiation, and re-implantation in limb salvage for bony malignancies. J Bone Joint Surg Br. 2005;87:851–7. doi: 10.1302/0301-620X.87B6.15950. [DOI] [PubMed] [Google Scholar]
- 12.Gulia A, Puri A, Agarwal MG, Laskar S, Reddy K. Diaphyseal reconstruction with extrcorporeal irradiated autogenous tumor bone. Orthop Proc. 2012;94-B(Suppl 14):30. [Google Scholar]
- 13.Mei J, Zhu XZ, Wang ZY, Cai XS. Functional outcomes and quality of life in patients with osteosarcoma treated with amputation versus limb-salvage surgery: A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2014;134:1507–16. doi: 10.1007/s00402-014-2086-5. [DOI] [PubMed] [Google Scholar]
- 14.Eiser C, Darlington AS, Stride CB, Grimer R. Quality of life implications as a consequence of surgery: Limb salvage, primary and secondary amputation. Sarcoma. 2001;5:189–95. doi: 10.1080/13577140120099173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagarajan R, Kamruzzaman A, Ness KK, Marchese VG, Sklar C, Mertens A, et al. Twenty years of followup of survivors of childhood osteosarcoma: A report from the childhood cancer survivor study. Cancer. 2011;117:625–34. doi: 10.1002/cncr.25446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grimer RJ, Carter SR, Tillman RM, Abudu S, Jeys L. Osteosarcoma with poor necrosis and close margins – Amputation or limb salvage? J Bone Joint Surg Br. 2012;94-B(Suppl 14):45. [Google Scholar]
- 17.Andreou D, Bielack SS, Carrle D, Kevric M, Kotz R, Winkelmann W, et al. The influence of tumor- and treatment-related factors on the development of local recurrence in osteosarcoma after adequate surgery. An analysis of 1355 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. Ann Oncol. 2011;22:1228–35. doi: 10.1093/annonc/mdq589. [DOI] [PubMed] [Google Scholar]
- 18.Renard AJ, Veth RP, Schreuder HW, Schraffordt Koops H, van Horn J, Keller A, et al. Revisions of endoprosthetic reconstructions after limb salvage in musculoskeletal oncology. Arch Orthop Trauma Surg. 1998;117:125–31. doi: 10.1007/s004020050211. [DOI] [PubMed] [Google Scholar]
- 19.Mavrogenis AF, Abati CN, Romagnoli C, Ruggieri P. Similar survival but better function for patients after limb salvage versus amputation for distal tibia osteosarcoma. Clin Orthop Relat Res. 2012;470:1735–48. doi: 10.1007/s11999-011-2238-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kempf-Bielack B, Bielack SS, Jürgens H, Branscheid D, Berdel WE, Exner GU, et al. Osteosarcoma relapse after combined modality therapy: An analysis of unselected patients in the cooperative osteosarcoma study group (COSS) J Clin Oncol. 2005;23:559–68. doi: 10.1200/JCO.2005.04.063. [DOI] [PubMed] [Google Scholar]
- 21.Berner K, Hall KS, Monge OR, Weedon-Fekjær H, Zaikova O, Bruland ؘS, et al. Prognostic factors and treatment results of high-grade osteosarcoma in Norway: A scope beyond the “classical” patient. Sarcoma. 2015;2015:516843. doi: 10.1155/2015/516843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bacci G, Longhi A, Ferrari S, Lari S, Manfrini M, Donati D, et al. Prognostic significance of serum alkaline phosphatase in osteosarcoma of the extremity treated with neoadjuvant chemotherapy: Recent experience at Rizzoli institute. Oncol Rep. 2002;9:171–5. [PubMed] [Google Scholar]
- 23.Eselgrim M, Grunert H, Kühne T, Zoubek A, Kevric M, Bürger H, et al. Dose intensity of chemotherapy for osteosarcoma and outcome in the cooperative osteosarcoma study group (COSS) trials. Pediatr Blood Cancer. 2006;47:42–50. doi: 10.1002/pbc.20608. [DOI] [PubMed] [Google Scholar]
- 24.Errani C, Longhi A, Rossi G, Rimondi E, Biazzo A, Toscano A, et al. Palliative therapy for osteosarcoma. Expert Rev Anticancer Ther. 2011;11:217–27. doi: 10.1586/era.10.172. [DOI] [PubMed] [Google Scholar]
- 25.Jawad MU, Cheung MC, Clarke J, Koniaris LG, Scully SP. Osteosarcoma: Improvement in survival limited to high-grade patients only. J Cancer Res Clin Oncol. 2011;137:597–607. doi: 10.1007/s00432-010-0923-7. [DOI] [PubMed] [Google Scholar]
- 26.Meyers PA, Gorlick R, Heller G, Casper E, Lane J, Huvos AG, et al. Intensification of preoperative chemotherapy for osteogenic sarcoma: Results of the memorial Sloan-Kettering (T12) protocol. J Clin Oncol. 1998;16:2452–8. doi: 10.1200/JCO.1998.16.7.2452. [DOI] [PubMed] [Google Scholar]
- 27.Imran H, Enders F, Krailo M, Sim F, Okuno S, Hawkins D, et al. Effect of time to resumption of chemotherapy after definitive surgery on prognosis for non-metastatic osteosarcoma. J Bone Joint Surg Am. 2009;91:604–12. doi: 10.2106/JBJS.H.00449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scully SP, Ghert MA, Zurakowski D, Thompson RC, Gebhardt MC. Pathologic fracture in osteosarcoma: Prognostic importance and treatment implications. J Bone Joint Surg Am. 2002;84-A:49–57. [PubMed] [Google Scholar]
- 29.Salunke AA, Chen Y, Tan JH, Chen X, Khin LW, Puhaindran ME, et al. Does a pathological fracture affect the prognosis in patients with osteosarcoma of the extremities? a systematic review and meta-analysis. Bone Joint J. 2014;96-B:1396–403. doi: 10.1302/0301-620X.96B10.34370. [DOI] [PubMed] [Google Scholar]