The infrapatellar branch of the saphenous nerve (IBSN) is purely sensory and innervates both the anteromedial aspect of the knee and the anterior-inferior portion of the knee capsule.1,2,7 The IBSN arises from the saphenous nerve in the adductor hiatus before piercing the fascia lata to become subcutaneous.7
Infrapatellar pain syndrome (IPS), also known as an infrapatellar nerve injury, is not a widely known syndrome. The IBSN in the literature is also known as prepatellar nerve. It is not a novel phenomenon. As early as 1945, surgeons were cautioned regarding potential surgical trauma to the IBSN.16
IPS can be caused by trauma, such as a fall on the knee or a direct blow to the knee joint,5,8,14 as well as by surgical procedures, such as arthroscopy, total knee replacement, bone–patellar tendon–bone or hamstring tendon harvest for anterior cruciate ligament (ACL) procedures, tibial nailing, and open procedures of the knee.16
The paramount problem with IPS is the potentially long time for a proper diagnosis of anterior knee pain syndrome. IPS is not often reported and can be overlooked or misdiagnosed as it develops.14 In the literature, we have found patients with a history of IPS lasting 75 and even 13 years.8 Gordon5 described IPS pain as being similar to a “toothache.”5 Figueroa et al3 reported 4 types of disturbance of the IBSN, including hypoesthesia, dysesthesia, painful neuroma, and reflex sympathetic dystrophy.
Case Report
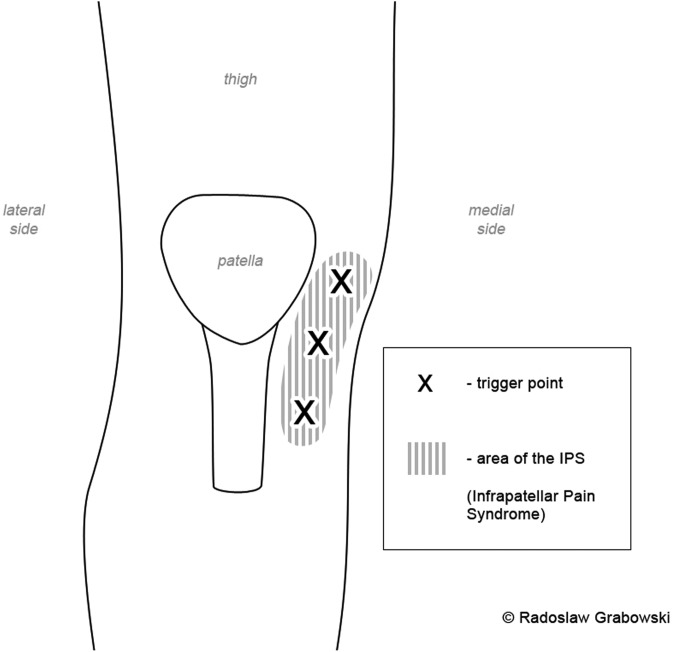
A 46-year-old patient had a history of chronic knee pain at the anteromedial region of his left knee joint for several years. This pain was present even at rest and increased during palpation of the skin at this region. We found 3 precise trigger points (Figure 1). The patient had a history of 3 surgeries on his left knee, but he denied any injury or significant trauma to his knee, such as a blow to the knee or a fall on the knee. The IPS described by the patient started after the first surgery.
Figure 1.
Schematic showing the trigger points.
1. In 2013, during arthroscopy: excision of the thickened medial and lateral synovial plicae and suprapatellar plica, shaving of anterior part of the knee, excision of infrapatellar bursa, microfracture of the tibial tuberosity
2. In 2014, again during arthroscopy: excision of the fibrosed medial and lateral synovial plicae, shaving of patellar ligament, excision of synovial plica at the basis of the patella
These 2 surgeries were performed in another hospital. Because of the pain and the lack of improvement, we decided to perform another arthroscopy.
3. In March 2015: 8 microfractures of femoral trochlea, 9 microfractures of medial femoral condyle, injection of lignocaine solution in the prepatellar area. We found the medial meniscus, lateral meniscus, ACL, and posterior cruciate ligament structures to be normal.
Despite these surgeries, the patient still complained about the pain and paraesthesia of the anteromedial part of his knee.
We palpated the 3 triggering points (Figure 1) for the pain. Injection of 3 mL of 1% lignocaine solution resulted in 2 weeks of relief. The injection was performed by moving the needle in the subcutaneous layer of the area, which was approximately 2.0 × 3.5 cm.
In March 2016, we decided to perform surgery. During the surgery, we dissected the branches of the IBSN (Figures 2 and 3). Macroscopically, we saw a neuroma (Figure 4). We injected 1% bupivacaine solution into the region of the neuroma (Figure 5). Next, we ligated the nerve and cut proximally to the neuroma (Figure 6). In addition, we smashed the ending of the branch using a Pean surgical instrument.
Figure 2.
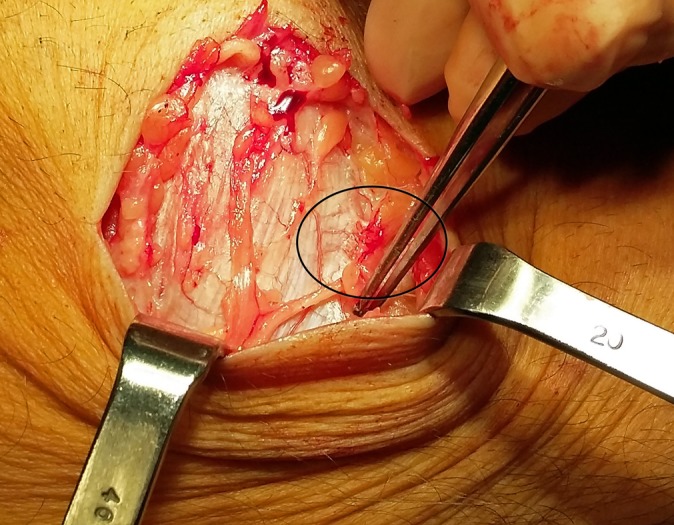
Infrapatellar branch of saphenous nerve during dissection. The neuroma is circled.
Figure 3.

Infrapatellar branch of saphenous nerve with neuroma (circled).
Figure 4.
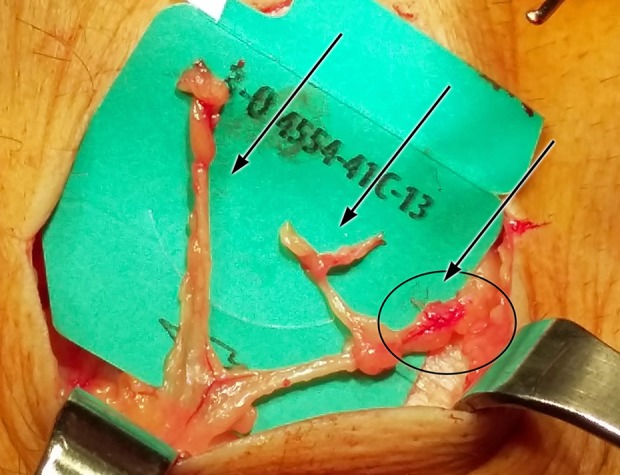
Infrapatellar branch of saphenous nerve showing the 3 branches (arrows).
Figure 5.
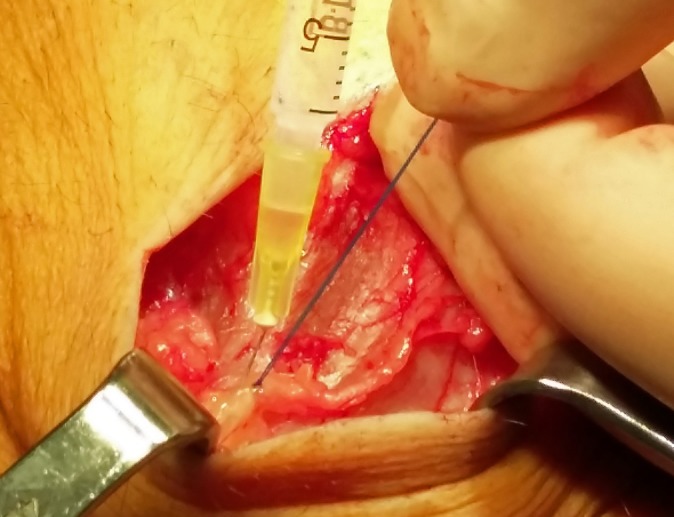
Infrapatellar branch of saphenous nerve during injection of bupivacaine solution.
Figure 6.

Infrapatellar branch of saphenous nerve after excision of the neuroma.
After the surgery, the patient no longer felt pain at the region of the trigger point, and we received histological confirmation of posttraumatic neuroma. We think that the neuroma began after the first surgery. After an 18-month follow-up, the patient is free of pain.
Discussion
IPS can be a posttraumatic and a postsurgical syndrome. In 1995, Mochida and Kikuchi11 found a 22% injury rate of the IBSN after knee arthroscopy. Despite being minimally invasive, arthroscopic surgery of the knee can be associated with postoperative pain in as many as 60% to 90% of patients. In 2013, Kerver et al9 reported that there are no safe zones for portal placement. We have only low-risk zones because of the high variability of the IBSN.
During arthroscopy-assisted ACL reconstruction, the incidence rate of the injury of the IBSN is higher than that during arthroscopy procedure alone. In 2015, de Padua et al12 reported that graft harvesting is not risk-free. While harvesting graft from hamstrings muscles for ACL reconstruction, Figueroa et al3 pointed out that injury to the IBSN was electrophysiologically detected in 68% of knees. Sanders et al15 reported that after hamstring harvesting, 74% had sensory disturbances. Papastergiou et al13 compared vertical and horizontal incisions for graft harvesting. They reported that the incidence rate of injuries to the IBSN during vertical incision was 39.7% and during horizontal incision was 14.9%. Gali et al4 recommended oblique incision for graft harvesting. Figueroa et al3 also reported that the presence of sensory loss associated with damage to the IBSN did not correlate with the size of the incision or the distance to the tibial tubercle. The injury mainly occurs during tendon harvesting. According to de Padua et al,12 harvesting only the semitendinosus tendon for the graft results in a lower (36.1%) injury rate than harvesting both the semitendinosus and gracilis tendons (58.1%).
There are many studies regarding the variants of the IBSN. The IBSN arises from the saphenous nerve and has 3 branches in the subcutaneous layer in the anteromedial part of the knee.16 The study performed by Kerver et al,9 which used a computer-assisted surgical anatomy mapping tool, showed high anatomical variability of the branches of the IBSN. One of the latest cadaveric studies on the anatomy of the IBSN showed that the oblique incision had the lowest nerve injury rate.6 The anatomy of the infrapatellar nerve varies from individual to individual and can even vary from left to right lower limb in any single individual.1
Thinking about the neuroma of the infrapatellar branch of the knee, it is important to remember the other nerves of this region: the lateral cutaneous nerve of the thigh, the intermediate cutaneous nerve of the thigh, and the anterior division of the medial cutaneous nerve of the thigh.11
We have found that the excision of the IBSN neuroma is a good treatment method. There are also other methods, such as cryoanalgesia. Lloyd et al10 proposed that cryoanalgesia was superior to other methods of peripheral nerve destruction, including alcohol neurolysis, phenol neurolysis, or surgical lesions.
Despite the fact that arthroscopy of the knee is a minimally invasive surgery, the incidence rate of IBSN injuries can be very high. In this case study, the pain (burning) started after the first surgery. It lasted for several years until the excision of the neuroma. Hyposensibility is one of the weakest types of IPS. We focused on the most disturbing and annoying symptoms, such as the burning sensation and sharp pain that presented even at rest and awakened the patient at night.
There is a need for more information regarding IBSN injury so that it can become more widely known among surgeons. Dissection and excision of the IBSN neuroma can be a successful treatment method.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.G. is a scientific consultant for Anika Therapeutics.
References
- 1. Arthornthurasook A, Gaew-Im K. Study of the infrapatellar nerve. Am J Sports Med. 1988;16(1):57–59. [DOI] [PubMed] [Google Scholar]
- 2. Le Corroller T, Lagier A, Pirro N, Champsaur P. Anatomical study of the infrapatellar branch of the saphenous nerve using ultrasonography. Muscle Nerve. 2011;44(1):50–54. [DOI] [PubMed] [Google Scholar]
- 3. Figueroa D, Calvo R, Vaisman A, Campero M, Moraga C. Injury to the infrapatellar branch of the saphenous nerve in ACL reconstruction with the hamstrings technique: clinical and electrophysiological study. Knee. 2008;15(5):360–363. [DOI] [PubMed] [Google Scholar]
- 4. Gali JC, Resina AF, Pedro G, et al. Importance of anatomically locating the infrapatellar branch of the saphenous nerve in reconstructing the anterior cruciate ligament using flexor tendons. Rev Bras Ortop. 2014;49(6):625–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gordon GC. Traumatic prepatellar neuralgia. J Bone Joint Surg Br. 1952;34-B(1):41–44. [DOI] [PubMed] [Google Scholar]
- 6. Henry BM, Tomaszewski KA, Pekala PA, et al. Oblique incisions in hamstring tendon harvesting reduce iatrogenic injuries to the infrapatellar branch of the saphenous nerve [published online June 1, 2017]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-017-4590-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hsu LP, Oh S, Nuber GW, et al. Nerve block of the infrapatellar branch of the saphenous nerve in knee arthroscopy: a prospective, double-blinded, randomized, placebo-controlled trial. J Bone Joint Surg Am. 2013;95(16):1465–1472. [DOI] [PubMed] [Google Scholar]
- 8. Ikpeme JO, Gray C. Traumatic prepatellar neuralgia. Injury. 1995;26(4):225–229. [DOI] [PubMed] [Google Scholar]
- 9. Kerver AL, Leliveld MS, den Hartog D, Verhofstad MH, Kleinrensink GJ. The surgical anatomy of the infrapatellar branch of the saphenous nerve in relation to incisions for anteromedial knee surgery. J Bone Joint Surg Am. 2013;95(23):2119–2125. [DOI] [PubMed] [Google Scholar]
- 10. Lloyd JW, Barnard JD, Glynn CJ. Cryoanalgesia. A new approach to pain relief. Lancet. 1976;2(7992):932–934. [DOI] [PubMed] [Google Scholar]
- 11. Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop Relat Res. 1995;(320):88–94. [PubMed] [Google Scholar]
- 12. de Padua VB, Nascimento PE, Silva SC, de Gusmao Canuto SM, Zuppi GN, de Carvalho SM. Saphenous nerve injury during harvesting of one or two hamstring tendons for anterior cruciate ligament reconstruction. Rev Bras Ortop. 2015;50(5):546–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Papastergiou SG, Voulgaropoulos H, Mikalef P, Ziogas E, Pappis G, Giannakopoulos I. Injuries to the infrapatellar branch(es) of the saphenous nerve in anterior cruciate ligament reconstruction with four-strand hamstring tendon autograft: vertical versus horizontal incision for harvest. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):789–793. [DOI] [PubMed] [Google Scholar]
- 14. Pendergrass TL, Moore JH. Saphenous neuropathy following medial knee trauma. J Orthop Sports Phys Ther. 2004;34(6):328–334. [DOI] [PubMed] [Google Scholar]
- 15. Sanders B, Rolf R, McClelland W, Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23(9):956–963. [DOI] [PubMed] [Google Scholar]
- 16. Trescot AM, Brown MN, Karl HW. Infrapatellar saphenous neuralgia: diagnosis and treatment. Pain Physician. 2013;16(3): E315–E324. [PubMed] [Google Scholar]