Abstract
CONTEXT:
Shortage of physicians particularly in specialty levels is considered as an important issue in Iran health system. Thus, in an uncertain environment, long-term planning is required for health professionals as a basic priority on a national scale.
AIMS:
This study aimed to estimate the number of required neurosurgeons using system dynamic modeling.
SETTING AND DESIGN:
System dynamic modeling was applied to predict the gap between stock and number of required neurosurgeons in Iran up to 2020.
SUBJECTS AND METHODS:
A supply and demand simulation model was constructed for neurosurgeons using system dynamic approach. The demand model included epidemiological, demographic, and utilization variables along with supply model-incorporated current stock of neurosurgeons and flow variables such as attrition, migration, and retirement rate.
STATISTICAL ANALYSIS USED:
Data were obtained from various governmental databases and were analyzed by Vensim PLE Version 3.0 to address the flow of health professionals, clinical infrastructure, population demographics, and disease prevalence during the time.
RESULTS:
It was forecasted that shortage in number of neurosurgeons would disappear at 2020. The most dominant determinants on predicted number of neurosurgeons were the prevalence of neurosurgical diseases, the rate for service utilization, and medical capacity of the region.
CONCLUSIONS:
Shortage of neurosurgeons in some areas of the country relates to maldistribution of the specialists. Accordingly, there is a need to reconsider the allocation system for health professionals within the country instead of increasing the overall number of acceptance quota in training positions.
Keywords: Demand, forecast, shortage, supply, system dynamics
Introduction
To have a well-functioning health-care system, it is inevitable to have adequate number with proper performance of health workforce.[1] Shortage of health professionals whether for poor distribution or insufficient admission quota in the profession has become a significant problem in many countries.[2] To resolve such problems, planning for health professionals has got a great importance.[3,4] The aim is to ensure that health professionals are available and ready to provide services in “the right place at the right time with the right skills.”[5,6]
Effective planning in this field requires an accurate forecasting of supply and demand for health human resources. There are several approaches including need-, demand-, and supply-based modeling which apply different methods such as regression models, simulation, and Markov chains to project the supply and demand for health workforce.[7,8,9] Although the diversity of methods, a desirable one should contain dynamic variables both in supply and demand side of the model.[7] It is highly recommended to include epidemiological, demographic, and supply-based determinants into the forecasting model to ensure the comprehensiveness of the model.[10]
System dynamics (SD) has such ability besides reflecting the changing environment over time. The method was introduced by Forrester in 1956 for planning business and commercial activities and now is widely used in policy-making of the health system.[11] Since then, many studies have used SD modeling to predict the number of required health workforce.[12,13,14,15,16] SD is a “computer-based approach to policy analysis which can be applied to deal with dynamic problems arising in social, economic, managerial, or ecological systems.”[11] This approach has the ability to consider a comprehensive set of dynamic variables in workforce forecasting and to take into account both quantitative and qualitative variables. The model is also useful in evidence-based policy-making for workforce supply and demand by forecasting purposes in long periods of time and responding to “what-if” scenarios. Despite the importance, no study has applied such an approach to estimate supply and demand for health providers in Iran.
Both lack of adequate number of physicians and maldistribution of professionals within the country cause an improper situation which worsens some areas’ condition to meet basic health objectives of the community. Based on the governmental policies in health system, one of the most dominant priorities was to expand specialty positions and admission capacities to improve the situation.[17] In addition, to deal with such challenges, policymakers have acknowledged that number of specialists must be determined in accordance with health needs of the population.[18] Thus, planners and decisionmakers in Iran's health system got a tendency to design an evidence-based model with a comprehensive approach and dynamic nature which is able to estimate number of required health professionals for a long-term period of time.
Shortage of neurosurgeons has been reported in some areas of the country causing serious problems, especially for regions with high rate of road accidents or considerable prevalence of brain and spine diseases.[17,18] A report by Iran Ministry of Health and Medical Education (MOHME) in 2011 announced that the greatest shortage in health human professionals belonged to neurosurgeons.[19] Since then, considerable efforts have been dedicated by MOHME to distinguish between shortage of absolute number of specialists within the country and maldistribution among regions.[18] In fact, increased number of patients diagnosed as a result of accidents and other traumas highlighted the need for a scientific and logical model to predict number of required neurosurgeons in a national level. In achieving the purpose also to permit the evaluation of different policy effects (residency admission quota, retirement age, medical services utilization rate, and patient population) on supply and demand of neurosurgeons, we constructed a system dynamic model. The method was applied to predict the gap between current and required number of neurosurgeons up to 2020.
Subjects and Methods
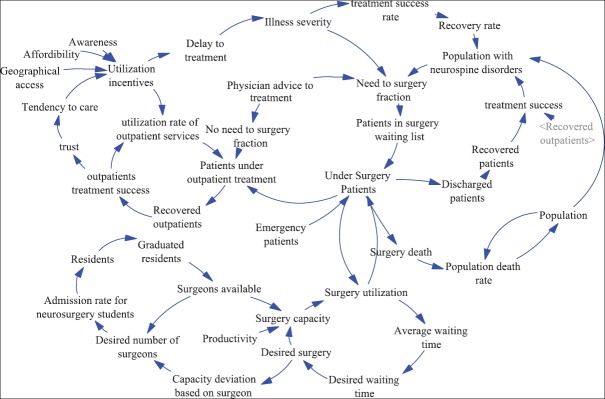
As the health human resource market is a dynamic system comprised of several influencing factors, we implemented SD model in Vensim PLE Version 3.0 (Ventana systems Inc, UK), Ventana Systems UK Ltd to address the flow of health professionals, clinical infrastructure, population demographics, and disease prevalence during the time.[12] The base year for projection was 2015 and simulation was conducted up to 2020. Model is able to acknowledge the procedures that opt to improve the system or resolve its problems. To represent the most important determinants of the system and their causal relations in SD model, causal loop diagram was used [Figure 1].
Figure 1.
Causal loop diagram of neurosurgeons workforce model
Model was consisted of two main components: the supply and demand submodels. In the supply side, the flow of neurosurgery residents from training until retirement was depicted beginning with admission to the university as a specialty resident. Some scenarios were considered to examine their effects on physicians’ supply including the admission quota to neurosurgery, acceptance rate in preboard examination, number of available residencies, number of active neurosurgeons, retirement age, and migration rate both into the specialty and out of the specialty. We used sensitivity analysis to estimate the impact of uncertainties in above variables on the forecast analysis results.
The demand side of the model focused on estimating the number of neurosurgeons required to meet population health needs. To this purpose, conceptual framework of the model was based on three main elements: population size and demographic characteristics, health needs, and service utilization rate corresponding to neurosurgery specialty. By multiplying the components, number of neurosurgery services required to meet health needs of Iran population would be achieved. The prevalence of neurospine disorders or injuries (including trauma, stroke, tumors of the brain and spinal cord, and degenerative disorders of the spine) results in the need for neurosurgery services in a specific time duration. In demand submodel, the parameters which manipulated to make alternative scenarios were population growth or ageing, change in prevalence of neurospine disorders representing population health needs, variation in level of neurosurgery service utilization, and clinical infrastructure capacity in community. The ability of the model to assess the effect of various scenarios turned it into an instrument that allowed managers and decisionmakers in Ministry of Health to improve the situation to an optimal level.
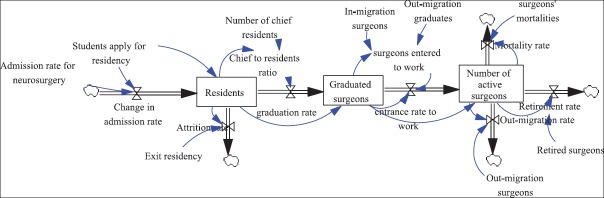
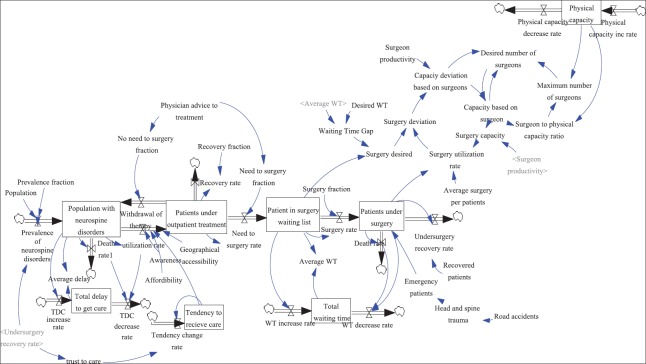
After identification of the variables, stock and flow diagram was outlined for both supply and demand models [Figures 2 and 3] in which squares were representative for stocks, arrows for flows, and circles for auxiliary variables.[16]
Figure 2.
Stock and flow diagram for supply submodel
Figure 3.
Stock and flow diagram for demand sub-model
Stock variables illustrate the current status of the system such as number of active neurosurgeons while flow variables represent the rates of change in stocks such as graduation rate in neurosurgery residents. In fact, stocks are built up of flows and mathematically estimated as below.
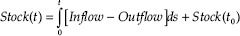
Inflow and outflow expressions in the equation stand for their values in an interval between initial time (s) and the present time (t).
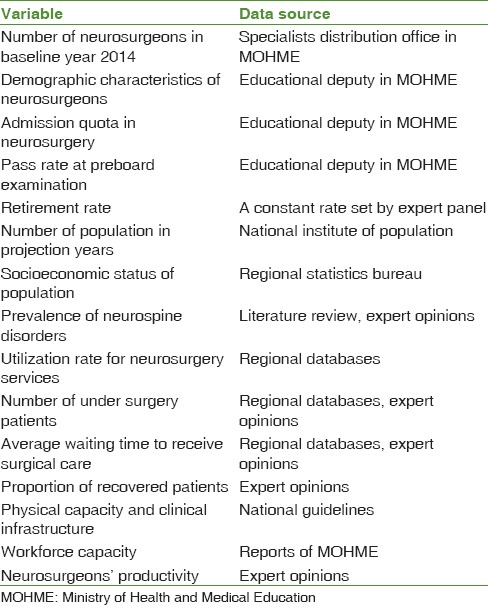
To estimate calculations on both supply and demand sides, sixty-one mathematical equations were defined for each variable on the basis of empirical data collected from different sources including expert panel viewpoints. Sample of some equations are listed in Table 1 and data sources used for the simulation model are presented in Table 2.
Table 1.
Equation models in stock and flow diagram
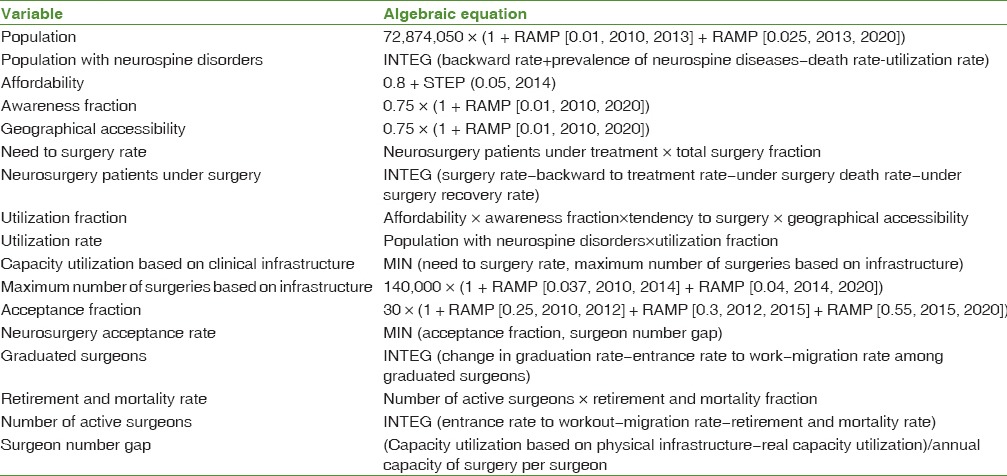
Table 2.
Data sources for the simulation model
The main outputs of the model were expected to be: number of neurosurgeons each year of projection, their full-time equivalents, number of required neurosurgeons depending on neurospine diseases, service utilization, workforce, and clinical infrastructure capacity in the community and gap existing in supply and demand for neurosurgeons each year.
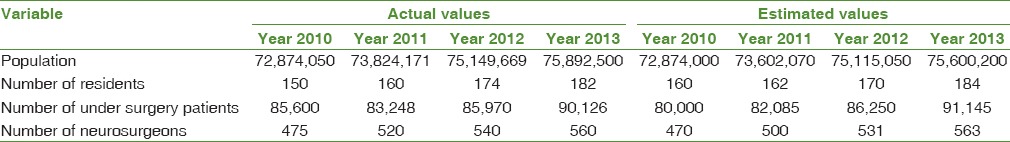
Finally, to confirm validity of the model, we compared the actual and estimated number of some variables in a time period which data were available for Table 3.
Table 3.
Validity test for the model
Results
Study results confirmed the validity of the model as shown in Table 3. The predicted number of residents in 2013 was 184 which was close to the actual value. As shown in Table 3, other estimates were also close to reality.
In 2010, there were 470 neurosurgeons working in public sector of health-care system in Iran. To meet population health needs (based on the estimated prevalence of neurospine disorders and service utilization rate), approximately 170 specialists would be required in 2015. As it is obvious, findings affirmed the available data for the existing year [Table 4]. Results also suggested that by maintaining the status quo without any policy intervention, the estimated shortage would increase gradually over the next 10 years and more surgeons would be required to bring desired level of services to a population.
Table 4.
Baseline model
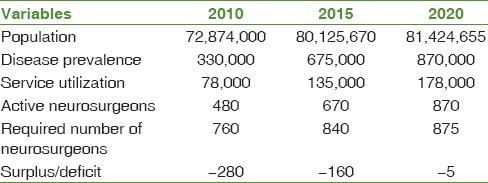
In the next step, some policy scenarios were applied to address the estimated shortage including change in admission quota for neurosurgery specialty, change in pass rate for preboard examination, change in retirement age, and attrition rate from labor market. By increasing the quota to 25% in 2014 and consequently a raise in the proportion of graduated surgeons entering to work, physician shortage dramatically reduced in a way that it completely disappeared by the year 2020. Furthermore, an improvement in the pass rate for preboard examination among graduated neurosurgery residents (5% annually) cut the shortage by approximately 15% over 10 years. Similarly, a 5-year increase in retirement age and 30% decrease in attrition rate reduced the specialists’ shortage by approximately 5%.
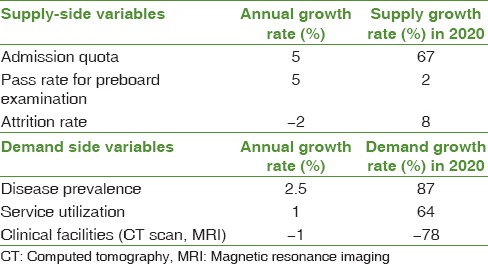
On the other hand, some scenarios were considered in relation to the demand side such as increase in the prevalence of neurospine disorders and service utilization among patients resulting from improvement in economic access and awareness of people toward their health status. Results confirmed that a 20% increase in disease prevalence and 10% enhancement in service utilization resulted in 46% and 34% increase in neurosurgeons’ shortage, respectively. Similar studies agreed that number of CT scan and MRI units in a community had significant effect on the required number of surgeons. Thus, as one of the policy scenarios, we examined the effect of 1% annual decrease in such clinical facilities on projection results [Table 5].
Table 5.
Growth rates for the supply and demand of neurosurgeons, 2010-2020
Discussion
Study results acknowledged that number of neurosurgeons will continue to increase during 2010–2020 in a way that shortage in their absolute number would be diminished during the projection time of the SD model. A range of factors have been considered to create our forecasting model until 2020 including population demographic and epidemiological change according to age and prevalence of neurospine disorders, incidence of neurospine diseases, utilization rate for outpatient and surgical services among population, clinical infrastructure capacity, supply of neurosurgeons, variations in number of residents and graduated surgeons, and attrition rate due to migration, retirement, or death.
One of the main objectives of the model was to examine the effects of different policies on neurosurgeons’ supply and demand heading for improvement in health workforce capacity of Iran health system. In fact, we applied some policy decisions (such as raising the admission quota for neurosurgery specialty and increase in retirement age of specialist) in the SD model to provide applicable information for planners and simulate their potential effects on their choices.
Before this study was conducted, there was a lack of long-term information about the future status of health professionals in Iran, especially provided by a comprehensive approach and system dynamic modeling. In addition, training policies were on the basis of the results of annual surveys which increased future imbalances in staffing levels in an inappropriate manner.[20]
Previous studies have estimated the number of health professionals by different methods. The main constraint of such models was due to their static nature.[7,21,22] To resolve such limitations, we made an effort to establish an inclusive model comprised of a large set of interrelated and dynamic variables related to population health needs, service utilization, human resources capacity, and medical infrastructure to predict the absolute number of required neurosurgeons in the study. Researchers introduced SD during the 1950s and have broadly applied it in human resource planning in recent years. Model has the potential to apply dynamic feedback loops to generate useful tool for policy planning which effectively clarifies the structures of problems, processes, relations among various factors, and feedback mechanisms.[23] Such a proactive approach in management and policymaking of health workforce would facilitate more realistic projections and decrease the probability of imbalances in supply and demand conditions.[24]
Strengths and limitations of the study
The main strength of our study was to ensure a precise estimation of neurosurgeons’ supply using key influential factors of surgeon demographics, graduation and pass rate in preboard examination, migration, and retirement. Similarly, important information such as incidence and prevalence of neurospine disorders, current stock of surgeons, clinical capacities of the community, utilization rate for inpatient, and outpatient services were considered in the demand model to guarantee the comprehensiveness. However, the study had some limitations based on the difficulty to acquire data. Improvement in data collection process both on workforce supply and demand would reduce the drawbacks. Study emphasized that the main barriers to quantitative health human resource modeling were data collection process and selection of proper demand drivers. As the abovementioned limitations, it is apparent that no forecasting model can provide an exact prediction.[25] In fact, each approach has its own weaknesses and the model applied in this study is no exception. However, developing a comprehensive health workforce model with a conceptual framework including as many of these factors as possible and their causal effects in a dynamic model was a solution that has been proposed.
Interpretation and implications in the context
Effective health workforce planning is critical to guarantee adequate number of staff available and consequently good quality and resourceful health-care services delivered to population.[26] Lack of adequate attention to this key process will decrease the quality of health services patients receive and increase the burden of expenses enforced to health system.
Conclusion
To address an appropriate number of health workforce, there are a number of forecasting approaches and methods. Since there is always a challenge for selecting an appropriate one, this paper attempted to apply an evidence-based framework to facilitate the process. Our study is the first quantitative and comprehensive effort in the Iranian context to define a systematic method for strategic planning and health human resource forecasting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge Iran Ministry of Health and Medical Education that helped us in gathering required data of the study.
References
- 1.Roberfroid D, Stordeur S, Camberlin C, Van de Voorde C, Vrijens F, Léonard C. Brussels: Belgian Health Care Knowledge Centre (KCE); 2008. Physician workforce supply in Belgium: Current situation and challenges. Health Services Research (HSR). KCE Reports C. [Google Scholar]
- 2.Simoens S, Hurst J. The supply of physician services in OECD countries. OCDE Work Pap. 2006;21:62. [Google Scholar]
- 3.World Health Organization. Working together for health. World Health Report. Geneva: World Health Organization; 2006. [Google Scholar]
- 4.Buchan J, Wismar M, Glinos IA, Bremner J. Health Professional Mobility in a Changing Europe. World Health Organization: The European Observatory on Health Systems and Policies. 2014 [PubMed] [Google Scholar]
- 5.Birch S. Health human resource planning for the new millennium: Inputs in the production of health, illness, and recovery in populations. Can J Nurs Res. 2002;33:109–14. [PubMed] [Google Scholar]
- 6.Stokker JH, Gillian H. The right person, in the right job, with the right skills, at the right time. A workforce planning model that goes beyond metrics. Libr Manag. 2009;30:561–71. [Google Scholar]
- 7.Roberfroid D, Leonard C, Stordeur S. Physician supply forecast: Better than peering in a crystal ball? Hum Resour Health. 2009;7:10. doi: 10.1186/1478-4491-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Busato A, Künzi B. Primary care physician supply and other key determinants of health care utilisation: The case of Switzerland. BMC Health Serv Res. 2008;8:8. doi: 10.1186/1472-6963-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Retail Online Integration. Contact Centers: How to Calculate Staff Levels and Scheduling Requirements. [Last retrieved on 2011 Jul 13]. Available from: http://www.retailonlineintegration.com/article/contact-centers-how-calculate-staff-levels-scheduling-requirements-27109/1 .
- 10.Murphy TG, Birch S, MacKenzie A. Ottawa: Canadian Nurses Association and Canadian Medical Association; 2007. Needs-based Health Human Resources Planning: the Challenge of Linking Needs to Provider Requirements. [Google Scholar]
- 11.Araseki M, Yokooka Y, Ishikawa T, Ogasawara K. The number of Japanese radiologic technologists will be increased in 40 years. Radiol Phys Technol. 2013;6:467–73. doi: 10.1007/s12194-013-0220-7. [DOI] [PubMed] [Google Scholar]
- 12.Homer JB, Hirsch GB. System dynamics modeling for public health: Background and opportunities. Am J Public Health. 2006;96:452–8. doi: 10.2105/AJPH.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joyce C, McNeil J, Stoelwinder J. More doctors, but not enough: Australian medical workforce supply 2001-2012. Med J Aust. 2006;184:441–6. doi: 10.5694/j.1326-5377.2006.tb00315.x. [DOI] [PubMed] [Google Scholar]
- 14.Mills MD, Thornewill J, Esterhay RJ. Future trends in the supply and demand for radiation oncology physicists. J Appl Clin Med Phys. 2010;11:3005. doi: 10.1120/jacmp.v11i2.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung SH, Jung Chae D, Yoon S, Lee D. A dynamic forecasting model for nursing manpower requirements in the medical service industry. Serv Bus. 2010;4:225–36. [Google Scholar]
- 16.Barber P, López-Valcárcel BG. Forecasting the need for medical specialists in spain: Application of a system dynamics model. Hum Resour Health. 2010;8:24. doi: 10.1186/1478-4491-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taati E, Meshkini A, Khorasani Zavareh D. Distribution of specialists in public hospitals of Iran. Health Inf Manag. 2012;9:548–57. [Google Scholar]
- 18.Taghavi M. Need Assesment and Policy Manking to Develop Specialized Human Resources. Research and Planning Center of Higher Education. Iran, Tehran. 2001 [Google Scholar]
- 19.Simforoosh N, Ziaee SA, Tabatabai SH. Growth trends in medical specialists education in Iran; 1979 – 2013. Arch Iran Med. 2014;17:771–5. [PubMed] [Google Scholar]
- 20.Nikpajouh A. Projecting the demand for cardiologists in Iran: Benchmarking. Payesh. 2012;11:589–4. [Google Scholar]
- 21.Joyce CM, McNeil JJ, Stoelwinder JU. Time for a new approach to medical workforce planning. Med J Aust. 2004;180:343–6. doi: 10.5694/j.1326-5377.2004.tb05972.x. [DOI] [PubMed] [Google Scholar]
- 22.Deloitte Center for Health Solutions. Better Health Care Worker Demand Projections: A Twenty First Century Approach. United States: Bipartisan Policy Center. 2013 [Google Scholar]
- 23.Forrester JW. Industrial Dynamics. Cambridge MA: MIT Press; 1961. [Google Scholar]
- 24.Chopra M, Munro S, Lavis JN, Vist G, Bennett S. Effects of policy options for human resources for health: An analysis of systematic reviews. Lancet. 2008;371:668–74. doi: 10.1016/S0140-6736(08)60305-0. [DOI] [PubMed] [Google Scholar]
- 25.Senese F, Tubertini P, Mazzocchetti A, Lodi A, Ruozi C, Grilli R, et al. Forecasting future needs and optimal allocation of medical residency positions: The Emilia-Romagna region case study. Hum Resour Health. 2015;13:7. doi: 10.1186/1478-4491-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rafiei S, Arab M, Rashidian A, Mahmoudi M, Rahimi-Movaghar V. Factors influencing neurosurgeons’ decision to retain in a work location: A Qualitative study. Glob J Health Sci. 2015;7:333–51. doi: 10.5539/gjhs.v7n5p333. [DOI] [PMC free article] [PubMed] [Google Scholar]