Abstract
Carpal instability is often related to ruptured or lax carpal ligaments. Wrist cineradiography has been shown to be a good modality for diagnosing carpal instability. To create uniformity in obtaining and assessing wrist cineradiography, a wrist cineradiography protocol is desirable. This protocol will focus on wrist cineradiography for diagnosing carpal instabilities. It describes the pathologic motions of the carpus and correlates these with a clinical diagnosis.
Level of evidence: III
Keywords: Carpal instability, fluoroscopy, scapholunate dissociation, scapholunate ligament, wrist cineradiography
Introduction
Carpal instability is often related to ruptured or lax ligaments (Garcia-Elias et al., 1995; Short et al., 2007; Watson and Ballet, 1984) and can be classified as: carpal instability dissociative (CID), carpal instability non-dissociative (CIND), and carpal instability combined or complex (Garcia-Elias, 1997; Lichtman and Wroten, 2006; Wolfe et al., 2012; Wright et al., 1994).
The best known form of a CID is scapholunate dissociation (SLD), which is usually provoked by a fall onto the outstretched hand. It may also lead to radiocarpal and midcarpal osteoarthritis (O’Meeghan et al., 2003; Watson and Ballet, 1984). CIND describes a carpal instability between the carpal rows and is often caused by rupture of hyperlax carpal ligaments.
Wrist cineradiography has been shown to be a good modality for diagnosing carpal instability (Langner et al., 2015; Pliefke et al., 2008; Sulkers et al., 2014a). To create uniformity in obtaining and assessing wrist cineradiography, a protocol is desirable. To this end, knowledge of normal carpal kinematics and the kinematics of the various patterns of carpal instability is crucial in the assessment of wrist cineradiography and has been extensively described. This protocol will focus on wrist cineradiography for diagnosing carpal instabilities. It describes the pathologic motions of the carpus and correlates these with a clinical diagnosis.
Wrist cineradiography
To obtain a wrist cineradiography a digital substraction angiography imager, a (mini) C-arm, or standard fluoroscopy with a minimum frequency of eight images per second is needed. Maximum radiation protection, including lead gloves, is advised to protect the examiner from radiation. It is important to familiarize the patient with the examination and to compare the injured wrist with the non-injured wrist; the non-injured wrist is always examined first (Appendix 1, available online). The patient’s arm is supported and held by the examiner.
Both postero-anterior (PA) and lateral views should be taken. To obtain the PA view, the patient’s shoulder should be held in 90° of abduction and the elbow in 90° of flexion. The PA images should include a neutral view and views in radial and ulnar deviation. This is followed by the lateral views with the patient’s upper arm alongside the body and the elbow in 90° of flexion. The lateral views should be taken in neutral, in flexion and extension, and in radial and ulnar deviation. While doing this, active wrist movements should be compared with passive ones. These movements may differ during active movement as the carpals are subject to different tension forces from the tendons, which have an additional stabilizing effect on the wrist during active motion (Milner, 2002). After obtaining the carpal movements, provocation tests are done while viewing the wrist, first in PA and then lateral projections (Appendix 1). A few provocation tests (e.g. Watson test) are not suitable for cineradiography, as the radiation protection gloves worn by the examiner block the field of view.
It is important for the investigator to establish if the patient’s complaints are due to a trauma, and differences between the wrists should be anticipated. If no injury is sustained, then the same findings (e.g. due to CIND) may be present in both the symptomatic and asymptomatic wrist.
PA view: neutral position
The radius and ulna must be projected next to each other. The styloid process of the radius must be seen as a single contour and the styloid process of the ulna must be projected most medially. The third metacarpal must be in line with the radius (Brink et al., 2010). The proximal border of the field of view should be just proximal to the distal radio-ulnar joint and the distal border at the proximal third of the metacarpals.
When in a neutral position, the carpals can be assessed the same way as in a conventional PA radiograph. Signs of a static SLD are a widened scapholunate (SL) distance (⩾3 mm) and the cortical ring sign whereby increased flexion of the scaphoid makes the waist of the scaphoid look like a ring (Figure 1). Measurements can be performed from a Picture Archiving Communication System (PACS, Philips Medical Systems, Best, The Netherlands). With a digital ruler, the SL distance can be digitally measured, starting from the middle of the medial facet of the scaphoid to the lunate (Totty and Gilula, 1992). Also, if the lunate is extended, known as a dorsal intercalated segment instability (DISI), this is an indicator of static SLD. In this configuration, the lunate appears more triangular-shaped and is projected over the proximal pole of the capitate (Sulkers et al., 2014a). Finally, disruption of the first and second lines of Gilula is also a sign of a static SLD.
Figure 1.

Conventional radiography, PA view. Suspected static SLD.
A displaced lunotriquetral junction and/or the lunate in a more flexed position (known as a volar intercalated segment instability (VISI)), are signs of a lunotriquetral dissociation or might be a sign of a radial-, ulnar-, or combined CIND. This can be recognized by a box-shaped lunate (Linn et al., 1990; Ritt et al., 1998).
PA view: radial-ulnar deviation (RUD)
After the wrist has been examined in a neutral position, it is then actively moved to maximum radial deviation followed by maximum ulnar deviation under continuous fluoroscopy and within the limits of pain. To obtain a possibly increased range of motion, the examiner repeats these movements passively. This should be repeated until all movements of the carpal bones have been visualized and assessed. In a normal wrist, the proximal carpal row (PCR) will flex and extend during RUD and all movements within the PCR are synchronous (Video 1, available online).
A dynamic SLD can only be seen during motion of the wrist and if there is no suspicion of static SLD in neutral position. If the movement between the scaphoid and lunate is not synchronous and a diastasis between the two bones can be provoked, then a dynamic SLD is suspected (Video 2). In this, the lunate moves partially with the scaphoid and the SL gap changes (Appendix 2, available online). It is important to note that the gap between the scaphoid and lunate is usually not at its widest in extreme ulnar deviation. Moreover, in some cases, the gap between these bones may be normal in extreme ulnar deviation. Finally, the lunate will not flex normally during radial deviation.
When moving the hand in RUD, a widening of the scaphotrapezium-trapezoid joint is sometimes observed – this can be an indication of a radial-sided palmar CIND. Similarly, on radial deviation, a widened triquetrum-hamate joint can be observed and might be an indication of an ulnar-sided palmar CIND (Garcia-Elias, 2008; Wolfe et al., 2012).
The sudden ‘clunk’ of the PCR from flexion into extension suggests a combined CIND (Lichtman and Wroten, 2006).
If a nonsynchronous movement between the lunate and triquetrum can be provoked during radial deviation, then a lunotriquetral dissociation may be suspected (Böttcher et al., 2005). In this, the triquetrum will move more distally than the lunate during radial deviation (Video 3, available online).
Increased range of motion and a hypermobile lunotriquetral (LT) joint can be found in hypermobile patients (Garcia-Elias et al., 1995, 2003).
Lateral view: neutral position
In this view, the proximal border of the field should be just proximal to the distal radio-ulnar joint and the distal border at the level of the proximal third of the metacarpals. The radius and ulna should be projected over one another. The lunate bone should be covered by the scaphoid and the distal pole of the scaphoid covered by the pisiform (Brink et al., 2010).
An increased SL angle (⩾60°) or increased radiolunate angle (⩾12°) in which the lunate is in an extended position (DISI) may indicate a static SLD (Sulkers et al., 2014a).
In patients with a dorsally displaced distal radius fracture, the lunate can be rotated palmarly to compensate for the increased inclination of the distal radial joint surface. The capitate is then collinear with the lunate, but dorsal to the longitudinal axis of the radius. Alternatively, the increased inclination of the distal radial joint surface will be compensated by relative flexion of the capitate, whereby the capitate is collinear with the radius, but dorsal to the longitudinal axis of the radius (Figure 2).
Figure 2.
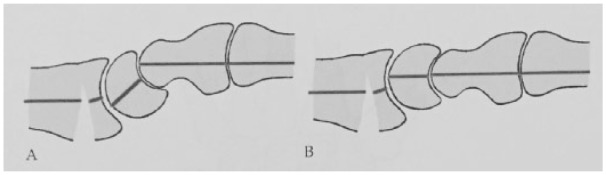
Adaptive CIND. In patients with a dorsally displaced distal radius fracture, the increased inclination can be compensated by a relative flexion of the capitate. In this movement the capitate is collinear with the radius, but dorsal to the longitudinal axis of the radius (a). Alternatively, the lunate can be rotated palmarly to compensate for the increased inclination of the distal radial joint surface. The capitate is collinear with the lunate, but dorsal to the longitudinal axis of the radius (b).
These compensations suggest an adaptive CIND (Lichtman and Wroten, 2006).
Signs of a VISI, in which the lunate and scaphoid are in flexion and the posterior horn of the lunate may project onto the capitate, suggest a lunotriquetral dissociation (Linn et al., 1990; Ritt et al., 1998). However, a VISI pattern may also present in patients with radial-, ulnar-, or combined CIND.
Lateral view: flexion/extension
After examining the wrist in neutral position in the lateral view, the wrist must be moved actively from extension to flexion within the limits of pain. This is repeated in a passive manner by the examiner to possibly achieve an increased range of motion. This should be repeated until all movements of the carpal bones have been visualized and assessed.
In normal circumstances where the SL ligament is intact, the lunate moves from extension to flexion and passes the 0° line of the radiolunate angle without any problems (Video 4). However, if the lunate does not pass the 0° line of the radiolunate angle during flexion, there is a high probability of dynamic SL instability (Video 5 and Appendix 2, available online). A lunate that stays in an extended position during flexion implies a static SLD.
Finally, if the capitate can flex or extend more than 90° then a hypermobile wrist is suspected.
Lateral view: RUD
After flexion/extension in the lateral view, the wrist should be moved actively from ulnar deviation to radial deviation under continuous fluoroscopy within the limits of pain. Subsequently, the examiner obtains passive RUD in order to achieve a possibly increased range of motion.
In a normal wrist, the lunate will flex and extend during RUD (out-of-plane movement of the PCR) (Video 4). However, if the lunate does not flex fully and is in a more extended position during radial deviation, a dynamic SLD may be suspected (Video 6, available online) (Linn et al., 1990; Ritt et al., 1998).
If the lunate stays in an extended position during radial deviation then a static SLD is present. If rotation of the PCR from flexion to extension is jerky this may indicate a radial- or ulnar-sided palmar CIND.
If the PCR is flexed during radial deviation, while during ulnar deviation, the PCR clunks into extension (as in a palmar CIND), a combined CIND is suspected. In addition, extreme ulnar deviation causes a dorsal subluxation of the capitate, similar to dorsal CIND.
If intact carpal ligaments are incapable of preventing excessive dorsal translation of the capitate and ulnar deviation produces a clunk on dorsal translation, a dorsal CIND is suspected (Lichtman and Wroten, 2006).
Provocation tests
The midcarpal shift test can be performed to diagnose a palmar CIND (Lichtman and Wroten, 2006). The patient’s wrist is placed in a neutral position. Palmar translation is then applied so that the PCR is flexed. In this flexed position, the wrist must be simultaneously axially loaded and ulnarly deviated. By adding ulnar deviation the PCR is forced into extension. This motion may produce a rapid ‘catch-up clunk’ in which the PCR jumps from flexion into extension (Lichtman and Wroten, 2006). The test result is positive for a palmar CIND if a painful clunk occurs and reproduces the patient’s symptoms. If the clunk does not reproduce the patient’s symptoms, the diagnosis of hypermobile or lax wrist can be made (Video 7, available online). This test can be performed in both the PA and lateral views. In the PA view, the lunate and scaphoid will always move synchronously.
During the anterior drawer test the distal carpal row (DCR) is translated into a palmar direction. On the PA view, a widening of the scaphotrapezium–trapezoid joint can be seen in patients with a radial-sided palmar CIND. In these patients, a palmar capitolunate subluxation can be seen on the lateral view (Video 8, available online).
The dorsal capitate displacement stress test (Mayfield et al., 1980) or posterior drawer test are useful for diagnosing a dorsal CIND. The examiner applies dorsally directed pressure, while at the same time applying longitudinal traction to the wrist. In the lateral view cineradiography shows dorsal subluxation of the PCR and almost complete dorsal subluxation of the capitate from the lunate, in which the capitate may be brought beyond the dorsal lip of the lunate (Garcia-Elias, 2008; Lichtman and Wroten, 2006) (Video 8). The diagnosis of capitolunate instability pattern is made if instability at the capitolunate joint reproduces the patient’s symptoms (Lichtman and Wroten, 2006).
Discussion
This protocol describes how we have performed wrist cineradiography since our institute implemented it as a diagnostic tool for diagnosing carpal instabilities in 1987. The protocol is based on the sparse literature that has been published since Arkless et al. first described wrist cineradiography in 1966 (Arkless, 1966).
With its sensitivity of 85%–90% and specificity of 90%–97%, wrist cineradiography has been shown to be a good modality for diagnosing SLDs (Langner et al., 2015; Pliefke et al., 2008; Sulkers et al., 2014a). Additionally, using a score sheet (Appendix 2), a recent study showed excellent inter-observer correlations (κ = 0.84) and good to excellent intra-observer correlations (κ = 0.72–0.80) (Sulkers et al., 2014b).
Very few studies comparing cineradiography with the reference standard (arthrotomy or arthroscopy) for diagnosing lunotriquetral dissociation have been published (Böttcher et al., 2005). No sensitivity and specificity are calculated in these studies. Additionally, there is no gold standard for diagnosing a CIND or hypermobile wrist, as these are clinical diagnoses.
Cineradiography is the only available dynamic imaging technique that is able to detect a CID in real time, and therefore it is the only technique that can give information about the functional status of these joints. Carrying out stress tests (e.g. midcarpal shift test) under cineradiography can easily confirm the presence of a CIND, as the carpal kinematics typical of these tests are easily observed. Cineradiography is non-invasive, has relatively low costs, is widely available, and can be quickly performed.
A disadvantage of cineradiography is that patient and, to a lesser extent, the observer are both exposed to radiation with an average dose area product of 110 cGy × cm2 (Pliefke et al., 2008), which is three times the dose of a chest X-ray (Dutch Institute of Public Health and Environment). Fluid movements are sometimes hard to observe as pulsed radiation is often used during cineradiography in order keep the dose area product as low as possible. Also at the acute stage, physical examination during cineradiography may be too painful and could induce false negatives. Finally, it takes time to learn how to obtain a good study and can therefore be operator dependent. However, this should be evaluated further, as no data on this topic are available in the literature.
Physical examination and conventional radiographs remain essential in the primary work-up for carpal instability. Positive findings suggest the presence of carpal instability. However, in the diagnosing of SLDs, due to the low sensitivity of the scaphoid shift test (Marx et al., 1999; Prosser et al., 2011) and of conventional radiographs (with or without static provocation tests, e.g. ulnar deviation views) (Sulkers et al., 2014a), we recommend cineradiography if there is clinical suspicion of CID.
Cineradiography is a qualitative rather than a quantitative tool, and more research is needed to determine its exact role in diagnosing carpal instability.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Arkless R. Cineradiography in normal and abnormal wrists. AJR. 1966, 96: 837–44. [DOI] [PubMed] [Google Scholar]
- Böttcher R, Mutze S, Lautenbach M, Eisenschenk A. Diagnosis of lunotriquetral instability. Handchir Mikrochir Plast Chir. 2005, 37: 131–6. [DOI] [PubMed] [Google Scholar]
- Brink PRG, Bransz N, Deijkers RLM, et al. Dutch guideline for distal radius fractures: diagnoses and treatment. Utrecht, The Netherlands, Nederlandse Vereniging voor Heelkunde, 2010. [Google Scholar]
- Garcia-Elias M. The treatment of wrist instability. J Bone Joint Surg Br. 1997, 79: 684–90. [DOI] [PubMed] [Google Scholar]
- Garcia-Elias M. The non-dissociative clunking wrist: a personal view. J Hand Surg Eur. 2008, 33: 698–711. [DOI] [PubMed] [Google Scholar]
- Garcia-Elias M, Pitagoras T, Gilabert-Senar A. Relationship between joint laxity and radio-ulno-carpal joint morphology. J Hand Surg Eur. 2003, 28: 158–62. [DOI] [PubMed] [Google Scholar]
- Garcia-Elias M, Ribe M, Rodriguez J, et al. Influence of joint laxity on scaphoid kinematics. J Hand Surg Br. 1995, 20: 379–82. [DOI] [PubMed] [Google Scholar]
- Langner I, Fischer S, Eisenschenk A, Langner S. Cine MRI: a new approach to the diagnosis of scapholunate dissociation. Skeletal Radiol. 2015, 44: 1103–10. [DOI] [PubMed] [Google Scholar]
- Lichtman DM, Wroten ES. Understanding midcarpal instability. J Hand Surg Am. 2006, 31: 491–8. [DOI] [PubMed] [Google Scholar]
- Linn MR, Mann FA, Gilula LA. Imaging the symptomatic wrist. Orthop Clin North Am. 1990, 21: 515–43. [PubMed] [Google Scholar]
- Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980, 5: 226–41. [DOI] [PubMed] [Google Scholar]
- Marx RG, Bombardier C, Wright JG. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? J Hand Surg Am. 1999, 24: 185–93. [DOI] [PubMed] [Google Scholar]
- Milner TE. Adaptation to destabilizing dynamics by means of muscle cocontraction. Exp Brain Res. 2002, 143: 406–16. [DOI] [PubMed] [Google Scholar]
- O’Meeghan CJ, Stuart W, Mamo V, et al. The natural history of an untreated isolated scapholunate interosseus ligament injury. J Hand Surg Br. 2003, 28: 307–10. [DOI] [PubMed] [Google Scholar]
- Pliefke J, Stengel D, Rademacher G, et al. Diagnostic accuracy of plain radiographs and cineradiography in diagnosing traumatic scapholunate dissociation. Skeletal Radiol. 2008, 37: 139–45. [DOI] [PubMed] [Google Scholar]
- Prosser R, Harvey L, LaStayo P, et al. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. J Physiother. 2011, 57: 247–53. [DOI] [PubMed] [Google Scholar]
- Ritt MJPF, Linscheid RL, Cooney WP, et al. The lunotriquetral joint: kinematic effects of sequential ligament sectioning, ligament repair, and arthrodesis. J Hand Surg Am. 1998, 23: 432–45. [DOI] [PubMed] [Google Scholar]
- Short WH, Werner FW, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: part III. J Hand Surg Am. 2007, 32: 297–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulkers GSI, Schep NWL, Maas M, et al. The diagnostic accuracy of wrist cineradiography in diagnosing scapholunate dissociation. J Hand Surg Eur. 2014. a, 39: 263–71. [DOI] [PubMed] [Google Scholar]
- Sulkers GSI, Schep NWL, Maas M, et al. Intraobserver and interobserver variability in diagnosing scapholunate dissociation by cineradiography. J Hand Surg Am. 2014. b, 39: 1050–4. [DOI] [PubMed] [Google Scholar]
- Totty WG, Gilula LA. Imaging of the hand and the wrist. The traumatised hand and wrist. W.B. Saunders, 1992: 1–8. [Google Scholar]
- Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984, 9: 358–65. [DOI] [PubMed] [Google Scholar]
- Wolfe SW, Garcia-Elias M, Kitay A. Carpal instability nondissociative. J Am Acad Orthop Surg. 2012, 20: 575–85. [DOI] [PubMed] [Google Scholar]
- Wright TW, Dobyns JH, Linscheid RL, et al. Carpal instability nondissociative. J Hand Surg Br. 1994, 19: 763–73. [DOI] [PubMed] [Google Scholar]


