Abstract
Chondroblastomas are a primary benign cartilaginous tumor that accounts for approximately 1% of all benign bone tumors. Primarily they are treated by curettage. The patient presented 4 years after a successfully treated chondroblastoma (curettage and Bone cement). Wide resection of the proximal tibia with endoprosthesis replacement was done. Lung CT showed multiple lung metastasis and despite starting chemotherapy, he succumbed to the disease. We discuss regarding the possibilities of “aggressive” chondroblastoma and more recently termed chondroblastoma-like osteosarcoma which is a separate entity from chondroblastoma. Aggressiveness in chondroblastoma can be 1 of 3 types as follows: 1. benign chondroblastoma with lung metastasis. 2. malignant chondroblastoma. 3. subsequent malignant transformation of benign chondroblastoma. We have attempted to review the literature and describe the “aggressive” chondroblastoma and chondroblastoma-like osteosarcoma in this report.
Keywords: Aggressive chondroblastoma, sarcomatous transformation, secondary osteosarcoma
MeSH terms: Chondroblastoma, tumor, osteosarcoma, aggressiveness, review literature
Introduction
Chondroblastomas are a primary benign cartilaginous tumor that accounts for approximately 1% of all benign bone tumors.1 They are commonly seen at the epiphysis region in an immature long bone.2 Despite being benign, they do metastasis to the lung in 2% of cases. Chondroblastomas are primarily treated by curettage. Historically, radiation was used to achieve local control in selected cases, and this accounted for some post-irradiation sarcoma.3 Precaution is taken to minimize damage to the adjacent physeal plate. Commonly the remaining cavity is filled with either bone graft or cement to achieve stability and prevent joint collapse. In recent years, radio-frequency ablation is carried out and it gives promising results.4 As these treatments are considered intralesional, they carry a risk of local recurrence of 8%–40%.5,6 In the past, irradiation was not uncommon in treating chondroblastoma, and this accounted for some post-irradiation sarcoma. Malignancy associated with chondroblastoma without irradiation was unheard of until 1970 when Sirsat reported a case of chondroblastoma eventually presenting as a high-grade undifferentiated sarcoma.7 We report a case of benign chondroblastoma which subsequently manifested as high-grade conventional osteosarcoma. As far as we are concerned, this is a first of such case ever reported in the literature. We will discuss the three different types of aggressive chondroblastoma and additionally also discuss regarding a variant of osteosarcoma known as chondroblastoma-like osteosarcoma.
Case Report
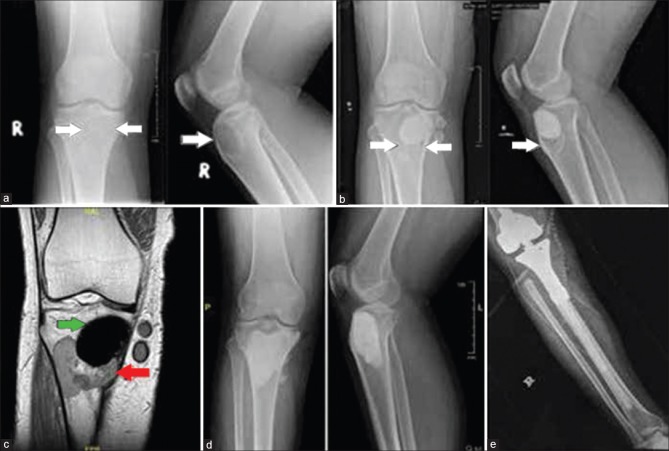
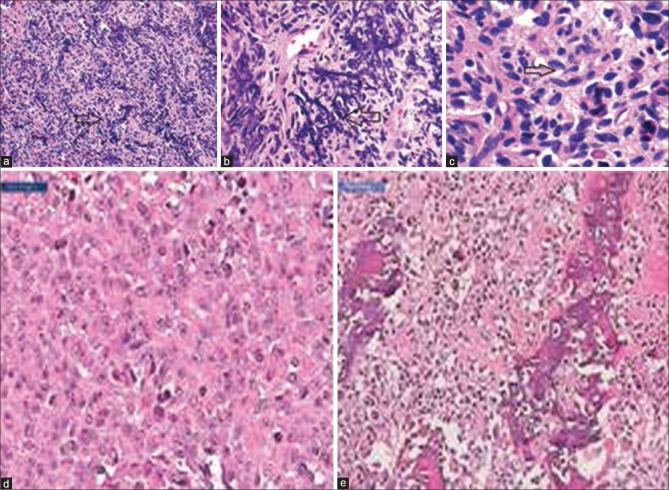
A 29-year-old male presented with a painful swelling over his right knee for 4 months duration in 2011. The plain radiograph showed an eccentric lytic lesion over the epiphysis of right proximal tibia [Figure 1a]. Open biopsy confirmed chondroblastoma extended curettage and bone using Bone cement [Polymethyl methacrylate (PMMA)] was performed. The final diagnosis remained as chondroblastoma [Figure 2a-c]. He was followed up monthly for the first 3 months, then 3 monthly for a year and 6 monthly until he developed local recurrence. At each followup, clinical palpation and X-ray were performed to look for local recurrence. He was symptom free for the next 4 years. In 2015, he presented to the followup clinic with pain and swelling over the right knee. Plain radiograph revealed a lytic lesion just adjacent to previous PMMA cement in keeping with local recurrence [Figure 1b]. Magnetic resonance imaging showed a homogenous lesion adjacent to the previous bone cement [Figure 1c]. Chest X-ray at this point was clear with no evidence of lung metastasis. Alkaline phosphatase and lactate dehydrogenase were within normal limit. Repeat curettage with bone cementation was done [Figure 1d] for the lesion. Within a few weeks, his knee pain and swelling worsened. He was in pain, especially while weight bearing and the pain did disturb his sleep. His knee range of motion was restricted from 15° to 110° of flexion. The histopathology report from the curettage unfortunately came back as conventional osteosarcoma. Further systemic staging showed multiple small lung nodules in keeping with distance metastasis. The bone scan, however, did not pick up any skeletal metastasis. He further underwent proximal tibia wide resection with endoprosthesis reconstruction and medial gastrocnemius flap followed by adjuvant chemotherapy [Figure 1e]. Postoperative, his wound healing was uncomplicated, and he started regaining good function of his right lower limb with physiotherapy. The resected specimen was send for histopathology and margins and revealed a high-grade conventional osteosarcoma [Figure 2d and e] with close margins. The histology was reviewed and confirmed by two bone and soft-tissue pathologist as the local pathologist was well aware of the rarity of this case. The patient was started on adjuvant chemotherapy consisting of doxorubicin 25 mg/m2 and cisplatin 50 mg/m2. Sadly, he succumb to lung metastasis after his 3rd cycle of chemotherapy.
Figure 1.
(a) Initial plain radiograph of the knee anteroposterior and lateral views showing an eccentric lytic lesion involving the epiphysis of right proximal tibia in keeping with chondroblastoma (white arrow) (b) Plain radiograph of the knee 5 years after the initial surgery showing a lytic lesion adjacent to previous bone cement in keeping with local recurrence of chondroblastoma (white arrow) (c) Coronal T2 weighted magnetic resonance image showing a heterogenous hypodense lesion at the metaphyseal region (red arrow) of right proximal tibia adjacent to previous cement (green arrow). (d) Plain radiograph of right knee post repeat curretage and polymethyl methacrylat cementation (e) X-ray of knee joint with leg bones anteroposterior view showing proximal tibia endoprosthesis
Figure 2.
Histopathology of slides showing (a) Uniform and cellular chondroblastic proliferation with calcification. (black arrow). (b) Areas with chicken wire calcification suggestive of chondroblastoma (black arrow). (c) Histiocytic-like cells displaying nuclear groves (black arrow). (d) The tumour consists of predominantly epithelioid cells exhibiting vesicular nuclei, clumped chromatin, prominent nucleoli and moderate amount of pale to eosinophilic cytoplasm. (e) Areas of lace like osteoid deposition with irregular mineralisation
Discussion
To the best of our knowledge, this is the first case of an established chondroblastoma which eventually transformed into conventional osteosarcoma in a non-iradiated limb. Although there may be an argument that the earlier disease might have been osteosarcoma from the beginning, we defer to disagree as the patient was well for 4 years before he developed a local recurrence. Naturally, in osteosarcoma with no chemotherapy on board, the patient would have succumbed within 2 years of the initial disease.
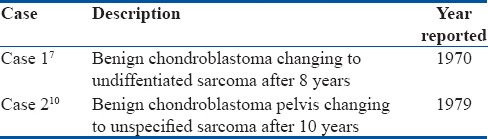
Aggressiveness in chondroblastoma can be subdivided into three types; malignant chondroblastoma, benign chondroblastoma with lung metastasis and benign chondroblastoma with subsequent development of high-grade malignancy. Subsequent development of malignancy is common in post-irradiation cases. However, a benign chondroblastoma subsequently presenting as a high-grade sarcoma is the rarest among all of them.8 To the best of our knowledge, there have been only two cases reported so far [Table 1].
Table 1.
Cases with malignant transformation of benign chondroblastoma reported previously
Chondroblastoma
Chondroblastomas are a rare benign bone lesions that predominantly occurs in growing bone in the epiphyseal region. It is histologically marked by the presence of chondroblast arranged in chicken-wire pattern with the presence of multinucleated giant cell and mononuclear stromal cells.9,10 They are treated by curettage and bone grafting or cementation. They carry a local recurrence rate of 8%–40%.5,6
Malignant Chondroblastoma
The term “malignant” is probably misnomer. In fact, Aycan et al. termed “malignant chondroblastoma” as a histologically benign lesion. The term “malignant” denotes its metastatic potential and aggressive behavior rather than histological malignancy.11 Approximately 2% of benign chondroblastoma do metastasis to the lung. The metastatic lesion in lung carries similar morphology of being benign as well. The term malignant chondroblastoma is synonymous with aggressive chondroblastoma and metastatic chondroblastoma; none of which are histologically malignant.
Malignant Transformation of a Chondroblastoma
Malignant transformation of chondroblastoma is defined as sarcoma arising in a previous chondroblastoma site. It can be subdivided into two more groups; post-irradiation sarcoma and “secondary” sarcoma at previous chondroblastoma site. When it comes to chondroblastoma, the “malignant” part of it is probably not as clearly defined as giant cell tumor. Malignancy in giant cell tumor (GCT) is divided into primary malignant GCT and secondary malignant GCT. Primary malignant GCT is defined as high-grade sarcoma arising side by side a benign GCT, and secondary malignant GCT is a high-grade sarcoma arising in a previous benign GCT site. Postradiation sarcoma is the most common type of secondary malignant GCT.12 This probably can be used for chondroblastoma, but due to its rarity, there has not been any formal classification of this sort before. In fact, there have only been two cases of sarcoma arising in previous chondroblastoma site [Table 1]. Our case is probably the first ever case of a secondary osteosarcoma arising at a previous chondroblastoma site.
Chondroblastoma-like Osteosarcoma
Although chondroblastoma-like osteosarcoma is completely separate entity from chondroblastoma, we would like to discuss it as it probably has significant historical relation to chondroblastoma. It was first described in 1990 by Schajowicz et al.13 Despite carrying the name chondroblastoma, it is a rare variant of osteosarcoma. It commonly occurs in the bone of the foot. It is thought to be <1% of all osteosarcoma. It is often misdiagnosed as a benign lesion and probably accounted for many of the “malignant” or “aggressive” chondroblastoma that were reported before 1990. In 1985, Kyriakos et al. reported a case of aggressive malignant chondroblastoma which presented with lung metastasis which eventually killed the patient.8 They did emphasis, while most malignant or aggressive behavior occurs after some surgical intervention, this case was not such as it was malignant from the presentation. It is cases like this that makes us wonder if they were probably chondroblastoma-like osteosarcoma from the onset and thus the aggressive behavior. It is not until the next 5 years before this entity is first described in 1990. As for now, we probably poorly understand chondroblastoma-like osteosarcoma due to its extremely rare occurrence.
To conclude, this case has been a unique and challenging case for us. It is definitely very interesting to find out that a merely benign chondroblastoma can present as an aggressive osteosarcoma after 4 years of being “disease-free.” The subsequent disease being very aggressive, presenting with lung metastasis and proved to be fatal despite patient being on chemotherapy.
Patient declaration statement
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jaffe HL, Lichtenstein L. Benign chondroblastoma of bone: A Reinterpretation of the so-called calcifying or chondromatous giant cell tumor. Am J Pathol. 1942;18:969–91. [PMC free article] [PubMed] [Google Scholar]
- 2.Elek EM, Grimer RJ, Mangham DC, Davies AM, Carter SR, Tillman RM, et al. Malignant chondroblastoma of the os calcis. Sarcoma. 1998;2:45–8. doi: 10.1080/13577149878154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akai M, Tateishi A, Machinami R, Iwano K, Asao T. Chondroblastoma of the sacrum. A case report. Acta Orthop Scand. 1986;57:378–81. doi: 10.3109/17453678608994417. [DOI] [PubMed] [Google Scholar]
- 4.Xie C, Jeys L, James SL. Radiofrequency ablation of chondroblastoma: Long term clinical and imaging outcomes. Eur Radiol. 2015;25:1127–34. doi: 10.1007/s00330-014-3506-1. [DOI] [PubMed] [Google Scholar]
- 5.Springfield DS, Capanna R, Gherlinzoni F, Picci P, Campanacci M. Chondroblastoma. A review of seventy cases. J Bone Joint Surg Am. 1985;67:748–55. [PubMed] [Google Scholar]
- 6.Lin PP, Thenappan A, Deavers MT, Lewis VO, Yasko AW. Treatment and prognosis of chondroblastoma. Clin Orthop Relat Res. 2005;438:103–9. doi: 10.1097/01.blo.0000179591.72844.c3. [DOI] [PubMed] [Google Scholar]
- 7.Sirsat MV, Doctor VM. Benign chondroblastoma of bone. Report of a case of malignant transformation. J Bone Joint Surg Br. 1970;52:741–5. [PubMed] [Google Scholar]
- 8.Kyriakos M, Land VJ, Penning HL, Parker SG. Metastatic chondroblastoma. Report of a fatal case with a review of the literature on atypical, aggressive, and malignant chondroblastoma. Cancer. 1985;55:1770–89. doi: 10.1002/1097-0142(19850415)55:8<1770::aid-cncr2820550825>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 9.Reyes CV, Kathuria S. Recurrent and aggressive chondroblastoma of the pelvis with late malignant neoplastic changes. Am J Surg Pathol. 1979;3:449–55. doi: 10.1097/00000478-197910000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Aycan OE, Vanel D, Righi A, Arikan Y, Manfrini M. Chondroblastoma-like osteosarcoma: A case report and review. Skeletal Radiol. 2015;44:869–73. doi: 10.1007/s00256-014-2068-2. [DOI] [PubMed] [Google Scholar]
- 11.Duttaluri R, Sultanpurkar GP, Raorane H, Vikram H. Malignant chondroblastoma of extraskeletal origin. Int J Appl Basic Med Res. 2016;6:146–8. doi: 10.4103/2229-516X.179028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bertoni F, Bacchini P, Staals EL. Malignancy in giant cell tumor of bone. Cancer. 2003;97:2520–9. doi: 10.1002/cncr.11359. [DOI] [PubMed] [Google Scholar]
- 13.Schajowicz F, de Próspero JD, Cosentino E. Case report 641: Chondroblastoma-like osteosarcoma. Skeletal Radiol. 1990;19:603–6. doi: 10.1007/BF00241285. [DOI] [PubMed] [Google Scholar]