Abstract
Background and Aims:
Supraglottic airways (SGAs) are generally used for airway management; but can also be used as a conduit for tracheal intubation. Our primary aim was to evaluate i-Gel and laryngeal mask airway (LMA) classic as conduits for tracheal intubation using ventilating bougie by assessing number of attempts and time for insertion of SGAs, ventilating bougie and endotracheal tube (ETT), and total intubation time.
Material and Methods:
A randomized clinical trial was carried out in 58 patients requiring general anesthesia and endotracheal intubation for planned surgery. They were randomly divided into Group I and Group C. After induction of anesthesia, i-Gel was inserted in Group I and LMA Classic in Group C; ventilating bougie was passed through SGA followed by the removal of SGA and railroading of ETT over ventilating bougie. Parameters observed were number of attempts and time taken for device insertion, total intubation time, and hemodynamic variables.
Results:
Twenty-nine patients were included in each group. First attempt success rate for SGA insertion (86.2% in Group I and 75.9% in Group C (P = 0.5)), ventilating bougie insertion (79.32% in Group I and 82.8% in Group C (P = 0.99)) and ETT insertion (100% in Group I and 96.5% in Group C) was not different in the two groups. Total intubation time was 93.3 ± 9.0 s in Group I and 108. 96 ± 16.5 s in Group C (P < 0.0001).
Conclusions:
i-Gel and LMA Classic both can be used as a conduit for tracheal intubation using ventilating bougie with stable hemodynamic parameters.
Key words: Dexmedetomidine, polyvinyl chloride endotracheal tube, supraglottic airways, tracheal tube introducer, ventilating bougie
Introduction
In case of difficult and/or failed intubation, supraglottic airways (SGAs) serve as an alternative airway, and can also serve as a conduit for tracheal intubation. Among them, some (intubating laryngeal mask airway [ILMA], C-Trach) allow intubation with appropriate sized endotracheal tube (ETT), but are costly while some SGAs (laryngeal mask airway [LMA] classic, i-Gel, ProSeal LMA) are cheaper, easily available, but intubation through them is possible only with small sized ETT. This problem has been overcome using tracheal tube introducers such as Aintree intubation catheter (AIC), guide wire/exchange catheter, and gum-elastic bougie.[1,2,3,4,5] Ventilating bougie is one such airway device, which helps in unhurried intubation through SGAs.
Our primary aim was to compare i-Gel and LMA Classic as a conduit for tracheal intubation, using ventilating bougie as a tracheal tube introducer, by assessing their efficacy in terms of number of attempts and insertion time for SGAs, ventilating bougie and ETT, and total intubation time. Secondary aim was to assess hemodynamic changes and complications if any.
Material and Methods
This randomized clinical trial was carried out after approval from the Institutional Ethics Committee for human research and clinical trial registration (NCT02566135, clinicaltrial.gov). Written and informed consent was obtained from all patients after explaining the study protocol. Preanesthetic assessment included medical/surgical history, general/systemic examination, airway examination, and investigations (complete hemogram, renal functions, blood sugar levels, chest X-ray, and electrocardiogram). We selected patients of 18–60 years of age, either gender, American Society of Anesthesiologists Physical Status Grade I or II, weighing 40–70 kg with normal airway (Mallampati Grade I/II), posted for planned surgery requiring general anesthesia and endotracheal (ET) intubation. Patients with obesity (body mass index >25), mouth opening <2 cm, Mallampati Grade III/IV, history of gastro-oesophageal reflux disease, inadequate fasting, and known or anticipated difficult tracheal intubation, or face mask ventilation were excluded from the study. All the patients were kept nil by mouth for 6–8 h. After taking the patient in operation theater, a vital sign monitor was attached and preoperative heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), oxygen saturation, and electrocardiogram were recorded. Intravenous (IV) line was secured and dextrose normal saline was started. Patients were randomly allocated into two groups of 29 each based on the computer-generated codes. Appropriate size i-Gel® (Intersurgical Inc., Berkshire, UK) and LMA Classic™ (Teleflex Medical Europe Ltd.) were inserted in Group I and Group C, respectively. Ventilating bougie was marked with a marker pen before its use. First marking was done at 21 cm from distal tip; the distance at which the ventilating bougie comes out of SGAs. Second mark was made at 26 cm; so that 5 cm of ventilating bougie is outside the SGAs, allowing hold over bougie preventing accidental displacement while removing SGAs. Another mark was made to indicate the direction of the angulated tip facing anteriorly. SGAs, ventilating bougie, and ETT were checked and lubricated using water-based jelly before procedure.
Patients were premedicated with glycopyrrolate 0.2 mg, ondansetron 4 mg, ranitidine 50 mg, and dexmedetomidine 1 μg/kg IV over 10 min before induction. Preoxygenation was done for 3 min with 100% oxygen with closed circuit. Anesthesia was then induced with propofol 2–2.5 mg/kg till loss of eyelid reflex followed by vecuronium bromide 0.1 mg/kg IV. Lungs were ventilated with 100% oxygen for 180 s. The patient's head was placed in sniffing the morning air position. Size selections of SGAs were done on the basis of weight as recommended by manufacturer's guidelines.[6] Appropriate sized SGA was inserted and closed circuit was attached. Proper placement of SGAs was confirmed by bilateral equal chest excursion, air entry on auscultation, absence of gastric insufflations, absence of audible leak on IPPV, and “sine” wave pattern on capnography. In case of absence of any one of the above criteria, SGAs were repositioned by doing up and down movement and head and neck maneuvers.[7] In case of failure to reposition the SGAs, it was removed and again inserted. After confirmation of correct positioning of SGAs, closed circuit was detached and ventilating bougie was introduced through SGA with its angled tip facing anteriorly up to 26 cm and closed circuit was attached to ventilating bougie. Correct insertion of bougie was confirmed by air entry over chest (using O2 flush) and absence of gastric insufflations sound. In case of failure to pass ventilating bougie into the trachea, it was taken out, rotated by 180°, and reinserted. Once placement of ventilating bougie was confirmed, closed circuit was detached and SGAs were removed gently (in case of LMA Classic after deflation of cuff) keeping ventilating bougie in situ. Then, appropriate-sized polyvinyl chloride ETT was railroaded over ventilating bougie with its bevel facing left, ventilating bougie was removed, and closed circuit was attached to ETT. ETT with internal diameter of 7.0 and 8.5 mm was used for female and male patients, respectively. In case of ETT impingement, ETT was removed and again railroaded with its bevel facing posteriorly. Successful intubation was confirmed by bilateral equal air entry and chest excursion, absence of gastric insufflations sound, and “sine” wave pattern on capnography. Anesthesia was maintained with O2:N2O (50:50), sevoflurane 2%–3%, and vecuronium bromide in the dose of 0.025 mg/kg. The patients were mechanically ventilated to keep the end-tidal carbon dioxide (EtCO2) between 35 and 45 mmHg and oxygen saturation (SpO2) 100%. After 15 min of ET intubation, all patients were given tramadol 1 mg/kg IV. At the end of surgery, the residual neuromuscular blockade was reversed with neostigmine 50 μg/kg and glycopyrrolate 10 μg/kg IV and trachea was extubated after fulfillment of the criteria for extubation. SGA and ventilating bougie were observed for blood staining or presence of any gastric content at the end of the procedure, number of attempts and time for insertion for SGA, ventilating bougie, and ETT were noted. Maximum 3 attempts were allowed for each device. SGA's insertion time was defined as the time from the removal of the facemask to the time ventilation was established through the SGA with EtCO2 confirmation. Ventilating bougie insertion time was defined as the time from disconnection of circuit for bougie insertion to the time of confirmed air entry through bougie. ETT insertion time was defined as the time from disconnection of the circuit for tracheal tube insertion to the time ventilation was established through the ETT with EtCO2 confirmation. Total intubation time was defined as the time from the removal of facemask for SGA insertion to the time when ventilation was established through ETT. If more than three attempts were required to insert either SGA, ventilating bougie or ETT, conventional laryngoscopy was done and trachea was intubated and these patients were excluded from the study. To prevent bias, SGAs were inserted by a qualified anesthesiologist with 10 years' experience.
Vital parameters such as heart rate, SBP, DBP, SpO2, and EtCO2 were observed at baseline, each time after dexmedetomidine injection, induction, SGA insertion, ventilating bougie insertion, ET intubation, and then, 3, 5, 7, 10, and 15 min after ETT insertion. Patients were observed for complications such as hypoxia, bradycardia, airway trauma, sore throat, and hoarseness of voice. The complications and their treatment were defined as following: hypoxia was defined as fall in SpO2 below 90% at any time during the study. Bradycardia was defined as fall in heart rate below 60/min or decrease in heart rate >20% from baseline level. Hypotension was defined as fall in blood pressure <80/60 or decrease in blood pressure >20% from baseline level.
Sample size estimation was performed using software “MedCalc” for Windows, version 12.5 (MedCalc Software, Ostend, Belgium), from the parameter “ first attempt success rate of SGA insertion” from the reference study.[8] First attempt success rate for i-Gel was 54% and LMA Classic was 86%. Taking alpha error as 0.05, beta error as 0.20, and ratio of cases to control as 1, the calculated minimum sample size was 29 in each group. Observed data were entered into Microsoft Excel 2010 and Statistical analyses were performed using MedCalc for Windows, version 12.7.5.0 (MedCalc Software, Ostend, Belgium). The results of the study were tabulated and statistically compared in the group and among the two groups. Qualitative data were analyzed using “Chi-square test” and continuous data were analyzed using paired and unpaired t-test.
Results
Demographic data were comparable in both the groups [Table 1]. Table 2 shows that the number of attempts for insertion of SGA, ventilating bougie and ETT were similar in the two groups. After 2nd attempt, success rate for insertion of SGA was 93.1% in both the groups. After 2nd attempt, success rate for insertion of ventilating bougie was 100% in Group I and 96.5% in Group C (P = 0.72). ETT was inserted at 1st attempt in all the patients in Group I. Only one patient in Group C required 2nd attempt for ETT insertion. Mean insertion time for SGA was significantly less in Group I than in Group C whereas mean insertion time for ventilating bougie was longer in Group I than in Group C. Mean insertion time for ETT was however comparable in Group I and Group C. Total intubation time was significantly less in Group I as compared to Group C [Table 3]. Baseline vital parameters were comparable in both the groups. No significant change in vital parameters was observed throughout the study on inter- and intra-group comparisons [Figures 1 and 2]. Airway trauma was noted in two patients in Group I and three patients in Group C. In Group C, tube impingement occurred in one patient.
Table 1.
Demographic data
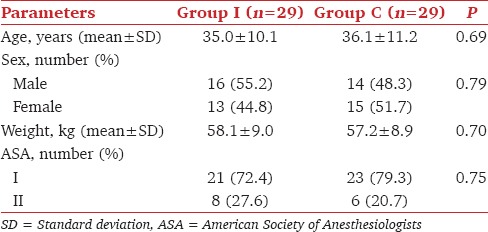
Table 2.
Number of attempts for device insertion and tracheal intubation
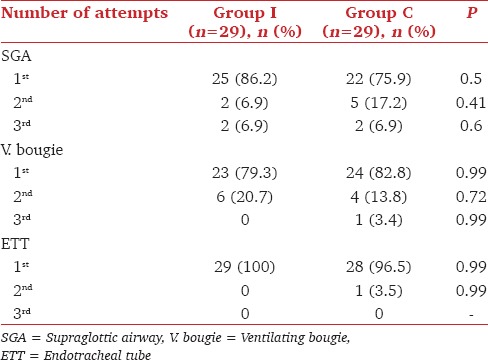
Table 3.
Time of insertion of various devices
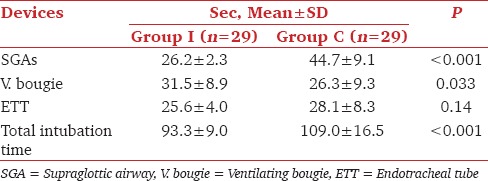
Figure 1.
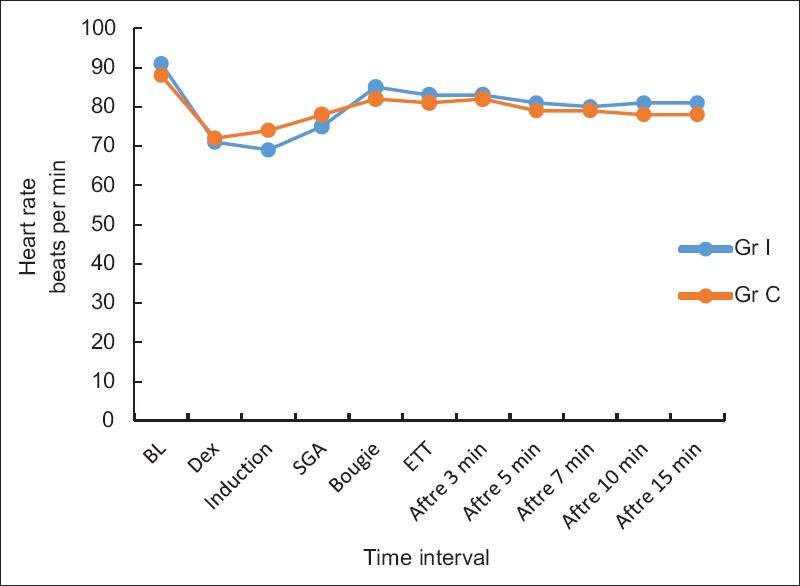
Heart rate
Figure 2.
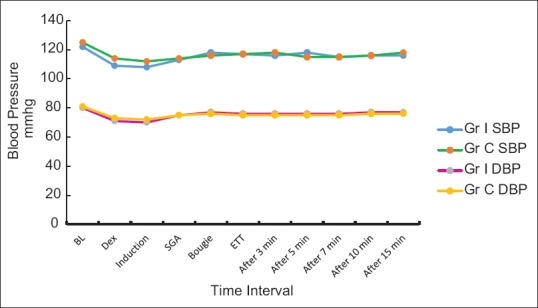
Blood pressure changes
Discussion
Our result shows that both the SGAs are compatible as a conduit for tracheal intubation using ventilating bougie. It is desirable to secure a definitive airway to achieve aims of airway protection and oxygenation both. Charters and O'Sullivan defined the concept of a dedicated airway, i.e., 'An upper airway device dedicated to the maintenance of airway patency while other major airway interventions are anticipated or in process.' It should be compatible with spontaneous and controlled ventilation.[9]
The laryngeal mask airway and other SGAs are now commonly used in the management of a failed intubation as dedicated airways.[10] The plan B of the Difficult Airway Society guidelines recommends the use of either classic or ILMA to maintain the airway, and then, to intubate through the selected device using a fiberoptic endoscope.[11,12] The major issues with the ILMA and fiberoptic endoscope are that they are costly and not available in most of setups. Furthermore, the experience of anesthesiologists with these devices is limited. Hence, simple and less costly SGAs such as LMA Classic and i-Gel are more popular among the anesthesiologists. Different SGAs have been used as a conduit for tracheal intubation using fiberoptic endoscope or blindly or using tracheal tube introducers.[1]
The LMA Classic was not primarily designed as a conduit for tracheal intubation and has noticeable limitations, e.g., aperture bars, when employed for this purpose. Despite these limitations, and in view of its role as an airway rescue device, on occasion, it is still relied on as a conduit for tracheal intubation.[5,13] i-Gel is a single-use device with a noninflatable cuff, made of thermoplastic elastomer. i-Gel has been reported both as an airway rescue device and as conduit for fiberoptic intubation in predicted difficult airways.[14,15] Compared to LMA Classic, i-Gel's design features a shorter and wider stem together with the absence of aperture bars which might facilitate fiberoptic intubation through this device.[16]
LMA Classic size 3 and 4 allow the passage of 6 mm ETT. i-Gel No. 3 and 4 allow passage of 6 and 7 mm ETT, respectively. These tube sizes may not be always appropriate for a particular patient. Under such circumstances, tracheal tube introducers such as AIC and gum-elastic bougie (ventilating or nonventilating) guide wire exchange catheter; and fiberoptic endoscope can all be used to facilitate tracheal intubation through SGAs.[1,8,17,18] Ventilating bougie is a flexible tracheal tube introducer. It is 65 cm long and external diameter is 5 mm. It has got central lumen and two ports for oxygenation, which maintains oxygenation if at all hypoxia occurs. Its distal tip is angled anteriorly at 38° which facilitates its insertion into the trachea. Proper alignment of SGA to the glottis and angulated (38°) tip of ventilating bougie facilitates the insertion of ventilating bougie into the trachea. Furthermore, in i-Gel and LMA Classic, the lumen is not being shared by gastric channel, so that bougie can be easily negotiated if both are well aligned to laryngeal inlet.
Although the overall success rate for insertion was comparable in the two SGAs the mean insertion time for i-Gel was less compared to LMA Classic. This is probably because of the fact that less flexible stem of the i-Gel makes insertion easier and there is no need for cuff inflation.[19] Previous studies have also reported comparable overall success rate for the two devices with less insertion time for i-Gel.[16,20,21] Jankiraman et al. on the other hand found higher 1st and 2nd attempt success rate for LMA Classic compared to i-Gel and concluded that with the current sizing recommendations, i-Gel is not an acceptable alternative to LMA Classic.[8]
Despite the presence of “aperture bars” in LMA Classic, we neither encountered any difficulty in passing ventilating bougie nor there was any incidence of breakage of aperture bars. Furthermore, the time required for insertion of ventilating bougie through LMA Classic was surprisingly less compare to i-Gel. No reason can be put forward for this less time in our study. Probably, it requires further evaluation of these two devices as a conduit for tracheal intubation. Unfortunately, we could not find any study comparing insertion time for ventilating bougie through LMA. ETT insertion time was comparable in both the groups. Allison and McCrory reported successful gum-elastic bougie aided blind tracheal intubation through LMA Classic in 21 out of 25 cases.[17] Successful use of LMA Classic as a conduit for gum-elastic bougie aided blind tracheal intubation has also been mentioned by other studies.[22,23,24] Atherton used LMA Classic as a conduit for ventilation exchange bougie - fiber optic laryngoscope assisted ET intubation. They reported 100% success rate and no difficulty was reported in railroading of ETT over ventilation exchange bougie.[25] Similarly, two studies compared i-Gel and LMA Fastrach as a conduit for tracheal intubation and concluded that blind tracheal intubation can be achieved using i-Gel as a conduit with a comparable first attempt success rate to the LMA Fastrach.[26,27] Total intubation time was less for i-Gel compared to LMA Classic in the present study. One manikin study reported significantly lesser intubation time with i-Gel compared to LMA Classic due to features of i-Gel, wider stem and absence of aperture bars; however, in our study, it was mainly due to lesser time required for i-Gel insertion.[15] Here, it is to mention that none of the patients were excluded from our study because of failure to insert either SGAs or ventilating bougie or ETT.
There was a significant fall in heart rate, SBP, and DBP following dexmedetomidine and induction of anesthesia in both groups, but intergroup comparison did not see any difference. These changes were within normal limits and did not require any treatment. Dexmedetomidine is a highly selective α2 adrenergic agonist with sedative, anxiolytic, analgesic, and sympatholytic effects. It has been shown to diminish airway and circulatory responses during intubation and extubation.[28,29,30,31] Various studies comparing the effect of dexmedetomidine–propofol and fentanyl–propofol for LMA insertion concluded that dexmedetomidine provides satisfactory conditions for successful LMA insertion while preserving hemodynamic stability and respiratory functions better than fentanyl.[30,32] We did not come across any article where hemodynamic parameters have been assessed while using SGAs as conduit for tracheal intubation. ETT impingement was noted in one patient in LMA Classic group. This problem was overcome by rotating the tube 90° counterclockwise before insertion. That allowed the bevel to face posteriorly, and hence, decreased the chances of tube impingement on glottic structure.[26,27] Airway trauma was noted in two patients in i-Gel group and three patients in LMA Classic group, i.e., SGAs were blood stained. After fixation of ETT, direct laryngoscopy was done and minor bleeding from the pharyngeal wall was managed by applying compression with gauge piece for 5–7 min. The limitations of our study are not using fiberoptic endoscope which would have been better as it helps in visualizing proper alignment of SGAs, placement of ventilating bougie and ETT into the trachea.[3,8,14] Furthermore, the use ILMA would have been better as a conduit for tracheal intubation.
Conclusions
Thus, from our study, we conclude that i-Gel and LMA Classic both can be used as a conduit for tracheal intubation using ventilating bougie with stable hemodynamic and with minimal complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wong DT, Yang JJ, Mak HY, Jagannathan N. Use of intubation introducers through a supraglottic airway to facilitate tracheal intubation: A brief review. Can J Anaesth. 2012;59:704–15. doi: 10.1007/s12630-012-9714-8. [DOI] [PubMed] [Google Scholar]
- 2.Arndt GA, Topp J, Hannah J, McDowell TS, Lesko A. Intubation via the LMA using a Cook retrograde intubation kit. Can J Anaesth. 1998;45:257–60. doi: 10.1007/BF03012912. [DOI] [PubMed] [Google Scholar]
- 3.Blair E J, Mihai R, Cook TM. Tracheal intubation via the classic and ProSeal laryngeal mask airways: A manikin study using the aintree intubating catheter. Anaesthesia. 2007;62:385–7. doi: 10.1111/j.1365-2044.2007.04994.x. [DOI] [PubMed] [Google Scholar]
- 4.Farag E, Bhandary S, Deungria M, Zura A, Seif J, Borkowski R, et al. Successful emergent reintubation using the aintree intubation catheter and a laryngeal mask airway. Minerva Anestesiol. 2010;76:148–50. [PubMed] [Google Scholar]
- 5.Heath ML, Allagain J. Intubation through the laryngeal mask. A technique for unexpected difficult intubation. Anaesthesia. 1991;46:545–8. doi: 10.1111/j.1365-2044.1991.tb09652.x. [DOI] [PubMed] [Google Scholar]
- 6.I-Gel User Guide. 7th ed. Wokingham, UK: Intersurgical Ltd; 2009. Available from: www.intersurgical.com/products/airway-management/i-gel-supraglottic-airway . [Google Scholar]
- 7.Verghese C. Anaesthesiology News Guide to Airway Management. MCMAHON PUBLISHING; 2010. Laryngeal mask airway devices: Three maneuvers for any clinical situation; pp. 15–6. Available from: http://kidocs.org/wp.content/uploads/2014/11/3Maneuvers_ANGAM10_WM.pdf . [Google Scholar]
- 8.Janakiraman C, Chethan DB, Wilkes AR, Stacey MR, Goodwin N. A randomised crossover trial comparing the I-gel supraglottic airway and classic laryngeal mask airway. Anaesthesia. 2009;64:674–8. doi: 10.1111/j.1365-2044.2009.05898.x. [DOI] [PubMed] [Google Scholar]
- 9.Charters P, O'Sullivan E. The 'dedicated airway': A review of the concept and an update of current practice. Anaesthesia. 1999;54:778–86. doi: 10.1046/j.1365-2044.1999.00888.x. [DOI] [PubMed] [Google Scholar]
- 10.Pandit JJ, MacLachlan K, Dravid RM, Popat MT. Comparison of times to achieve tracheal intubation with three techniques using the laryngeal or intubating laryngeal mask airway. Anaesthesia. 2002;57:128–32. doi: 10.1046/j.0003-2409.2001.02401.x. [DOI] [PubMed] [Google Scholar]
- 11.J. J. Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59:675, 94. doi: 10.1111/j.1365-2044.2004.03831.x. [DOI] [PubMed] [Google Scholar]
- 12.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 13.Alberts ANJ. The LMA Classic ™ as a conduit for tracheal intubation in adult patients: A review and practical guide. S Afr J Anaesth Analg. 2014;20:77–88. [Google Scholar]
- 14.Bhandari G, Shahi KS, Bhakuni R. A comparative study of tracheal intubation through I-Gel® and intubating laryngeal mask airway. Peoples J Sci Res. 2013;6:24–9. [Google Scholar]
- 15.Michalek P, Hodgkinson P, Donaldson W. Fiberoptic intubation through an I-gel supraglottic airway in two patients with predicted difficult airway and intellectual disability. Anesth Analg. 2008;106:1501–4. doi: 10.1213/ane.0b013e31816f22f6. [DOI] [PubMed] [Google Scholar]
- 16.de Lloyd L, Hodzovic I, Voisey S, Wilkes AR, Latto IP. Comparison of fibrescope guided intubation via the classic laryngeal mask airway and I-gel in a manikin. Anaesthesia. 2010;65:36–43. doi: 10.1111/j.1365-2044.2009.06155.x. [DOI] [PubMed] [Google Scholar]
- 17.Allisona MC, croryAllison A, McCrory J. Tracheal placement of a gum elastic bougie using the laryngeal mask airways. Anaesthesia. 1990;45:419–20. doi: 10.1111/j.1365-2044.1990.tb14809.x. [DOI] [PubMed] [Google Scholar]
- 18.Heard AM, Lacquiere DA, Riley RH. Manikin study of fibreoptic-guided intubation through the classic laryngeal mask airway with the aintree intubating catheter vs the intubating laryngeal mask airway in the simulated difficult airway. Anaesthesia. 2010;65:841–7. doi: 10.1111/j.1365-2044.2010.06412.x. [DOI] [PubMed] [Google Scholar]
- 19.Polat R, Aydin GB, Ergil J, Sayin M, Kokulu T, Öztürk I. Comparison of the I-gel™ and the laryngeal mask airway Classic™ in terms of clinical performance. Rev Bras Anestesiol. 2015;65:343–8. doi: 10.1016/j.bjan.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Helmy AM, Atef HM, El-Taher EM, Henidak AM. Comparative study between I-gel, a new supraglottic airway device, and classical laryngeal mask airway in anesthetized spontaneously ventilated patients. Saudi J Anaesth. 2010;4:131–6. doi: 10.4103/1658-354X.71250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh J, Yadav MK, Marahatta SB, Shrestha BL. Randomized crossover comparison of the laryngeal mask airway classic with I-gel laryngeal mask airway in the management of difficult airway in post burn neck contracture patients. Indian J Anaesth. 2012;56:348–52. doi: 10.4103/0019-5049.100815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chadd GD, Ackers JW, Bailey PM. Difficult intubation aided by the laryngeal mask airway. Anaesthesia. 1989;44:1015. doi: 10.1111/j.1365-2044.1989.tb09244.x. [DOI] [PubMed] [Google Scholar]
- 23.Murdoch JA. Emergency tracheal intubation using a gum elastic bougie through a laryngeal mask airway. Anaesthesia. 2005;60:626–7. doi: 10.1111/j.1365-2044.2005.04248.x. [DOI] [PubMed] [Google Scholar]
- 24.Sarma J. Intubation using an LMA and gum elastic bougie. Anesth Analg. 2006;102:975. doi: 10.1213/01.ANE.0000199177.76054.4B. [DOI] [PubMed] [Google Scholar]
- 25.Atherton DPL, O'Sullivan E, Lowe D, Charters P. A ventilation-exchange bougie for fibreoptic intubations with the laryngeal mask airway. Anaesthesia. 1996;51:1123–6. doi: 10.1111/j.1365-2044.1996.tb15047.x. [DOI] [PubMed] [Google Scholar]
- 26.Halwagi AE, Massicotte N, Lallo A, Gauthier A, Boudreault D, Ruel M, et al. Tracheal intubation through the I-gel™ supraglottic airway versus the LMA Fastrach™: A randomized controlled trial. Anesth Analg. 2012;114:152–6. doi: 10.1213/ANE.0b013e318236f438. [DOI] [PubMed] [Google Scholar]
- 27.Kapoor S, Jethava DD, Gupta P, Jethava D, Kumar A. Comparison of supraglottic devices I-gel(®) and LMA Fastrach(®) as conduit for endotracheal intubation. Indian J Anaesth. 2014;58:397–402. doi: 10.4103/0019-5049.138969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guler G, Akın A, Tosun Z, Eskıtascoglu E, Mızrak A, Boyac A. Single-dose dexmedetomidine attenuates airway and circulatory reflexes during extubation. Acta Anaesthesiol Scand. 2005;49:1088–91. doi: 10.1111/j.1399-6576.2005.00780.x. [DOI] [PubMed] [Google Scholar]
- 29.Maroof M, Khan RM, Jain D, Ashraf M. Dexmedetomidine is a useful adjunct for awake intubation. Can J Anaesth. 2005;52:776–7. doi: 10.1007/BF03016576. [DOI] [PubMed] [Google Scholar]
- 30.Uzümcügil F, Canbay O, Celebi N, Karagoz AH, Ozgen S. Comparison of dexmedetomidine-propofol vs. fentanyl-propofol for laryngeal mask insertion. Eur J Anaesthesiol. 2008;25:675–80. doi: 10.1017/S0265021508004213. [DOI] [PubMed] [Google Scholar]
- 31.Mondal S, Ghosh S, Bhattacharya S, Choudhury B, Mallick S, Prasad A. Comparison between dexmedetomidine and fentanyl on intubation conditions during awake fiberoptic bronchoscopy: A randomized double-blind prospective study. J Anaesthesiol Clin Pharmacol. 2015;31:212–6. doi: 10.4103/0970-9185.155151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashwini Halebid Ramaswamy, Safiya I, ShaikhRamaswamy AH, Shaikh SI. Comparison of dexmedetomidine-propofol versus fentanyl-propofol for insertion of laryngeal mask airway. J Anaesthesiol Clin Pharmacol. 2015;31:217–20. doi: 10.4103/0970-9185.155152. [DOI] [PMC free article] [PubMed] [Google Scholar]


