Abstract
BACKGROUND:
Tobacco use is a disease of addiction and a behavior choice. It is valuable to understand the psychosocial dimension of disease.
OBJECTIVES:
The research aimed to assess the (I) behavioral determinants and pattern of tobacco use (II) readiness to quit tobacco among patients with oral potentially malignant disorders (OPMDs) using transtheoretical model (TTM) approach visiting the dental college in Goa, India.
MATERIALS AND METHODS:
This cross-sectional analytical study was conducted among 300 patients over 3 months. Information about sociodemographics, determinants including age and reason of onset, behavioral stages, and the presence of OPMDs was collected using specially designed pro forma. Descriptive and inferential statistics were performed using SPSS 18.0.
RESULTS:
Smokeless form of tobacco 199 (66.34%) was most prevalent followed by smoking 79 (26.33%) and dual tobacco use 22 (07.33%) in males. Majority belonged to low socioeconomic class. Peer influence was the most-cited reason. Around 1/3rd of the participants had OPMDs associated with tobacco use. Significant association was observed between the presence of OPMDs and TTM behavioral stages. Patients with OPMDs are more motivated for tobacco cessation (odd's ratio = 2.30, P = 0.002), that is, they are more in preparation and action stages.
CONCLUSION:
The findings reflect that smokeless tobacco use is more prevalent in males with low level of education and socioeconomic class. Readiness to quit tobacco increases among patients with OPMDs using TTM.
Keywords: Smokeless tobacco, smoking, tobacco cessation, tobacco use
Introduction
Tobacco use in India is alarmingly increasing to a higher level adding the burden of noncommunicable diseases. More than one-third of adults in India consume tobacco according to the Global Adult Tobacco Survey (GATS), India report.[1] India is the third largest tobacco producer and second largest tobacco consumer after China.[2] Apart from systemic complications, the association between tobacco use and oral lesions, including oral potentially malignant disorders (OPMDs) are evidently reported.[3,4,5]
Globally, cigarette smoking is the dominant form of tobacco use. In the Indian context, smoking, smokeless, and a noticeable proportion of dual use are seen.[6,7,8] Various smoking and smokeless forms are bidi, gutka, khaini, pan masala, gul, mawa, misri, hookah, cigarettes, cigars, chillum, chutta, etc.[6,7,8,9,10,11]
Tobacco use is a disease of addiction and a behavior choice with most of the users start during their childhood or adolescence. Various psychosocial factors leading to the initiation of tobacco use are family history of tobacco use, peer influence, experimentation, easy access, personality factors, emotional, and psychological problems.[10,11,12,13,14,15,16] Considering above factors, it is essential to understand the psychosocial dimension of the disease.
There are a number of established aids for tobacco cessation, including a range of pharmacotherapies and behavioral approaches.[17,18] One widely used behavioral approach is the “stages of change” or transtheoretical model (TTM), propounded by Prochaska et al. for tobacco cessation has success rate from 4.5% to 39.5%.[19] It assumes that smokers pass through a discrete series of motivational stages. These are precontemplation, contemplation, preparation, action, and maintenance stage. People who are in the preparation stage have high motivation for cessation.[20]
It is of utmost importance to recognize the behavioral determinants for tobacco use. Very few studies have been done to understand the pattern and prevalence of tobacco use in Goa.[17,21,22] Furthermore, little information is available on the association between behavioral stages and readiness to quit tobacco. In the present study, we aimed to assess the readiness to quit tobacco among patients with OPMDs visiting the dental college in Goa. We hypothesized that the presence of OPMDs will influence patients’ readiness to quit tobacco.
Materials and Methods
The present cross-sectional, institutional-based, analytical study was conducted over 3 months (January to March 2017) on patients referred for the Tobacco Cessation Counseling (TCC) to the Department of Public Health Dentistry in a Dental College in Goa. Ethical clearance was provided by the Institutional Ethical Committee. Informed written consent was obtained from the participants after explaining the purpose of the research.
A pilot study was carried out on a sample of 20 participants to check the feasibility of the study and to check if any modification was required for the pro forma. All patients visiting for TCC during the study period were included. Patients who had alcohol habit along with tobacco were excluded from the study.
Data were collected using a specially designed pro forma based on thorough literature search.[10,11,13,14,15,16] Behavioral determinants and pattern for tobacco use were assessed using following parameters; age, gender, socioeconomic status, type, number and frequency of tobacco use, an age of onset, years of exposure, and the reason for initiation. Socioeconomic status was defined assessed using Kuppuswamy classification.[23] Information about OPMDs were ascertained from records of the patients. Behavioral stages were determined using TTM criteria. These are precontemplation (no thoughts of quitting in next 6 months), contemplation (thinking about quitting in next 6 months), preparation (planning to quit in the next 30 days), action (quitting successfully for up to 6 months), and maintenance (no smoking for more than 6 months).[18] No separate questionnaire was used to classify patients for behavioral stages. The questionnaire was filled simultaneously while doing TCC of the patient during their first visit. Questions were asked to the patients and responses were recorded by the investigators.
Data analysis
After collection of data, pro forma were checked and verified for any omissions, errors, or irrelevancies. The data were first transferred to Microsoft Excel, and then the results were analyzed using SPSS version 18 (IBM Corporation, SPSS Inc., Chicago, IL, USA). Descriptive statistics were performed to summarize numeric and qualitative data. For inferential statistics, Chi-square test was applied and odd's ratio (OR) was calculated. To check the association, data were dichotomized as the presence or absence of oral lesions; behavioral stages were dichotomized as (precontemplation + contemplation) into one and (preparation + action) into another. P < 0.05 was considered to be statistically significant.
Results
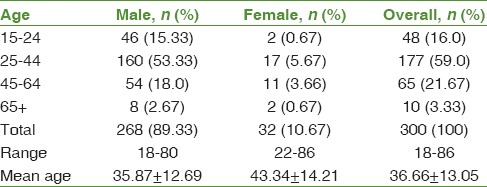
The study sample comprised 300 patients, among whom 268 (89.33%) were male. The majority of the participants in both the gender were in 25–44 years of age [Table 1]. Around 167 (56%) of participants completed their study till high school and 56 (18.66%) with no formal education. Majority of the participants were in a low-income category and belonged to low socioeconomic class.
Table 1.
Distribution of the study participants based on age (years)
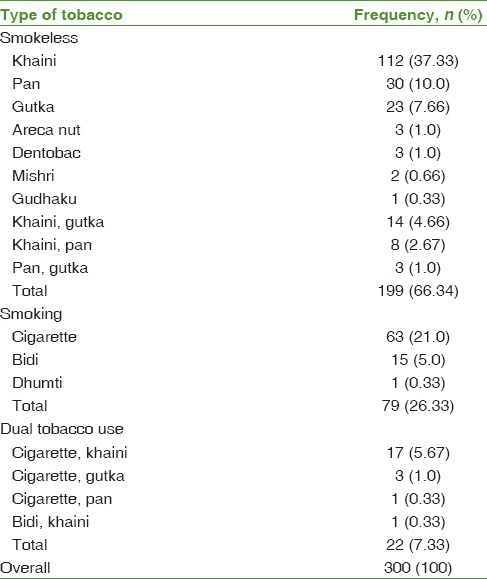
Out of 300 participants, 91 (30.33%) (84 [92.30%] males, 7 [07.70%] females) had some oral lesion associated with tobacco use. The lesions encountered were tobacco pouch keratosis, leukoplakia, erythroplakia, oral submucous fibrosis, and smoker's palate. For the type of tobacco use, majority had smokeless tobacco habit 199 (66.33%) (173 [86.93%] males, 26 [13.07%] females), trailed by smoking 79 (26.33%) (73 [92.40%] males, 06 [7.60%] females), and dual tobacco use 22 (07.34%) (22 [100%] males, none in females) [Table 2].
Table 2.
Distribution of the study participants based on type of tobacco use
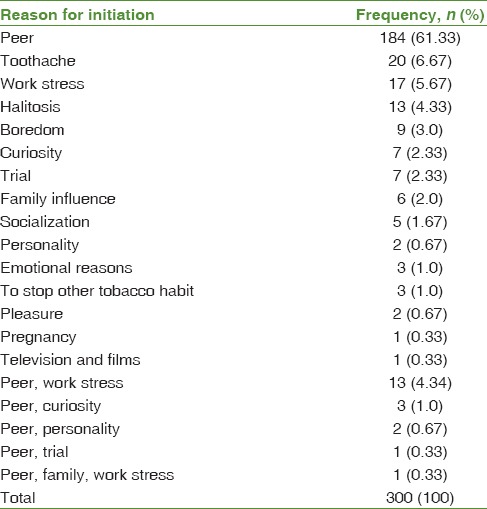
Participants in the age range of 25–44 years were comparatively higher for all kind of tobacco use. The age of onset and years of exposure to tobacco use ranged from 10 to 52 years (Mean age 25.44 ± 8.34 years) and 1–55 years (Mean age 11.19 ± 10.66 years), respectively. Majority 144 (48%) had the onset of tobacco use between 21 and 30 years and years of exposure between 1 and 10 years 194 (64.67%). When asked for the reason of initiation of tobacco use, peer influence, toothache, work stress, halitosis, boredom, curiosity, experimental or trial, family influence, etc., were cited [Table 3].
Table 3.
Distribution of the study participants based on reason for initiation of tobacco use
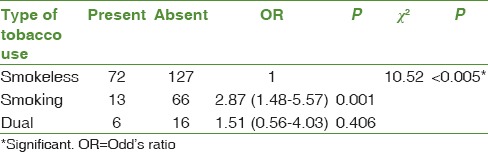
Approximately 141 (47%) of the participants were in contemplation stage and least in action stage 11 (03.67%) [Table 4]. Significant association was seen between the presence of oral lesions and behavioral stages of TTM (OR = 2.30, P < 0.05). Those who had oral lesions associated with tobacco use were more in preparation and action stage [Table 5]. When checked for the type of tobacco use and the presence of an oral lesion, smokers had higher chances of getting an oral lesion (OR = 2.87, P < 0.001) [Table 6]. There was no significant association between gender and presence of an oral lesion (P = 0.314).
Table 4.
Distribution of the study participants based on transtheoretical model behavioral stages
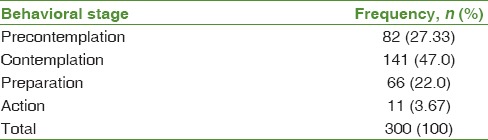
Table 5.
Association between OPMDs and transtheoretical model behavioral stages

Table 6.
Association between type of tobacco use and OPMDs
Discussion
The present study was conducted to assess the readiness to quit tobacco in patients with OPMDs using TTM approach among patients visiting a dental college in Goa, India. The key finding was that participants with OPMDs were more motivated for tobacco cessation than without OPMDs. Smokeless tobacco use was the most common habit with peer influence most-cited reason for the initiation of tobacco use.
Behavioral determinants for tobacco use
The prevalence of tobacco use was much higher in males than females with a ratio of 9:1 approximately. The finding of this study is in line with GATS survey of India and World Statistics where males are more indulged in tobacco use habits.[17] Furthermore, studies in the literature have reported the same.[8,10,12,21,24,25]
Children and adolescents are the most vulnerable population to initiate tobacco use.[11,13,14,15,16] The average age of onset was 25.44 ± 8.34 years which is higher than reported by the report in India (17.8 years)[17] and Khan and Mahmood.[10] Around 4/5th of the total participants started using tobacco before the third decade of life. The majority of the participants consuming tobacco in the age range of 25–44 years concords with the GATS survey[17] where smokeless tobacco use and dual use were highest in the age group 25–44 years.
Education is one of the most important established determinants of tobacco use irrespective of the type of use.[1,26,27] The lower level of education coupled with less awareness leads to early initiation of tobacco use. The majority of the study participants had the lower level of educational attainment. Approximately 1/5th of the total participants were illiterate.
Majority of the participants belonged to low socioeconomic status. The rich-poor differences are more observed among the smokeless tobacco and dual users. More prevalence of smokeless tobacco in this study reflects the evidence available in the literature.[1,7,21,26,27]
Smokeless tobacco was most commonly used followed by smoking and dual tobacco use. The pattern of tobacco use found in this study is in line with GATS, India,[17] but in contrast to a study conducted in Goa[21] where smoking was more prevalent than smokeless tobacco. Approximately 4/5th of the females, when compared to 3/5th males, had smokeless tobacco habit suggestive of more smokeless tobacco habit in females. In the smokeless tobacco category khaini, pan, and gutka chewing were dominating forms similar to study in Goa.[21] Pan chewing was dominant form in the previous study[21] unlike khaini chewing in the present study. Very few used Dentobac, mishri, and gudhaku for cleaning teeth. Smoking was reported in 79 (26.33%) of participants with males contributing 73 (92.40%).[27]
Cigarettes, bidi, and dhumti were reported in smoking forms. Finding is in line with Rama and Vanita study.[21] Dual users are at much higher health risks than those who consume the individual tobacco product. It was reported by 22 (7.33%) of the study population. None of the females were dual tobacco users. The difference in finding with the previous study in Goa can be due to different population involved. When checked for the association between type of tobacco use and the presence of the lesion, smokers had 2.87 times more chances of getting oral lesion when compared to smokeless tobacco use. Dual users had 1.51 times more chances of getting oral lesions than smokeless tobacco users, but it was not statistically significant.
Three in five participants cited peer influence as the main reason for the initiation of tobacco use. Very few told curiosity, experimentation, personality, television, and films for initiation. The findings support available literature.[11,13,14,16] It was reported toothache a reason for initiation as keeping tobacco in the mouth temporarily relieves pain and subsequently, they get addicted to it. Tobacco use is also cited to mask halitosis by 13 (4.33%) participants. Tobacco is also a part of the sociocultural milieu in various societies, especially in the Eastern, Northern, and Northeastern parts of the country.[17] Family influence and socialization were the reason for 3.67% of participants. Initiation during pregnancy was reported in the first trimester by a participant. Emotional reason and to stop other tobacco habit each reported by 3 (01%) participants.
Oral potentially malignant disorder
Nearly 1 in 3 participants had oral lesion associated with tobacco use. This shows how severely tobacco is affecting its users. Out of 91, 59 (64.83%) had oral lesion present within 10 years of onset of tobacco use. One in 4 females, when compared to 1 in 3 males, had oral lesion due to tobacco use. No significant association was seen between gender and presence of an oral lesion.
Behavioral stages
Approximately 1 in 2 participants were in contemplation stage followed by precontemplation, preparation, and action stage. The precontemplation and contemplation stages of change are filled with ambivalence. In these stages, individuals are either unaware of the problematical behavior or reluctant about the behavioral change.[28] They have a low self-reliance to change the behavior.[29] While individuals in preparation stage have high motivation for cessation, considering the cons of habit are higher than the pros.[20] It is well established that people in the preparation and action stages of quitting require different types of intervention from those in precontemplation or contemplation.[18]
Significant association was seen between OPMDs and TTM behavioral stages. Participants with OPMDs were 2.30 times more likely to move in preparation and action stage than precontemplation and contemplation stage. Based on the findings, it can be highlighted that those who are aware of the presence and consequence of potentially malignant disorders, they are more motivated toward the cessation of tobacco habits.
Strengths, limitations, and recommendations for future research
This study has few limitations in its generalizability. Being a cross-sectional design, the study was done on patients visiting the dental college for some treatment. Pro forma used for data collection may suffer from reporting bias, social desirability bias, memory, or recall bias. Within the limitations of the study, an assumption on the current pattern of tobacco use in Goa can be done as patients are visiting dental college from all parts of Goa. Being only dental college in Goa state, the study population gives a fair representation of Goa. This study however offers an interesting insight into the significant association between TTM behavioral stages and OPMDs. Future research is necessary to address these limitations. High prevalence of smokeless tobacco among both males and females need targeted interventions. Policymakers should consider socioeconomic patterning of tobacco use for tobacco control. There is a need to focus and address adolescent population to overcome peer influence and initiate tobacco habits. It is important that all health providers including dental personnel must involve in combating today's tobacco war as no single health-care professional can access all tobacco users.
Conclusion
High prevalence of smokeless tobacco was seen in both the gender among the low socioeconomic status population. Significant association was observed between the presence of OPMDs and TTM behavioral stages. Readiness to quit tobacco increases in patients with OPMDs. A greater understanding of behavioral stages in TTM along with factors associated with tobacco use will assist dental professionals to move forward toward the cessation of habits.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Singh A, Ladusingh L. Prevalence and determinants of tobacco use in India: Evidence from recent global adult tobacco survey data. PLoS One. 2014;9:e114073. doi: 10.1371/journal.pone.0114073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mishra GA, Pimple SA, Shastri SS. An overview of the tobacco problem in India. Indian J Med Paediatr Oncol. 2012;33:139–45. doi: 10.4103/0971-5851.103139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen PE. Tobacco and oral health – the role of the World Health Organization. Oral Health Prev Dent. 2003;1:309–15. [PubMed] [Google Scholar]
- 4.Johnson NW, Bain CA. Tobacco and oral disease. EU-working group on tobacco and oral health. Br Dent J. 2000;189:200–6. doi: 10.1038/sj.bdj.4800721. [DOI] [PubMed] [Google Scholar]
- 5.Sham AS, Cheung LK, Jin LJ, Corbet EF. The effects of tobacco use on oral health. Hong Kong Med J. 2003;9:271–7. [PubMed] [Google Scholar]
- 6.Kashyap GC, Singh SK. Progression in tobacco use in India: An application of survival function analysis. Int J Soc Sci Manag. 2016;3:22–30. [Google Scholar]
- 7.Thakur JS, Prinja S, Bhatnagar N, Rana SK, Sinha DN, Singh PK, et al. Widespread inequalities in smoking and smokeless tobacco consumption across wealth quintiles in states of India: Need for targeted interventions. Indian J Med Res. 2015;141:789–98. doi: 10.4103/0971-5916.160704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vol. 1. India, Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06. [Google Scholar]
- 9.Gonmei D, Shanbhag N, Puranik MP. Strategies for tobacco cessation counseling by dental personnel. Int J Adv Health Sci. 2015;2:33–41. [Google Scholar]
- 10.Khan NR, Mahmood AR. Pattern of tobacco consumption and related factors among the people residing in a rural area. Bangladesh Med J. 2015;44:32–7. [Google Scholar]
- 11.Chadda R, Sengupta S. Tobacco use by Indian adolescents. Tob Induc Dis. 2002;1:111–9. doi: 10.1186/1617-9625-1-2-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Preeti S, Raut DK. Prevalence and pattern of tobacco consumption in India. Int Res J Soc Sci. 2012;1:36–43. [Google Scholar]
- 13.Anjum M, Srikanth MK, Reddy PP, Monica M, Rao KY, Sheetal A. Reasons for smoking among the teenagers of age 14–17 years in Vikarabad town: A cross-sectional study. J Indian Assoc Public Health Dent. 2016;14:80–3. [Google Scholar]
- 14.Naing NN, Ahmad Z, Musa R, Hamid FR, Ghazali H, Bakar MH, et al. Factors related to smoking habits of male adolescents. Tob Induc Dis. 2004;2:133–40. doi: 10.1186/1617-9625-2-3-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhojani UM, Chander SJ, Devadasan N. Tobacco use and related factors among pre-university students in a college in Bangalore, India. Natl Med J India. 2009;22:294–7. [PubMed] [Google Scholar]
- 16.Sharma V, Hiremath SS, Puranik M, Somasundara S. Prevalence of tobacco use among 15-20 years old college students in Bengaluru city. J Indian Assoc Public Health Dent. 2015;13:24–9. [Google Scholar]
- 17.New Delhi, Mumbai: IIPS, MoHFW, Government of India; 2010. International Institute for Population Sciences (IIPS), Ministry of Health and Family Welfare (MoHFW), Government of India. Global Adult Tobacco Survey India Report (GATS India), 2009-10. [Google Scholar]
- 18.Cahill K, Lancaster T, Green N. Stage-based interventions for smoking cessation. Cochrane Database Syst Rev. 2010;10:CD004492. doi: 10.1002/14651858.CD004492.pub4. [DOI] [PubMed] [Google Scholar]
- 19.Koyun A, Eroǧlu K. The transtheoretical model use for smoking cessation. European Journal of Research on Education, 2014; Special Issue: Contemporary Studies in Social Science. :130–4. [Google Scholar]
- 20.Eslami AA, Charkazi A, Mostafavi F, Shahnazi H, Badeleh MT, Sharifirad GR, et al. Smoking behavior, nicotine dependency, and motivation to cessation among smokers in the preparation stage of change. J Educ Health Promot. 2012;1:47. doi: 10.4103/2277-9531.104818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rama GS, Vanita SP. Prevalence and patterns of tobacco use: A cross sectional study in Santa Cruz, Goa, India. Int J Thesis Projects Diss. 2015;3:43–52. [Google Scholar]
- 22.Pednekar MS, Gupta PC. Tobacco use among school students in goa, India. Indian J Public Health. 2004;48:147–52. [PubMed] [Google Scholar]
- 23.Patro BK, Jeyashree K, Gupta PK. Kuppuswamy's socioeconomic status scale 2010-the need for periodic revision. Indian J Pediatr. 2012;79:395–6. doi: 10.1007/s12098-011-0517-7. [DOI] [PubMed] [Google Scholar]
- 24.New Delhi: Ministry of Statistics and Programme Implementation, Government of India; 1997. National Sample Survey Organization (NSSO). Fifty Second Round of National Sample Survey on Household Expenditure (1997) [Google Scholar]
- 25.Vol. 1. India, Mumbai: IIPS; 2000. International Institute for Population Sciences (IIPS), Macro International. National Family Health Survey (NFHS-2), 1998-99. [Google Scholar]
- 26.Agrawal S, Karan A, Selvaraj S, Bhan N, Subramanian SV, Millett C, et al. Socio-economic patterning of tobacco use in Indian states. Int J Tuberc Lung Dis. 2013;17:1110–7. doi: 10.5588/ijtld.12.0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohan P, Lando H. Oral tobacco and mortality in India. Indian J Clin Med. 2016;7:5–12. [Google Scholar]
- 28.Prochaska JO, Norcross JC, DiClemente CC. Harper Collins Publishers; 2011. Changing for Good: A Revolutionary Six-Stage Program for Overcoming Bad Habits and Moving Your Life Positively Forward. [Google Scholar]
- 29.Hollis JF, Polen MR, Whitlock EP, Lichtenstein E, Mullooly JP, Velicer WF, et al. Teen reach: Outcomes from a randomized, controlled trial of a tobacco reduction program for teens seen in primary medical care. Pediatrics. 2005;115:981–9. doi: 10.1542/peds.2004-0981. [DOI] [PubMed] [Google Scholar]


