Abstract
Background and Aims:
Increasing number of pediatric ambulatory surgeries are being carried out in general anesthesia using supraglottic airways (SGAs). Literature comparing sevoflurane and desflurane for the maintenance of SGA-based anesthesia is limited. Hence, we planned this prospective randomized study to compare the maintenance, emergence and recovery characteristics of sevoflurane and desflurane for pediatric ambulatory surgery.
Material and Methods:
Sixty children aged 6 months to 6 years posted for short surgical procedures were enrolled into the study. Anesthesia was induced with intravenous propofol (maximum 4 mg/kg), SGA was inserted, and children were randomized to receive sevoflurane or desflurane for the maintenance of anesthesia. No muscle relaxants were administered, and all children received caudal block and rectal paracetamol suppository. Demographic data, perioperative hemodynamics and adverse events, emergence and recovery characteristics, postoperative pain, and emergence agitation (EA) were recorded. Data were analyzed using SPSS (version 16.0, IBM Corporation, Armonk, New York, USA). P < 0.05 was considered statistically significant.
Results:
Demography, perioperative hemodynamics, and duration of inhalational anesthesia were comparable between two groups. There were no respiratory adverse events in either group during maintenance. Time to awakening and time to removal of SGA were shorter with desflurane (5.3 ± 1.4 and 5.8 ± 1.3 min) than sevoflurane (9.1 ± 2.4 and 10.0 ± 1.6 min) (P < 0.0001). Recovery (steward recovery score = 6) was faster with desflurane (18 ± 8.4 min) than sevoflurane (45.3 ± 9.7 min) (P < 0.001). The incidence of EA was 16.7% with desflurane and 10% with sevoflurane (P = 0.226).
Conclusion:
Desflurane provides faster emergence and recovery in comparison to sevoflurane when used for the maintenance of anesthesia through SGA in children. Both sevoflurane and desflurane can be safely used in children for lower abdominal surgeries.
Keywords: Desflurane, emergence, pediatric, recovery, sevoflurane
Introduction
Desflurane, an inhalational agent with the least blood gas solubility coefficient and hence fastest recovery has been widely used for the maintenance of general anesthesia for ambulatory surgery in adults. However, desflurane has not been widely used in pediatric population because of its two main concerns: its pungent smell and irritant nature making it unsuitable for its use for induction of general anesthesia; the possibility of airway complications such as a cough, laryngospasm, and breath holding, especially when the airway is unprotected.[1] This concern is of real importance considering the fact that more and more pediatric ambulatory surgeries are now being carried out in general anesthesia without muscle relaxation using supraglottic airway (SGA). Unlike adults, there is a dearth of literature comparing various inhalational agents for maintenance of anesthesia using SGA in children.[2,3] Therefore, we carried out the prospective observational study to compare maintenance, emergence and recovery characteristics of sevoflurane and desflurane in pediatric ambulatory surgery following propofol induction.
Material and Methods
In a prospective, randomized study, 60 children between 6 months and 6 years of either sex and American Society of Anesthesiologists Grade I and II undergoing lower abdominal surgeries lasting 30–60 min under general anesthesia with SGA were enrolled. Patients with reactive airway disease, respiratory tract infections, significant systemic diseases, sleep apnea, developmental delay, or psychological disorders were excluded. Institutional review board approval was obtained and trial was registered with Clinical Trial Registry India (CTRI/2015/02/005570 - Registered on: 24/02/2015).
A detailed history was obtained and thorough physical examination was carried out. Informed consent was obtained from the parents/legal guardians of the children meeting the inclusion criteria. Selected patients were randomly assigned to one of the two anesthetic treatment groups of 30 each (Group S - sevoflurane and Group D - desflurane) according to a computer-generated random numbers table.
Children's behavior was assessed at the time of separation from parents by using a separation scale 1–4 (1 = excellent [separates easily], 2 = good [not clinging, whimpers, calm with reassurance], 3 = fair [not clinging, crying, will not calm or quiet], 4 = poor [crying, clinging to parent]). A separation score of 1 or 2 was considered satisfactory, whereas a score of 3 or 4 was considered unsatisfactory.
All patients were premedicated with intravenous glycopyrrolate 4 mcg/kg and midazolam 0.02 mg/kg before induction of general anesthesia. Anesthesia was induced with intravenous propofol (in titrated dosed to achieve adequate depth with the maximum dose not exceeding 4 mg/kg). A SGA device was then inserted. The patient was connected to a circle absorber system and general anesthesia was maintained with oxygen + nitrous oxide at the flow rate of 1 L each. Sevoflurane or desflurane was added as maintenance inhalational agent according to the randomization. The concentration (volume percent) of sevoflurane (3%–1.5%) or desflurane (8%–3%) was adjusted as per the clinical indicators of the depth of anesthesia (hemodynamic alteration and movement in response to stimulus). The depth of anesthesia was adequate enough to allow pressure assist control ventilation without administration of neuromuscular blocker. Continuous intraoperative monitoring included heart rate, Noninvasive blood pressure, SpO2, and end-tidal CO2.
Analgesia was provided by local anesthetics in caudal block. All patients received per rectal paracetamol suppository (30 mg/kg). Hemodynamic changes at the skin incision served as the test of analgesic adequacy of the regional block. The block was considered inadequate if the child's heart rate increased by more than 20% within 60 s of skin incision or if there was movement in response to surgical stimulus. Only the children judged to have an adequate block were continued in the study. Children with a heart rate response to skin incision received supplemental opioid analgesia with intravenous fentanyl 1–2 mcg/kg and were not included in the study.
Hemodynamic parameters following SGA insertion and before starting the maintenance inhalational agent were considered as baseline parameters and any change more than 20% from the baseline was considered as hemodynamic adverse event and was recorded. Increasing the concentration of inhalational agent (sevoflurane >3% and desflurane >8%) was not permitted and the need of additional intravenous propofol to maintain adequate depth of anesthesia was also noted.
Maintenance anesthetics were discontinued at the end of surgery. Duration of inhalation anesthesia (from the start to discontinuation of sevoflurane/desflurane) was noted. Once the patient showed good respiratory attempts, he/she was allowed to breathe spontaneously with 100% oxygen. SGA was removed when the child demonstrated complete emergence from anesthesia by displaying a regular respiration, facial grimacing, swallowing, gag reflex, and purposeful movement.
Emergence parameters such as time to regular breathing, time to awakening (i.e., eye-opening, purposeful movements), and time to removal of SGA were recorded after discontinuing the volatile anesthetics.
During the maintenance and emergence phase, patients were observed for the adverse airway events like signs of airways obstruction (paradoxical chest or abdominal movements, sternal retraction), breath holding, excessive secretions, coughing on the SGA, hiccups, and desaturation (SpO2< 94%).
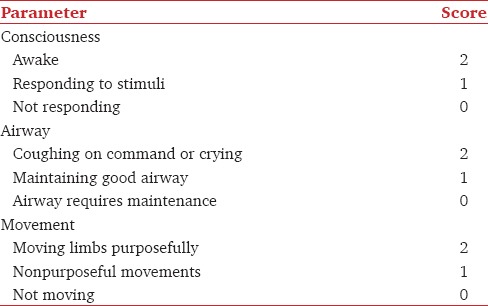
In the postanesthesia care unit (PACU), an observer who was unaware of the inhalational agent used recorded following parameters every 10 min: (A) Steward's recovery score [Table 1]; (B) degree of agitation using the 5-point agitation score (1 - Asleep, 2 - Awake, calm and cooperative 3 - Crying, requires consoling, 4 - Irritable, restless, screaming and inconsolable, 5 - Combative, disoriented); (C) Postoperative pain by FLACC score (each of the five categories [F] Face, [L] Legs, [A] Activity, [C] Cry, [C] Consolability was scored from 0 to 2, which results in a score between 0 and 10).
Table 1.
Steward's simplified postanesthesia recovery score
Children with severe postoperative agitation (score ≥4 for 5 min) or significant pain (FLACC score ≥4) received intravenous fentanyl 0.25 mcg/kg. Repeat dose of fentanyl was allowed with the lock period of 15 min with the maximum total dose of 1 mcg/kg. Children who received rescue dose of fentanyl were not discharged for minimum 45 min after the last dose. Recovery time (defined by the time of discontinuing the anesthetics until steward recovery score of 6) was also recorded.
Statistical analysis
Assuming the mean difference in time to awakening of 3 min between the two groups, standard deviation (SD) of 4 min,[2] with the power of 80% and alpha error of 0.05, Power and Sample Size Calculation software (version 3.1.2, 2014, Vanderbilt University School of Medicine, Nashville, TN 37203-1741, USA) determined the requirement of 29 patients for each group. Parametric data were reported as mean ± SD and was analyzed by two-sided Student's unpaired t-test. Categorical data were reported as number and percent (n, %) and analyzed using the Pearson's Chi-square test/Fischer exact test. P < 0.05 was considered as statistically significant.
Results
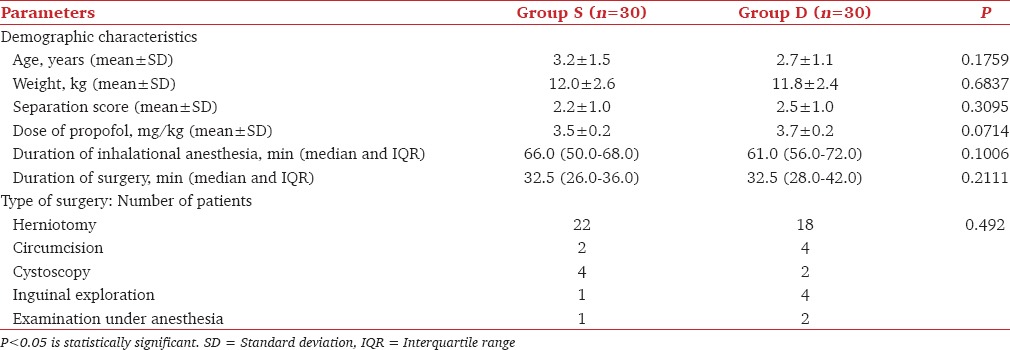
Patients in Group S and Group D had comparable demographic profile [Table 2]. Mean separation score and total dose of propofol required for the induction of general anesthesia was also comparable between the two groups [Table 2]. As the data were not normally distributed for the duration of inhalational anesthesia, median and interquartile range were calculated and was analyzed using Mann–Whitney U-test [Table 2].
Table 2.
Demographic data and type of surgery
Intraoperative hemodynamics were comparable between the two groups with mean arterial pressure and heart rate maintained within ±20% of baseline values. None of our patients had major hemodynamic or respiratory adverse events during maintenance and emergence.
Emergence characteristics like time to regular breathing, time to awakening and time to removal of SGA were shorter with desflurane than sevoflurane maintenance anesthesia (P < 0.0001) [Table 3]. Patients who received Desflurane attained the recovery endpoints (steward recovery score of 6) much early (P < 0.0001) as compared to those who received Sevoflurane [Table 3].
Table 3.
Emergence and recovery characteristics
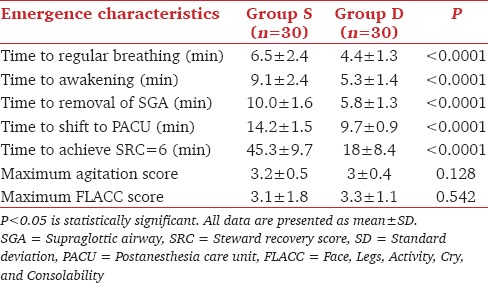
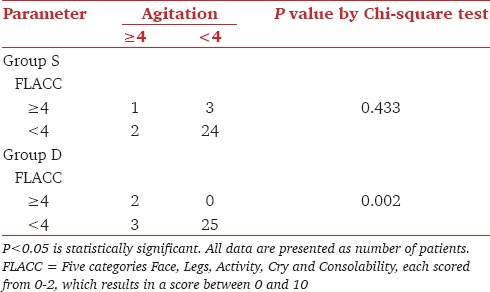
There was no significant difference in the maximum pain scores between the two groups (P = 0.921). Four out of 30 patients in Group S and 2 out of 30 patients in Group D required rescue analgesia in the postanesthesia recovery room (P = 0.671). The incidence of emergence agitation (EA) (agitation score ≥4) was comparable in two groups, 10% (3 out of 30 patients) in group S and 16.7% (5 out of 30 patients) in group D (P = 0.226). There was no significant difference in the mean agitation score [Table 3] between the two groups (P = 0.128). The relation between high pain scores (FLACC ≥4) and agitation is shown in Table 4. A positive correlation (P = 0.000) was observed between higher FLACC scores and agitation in Group D (Pearson correlation coefficient = 0.745). However, no such correlation (P = 0.414) was observed in group S (Pearson correlation coefficient = 0.169). Four (13%) patients who received desflurane had cough in the PACU, compared to none in sevoflurane group (P = 0.112).
Table 4.
Correlation between pain and agitation
Discussion
Increasing number of procedures in the pediatric ambulatory setup is now being carried out using SGA-based anesthesia without using muscle relaxants. In a historical cohort study of 14,153 children, Oofuvong et al. noticed that after adjusting for other risk factors, hazard ratio of intraoperative respiratory adverse events was higher with assisted ventilation through face mask and laryngeal mask airway (LMA) as compared to endotracheal tube and they concluded that anesthesiologists should be more careful, especially when certain airway devices or desflurane are used.[3] The ideal anesthetic for pediatric ambulatory surgeries should provide good quality maintenance with no or minimal airway and hemodynamic adverse events. It should also provide rapid emergence and smooth recovery.[4] Few short-acting agents available are propofol, sevoflurane, and desflurane. Intravenous propofol provides rapid clear recovery and can be used for both induction and maintenance of general anesthesia. However, maintenance with propofol is not economical, considering the cost of infusion pumps, extension lines, syringes, etc.[5] Therefore, inhalational anesthesia still remains the most commonly used method for maintenance of general anesthesia in children.
Sevoflurane and desflurane have increasingly become more popular because of their low blood-gas and blood-tissue solubility, leading to rapid recovery after general anesthesia.[6,7] Sevoflurane is well known to cause EA. Recent Cochrane review revealed that desflurane has relative risk of EA of 1.46 with 95% confidence interval of 0.92–2.31 compared to sevoflurane.[8]
Although there are studies comparing sevoflurane and desflurane anesthesia in children, the results are varying and lack uniformity. In the majority of the studies, muscle relaxant was used[9,10,11,12,13,14,15] which would cause difficulty in assessing the effect of inhalational agent on the airway (breath holding, cough, and laryngospasm). In addition, it would increase the overall cost and delay the discharge after the short surgical procedures. Therefore, we avoided the use of muscle relaxants in our study.
Desflurane cannot be used for induction of anesthesia. Most authors had used halothane[9] or sevoflurane[12,14,15,16] for induction of anesthesia and then randomized patients to receive sevoflurane or desflurane for maintenance of anesthesia. In that case, one may not get true picture about emergence characteristics and incidence of agitation, etc. We used propofol as induction agent to avoid such bias. As such for children who accept insertion of intravenous cannula, propofol is a preferred anesthetic induction agent. For maintenance, inhalational anesthetic agent is used so that extra cost for setting up propofol infusion is not needed.
We, therefore, planned this study to compare the maintenance and emergence characteristics of sevoflurane and desflurane in children who receive SGA-based general anesthesia without using muscle relaxants. Only after SGA was inserted, sevoflurane or desflurane was started for maintenance anesthesia in the respective groups.
We found desflurane as satisfactory as sevoflurane for the maintenance of general anesthesia as both the groups did not have any major respiratory and hemodynamic adverse event. Lerman et al.[17] reported higher incidence (P < 0.006) of major adverse events, when LMA was removed in deep anesthesia (15%) as compared to that in awake state (5%). We did not find any adverse event during emergence possibly because we removed SGA in an awake state.
Emergence characteristics like time to regular breathing, time to awakening and time to extubation was faster with desflurane than sevoflurane when used for maintenance of general anesthesia. As a result of the lower solubility of desflurane in blood and lean tissues, it is expected to find faster emergence with desflurane than sevoflurane.[18,19] Similar results were also obtained by Welborn et al.[9] and Cohen et al.[12] in their studies. Macario et al.[20] in their meta-analysis also reported similar observations. This faster emergence with desflurane is really important in busy pediatric ambulatory setups.
Time required for recovery after desflurane (18 ± 8.3 min) was 40% of the time for recovery after sevoflurane (45 ± 9.7 min). Our results were comparable to Mayer et al.[21] who reported faster recovery after desflurane anesthesia (36.2 ± 9.9 min) than after sevoflurane anesthesia (39.3 ± 8.1 min). They compared Aldrete score ≥9 as criteria for discharge from PACU.
Child's behavior and state of anxiety before surgery is an important factor in affecting the incidence of postoperative EA.[22,23] We chose to check and record the separation score as a marker for preoperative state of anxiety in children. Both groups in our study had similar preoperative anxiety [Table 2]. We noted 10% and 18% incidence of EA in Group S and Group D, respectively. Singh et al.[15] used inhalational anesthetic (1–1.2 minimum alveolar concentration [MAC]) for maintenance of anesthesia and reported a higher incidence of EA with sevoflurane (40%) than with desflurane (28%). The higher incidence of EA in their study was probably because of relatively longer anesthetic duration (80–90 min). Furthermore, they used sevoflurane (8 volume %) for the induction of anesthesia in both the groups which is known to increase the incidence of EA as reported by Mayer et al.[21] We found lower and comparable incidence of EA after sevoflurane (10%) and desflurane (18%) maintenance probably because we used intravenous propofol for induction of general anesthesia. Also, the mean duration of inhalational anesthetic in our study was shorter [Table 2]. Valley et al.[16] reported less frequent agitation in children receiving sevoflurane (25%) than with desflurane (43%). The incidence of EA reported by various authors is variable and this could possibly be because of different criteria and different scoring system adapted to assess EA and multifactorial etiology of EA.[24]
Although, Cravero et al.[25] had shown that EA can also occur in pain-free children, pain can still be an important contributing and confounding factor which would interfere in assessing EA and could bias our results.[8] Hence, we tried to study any correlation between severe pain (FLACC score ≥4) and occurrence of agitation [Table 4]. A positive correlation was seen between higher FLACC scores and agitation among children, who received desflurane (P = 0.000).
White et al.[2] in their study observed a higher incidence of perioperative coughing in the desflurane group than in sevoflurane group. However, they reported that incidence of coughing during the actual administration of the volatile anesthetics (i.e., the maintenance period) did not differ between the two groups. Similar observations were made in our study, 4 (13%) patients from Group D versus none from group S had cough in the recovery period. Although this is not statistically significant (P = 0.112), it may not be acceptable after certain procedures like ophthalmic' procedures, etc., where it can affect the surgical outcome.
There were certain other limitations to our study. There was a possibility of the bias since the anesthesiologist administering the inhalational agent was not blinded. Monitoring the MAC of inhalational agents was not available. However, the attending anesthesiologist was instructed to adjust the concentration of sevoflurane (3%–1.5%) or desflurane (8%–3%) as per the clinical indicators (movement in response to stimulus and hemodynamic alterations). This was possible because we did not use neuromuscular blockade. MAC monitoring would have been all the more necessary if we would have used balanced anesthesia with muscle relaxants in our study. Although the scores used to assess EA and pain are easy and have been used in many studies, these are very subjective with overlapping variables. Hence, the results obtained in our study cannot be extrapolated in children younger than 6 months where such confounding variables can be too many.
Conclusion
Desflurane provides faster emergence and recovery in comparison to sevoflurane when used for maintenance of anesthesia through SGA in children. Both sevoflurane and desflurane can be safely used in children for lower abdominal surgeries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Klock PA, Jr, Czeslick EG, Klafta JM, Ovassapian A, Moss J. The effect of sevoflurane and desflurane on upper airway reactivity. Anesthesiology. 2001;94:963–7. doi: 10.1097/00000542-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 2.White PF, Tang J, Wender RH, Yumul R, Stokes OJ, Sloninsky A, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: The effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009;109:387–93. doi: 10.1213/ane.0b013e3181adc21a. [DOI] [PubMed] [Google Scholar]
- 3.Oofuvong M, Geater AF, Chongsuvivatwong V, Pattaravit N, Nuanjun K. Risk over time and risk factors of intraoperative respiratory events: A historical cohort study of 14,153 children. BMC Anesthesiol. 2014;14:13. doi: 10.1186/1471-2253-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eger EI, White PF, Bogetz MS. Clinical and economic factors important to anaesthetic choice for day-case surgery. Pharmacoeconomics. 2000;17:245–62. doi: 10.2165/00019053-200017030-00003. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg MK, Bridge P, Brown M. Cost comparison: A desflurane- versus a propofol-based general anesthetic technique. Anesth Analg. 1994;79:852–5. doi: 10.1213/00000539-199411000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Lerman J. Inhalational anesthetics. Paediatr Anaesth. 2004;14:380–3. doi: 10.1111/j.1460-9592.2004.01334.x. [DOI] [PubMed] [Google Scholar]
- 7.Murat I. Is there a place for desflurane in paediatric anaesthesia? Paediatr Anaesth. 2002;12:663–4. doi: 10.1046/j.1460-9592.2002.00794.x. [DOI] [PubMed] [Google Scholar]
- 8.Costi D, Cyna AM, Ahmed S, Stephens K, Strickland P, Ellwood J, et al. Effects of sevoflurane versus other general anaesthesia on emergence agitation in children. Cochrane Database Syst Rev. 2014:CD007084. doi: 10.1002/14651858.CD007084.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996;83:917–20. doi: 10.1097/00000539-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Uzun S, Tuncer S, Tavlan A, Reisli R, Sarkilar G, Ökesli S. Comparison of maintenance and recovery characteristics of desflurane and sevoflurane in children. Turk J Anaesthesiol Reanim. 2003;31:415–21. [Google Scholar]
- 11.Demirbilek S, Togal T, Cicek M, Aslan U, Sizanli E, Ersoy MO. Effects of fentanyl on the incidence of emergence agitation in children receiving desflurane or sevoflurane anaesthesia. Eur J Anaesthesiol. 2004;21:538–42. doi: 10.1017/s0265021504007069. [DOI] [PubMed] [Google Scholar]
- 12.Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg. 2002;94:1178–81. doi: 10.1097/00000539-200205000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Jindal R, Kumra VP, Narani KK, Sood J. Comparison of maintenance and emergence characteristics after desflurane or sevoflurane in outpatient anaesthesia. Indian J Anaesth. 2011;55:36–42. doi: 10.4103/0019-5049.76604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta P, Rath GP, Prabhakar H, Bithal PK. Comparison between sevoflurane and desflurane on emergence and recovery characteristics of children undergoing surgery for spinal dysraphism. Indian J Anaesth. 2015;59:482–7. doi: 10.4103/0019-5049.162985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh R, Kharbanda M, Sood N, Mahajan V, Chatterji C. Comparative evaluation of incidence of emergence agitation and post-operative recovery profile in paediatric patients after isoflurane, sevoflurane and desflurane anaesthesia. Indian J Anaesth. 2012;56:156–61. doi: 10.4103/0019-5049.96325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valley RD, Freid EB, Bailey AG, Kopp VJ, Georges LS, Fletcher J, et al. Tracheal extubation of deeply anesthetized pediatric patients: A comparison of desflurane and sevoflurane. Anesth Analg. 2003;96:1320–4. doi: 10.1213/01.ANE.0000058844.77403.16. [DOI] [PubMed] [Google Scholar]
- 17.Lerman J, Hammer GB, Verghese S, Ehlers M, Khalil SN, Betts E, et al. Airway responses to desflurane during maintenance of anesthesia and recovery in children with laryngeal mask airways. Paediatr Anaesth. 2010;20:495–505. doi: 10.1111/j.1460-9592.2010.03305.x. [DOI] [PubMed] [Google Scholar]
- 18.Yasuda N, Lockhart SH, Eger EI, 2nd, Weiskopf RB, Johnson BH, Freire BA, et al. Kinetics of desflurane, isoflurane, and halothane in humans. Anesthesiology. 1991;74:489–98. doi: 10.1097/00000542-199103000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Steward A, Allott PR, Cowles AL, Mapleson WW. Solubility coefficients for inhaled anaesthetics for water, oil and biological media. Br J Anaesth. 1973;45:282–93. doi: 10.1093/bja/45.3.282. [DOI] [PubMed] [Google Scholar]
- 20.Macario A, Dexter F, Lubarsky D. Meta-analysis of trials comparing postoperative recovery after anesthesia with sevoflurane or desflurane. Am J Health Syst Pharm. 2005;62:63–8. doi: 10.1093/ajhp/62.1.63. [DOI] [PubMed] [Google Scholar]
- 21.Mayer J, Boldt J, Röhm KD, Scheuermann K, Suttner SW. Desflurane anesthesia after sevoflurane inhaled induction reduces severity of emergence agitation in children undergoing minor ear-nose-throat surgery compared with sevoflurane induction and maintenance. Anesth Analg. 2006;102:400–4. doi: 10.1213/01.ane.0000189561.44016.99. [DOI] [PubMed] [Google Scholar]
- 22.Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. 2004;99:1648–54. doi: 10.1213/01.ANE.0000136471.36680.97. [DOI] [PubMed] [Google Scholar]
- 23.Aguilera IM, Patel D, Meakin GH, Masterson J. Perioperative anxiety and postoperative behavioural disturbances in children undergoing intravenous or inhalation induction of anaesthesia. Paediatr Anaesth. 2003;13:501–7. doi: 10.1046/j.1460-9592.2003.01002.x. [DOI] [PubMed] [Google Scholar]
- 24.Silva LM, Braz LG, Módolo NS. Emergence agitation in pediatric anesthesia: Current features. J Pediatr (Rio J) 2008;84:107–13. doi: 10.2223/JPED.1763. [DOI] [PubMed] [Google Scholar]
- 25.Cravero J, Surgenor S, Whalen K. Emergence agitation in paediatric patients after sevoflurane anaesthesia and no surgery: A comparison with halothane. Paediatr Anaesth. 2000;10:419–24. doi: 10.1046/j.1460-9592.2000.00560.x. [DOI] [PubMed] [Google Scholar]


