Abstract
Introduction
The aim of this study was to find an ideal method for the application of a transrectal ultrasound-guided prostate biopsy (TRUS-Bx) without deteriorating patient comfort.
Material and methods
TRUS-Bx was applied in a total of 93 patients. Taking the application method into consideration, these patients were divided into three groups, each consisting of 31 patients. Methods applied for pain control in the different groups were compared (groups 1, 2 and 3). Age, prostate specific antigen (PSA), prostate volume, cancer detection rate, re-biopsy consent ratio, complication rates, visual analog scale (VAS), and International Index of Erectile Function (IIEF-5) scores were compared among the groups.
Results
Age, PSA, prostate volume, cancer detection rate, and fever complication rate were not statistically different between the three groups. However, a statistically significant difference was detected among the groups for the VAS measured during and after TRUS-Bx, re-biopsy consent ratio, and hematuria (p <0.001, p <0.001, p <0.001, and p = 0.027, respectively). There was no detected difference in pre-operation IIEF-5 scores, but the difference in IIEF-5 scores in the first month after the operation was significant (p = 0.116, p = 0.024, respectively).
Conclusions
Anal dilatation after the application of intrarectal topical anesthetic to provide anesthesia during TRUS-Bx and giving lidocaine hydrochloride with epinephrine for periprostatic nerve blockage (PNB) is a successful and effective method to maintain patient comfort, especially as it relates to pain control and sexual function. Anal dilatation seems to minimize any pain that may occur due to probe transition, and adding epinephrine as a vasopressor to the anesthetic agent chosen during the operation will be rather helpful for hemostasis control and pain that results from the needle.
Keywords: transrectal ultrasound guided prostate biopsy, pain, sexual functions, local anesthetic, prostate cancer
INTRODUCTION
Prostate cancer is the most common extracutaneous cancer in elderly males (>70) in Europe and the second most common cause of cancer-related deaths in Australia. Therefore, it constitutes a source of concern in developed countries where the population of elderly males is higher [1, 2]. Biopsies guided by serum Prostate Specific Antigen (PSA) levels, Digital Rectal Examination (DRE) and Transrectal Ultrasonography (TRUS) are routinely used for scanning, detection and diagnosis of prostate cancer [1, 3]. Transrectal ultrasound-guided prostate biopsy (TRUS-Bx) is the method mostly preferred due to its short application time, it not requiring special equipment and re-usability of the equipment used, and it being cheaper and easier to learn. Despite the developments in prostate imaging, TRUS-Bx is used as the standard procedure for prostate cancer diagnosis [3, 4].
This operation is an invasive intervention which is painful, disturbing and can cause complications such as rectal bleeding and infection [5, 6].
The European Association of Urology (EAU) has recommended that a prostate biopsy should be accompanied by TRUS and that sample sites should be bilateral from apex to base, as far posterior and lateral as possible in the peripheral gland with an average of 10 and 12 core biopsies [1]. In studies, prostate biopsy was reported to be a painful procedure for the patients [7, 8]. Thus, providing effective pain control in patients who will have a prostate biopsy is important. Researchers recommended different analgesic methods such as sedation and general anesthesia, periprostatic lidocaine injection, intrarectal lidocaine instillation and use of oral or rectal non-steroidal anti-inflammatories [9, 10]. However, there is not yet a clear consensus on the ideal method in this regard. Another controversial issue is that TRUS-Bx may have a negative impact on erectile function.
In current literature, studies have investigated the effect of TRUS-Bx on erectile dysfunction (ED). Many studies have shown that these post-biopsy effects occur over a short period of time and are transient. However, recent studies have reported that some men could still have ED at 6 months after TRUS-Bx [11].
With these facts in mind, we aimed to find an ideal method that provides maximum patient comfort during TRUS-Bx as well as minimal effect on erectile function after the intervention.
MATERIAL AND METHODS
We retrospectively evaluated the records of all patients (n = 154) who underwent prostate biopsy from November 2014 and June 2016.
The indications for biopsy were the elevation of prostate-specific antigen (PSA) and/or abnormal digital rectal examination findings. Patients who systemically used effective oral, intravenous and intramuscular analgesic drugs before the biopsy, those that had chronic pain and patients with lack of file information were excluded from the study.
We divided patients into 3 group according to the physician's preference of analgesia-anesthesia technique during the biopsy. A total of 93 patients were included in the study.
In group 1 (n = 31), intrarectal 10 cc 2% lidocaine hydrochloride gel was applied as standard care 10 minutes before the biopsy. Digital anal dilatation (DAD) and periprostatic nerve block (PNB) were not performed.
In group 2 (n = 31), 10 minutes after the application of intrarectal 10 cc 2% lidocaine hydrochloride gel DAD was applied by the physician. Additionally, a periprostatic nerve block (PNB) was applied by injecting a total of 80 mg (left neurovascular bundle (NVB): 40 mg, right NVB: 40 mg) 2% lidocaine hydrochloride (Jetokain Simplex®, Adeka Pharmaceutical Industry, Turkey).
In group 3 (n = 31), 10 minutes after the application of 10 cc intrarectal 2% lidocaine hydrochloride gel, the physician applied both DAD and periprostatic nerve block by injecting a total of 160 mg (left NVB: 80 mg, right NVB: 80 mg) of 2% lidocaine hydrochloride + epinephrine (Jetokain Simplex®, Adeka Pharmaceutical Industry, Turkey).
Prostate dimensions of all patients were measured before the operation. 18 Gauge needles were used during the procedure. In all patients, 12 core biopsies, six from the right and six from the left, were taken guided by an Acuson S2000, 4–9 Mhz transrectal probe (Siemens, Erlangen, Germany).
Pain severity of the patients was assessed by the visual analog scale (VAS), in the middle of the biopsy procedure and at the fifth minute post-biopsy. Sexual function was evaluated by the International Index of Erectile Function (IIEF-5) score before and a month after the operation.
When the patients were seen after the first month, they were asked whether they would have a biopsy again if required.
We also investigated age, PSA, prostate volume, and possible complication such as fever (≥38°), burning sensation during urination, and gross or low degree macroscopic hematuria related to the procedure. Gross hematuria was defined as dark red and grumous urination accompanied by symptomatic irritative findings, while low degree macroscopic hematuria was defined as colour of urine between light and dark pink without any symptomatic findings in the patient.
Statistical analysis
SPSS 16 statistical software was used for data processing. Counting data were showed as x ±s, whereas grade data were displayed as median (inter-quartile range). Nonparametric analysis included Mann-Whitney test and Kruskal-Wallis H test were used to compare pain scores. Chi-square (χ2) test was used to compare the rates of complications at inter-subgroup or intra-subgroup levels. The significant value was set at p <0.05.
RESULTS
Demographic, clinical, and pathological data from three groups are shown in Table 1. Age, PSA, prostate volume, cancer detection rate, and fever complication rate were not statistically different between the three groups (p = 0.501, p = 0.353, p = 0.446, p = 0.948, p = 0.654, p = 0.982 respectively). Difference in IIEF-5 scores in the first month after the operation was significant.
Table 1.
Demographic, clinical and pathological datas from three groups
| Group 1 | Group 2 | Group 3 | p value | |
|---|---|---|---|---|
| Age | 64.2 ±4.1 | 63.7 ±4.6 | 65.2 ±4.2 | 0.501 |
| PSA (ng/ml) | 8.64 ±3.2 | 7.37 ±2.9 | 9.65 ±3 | 0.353 |
| Prostate | ||||
| volume (ml) | 48.93 ±11.1 | 54.4 ±8.6 | 51.5 ±9.1 | 0.446 |
| Cancer | 8/31 | 8/31 | 9/31 | |
| detection rate (%) | (25.8%) | (25.8%) | (29.03%) | 0.948 |
| Gleason score (mean) | 6.8 ±0.8 | 7.2 ±0.9 | 7.12 ±0.8 | 0.654 |
| Fever | 1/31 (3.22%) | 1/31 (3.22%) | 0 | 0.982 |
| Gross rectal bleeding | 0 | 0 | 0 | |
| Gross Hematuria | 0 | 0 | 0 | |
| Low degree macroscopichematuria | 7 (22.5%) | 4 (12.9%) | 2 (6.4%) | 0.027 |
PSA – prostate specific antigen
The VAS measured for groups 1, 2, and 3 during TRUS-Bx were 6.14 ±1.1, 3.34 ±0.75, and 0.43 ±0.32, respectively, while the VAS measured after TRUS-Bx were 5.97 ±1, 3.02 ±.69, and 0.36 ±0.28, respectively. The re-biopsy consent ratios (%) for these groups were 29.03, 83.3, and 93.5, respectively. A statistically significant difference was detected between the groups for the VAS measured during and after TRUS-Bx and the re-biopsy consent ratio (p <0.001, p <0.001, and p <0.001, respectively). For group 3, VAS values were found to be quite low, and the re-biopsy consent ratio was found to be very high.
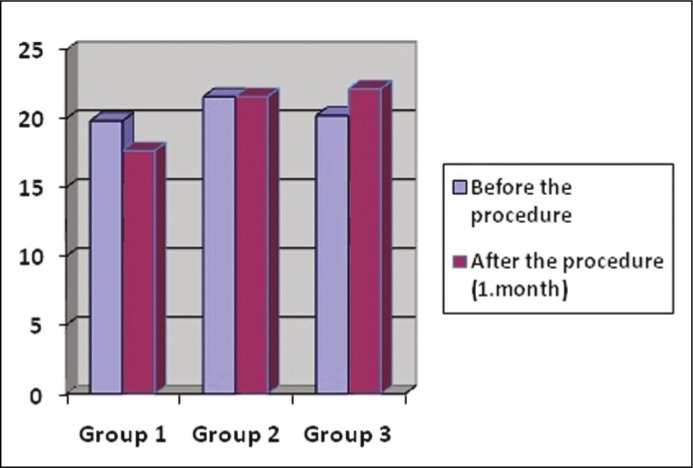
For groups 1, 2 and 3, the IIEF-5 scores before the procedure were 19.83 ±3.3, 21.59 ±3.4, and 20.23 ±3.1, respectively (p = 0.116); the IIEF-5 scores in the first month after the procedure were 17.67 ±2.1, 21.61 ±2.6, and 22.16 ±3.6, respectively (p = 0.024). There was no detected difference for the pre-operation IIEF-5 score, but the difference in the first month after the procedure was significant. IIEF-5 and VAS scores and re-biopsy consent ratios for the patients can be seen in Table 2. The IIEF-5 score decreased 10.8% in the first month in the first group and increased 9.5% in the third group. A graphic containing the IIEF-5 scores of the groups before and after the procedure can be seen in Figure 1.
Table 2.
IIEF and VAS scores and re-biopsy consent ratios for the patients
| Group 1 | Group 2 | Group 3 | p value | |
|---|---|---|---|---|
| VAS measured during TRUS-Bx | 6.14 ±1.1 | 3.34 ±0.75 | 0.43 ±0.32 | <0.001 |
| VAS measured after TRUS-Bx | 5.97 ±1 | 3.02 ±0.69 | 0.36 ±0.28 | <0.001 |
| Re-biopsy consent ratio (%) | 29.03 | 83.3 | 93.5 | <0.001 |
| Before procedure IIEF-5score | 19.83 ±3.3 | 21.59 ±3.4 | 20.23 ±3.1 | 0.116 |
| After procedure IIEF-5 score (1st month) | 17.67 ±2.1 | 21.61 ±2.6 | 22.16 ±3.6 | 0.024 |
VAS – visual analog scale, IIEF – International Index of Erectile Function, TRUS-Bx – transrectal ultrasound guided prostate biopsy
Figure 1.
The graphic showing the IIEF scores of the groups before and after the TRUS-Bx.
In two patients, we observed a 39° fever and 100.000 colony/CFU Escherichia coli in the urine culture after the biopsy. The patients were treated with suitable IV antibiotics and hydration after hospitalization. There was no statistically significant difference between the groups in terms of fever complication.
We did not observe any gross rectal bleeding and hematuria after biopsy in any patient among the groups. No patients returned with rectal bleeding after being discharged. We observed mild macroscopic hematuria not harming the general condition and not causing active complaint in a total of 19 patients (15%) (seven patients in group 1 (22.5%), four patients in group 2 (12.9%) and two patients in group 3 (6.4%). A significant difference was observed in mild hematuria among the groups (p = 0.027). Duration of mild macroscopic hematuria was measured at approximately 33.4 hours and it recovered without any intervention in all patients.
DISCUSSION
TRUS-Bx is the golden standard for cancer diagnosis. TRUS guided systematic sextant prostate biopsy technique was defined in 1989 for the first time and was developed and partially modified in time and has become a standard procedure in most clinics today [12, 13]. Even though TRUS-Bx is tolerated well in many patients, most of them complain about the pain. There are two reasons for the pain felt during the biopsy. One of these reasons is the pain and feeling of strain occurring when the ultrasound probe is passing through the anus and the other is the pain occurring during the entrance of the biopsy needle to stroma by penetrating the prostate capsule [9]. Rodriguez et al. reported that 25% of the cases that had TRUS-Bx felt a moderate or severe level of discomfort and 19% wouldn't accept non-anesthetized re-biopsy [8]. Bastide et al. measured the procedure-related discomfort ratio as 80% even though the biopsy quadrant number is below six in most of the patients who have unanaesthetized TRUS-Bx [14]. Thus, it is extremely important to provide analgesia/anesthesia during TRUS-Bx for the comfort of the patient and being able to produce multiple biopsies during the operation. Methods such as intrarectal ice application, intrarectal lidocaine gel instillation, oral or rectal non-steroidal anti-inflammatory drugs, sedation and general anesthesia, and periprostatic nerve block (PNB) were used for anesthesia [9, 10, 15].
Periprostatic nerve block has generally become a preferable method of anesthesia due to positive results such as low side effect profile and efficiency in pain control [16–19]. Peripheral nerve block provides temporary anesthesia/analgesia by giving local anesthetic around peripheral nerves around each neurovascular bundle. Adrenaline (epinephrine) is usually added to local anesthetics as a vasopressor. As the absorption from the place of application will be slow with the addition of vasopressor in local anesthetics, the effect of short and moderately effective local anesthetics lasts longer and blood concentrations increase slowly. Vasoconstrictor effects are also helpful in hemostasis [20, 21]. Thus, we think that in the third group which was given intrarectal topical anesthesia (2% lidocaine gel 10 ml +160 mg 2% lidocaine +0.05 mg epinephrine) in this study, a high dose of local anesthetic and vasopressor application may have provided an effective and long nerve block.
In literature, only the isolated efficiency of anal dilatation in relieving pain was not measured. But the first painful step during TRUS-Bx is placing the ultrasound probe into the anal channel. Inserting the ultrasound probe directly in an unrelaxed anal sphincter causes mechanical stretching, local inflammation in the anal area and severe pain. In different studies, it was reported that applications such as rectal digital examination, rectal enema dilating and intrarectal local analgesic gel application significantly decreases the pain and discomfort felt during probe insertion [8, 16, 17]. We introduced the ultrasound probe into the anal channel after digital anal dilatation to provide pain control in the present study. It was interesting that VAS measurement was close to zero in group 3. When compared with other groups, a statistically significant difference was detected in pain (p <0.001). Even though the method applied in Group 2 was similar to that in group 3, VAS was measured as 3.34 due to the use of a lower dose of lidocaine (40 mg for each NVB). This value was rather high as compared to Group 3. According to this study, active dose application during PNB and presence of vasopressor (epinephrine) in addition to the anesthetic agent used, were found to be important for a comfortable and painless operation. Lidocaine gel application as local anesthetic before the operation, digital anal dilatation before inserting the ultrasound probe, and a PNB with double the amount of lidocaine (total of 160 mg) containing epinephrine, caused the patients to be comfortable during the operation, pain scores to be close to zero and enabled us to reach better results in the third group.
Lunacek et al. measured VAS as 1 during the TRUS-Bx operation made by applying PNB anesthesia with 60-mg lidocaine suppository+ a total of 10 ml 2% lidocaine (200 mg). They used an 18 G needle during the operation [19]. It was observed that these results were rather close to our study. We applied a total of 160 mg lidocaine hydrochloride, 80 mg per each neurovascular bundle and used an 18 G needle during the operation. The difference in our study was digital anal dilatation after intrarectal topical lidocaine application before TRUS-Bx and use of an epinephrine containing anesthetic agent. These differences probably provided pain values close to zero during the operation.
Hızlı et al. used an Iliohypogastric Nerve Block and intrarectal prilocaine-lidocaine cream together for TRUS-Bx andmeasured the VAS as 0.5 during the probe entrance and 1.8 during the biopsy. The complication ratio was measured as 35% in this operation-related combined group, most of which were rectal bleeding and hematuria-related [5]. Hematuria ratios in the third group in our study were measured as 6.4%, which was significantly low. We think that this low ratio may be due to the vasoconstrictor effect of the epinephrine present, in addition to the lidocaine given during PNB.
Murray et al. measured IIEF scores, of the patients who had TRUS-Bx, on the 1st, 4th and 12th weeks and a decrease, of 20% in the fourth week and 24% in the twelfth week after the biopsy, were detected [22]. IIEF scores may decrease in these patients due to the anxiety created by the increased cancer risk, especially in the patients for whom TRUS-Bx was planned. Anxiety accompanied especially by the pain during TRUS-Bx and complications such as hemospermia, hematuria, rectal bleeding and fever, which may be observed after the operation, may negatively affect erectile function. While IIEF scores decreased 10.8% in the first group in our study, it was increased by 9.5% in group 3. It was considered that this situation was related to the low pain level during the operation and the low side effect profile observed after the procedure. We also think that the lack of malignity in 74.2% of the patients in group 3 may have contributed to the increase in IIEF score compared to pre-operation.
Our study has rather low VAS scores – close to zero – when compared to studies in the literature and the discomfort ratio and re-biopsy consent ratios of the patients were found to be high. A rather low side effect profile and positive effect in IIEF scores were also detected. Thus, we think that anal dilatation after intracranial topical anesthetic application to provide anesthesia during TRUS-Bx and giving lidocaine hydrochloride+epinephrine for PNB (minimum 160 mg) is a successful and effective method to manage pain control and sexual functions.
CONCLUSIONS
Anal dilatation after the application of intrarectal topical anesthetic to provide anesthesia during TRUS-Bx and giving lidocaine hydrochloride with epinephrine for periprostatic nerve blockage (PNB) is a successful and effective method to maintain patient comfort, especially as it relates to pain control and sexual function. Anal dilatation seems to minimize any pain that may occur due to probe transition, and adding epinephrine as a vasopressor to the anesthetic agent chosen during the operation will be helpful for hemostasis control and pain thatresult from the needle. Also, the negative effect of TRUS-Bx operations where pain and anxiety are minimalized will decrease. Prospective randomized controlled trials involving only placebo, anal dilatation, and intrarectal topical anesthetic groups will be more useful in this regard.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Mottet N, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG Guidelines on Prostate CancerPart 1: Screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–629. doi: 10.1016/j.eururo.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Cabarkapa S, Perera M, McGrath S, Lawrentschuk N. Prostate cancer screening with prostate specific antigen: A guide to the guidelines. Prostate Int. 2016;4:125–129. doi: 10.1016/j.prnil.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Çömez K, Bozkurt O, Mungan MU. Prostate Biopsy 2014: TRUS, MRI/TRUS Fusion? Transrectal? Transperineal? Bull Urooncol. 2015;14:128–135. [Google Scholar]
- 4.Fabiani A, Servi L, Filosa A, et al. May ultrasound probe size influence pain perception of needle piercing during transrectal prostate biopsy? A prospective evaluation. Arch Ital Urol Androl. 2016;88:223–227. doi: 10.4081/aiua.2016.3.223. [DOI] [PubMed] [Google Scholar]
- 5.Hizli F, Argun G, Özkul F, et al. Novel approach for pain control in patients undergoing prostate biopsy: iliohypogastric nerve block with or without topical application of prilocaine-lidocaine: arandomized controlled trial. Urol J. 2015;12:2014–2019. [PubMed] [Google Scholar]
- 6.Zengin K, Tanık S, Albayrak S, Bakırtaş H, İmamoglu MA, Bozok MG. The comparison of two different anesthetical methods in transrectal ultrasound guided biopsy. J Clin Anal Med. 2015;6:601–603. [Google Scholar]
- 7.Bolat D, Aydın ME, Günlüsoy B, et al. Evaluation of the relationship between pathology results and pain scores in patients who underwent transrectal ultrasound-guided prostate. Bull Urooncol. 2016;15:86–89. [Google Scholar]
- 8.Rodríguez LV, Terrisa MK. Risks and complications of transrectal ultrasound. Curr Opin Urol. 2000;10:111–116. doi: 10.1097/00042307-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Izol V, Soyupak B, Seydaoglu G, Aridogan IA, Tansug Z. Three different techniques for administering analgesia during transrectal ultrasound-guided prostate biopsy: a comparative study. Int Braz J Urol. 2012;38:122–128. doi: 10.1590/s1677-55382012000100017. [DOI] [PubMed] [Google Scholar]
- 10.Chang SS, Alberts G, Wells N, Smith JA, Jr, Cookson MS. Intrarectal lidocaine during transrectal prostate biopsy: results of a prospective double-blind randomized trial. J Urol. 2001;166:2178–2180. doi: 10.1016/s0022-5347(05)65529-2. [DOI] [PubMed] [Google Scholar]
- 11.Tuncel A, Toprak U, Balci M, et al. Impact of transrectal prostate needle biopsy on erectile function: results of power Doppler ultrasonography of the prostate. Kaohsiung J Med Sci. 2014;30:194–199. doi: 10.1016/j.kjms.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoon BI, Shin TS, Cho HJ, et al. Is it effective to perform two more prostate biopsies according toprostate-specific antigen level and prostate volume in detecting prostate cancer? Prospective study of 10-core and 12-core prostate biopsy. Urol J. 2012;9:491–497. [PubMed] [Google Scholar]
- 13.Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71–74. doi: 10.1016/s0022-5347(17)38664-0. [DOI] [PubMed] [Google Scholar]
- 14.Bastide C, Lechevallier E, Eghazarian C, Ortega JC, Coulange C. Tolerance of pain during transrectal ultrasound-guided biopsy of the prostate: risk factors. Prostate Cancer Prostatic Dis. 2003;6:239–241. doi: 10.1038/sj.pcan.4500664. [DOI] [PubMed] [Google Scholar]
- 15.Çaliskan B, Mutlu N. Intrarectal ice application prior to transrectal prostate biopsy: a prospective randomised trial accessing pain and collateral effects. Int Braz J Urol. 2015;41:101–109. doi: 10.1590/S1677-5538.IBJU.2015.01.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giannarini G, Autorino R, Valent F, et al. Combination of perianal-intrarectal lidocaine- prilocainecream and periprostatic nerve block for pain control during transrectal ultrasound guided prostate biopsy: a randomized, controlled trial. J Urol. 2009;181:585–591. doi: 10.1016/j.juro.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Nazir B. Pain during transrectal ultrasound-guided prostate biopsy and the role of periprostatic nerve block: what radiologists should know. Korean J Radiol. 2014;15:543–553. doi: 10.3348/kjr.2014.15.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Temiz MZ, Kandirali E, Colakerol A, Tuken A, Semercioz A. Local anesthesia type affects cancer detection rate in transrectal ultrasound guided prostate biopsy. Int Braz J Urol. 2015;41:859–863. doi: 10.1590/S1677-5538.IBJU.2014.0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lunacek A, Mrstik C, Simon J, et al. Combination of lidocaine suppository and periprostatic nerve block during transrectal prostate biopsy: a prospective randomized trial. Int J Urol. 2014;21:1126–1130. doi: 10.1111/iju.12542. [DOI] [PubMed] [Google Scholar]
- 20.Berde CB, Strichartz GR. Local Anesthetics: Anesthesia. In: Miller RD, editor. 5th. Phileldelphia: Churchill Livingstone; 2000. pp. 491–521. [Google Scholar]
- 21.Hollman MW, Durieux ME, Graf BM. Novel local anaesthetics and novel indications for local anaesthetics. Curr Opin Anaesthesiol. 2001;14:741–749. doi: 10.1097/00001503-200112000-00023. [DOI] [PubMed] [Google Scholar]
- 22.Murray KS, Bailey J, Zuk K, Lopez-Corona E, Thrasher JB. A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy. BJU Int. 2015;116:190–195. doi: 10.1111/bju.13002. [DOI] [PubMed] [Google Scholar]