Abstract
INTRODUCTION:
Primary dysmenorrhea without pelvic pathology is one of the most common complaints in women's medicine. Primary dysmenorrhea can affect the quality of life of women. Aerobic exercise is one of the ways to reduce the severity of primary dysmenorrhea. The present study aimed to determine the effect of 8 weeks of aerobic exercise on the severity of primary dysmenorrhea.
METHODS:
This is a clinical trial study performed on 70 students with primary dysmenorrhea in dormitories of Mashhad University of Medical Sciences in 2015. Participants were randomly assigned to intervention and control groups. The instrument was a visual pain questionnaire completed by the two groups in the first 3 days of the menstrual cycle. The exercise protocol included aerobic exercise, which performed the intervention group for 8 weeks, three times a week, and each time for 30 min. Data were analyzed by Fisher and Chi-square tests.
RESULTS:
The control and intervention groups were homogeneous in terms of demographic characteristics. Results showed that the severity of primary dysmenorrhea at the beginning of the study was not significantly correlated with the two groups. At the end of the 4 weeks after the intervention, the intervention group did not show any significant changes in the control group (P = 0.423) but At the end of 8 weeks after the study, the intervention group showed significant changes compared to the control group (P = 0.041).
CONCLUSION:
The results of this study showed that performing aerobic exercise can improve primary dysmenorrhea. Therefore, aerobic exercise can be used to treat primary dysmenorrhea.
Keywords: Aerobic exercise, pain intensity, primary dysmenorrhea
Introduction
Primary dysmenorrhea or painful menstruation without pelvic pathology is one of the most common complaints in women's medicine. More than 50% of women who have menstrual bleeding have a painful menstruation, as 10% of them are so severe that they disrupt 1–3 days of their lives each month.[1] The pain begins with the onset of menstrual bleeding and lasts for 72–12 h. Pain is usually in the middle line of the highest severity. Dysmenorrhea pain is often described as cramped and intermittent. Some women have severe back and thigh pain. Abdominal pain is often accompanied by nausea and vomiting, bruising and headache, and an unpleasant general feeling. Pain usually has the highest severity on the 1st day of bleeding and gradually decreases its severity.[2] Although primary dysmenorrhea is not a life-threatening person and does not cause organ failure, it can affect the quality of life of women and in severe cases, leads to disability and inability to function in the absence of school or work place.[3] The recommended treatment methods to reduce the severity of pain in the primary dysmenorrhea include the use of contraceptive pills, calcium channel blockers, skin electrical stimulation, dietary supplements, exercise and massage. Most of these methods are costly and time consuming and some people refuse to use them.[4,5] Given that the use of synthetic drugs, especially in long-term prescriptions, has side effects such as nausea, gastric ulcers and kidney papillary necrosis. During the past 30 years, exercise and physical activity have also been considered as an effective treatment for the prevention and treatment of dysmenorrhea.[3,6] Primary dysmenorrhea occurs when the uterus suffers from spasticity due to reduced blood supply. The release of prostaglandins and other inflammatory mediators in the uterus is thought to be one of the primary causes of dysmenorrhea. An increase in the amount of prostaglandins leads to ischemia and uterine contractions. In some studies, there is also a link between levels of hormones such as progesterone, estrogen, and vasopressin.[4] The reason for pain in dysmenorrhea is the increase in the level of prostaglandins in the body, as the decrease in the amount of progesterone at the end of the luteal phase leads to stimulation of the lubricating action of the enzymes, which causes the release of arachidonic acid from the phospholipids along with activation of the cyclooxygenase pathway. Increasing the level of prostaglandins leads to uterine contraction, uterine ischemia, and increased sensitivity to pain fibers and ultimately causes pelvic pain. Sports activity decreases the level of serum aldosterone by reducing the level of renin and increasing estrogen and progesterone and thus decreases and improves physical symptoms.[7,8,9] The study of Mohammadi et al. aimed at determining the effect of aerobic exercise on some of the menstrual symptoms of nonathlete students showed that with the regular and continuous exercise of aerobic exercise, early menstrual dysmenorrhea and severe menstrual bleeding can be controlled or Preventing it.[10] Shavandi et al. examined the effect of an isometric exercise on primary dysmenorrhea, and concluded that, given the positive effect of isometric exercise exercises on primary dysmenorrhea as an important problem for female student students that led to absenteeism from the classroom and Isometric exercise is a useful method for this age group, and it is possible to spend isometric exercises anywhere without spending money to reduce the complications of primary dysmenorrhea.[11]
However, according to Blakey et al. Study, which aimed to determine the relationship between primary dysmenorrhea and aerobic exercise on 654 female students, there was no significant relationship between primary dysmenorrhea and aerobic exercise, Also, according to Davaneghi et al. Study, There was no correlation between participation in sport activity and the severity of primary dysmenorrhea.[12,13] according to Sehati et al. study There was no significant relationship between the distribution of dysmenorrhea between athletic and nonathlete groups.[14]
Considering the high prevalence of dysmenorrhea in Iran and its adverse effects on the quality of life and social activities of women on the one hand and the different and contradictory results in some studies, and being low studies on aerobic exercise and the severity of primary dysmenorrhea, on the other hand, it seems that the study Identifying effective lifestyle factors like exercise can be a step in the prevention, control and even cure of it. Therefore, the aim of this study was to investigate the effect of 8 weeks of regular aerobic exercise on the severity of primary dysmenorrhea.
Methods
The present study was a clinical trial with registration code (IRCT2015021721116N1) and Code of ethics (code 931232) on 70 students of student dormitories at Mashhad University of Medical Sciences in 2015. Independent variable was aerobic exercise and the dependent variable was primary dysmenorrhea. Based on a pilot study conducted on 10 Participants, taking α = 0.05 and β = 0.2, Given the sample loss, the sample size was estimated to be 35 (35 controls and 35 intervention groups).
The criteria for entering the study were: Residents of the dormitory, written consent for participation in the study, having regular menstrual cycles (30–35 days) and bleeding time of 10-3 days, primary dysmenorrhea (based on a visual questionnaire and a pain leader) and criteria Exclusion from the study includes pregnancy, known genital diseases and chronic diseases (heart disease, respiratory, kidney, blood pressure, asthma, diabetes, epilepsy, migraine, thyroid, anemia, nervous disorders), passing training Physical activity and participation in other sports programs. Also, the research units provided that the withdrawal of the menstrual cycle during the 2 months of study was due to its natural order, dissatisfaction with the continuation of the research, failure to complete the questionnaire, the occurrence of stressful and unpleasant incidents during the research and the lack of training in 3 consecutive or 4 sessions alternate during the study were excluded from the study. In order to avoid influencing the intervention group on control, random allocation of dormitories to the intervention and control group was performed. In the intervention group, an aerobic exercise training session was taught to the units of the intervention group during an aerobic exercise session. At the end of the session, CDs and educational posters (containing all the movements performed) were provided to the units of the intervention group and they were asked to perform aerobic exercise for 8 weeks, three times a week, and each time for 30 min. Each exercise stage included warming movements (head movements, traction and shoulder rotation, and balance), cold movements (resting and sitting movements to return to initial state), and aerobic exercise (kinetic movements including rotation and elongation of the arms, upper rotation).
The instrument used in this study was a questionnaire, which was arranged in two main sections, the first part containing personal data, history of menstruation and the name of the medications used during menstruation and the history of the diseases and the severity of pain in the menstrual period based on the visual scale of the pain (A pain reliever with a score range of 0–10). The second part was about symptoms of dysmenorrhea, abdominal pain, back pain, leg pain, headache, breast pain, nausea, muscle cramps.
The pain intensity scale was a pain reliever that was categorized from zero (no pain) to ten (maximum pain), and pain score and pain severity were categorized and evaluated as follows:
(A) severe pain (pain score of 8–10) people requires limitation of activity, rest and drug use. (B) moderate pain (pain score 4–7) people need to take medication and resting does not affect it. (C) Mild pain (pain score of 1–3) people do not need to use medication and rest, there is no limitation in daily activity.
The validity of the tool was confirmed by ten midwifery professors of Mashhad University of Medical Sciences. The reliability of the test was confirmed by a re-test method (93%).
Initially, the researcher invited a group of people with primary dysmenorrhea to participate in the research, and then explained the research objectives and methodology for the participants. Participants entered the study with consent. Initially, in the first menstrual cycle, the severity of primery dysmenorrhea was determined by the participants on the pain reliever. Then, after random allocation, the participants in the intervention and control groups (using the paired numbers and nonpaired numbers, participants were placed in a control group with a paired numbers and participants were placed in a intervention group with a nonpaired numbers), the research samples in the intervention group, with Initiation of menstrual period performed aerobic exercise and completed the questionnaire related to menstrual pain. This questionnaire was completed in the first 3 days of each cycle and during the aerobic exercise period. In the control group, without intervention, the Participants should complete the questionnaires for two cycles in the first 3 days of menstruation. The follow up was done in the control and intervention groups by telephone (twice a week) and face-to-face (once every 2 weeks).
Dysmenorrheal pain was categorized according to visual pain criteria: mild (pain score <4), moderate (pain score between 4 and 7) and severe (pain score >7).
At the end of 8 weeks, questionnaires were collected. Information was encrypted and entered into SPSS (Version 23) software (IBM, SPSS Inc, Chicago, Illinois, USA). Then, descriptive statistics, Chi-square and Fisher's exact tests were used to analyze the data.
Results
The results of this study showed that the mean age of the intervention group was 41/4 ± 22/25 and the control group was 71/4 ± 06/24. 77.1% (27 persons) in the intervention group and 40% (18 persons) in the control group were single controls. 62.9% (22 persons) in the intervention group and 70% (21 persons) in the control group had a history of absenteeism from the work or class due to dysmenorrhea. Also, 45.7% (16 patients) of the intervention group reported a history of using the treatment. The duration of bleeding was 41/1 ± 6/6 days in the intervention group and was 34/1 ± 33/in the control group days. The menstrual periods in the intervention group were 34/69 ± 3/68 and 27/63 ± 3/39 in the control group. The severity of menstrual pain before intervention was 4/02 ± 3/52 in the intervention group and was 3/80 ± 2/85 in the control group. To examine the homogeneity of control and intervention groups in terms of age, marriage, history of treatment, type of treatment, effect of treatment, duration of bleeding, menstrual periods, dysmenorrheal pain, diet, menarche age and history of syndrome in first degree relatives (mother, sister) performed statistical tests that were homogeneous. According to a special purpose, statistical analysis was performed on dysmenorrhea.
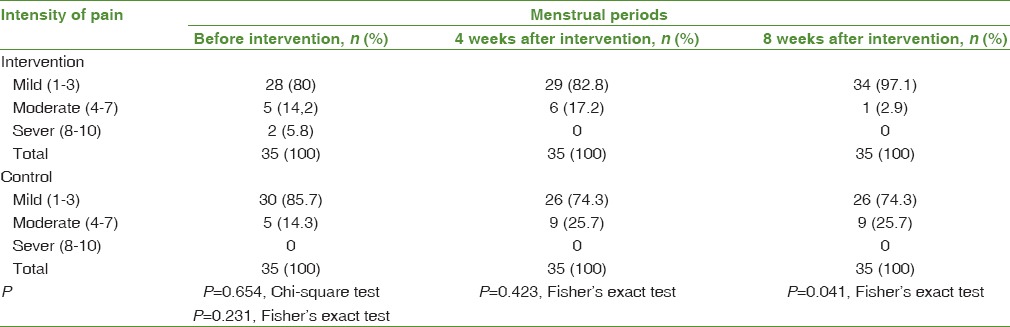
The results showed that the severity of primary dysmenorrhea in the intervention group at the end of 4 weeks after intervention was not significant (P = 0/423). However, at the end of 8 weeks after intervention, showed significant changes (P = 0/041) [Table 1].
Table 1.
Evaluation of pain intensity of dysmenorrhea before and after intervention in two groups: Control and intervention
Discussion
Today, different methods of treatment for primary dysmenorrhea have become prevalent, and uncomplicated treatments have found a special place in the research of researchers in the treatment of dysmenorrhea. The results of this study showed that 8 weeks of aerobic exercise significantly improved the severity of pain in the primary dysmenorrhea in the intervention group compared to the control group. Findings from various studies indicate that exercise therapy and physical activity are related to decreasing dysmenorrhea. According to research, sports exercises with increased premenstrual pelvic blood flow, the onset of prostaglandin accumulation in this area delayed the onset of pain; exercise during pain can lead to faster transfer of wastes and prostaglandins (which is the main cause of menstrual pain) from the uterus. On the other hand, regular exercise plays an important role in reducing stress and helps improve blood circulation and increases levels of endorphins and nerve transducers. As a result, dysmenorrhea decreases the blood flow to the uterus. Inhibition of stress is one of the most common causes of the relationship between exercise and menstruation.[15]
Shavandi et al. also examined the effect of 8 weeks of isometric exercises on primary dysmenorrhea in female students, and concluded that performing isometric exercises (including abdominal, pelvic and groin enhancement exercises) in reducing the severity and duration of pain and the rate of use of medication is effective.[11] Also, Chantler et al. showed that exercising due to the release of endorphins, relaxation, stress relief and improved blood flow can reduce the severity and duration of dysmenorrhea.[16] Mohammadi et al. also examined the effect of aerobic exercise on some menstrual symptoms of nonathletic students, and concluded that regular and continuous aerobic exercises can control initial dysmenorrhea and severe menstrual bleeding,[5] Which was consistent with the results of the present study. The study of Aganoff and Boyle, aimed at the effect of aerobic training on menstrual cycle symptoms and women's psychological state, showed that regular aerobic exercise can increase relaxation in the mood and body.[17] In the present study, it seems that the improvement of the flow blood and increased mental and physical relaxation are one of the reasons for the effect of aerobic exercise on dysmenorrhea.
Harlow and Park, Blakey et al. Reported that there was no relationship between exercise and primary dysmenorrhea.[12,18] Also according to Sehati et al. study, there was no significant relationship between the distribution of dysmenorrhea between athletic and non-athlete groups.[14] In their study, Davaneghi et al. also concluded that there was no relationship between the level of physical activity and the severity of dysmenorrhea,[13] this discrepancy between the studies with this study is likely to be due to differences in the type of exercise protocol and participants in the study.
Exercise is widely used as a way to reduce daily stress and control chemical changes in the immune system. Performing favorite things, listening to music, meditating, self-hypnosis, and exercising have been introduced as treatments for stress management. Exercise can reduce stress by reducing the sympathetic nervous activity and increasing the activity of parasympathetic nerves during rest while reducing the symptoms of menstruation. In fact, the degree to which people respond to pain is different. This phenomenon is partly due to the ability of the brain to suppress the input signals of the brain by the pain control system.[19] Therefore, differences in findings may be due to individual differences in the amount of pain perception. Menstrual pain is probably due to increased uterine muscle contraction, which is nerve-mediated by the sympathetic nervous system.[20,21] Stress helps to increase the activity of the sympathetic nerves and may increase the contraction of the muscles of the uterus and increase the pain of the menstrual period. Exercise by reducing stress can reduce the activity of the sympathetic nervous system and as a result, the symptoms and symptoms of menstruation can be reduced.[13]
Conclusion
Based on the findings of this study, it can be concluded that the use of regular aerobic exercise with moderate intensity can reduce or prevent the occurrence of certain menstrual disorders. Therefore, aerobic exercise can be used as a preventive, therapeutic or therapeutic approach to control dysmenorrhea and other menstrual disorders. In fact, it can be said that performing regular aerobic exercise through mental and physical relaxation and improving blood flow can improve menstrual symptoms.
Financial support and sponsorship
This study was funded by Mashhad University of Medical Science.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study is a research project with the code 93,123 approved by Mashhad University of Medical Sciences. For this purpose, we thank the research Vice President of Mashhad University of Medical Sciences for the cost of this study and all the participants in the study.
References
- 1.Jalili Z, Safizade H, Shamspour N. Prevalence of primary dysmenorrheal on high school student Sirjan. Payesh. 2004;4:61–7. [Google Scholar]
- 2.Berek J. Berek and Novak's Gynecology. Philadelphia: Lippincott Williams and Wilkins; 2012. [Google Scholar]
- 3.Shahrjerdi S, Shaych Hosaini R. The effect of 8 weeks stretching exercise on primary dysmenorrhea in 15-17 aged high school student girls in Arak. J Shahrekord Univ Med Sci. 2010;11:84–91. [Google Scholar]
- 4.Saadatabadi F, Bambaichi E, Esfarjani F. Effect of six weeks flexibility training on dysmenorrhea. J Isfahan Med Sch. 2010;28:109. [Google Scholar]
- 5.Mohammadi B, Azamian Jazi A, Fathollahi Shourabeh F. The effect of aerobic exercise training and detraining on some of the menstrual disorders in non-athlete students in Lorestan universities. Horiz Med Sci. 2012;18:5–12. [Google Scholar]
- 6.Nasri M, Barati A, Ramezani A. Comparison of aerobic training and pelvic floor muscle exercise on primary dysmenorrhea in adolescent girls. J Clin Nurs Midwifery. 2016;5:53–61. [Google Scholar]
- 7.Ortiz MI, Cortés-Márquez SK, Romero-Quezada LC, Murguía-Cánovas G, Jaramillo-Díaz AP. Effect of a physiotherapy program in women with primary dysmenorrhea. Eur J Obstet Gynecol Reprod Biol. 2015;194:24–9. doi: 10.1016/j.ejogrb.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Haidari F, Akrami A, Sarhadi M, Mohammad-Shahi M. Prevalence and severity of primary dysmenorrhea and its relation to anthropometric parameters. Hayat. 2011;17:70–7. [Google Scholar]
- 9.ACOG issues guide.lines on diagnosis and treatment of PMS. Womens Health. 2005;5:20–2. [Google Scholar]
- 10.Mohammadi H, Pouretezad M, Shokri E, Tafazoli M, Dastjerdi M, Siouki H. The effect of forearm kinesio taping on hand grip strength of healthy people. J Kerman Univ Med Sci. 2010;17:248–56. [Google Scholar]
- 11.Shavandi N, Taghian F, Soltani V. The effect of isometric exercise on primary dismenorrhea. Arak Med Univ J. 2010;13:71–7. [Google Scholar]
- 12.Blakey H, Chisholm C, Dear F, Harris B, Hartwell R, Daley AJ, et al. Is exercise associated with primary dysmenorrhoea in young women? BJOG. 2010;117:222–4. doi: 10.1111/j.1471-0528.2009.02220.x. [DOI] [PubMed] [Google Scholar]
- 13.Davaneghi S, Tarighat-Esfanjani A, Dahri M. Association of nutritional factors and physical activity with severity of primary dysmenorrheal pain. J Health Care. 2016;18:93–100. [Google Scholar]
- 14.Sehati F, Homaee M, Zudfekr L. Comparison of the prevalence of menstrual disorders (amenorrhea, oligomenorrhea, dysmenorrhea and premenstrual syndrome) female athlete and non-athlete students of Tabriz university. J Obstet Gynecol Infertil. 2014;16:14–21. [Google Scholar]
- 15.Heidarianpour A, Zamiri Dalir F, Shouride Yazdi M. The effects of eight week aerobic exercise on menstrual cycle disorders and hormones levels of FSH and LH. Journal of Sabzevar University of Medical Sciences. 2016;23(2):336–343. [Google Scholar]
- 16.Chantler I, Mitchell D, Fuller A. Diclofenac potassium attenuates dysmenorrhea and restores exercise performance in women with primary dysmenorrhea. J Pain. 2009;10:191–200. doi: 10.1016/j.jpain.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Aganoff JA, Boyle GJ. Aerobic exercise, mood states and menstrual cycle symptoms. J Psychosom Res. 1994;38:183–92. doi: 10.1016/0022-3999(94)90114-7. [DOI] [PubMed] [Google Scholar]
- 18.Harlow SD, Park M. A longitudinal study of risk factors for the occurrence, duration and severity of menstrual cramps in a cohort of college women. Br J Obstet Gynaecol. 1996;103:1134–42. doi: 10.1111/j.1471-0528.1996.tb09597.x. [DOI] [PubMed] [Google Scholar]
- 19.Guyton and Hall Textbook of Medical Physiology. Tehran: Rafiee Publication, Hall J; 2006. [Google Scholar]
- 20.American Academy of Pediatrics Committee on Adolescence, American College of Obstetricians and Gynecologists Committee on Adolescent Health Care, Diaz A, Laufer MR, Breech LL. Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Pediatrics. 2006;118:2245–50. doi: 10.1542/peds.2006-2481. [DOI] [PubMed] [Google Scholar]
- 21.Jamieson DJ, Steege JF. The prevalence of dysmenorrhea, dyspareunia, pelvic pain, and irritable bowel syndrome in primary care practices. Obstet Gynecol. 1996;87:55–8. doi: 10.1016/0029-7844(95)00360-6. [DOI] [PubMed] [Google Scholar]


