ABSTRACT
A scoping review was performed to identify factors that may lead to human papillomavirus (HPV) vaccine hesitancy among women in low- and middle-income countries in South East Asian Region (SEAR) and Western Pacific Region (WPR). A systematic search of English and non-English articles using Pubmed, EMBASE, PsycINFO, Cochrane, MEDLINE, and CINAHL plus was conducted. Only 63 studies conducted in SEAR and WPR were included from inception until December 2016. Results of these studies have shown that poor awareness and knowledge of practices on cervical cancer prevention was evident in both SEAR and WPR. Concerns on safety and efficacy of the vaccine, and costs in getting vaccinated were significant barriers. Most women stated that they needed more information, and strongly welcomed a physician's recommendation in both geographical regions. Women also felt they have a low risk of acquiring HPV infection and cervical cancer. Most women in SEAR and WPR were unable to decide on whether to accept HPV vaccination.
KEYWORDS: human papillomavirus, South East Asian region, vaccine hesitancy, Westerns Pacific region
Introduction
Cervical cancer accounts for an estimated 528,000 of female deaths per year, with more than 85% of the global burden occurring in less developed regions of the world.1,2 To date, Africa and certain parts of South America have the highest incidence rates in cervical cancer, followed by the South East Asia (SEAR) and Western Pacific (WPR) regions with an age-standardised rate (ASR) of 21.99 (per 100,000) in India, and 34.51 (per 100,000) in Papua New Guinea.1
The human papillomavirus (HPV) is one of the most common sexually-transmitted infections worldwide, with an estimated 290 million women being infected.3 It has been acknowledged as the causative agent for the development of cervical cancer, with subtypes 16 and 18 consistently linked to 70% of cervical cancer cases globally, while subtypes 31, 33, 45, 52, and 58 responsible for another 20% of cervical cancer cases.4-6
The licensure of the HPV vaccine provided a major step forward in reducing the global burden of both cervical cancer and HPV infection. Three vaccines have been approved by the FDA: the bivalent vaccine, Cervarix® and the quadrivalent vaccine, Gardasil® in 2006 with the more recent 9-valent vaccine, Gardasil® 9 in 2014.6 From June 2006 to October 2014, around 118 million women have been targeted for HPV vaccination worldwide.7 Generally, the target population for HPV immunisation are young adolescent girls between nine to 14 years of age, ideally before sexual debut.8 According to WHO, older women (aged ≥ 15 years old), immunocompromised or HIV infected women are also recommended to undergo HPV vaccination.9
HPV immunisation programs and educational campaigns differ markedly across countries, and there have been concerns on rates of vaccination uptake since its licensure in 2006.7 Countries of the SEA and WP regions are mostly made up of low- to middle-income countries (LMIC), hence, representing a population highly at risk of cervical cancer. In addition to this, although the HPV vaccine has been approved and is commercially available in these countries (except China), uptake among the targeted population in these countries is expected to be low.7,10-18 Up until October 2014, 47 million girls (aged between 10–20 years old) have received the full dose of the HPV vaccine, and 59 million have received at least one dose, but only 2.7 million of these females were from less developed regions.7,16 This leaves a large population from less-developed countries largely unprotected from HPV infection and cervical cancer.7,16
Since 2006, there has been a proliferation of studies examining factors predicting vaccine acceptability and decision-making among different key stakeholders, which includes the women themselves, their parents, and healthcare professionals. Hence, the objectives of this review are to: 1) systematically review all influencing factors predicting HPV vaccine acceptability among women in SEAR and WPR; 2) provide a summarised literature of evidence on these factors; and 3) suggest recommendations that can improve HPV vaccine acceptability and diffuse any barriers identified in this review.
Methods
Review protocol
To ensure that the scoping review methods are reproducible, transparent, and devoid of bias in selective outcome reporting, a review protocol was developed a priori. The protocol, and inclusion and exclusion criteria are available from the University of York Centre for Reviews and Dissemination at the following website: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016035749.
Search strategy
Highly relevant studies were identified by systematically searching electronic databases and scanning the reference lists of articles. The databases utilised for screening of primary literature from inception until December 2016 were Pubmed, EMBASE (Ovid), PsycINFO (Ovid), Cochrane, MEDLINE (EBSCOhost), and CINAHL Plus (EBSCOhost). To ensure all relevant influential factors were captured in the search strategy, a broad search was conducted in PubMed with the following MesH terms “papillomavirus infections” and “female”, “papillomavirus vaccines” and “health knowledge OR attitudes OR practice”,. The search strategies in the other remaining databases are available in S1 Table.
Inclusion criteria
A study was considered eligible for inclusion if it had the following study and reporting characteristics:
-
a)
Types of studies: Research investigations assessing the influencing factors in HPV vaccine acceptability. This includes studies determining the awareness, knowledge, attitudes and beliefs, perceptions, opinions, and practices towards HPV vaccination. No language or publication date restrictions were imposed. Non-English articles were included if sufficient information was available in the abstract section. Only peer-reviewed articles conducted in World Health Organization (WHO) SEAR and WPR, were eligible for review and inclusion.
-
b)
Types of participants: Targeted populations for HPV vaccination programs which include young adolescent girls between nine to 14 years of age, women aged ≥ 15 years old, and HIV infected or immunocompromised women. Third party individuals who may influence a woman's decision in taking the vaccine, such as healthcare workers and female parents, were also considered.
-
c)
Types of outcome measures: Description of either awareness, knowledge, attitudes, beliefs, perceptions, concerns and/or practices of a women with regard to HPV-related issues.
Study selection
Articles returned from the initial search strategy were screened by reading the title and abstracts. Studies considered eligible for inclusion were then reviewed by reading the full-text articles before final inclusion in the review. Disagreements and uncertainties about study inclusion were resolved by discussion by three reviewers (DS, YYY and CPY). If no agreement could be reached, the remaining two reviewers (TK and PSS) were consulted in order to reach consensus. The final number of included studies were determined by three reviewers (DS, TK and PSS). Articles included in the review were saved into EndNote reference manager software, version X7 and duplicates were removed.
Data extraction
Each quantitative study was subjected to data extraction using a pre-defined data extraction form. The extraction form was developed in an Excel spreadsheet, and piloted from two trial reports beforehand to ensure suitability for use. Information was extracted from each included study on:
-
a)
Study characteristics: Study country, objectives of the research, recruitment site, study design and research period, respondents, measurement tool(s), outcomes measured, and conclusions.
-
b)
Participant characteristics: sample size, respondent's age (mean/range), place of residence, socioeconomic background, marital status, number of children, sexual debut, sexual history and HPV vaccination and/or Pap Smear status.
-
c)
Results: History of Pap Smear (normal and abnormal), components of awareness, knowledge, attitudes and beliefs assessed, willingness to vaccinate, source(s) of information, factors influencing decision to consider or reject vaccination, and additional comments.
Three reviewers (DS, YYY and CPY) extracted the relevant data from each included study, and two review authors checked the extracted data (TK and PSS). Authors TK and PSS independently appraised the paper and were consulted to reach consensus. No attempt was made to seek additional information from the included primary studies. The data extraction form with details extracted from each included study is available in S2 Table.
Data analysis
Synthesis of literature findings was conducted by reading full-text articles of included studies, identifying influencing factors in HPV vaccine acceptance, recognising similarities and differences between studies, and pooling together similar reporting measures and outcomes across studies. All relevant influencing factors were thematically categorised and presented using a descriptive approach.
Results
A total of 63 primary research studies were included for review, with over 90% of the articles in English (57/63) and five in Korean.19-23 Hong Kong,14,24-31 Korea,17,19-23,32-35 and Malaysia15,35-42 contributed to 44% (28/63) of the studies, while the remaining studies were fairly distributed over other countries such as Taiwan,12,35,43-47 Australia,4,48-52 China,10,53-57 India,13,58,59 Japan,60-62 Singapore,18,63 Philippines, Cambodia, Nepal, and Vietnam.5,64-66 Publication dates ranged between 2006 and 2016 (Fig. 1), with publications on factors that influence women in making an informed decision on HPV vaccination more commonly seen between year 2010 and 2011.
Figure 1.
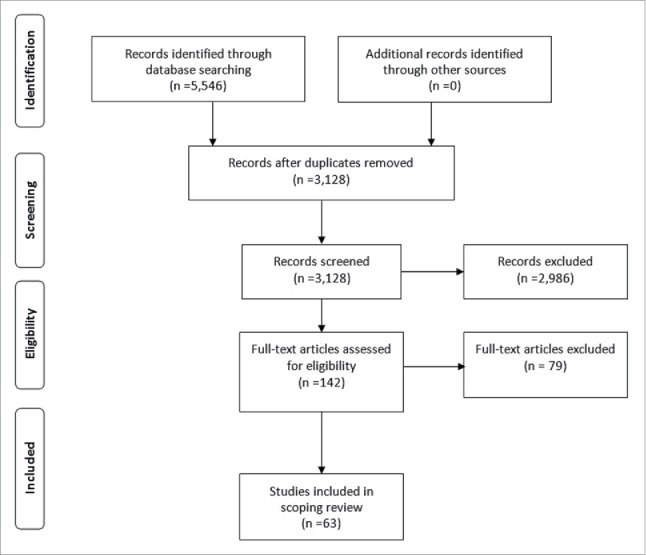
PRISMA Flowchart for identification and inclusion of articles in scoping review.
Study respondents were mostly targeted populations for HPV immunisation, which includes young girls between nine to 14 years of age, and women aged 15 years and older. All were healthy except for one study that recruited women with physical disabilities.43 The respondents were recruited from a variety of settings: healthcare which includes obstetrics and gynaecology clinics,4,15,20,24,38,43,46,58,60 women's clinic57 university health centres,25,41,54,59,67 community or social settings,10,14,19,21,26,28,30-32,35,37,39,45,48-52,55,56,61,62,64-66,68 and educational settings which includes colleges,17,44,47 schools17,27,28,40,69,70 and universities.11-13,18,33,36,42,71
About 90% (57/63) of the studies utilised descriptive, cross-sectional surveys, while other studies used a qualitative approach.30,32,42,68 and mixed-methods approach.28,66 Questionnaires (53/63) were largely employed for reporting measures; while the remaining studies used face-to-face interviews35,36,63 computer-assisted telephone interviews,26,50,51,63 focus group discussions,32 or a combination of interviews and discussions.30,68 The total sample size for all included studies was 62,296, with response rates ranging from 34.3% to 99.3%.
The majority of included articles examined (41/63) attitudes and beliefs towards vaccination, and awareness and knowledge levels related to practices and preventive measures of HPV infection, as shown in Table 1. Knowledge level toward HPV vaccination was assessed in about 15 studies details of which are described in Table 1.
Table 1.
Outcomes measured in included studies.
| Outcomes measured |
||||
|---|---|---|---|---|
| Study | Country | Awareness | Knowledge | Attitudes and beliefs |
| Abudukadeer A et al., 201554 | China | √ | √ | |
| Al-Dubai SAR et al., 201037 | Malaysia | √ | √ | |
| Al-Naggar RA et al., 201041 | Malaysia | √ | √ | |
| Al-Naggar RA et al., 201138 | Malaysia | √ | √ | |
| Bang KS et al., 201118 | Korea | √ | ||
| Chan KKL et al., 201227 | Hong Kong | √ | ||
| Charakorn C, 201166 | Thailand | √ | √ | |
| Choi HCW et al., 201413 | Hong Kong | √ | ||
| Chow S-N et al., 201034 | Korea, Malaysia, Taiwan and Thailand | √ | √ | √ |
| Egawa-Takata T et al., 201560 | Japan | √ | √ | |
| Egawa-Takata T et al., 201659 | Japan | √ | ||
| Ezat SWP et al., 201314 | Malaysia | √ | ||
| Feng S et al., 201256 | China | √ | √ | |
| Giles M, 200651 | Australia | √ | √ | |
| Gu C et al., 201553 | China | √ | √ | √ |
| Hong Y et al., 201352 | China | √ | √ | |
| Hsu Y-Y et al., 200911 | Taiwan | √ | ||
| Hsu Y-Y et al., 201045 | Taiwan | √ | ||
| Johnson DC et al., 201464 | Nepal | √ | √ | |
| Juntasopeepun P et al., 201170 | Thailand | √ | ||
| Juntasopeepun P et al., 201271 | Thailand | √ | √ | |
| Juntasopeepun P et al., 201210 | Thailand | √ | √ | |
| Kang H-Y et al., 201132 | Korea | √ | √ | |
| Kang HS et al., 201016 | Korea | √ | ||
| Kang HS et al., 201031 | Korea | √ | ||
| Kang HS et al., 201133 | Korea | √ | ||
| Kim H-W et al., 201219 | Korea | √ | √ | |
| Kruiroongroj S et al., 201469 | Thailand | √ | ||
| Kuo PF et al., 201443 | Taiwan | √ | ||
| Kwan TTC et al., 200823 | Hong Kong | √ | √ | |
| Kwan TTC et al., 201627 | Hong Kong | √ | √ | |
| Kyu E et al., 201420 | Korea | √ | ||
| Lan Y-L et al., 201344 | Taiwan | √ | ||
| Lee A et al., 201426 | Hong Kong | √ | ||
| Lee E-J et al., 201121 | Korea | √ | √ | |
| Lee PWH et al., 200729 | Hong Kong | √ | √ | |
| Li J et al., 200955 | China | √ | √ | |
| Li SL et al., 201368 | Hong Kong | √ | ||
| McNair R et al., 200848 | Australia | √ | √ | |
| Miyagi E et al., 201461 | Japan | √ | √ | |
| Montgomery MP et al., 201557 | India | √ | √ | |
| Park J-S et al., 201122 | Korea | √ | √ | √ |
| Paul P et al., 201265 | Vietnam | √ | √ | |
| Pitts M et al., 200962 | Singapore | √ | √ | √ |
| Pitts M et al., 200750 | Australia | √ | √ | √ |
| Rashid S et al., 201612 | India | √ | √ | √ |
| Sam I-C et al., 200940 | Malaysia | √ | √ | √ |
| Siddhartar J et al., 201458 | India | √ | √ | |
| Siu JY-M, 201467 | Hong Kong | √ | ||
| Tu Y-C et al., 201546 | Taiwan | √ | √ | |
| Tung ILY et al., 201647 | Australia | √ | √ | |
| Wadhera P et al., 20145 | Cambodia | √ | ||
| Wang LDL et al., 201525 | Hong Kong | √ | ||
| Weisberg E, 20094 | Australia | √ | √ | √ |
| Wong LP et al., 201035 | Malaysia | √ | √ | √ |
| Wong LP, 201136 | Malaysia | √ | √ | |
| Wong LP et al., 201639 | Malaysia | √ | √ | |
| Wong WCW et al., 200924 | Hong Kong | √ | √ | |
| Yen CF et al., 201142 | Taiwan | √ | ||
| Young AM et al., 201063 | Philippines | √ | ||
| Yu Y et al., 20169 | China | √ | √ | |
| Zhuang QY et al., 201617 | Singapore | √ | √ | |
Awareness
Awareness among women on HPV infection, HPV vaccine, and cervical cancer
Respondents' awareness to HPV related issues were investigated in 46% of included studies, in which 83% assessed awareness of HPV infection,5,10,24,30,33,38,39,41-43,46,47,51-58,63,65,67,69 38% on HPV vaccine,23,38,41,46,53-55,57,59,62,69 31% on cervical cancer,24,35,42,53-55,58,59,65 and one study on awareness of genital warts.41 In summary, poor awareness levels on aspects of HPV was identified across studies, with awareness ranging between 10% and 40% among study respondents.
Women's awareness on cervical cancer was generally better compared to HPV infection and vaccine,35,42,53-55,58,59,65 where more women had heard of cervical cancer compared to its vaccination or causative agent. In addition, female university students were twice as likely to have heard of HPV infection, HPV vaccine, and cervical cancer23,33,42,46,54 compared to women recruited from healthcare30,38,67 or community settings.5,53,55,63 Awareness levels were similar among women recruited from healthcare, community, and school settings. Only one study reported that women recruited online showed better awareness, compared to women attending a healthcare facility, household recruitment, or an institution of higher learning.62 Those with university education or higher were 16% more likely to be aware of HPV infection and vaccine in one study.43 Those with higher monthly household incomes also had better awareness on HPV infection and vaccine by 12% in one study.43
Awareness levels of female sex workers were similar5,53 compared to women visiting obstetrics and gynaecology clinics,30,38,41,59,67 women attending college,33,47 school girls,69 mothers of school girls,10 and women from community settings.58,63 It was also found that Australian women recruited from healthcare settings had a better awareness (51% to 83%) compared to women from neighbouring countries.51,52 Noticeable differences on awareness were also identified between women residing in urban and rural areas, with women residing in townships or cities being more aware of HPV infection, HPV vaccine, and cervical cancer compared to women recruited from rural settings.35,39,56,57,65 Respondents who were in a relationship or married were more likely to have heard of the HPV vaccine that those not in a relationship.36,37
Source of information on HPV infection and HPV vaccine
Most respondents recruited from healthcare settings and universities largely heard of HPV infection and vaccine from mass media sources, which includes television4,26,27,33,36,45,55 magazine,4,27,36,51,33,36 and newspapers.26,27,36,51 In addition, university students disclosed their respective universities as a source of information about HPV and its vaccination.11,23,25 However, among school-going adolescent girls or college girls aware of HPV infection and vaccine, approximately half of them heard about it from doctors40,44 and teachers.40,44 Women recruited from community settings either heard about it from friends18,37,63 or media sources,35,37,51,58,63 while friends were cited as the main source of information for women residing in rural areas in one study.37 The channelling of information from media sources and school, was found to lead to an increased level of knowledge in one study.27
Knowledge
Knowledge level of practices and preventive actions of HPV infection and cervical cancer
Knowledge of practices and preventive measures of HPV infection and cervical cancer was examined in most included studies (48/63), however, assessment of knowledge and reporting measures on knowledge level markedly varied across these studies. Despite good awareness levels among women in six studies,27,42,49,54,62,67 knowledge levels among respondents were reported to be inadequate. By collectively examining the descriptive statistics on questionnaire items (which included percentages, median score, mean, and standard deviation) or qualitative synthesis, most studies reported knowledge deficits and misconceptions among women.10,13,15,19,22,24,27,28,33,36,38,40-42,47,49,53-57,62,63,65,66,70,72 Many studies reported that most women (40–94% of study respondents) did not know the link between HPV and cervical cancer,13,24-26,28,30,33,37,38,40-42,45,47,49,53-55,57,58,65,66,70 and the transmission route of HPV.13,24,36-38,40,41,47,53,57,70
Similar to awareness levels, knowledge levels among female sex workers5,53 were similar to women recruited from other settings.41,55,59,63,72 Women with lower educational backgrounds had less knowledge of HPV infection, HPV vaccine, and cervical cancer compared to women with higher educational levels (undergraduate degree or higher).10,15,36,37,43,55-57,63,65,67 Two studies demonstrated that women unaware of HPV infection or vaccine were less knowledgeable than women aware of HPV infection or vaccine.11,49 Overall, the unemployed/house wives, and skilled women/artisans seemed to have less knowledge than professionals or those in managerial positions.10,40 Having children,15,18 and a history of regular pap smear testing43,49,53,57 also influenced the level of knowledge in women. Two studies10,27 showed no association between the household income level of respondents or their parents with knowledge level, whereas with one study demonstrated improved knowledge with higher income status.57 The knowledge levels of women who were vaccinated relative to women who weren't vaccinated against HPV were mixed, with two studies reporting significant differences,19,66 while one study reported otherwise.24 Age of respondents was observed to be associated with knowledge levels, however, age groups differed markedly across studies, causing difficulty in comparing and contrasting between studies.11,27,37,38,43,53,55,57,67,73
Readiness for HPV vaccination
Recommendations/ opinions from others to receive HPV vaccination
Influence from others such as partners/husbands,57,64 family members and friends,18,40,44,48,64 and healthcare providers such as a physician4,37,64,73 were seen as facilitators to a woman's intention to receive the vaccine. Indeed women who received support and encouragement from family/friends,18,26,28,44,48,64 and recommendations from doctors17,26,32,34,48,64 were more likely to receive the vaccine. One study reported that recommendations from doctors or friends and family are a more common reason to initiate HPV vaccination in younger women compared to older women.46 However, most women stated that doctors rarely discussed HPV vaccination with them,4,26,34 and the same was applied to discussions with family and friends.26,48,51
Cost and reluctance to pay out-of-pocket for HPV vaccination
In terms of cost, very few women were reluctant to pay for the full course of the vaccine at market price,14,27-29,32,34,43,64,69,70 with participants with lower educational levels,41,43 lower monthly household incomes41,43,69 living in rural areas,41 and no history of Pap Smear testing43 being less agreeable to pay for it. Those who were unaware of the HPV vaccine were also less likely to pay for it compared to those who were aware of it.43 The cost of the vaccine was not a barrier to women who were offered fully-subsidized HPV immunisations, such as in Australia.48
Concerns about HPV vaccination
Concerns on the adverse effects of vaccination were highlighted in 14 of the included studies.10,17,25,27,31,32,36-38,41,42,48,60,68,69 This issue was raised among 12% to 69% of respondents who opposed HPV vaccination. It was the major concern in five studies25,32,36,48,60 second27,38,41 or third most common reason cited10,31,68,69 in seven studies, while respondents in three studies were least concerned about this issue.17,37,42 Women who had doubts on the efficacy of the vaccine made up 28% to 55% of study respondents.32,36,37,41,44,57 Both of these concerns were associated with education level in one study.31,44
Some studies have reported shyness among 21% to 30% of women to receive the cervical cancer vaccine.36,37,54 Perceived embarrassment of receiving the vaccine was significantly associated with knowledge of cervical cancer and risk factors in one study.36 Education level and monthly income was not associated with shame of receiving the vaccine in one study.20
Fear of getting vaccinated or dislike towards the injection4,28,38,54,64 was reported by 21% to 28% of women when they refused HPV vaccination. Five studies reported the issue of risky sexual behaviours or premarital sex, although it was present only in 5% to 33% of respondents.32,34,41,48,68
Perceives themselves or their daughters as low risk of acquiring HPV infection
In summary, women in SEAR and WPR appear unable to make informed decisions on HPV vaccination due to severe low risk of acquiring HPV infection and cervical cancer as identified in 12 of the included studies, regardless of the study country and type of respondents.10,22,28,29,35,40,41,48,49,54,58,60,68,69,73 Only 6% to 30% of women recruited from schools, community, and universities10,27,35,37,53,64,70 felt themselves at risk of getting HPV or cervical cancer, and were also of the opinion that their daughters were too young to receive vaccination. In addition, these studies did not explore the reasons why women thought they or their daughters had a low risk of HPV infection or cervical cancer. One study reported that older women were more likely to perceive themselves as being at risk of getting HPV compared to their younger peers.46
Discussion
This scoping review maps all evidence on influencing factors that may lead to HPV vaccine hesitancy among women in SEA and WP. In a region with a high mortality rate of cervical cancer,1,7 an insight into the common reasons why women refuse HPV vaccination will help inform the development of strategies to improve vaccine uptake in LMICs. As echoed by findings from international literature, the decision-making process of a woman is influenced by a myriad of factors and is discussed below.8,74-76
There were more publications studying factors that influence women in making an informed decision on HPV vaccination between year 2010 to 2011, and this may be due to low vaccine uptake which may have then triggered an assessment on what hinders women in taking the HPV vaccine since its licensure in 2006.17,19,22,23,33,37,39,43,67,71 Having said so, it could also be a foundation to develop HPV immunisation programs in their countries by understanding people's concerns and perceptions. Irrespective of a country's income status, cervical cancer mortality rates, and HPV immunisation programs; the influencing factors that arise when a woman decides to obtain the vaccine were similar in both SEAR and WPR, as well as other countries at an international level. Themes on knowledge, awareness, safety and efficacy of the vaccine, effect on sexual behaviour, and cost of vaccination, also appeared in four systematic reviews in which three of it was a review on high-income countries (HIC) (mostly studies in USA, with a smaller proportion in UK, Canada, Australia, and some European countries) and one on a low-income country (Africa).8,77-79
Our review reports that the cost of the HPV vaccine is a significant barrier among women in both SEAR and WPR, as demonstrated by the reluctance of most women to pay for it themselves. As expected, financial concerns were a more profound barrier in women from poor families or rural residence due to the lower socioeconomic status of these populations. This barrier did not appear in Australian studies, where a nationally-funded HPV immunisation program resulted in a coverage rate of 73.4% for females aged 15 years, with 82.7% having received at least one dose.80 Cost of the vaccine was also a reported barrier among women in HIC such as USA, where a review by Kessels SJM et al. found that girls without health insurance were less likely to get vaccinated.8 Systematic reviews of studies involving young women and US adolescents by Holman DM et al. and Ferrer HB et al., concluded that cost was a barrier in the uninsured,74 families with lower household incomes,78 ethnic minorities,78 and immigrant women.78 This further cements the fact that financial liabilities would be a barrier to women of lower socioeconomic status. Government subsidies, donation programs, and insurance coverage for HPV vaccination would be useful to curb the costs associated with the vaccination.
Another factor that influences a woman's decision to obtain or oppose HPV vaccination is the concern on the side-effects of the vaccine. This concern was prevalent in both this review and international literature. In SEAR and WPR, regardless of study setting and geography, women had concerns on the side effects of the vaccine, which stemmed from doubts about its safety and efficacy.10,17,25,27,31,32,36-38,41,42,48,60,68,69 No particular side-effect was reported by respondents in the included studies, except the study by Chan KKL et al. where women were concerned with the duration of side-effects and whether it would affect their appearance.31 In a study by Cunningham MS et al. in the African region, 37% of parents brought up concerns on adverse effects and safety.81 This concern was also cited in a study by Holman DM et al. in the US, but it was not mentioned how common or important this concern was among US parents. Similar to other available vaccines, the side-effects of the HPV vaccine related to injection site are pain, erythema, and swelling, whereas the common systemic adverse effects are headache, pyrexia, nausea, dizziness, and fatigue.82 It may be possible that parents and the women themselves have the perception that the occurrence of side-effects is frequent. However, studies have shown that allergic reactions are actually extremely rare, and only affect 3 out of a million people.83 In addition, a study by Joura EA et al. reported that less than 0.1% of its study participants (n = 14,149) dropped-out from their study because of injection site-related and systemic side effects.82 Fear of needles and syringes also seems to arise from the psychology of the person receiving it, further enhancing a reason for vaccine hesitancy.
In general, irrespective of the participant's sociodemographic and geographic background, most included studies reported that women's knowledge of HPV, and awareness of its symptoms and prevention were cursory in SEAR and WPR. In addition, women's awareness on HPV infection, HPV vaccination, and cervical cancer does not warrant a good knowledge on these aspects. From previous studies, it was observed that respondent do have an awareness of HPV infection, HPV vaccination, and cervical cancer,27,42,49,54,62,67 however, most are unaware of the cause of cervical cancer,13,24-26,28,30,33,37,38,40-42,45,47,49,53-55,57,58,65,66,70 the route of transmission of HPV infection13,24,36-38,40,41,47,53,57,70 and some did not know three doses of the vaccine were needed for full-effect.50 Most women, adults and parents alike who were recruited from community and university settings, received HPV-related information from media sources, largely from television, newspapers, and magazines. Adolescent girls on the other hand received HPV-related information from their respective schools or teachers. Hence, to improve the health literacy levels on HPV infection and vaccination, a school-based education program for HPV will help improve awareness and knowledge among young adolescent girls. In comparison, mediums such as television, magazines, and newspapers will be effective in promoting knowledge on HPV infection to the general public. Poor health literacy levels on HPV-related aspects did not appear in international literature, although knowledge level was linked with vaccine acceptance. A comprehensive report of US studies by Brewer NT et al. before HPV vaccination licensure, reported that studies showed mixed findings between HPV knowledge and vaccine acceptability.84 Similar findings were apparent in countries in Africa, where the association between knowledge level of Pap Smear test with vaccine acceptability was mixed.81
Physicians' recommendations were mostly requested by young women and parents themselves in both SEAR and WPR alike when deciding on HPV vaccination. Healthcare providers as a trusted source of information, were consistently cited when parents and young women where asked whom they trusted for more information on HPV vaccination. This need was similar to parents and women in other countries. A review by Kessels SJM et al. reported that a doctor's recommendation, or having discussed the vaccine with a healthcare provider, was a positive predictor for initiating the HPV-vaccine course.8,78 Recommendation from a healthcare provider was an important cue for acceptance for parents in Africa, although some stated they did not trust doctors.81 Higher uptake was also found if the source of information were family and friends in HIC, while acknowledgment that members of their communities and others held favourable attitudes towards the vaccine was found to be important in African societies.8,81 It is recommended that pamphlets on HPV vaccination be available in clinics and hospitals to help motivate the public to make enquiries on HPV vaccination. Physicians and other healthcare professionals should also be prepared to provide strong recommendations to their patients on the benefits of HPV vaccination, and assure the public that the side-effects are treatable. In addition, health promotion programs for HPV vaccination conducted in schools and universities/colleges can be delivered to improve the health literacy levels of the targeted population (i.e. young adolescent girls and young women) to enable them to make informed decisions.
A low perception of contracting HPV infection and cervical cancer was evident among young women and female parents in both SEAR and WPR, resulting in a lack of urgency to receive HPV vaccination. It is possible that these women do not understand the risks factors that can lead to HPV infection. Studies in Africa had mixed reports, where parents perceived the risk for HPV infection and cervical cancer as high (41% to 78%) whereas those in universities felt the risk was low (6% to 7%).81
In summary, women in SEAR and WPR are unable to make informed decisions due to severe knowledge deficits on HPV-related aspects. This is evident from their request for more information, poor knowledge and awareness, low perceived risk of acquiring cervical cancer, and a preoccupation with the occurrence of side-effects with HPV vaccination. Lack of communication between healthcare providers and young women or parents on HPV vaccination could also explain the low uptake of the vaccine in the targeted population. Cost of the HPV vaccine is also a significant barrier among women in settings where they have to pay for the vaccine themselves.
Strength and limitations of this review
A systematic search of multiple databases resulted in the identification of all relevant literature on the decision-making process with regard to HPV vaccination. Studies were not excluded on the basis of research methods used or publication dates, but were selectively confined to women in WHO SEAR and WPR, providing a good reflection on vaccine refusal in LMICs. However, there were some limitations. There was a paucity of studies on this topic in some countries in SEAR and WPR, hence, the state of HPV vaccine uptake and the influencing factors in the decision making processes has yet to be established in some of these countries.
The findings from this review cannot be generalised to all low-income countries as there may be pilot schemes or GAVI projects which make vaccine refusal not applicable in these settings. Lack of sufficient English data in the abstract, and the exclusion of non-English research papers from this review could have introduced bias. Furthermore, not many of the included studies were conducted in rural settings or recruited ethnic minorities, causing some concerns such as issues of access to a healthcare facility, omitted from this review. Further research is needed to understand barriers in obtaining HPV vaccination in women residing in rural areas or ethnic minorities. Finally, there was a pronounced lack of standardisation in the measurement tools used, causing difficulty in comparison and contrasting of evidence.
Conclusion
Our findings show that the decision- making process of women in obtaining the HPV vaccine is governed by the perception of the women themselves, and the views of a third party, such as family, friends, and healthcare professionals. Future development of health promotion programs for HPV vaccination should highlight the benefits of the HPV vaccine, and how it outweighs the risks involved in vaccination. More cost-effective and culturally-appropriate strategies are also needed to improve access to the HPV vaccine.
Supplementary Material
Funding Statement
We would like to thank Global Asia 21 platform for providing financial support to hire research assistant for this project
Disclosure of potential conflicts of interest
All authors have no potential conflicts of interest to disclosed.
References
- [1].International Agency for Research on Cancer. GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Fact Sheets: Cervix Uteri. World Health Organization; 2012 [assessed 2017 Mar 5]. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx [Google Scholar]
- [2].Hopkins TG, Wood N. Female human papillomavirus (HPV) vaccination: Global uptake and the impact of attitudes. Vaccine. 2013;31:1673-9. doi: 10.1016/j.vaccine.2013.01.028. PMID:23375978 [DOI] [PubMed] [Google Scholar]
- [3].World Health Organization. Media Centre. Sexually Transmitted Infections (STIs): Fact Sheets; 2016 [assessed 2017 Feb 21]. http://www.who.int/mediacentre/factsheets/fs110/en/ [Google Scholar]
- [4].Weisberg E, Bateson D, McCaffery K, Skinner SR. HPV vaccination catch up program – utilisation by young Australian women. Australian Family Physician. 2009;38:72. PMID:19283241 [PubMed] [Google Scholar]
- [5].Wadhera P, Evans JL, Stein E, Gandhi M, Couture M-C, Sansothy N, Sichan K, Maher L, Kaldor J, Page K. et al.. Human papillomavirus knowledge, vaccine acceptance, and vaccine series completion among female entertainment and sex workers in Phnom Penh, Cambodia: the Young Women's Health Study. Int J STD AIDS. 2015;26:893-902. doi: 10.1177/0956462414563626. PMID:25505042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. https://www.cancer.gov/types/cervical/research/gardasil9-prevents-more-HPV-types National Cancer Centre. Cancer Types: Cervical Cancer. Gardasil 9 Protects against Additional HPV Types. US Department of Health and Human Services [assessed 2017 May 11]. [Google Scholar]
- [7].Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, de Sanjosé S, Castellsagué X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Global Health. 2016;4:e453-e63. doi: 10.1016/S2214-109X(16)30099-7. PMID:27340003 [DOI] [PubMed] [Google Scholar]
- [8].Kessels SJM, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: A systematic review. Vaccine. 2012;30:3546-56. doi: 10.1016/j.vaccine.2012.03.063. PMID:22480928 [DOI] [PubMed] [Google Scholar]
- [9].World Health Organization. Immunization, Vaccines and Biologicals: Human Papillomavirus (HPV); 2017 [assessed 2017 March 9]. http://www.who.int/immunization/diseases/hpv/en/ [Google Scholar]
- [10].Yu Y, Xu M, Sun J, Li R, Li M, Wang J, Zhang D, Xu A. Human Papillomavirus Infection and Vaccination: Awareness and Knowledge of HPV and Acceptability of HPV Vaccine among Mothers of Teenage Daughters in Weihai, Shandong, China. PloS One. 2016;11:e0146741. doi: 10.1371/journal.pone.0146741. PMID:26766565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Juntasopeepun P, Davidson PM, Suwan N, Phianmongkhol Y, Srisomboon J. Human papillomavirus vaccination intention among young women in Thailand. Asian Pacific J Cancer Prevention. 2011;12:3213-9 [PubMed] [Google Scholar]
- [12].Hsu Y-Y, Fetzer SJ, Hsu K-F, Chang Y-Y, Huang C-P, Chou C-Y. Intention to obtain human papillomavirus vaccination among Taiwanese undergraduate women.(Author abstract). Sexually Transmitted Dis. 2009;36:686. doi: 10.1097/OLQ.0b013e3181ad28d3 [DOI] [PubMed] [Google Scholar]
- [13].Rashid S, Labani S, Das BC. Knowledge, Awareness and Attitude on HPV, HPV Vaccine and Cervical Cancer among the College Students in India. PloS One. 2016;11:e0166713. doi: 10.1371/journal.pone.0166713. PMID:27861611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Choi C, Woo P, Jit M, Leung G, Wu J. Acceptability and uptake of female adolescent HPV vaccination in Hong Kong: A Survey Of Mothers And Adolescents. Vaccine. 2013;32:78-84. doi: 10.1016/j.vaccine.2013.10.068. PMID:24188759 [DOI] [PubMed] [Google Scholar]
- [15].Ezat SW, Hod R, Mustafa J, Mohd Dali AZ, Sulaiman AS, Azman A. National HPV immunisation programme: knowledge and acceptance of mothers attending an obstetrics clinic at a teaching hospital, Kuala Lumpur. Asian Pacific J Cancer Prevention. 2013;14:2991-9. doi: 10.7314/APJCP.2013.14.5.2991 [DOI] [PubMed] [Google Scholar]
- [16].Ginsburg O. Global disparities in HPV vaccination. Lancet Global Health. 2016;4:e428-e9. doi: 10.1016/S2214-109X(16)30107-3 [DOI] [PubMed] [Google Scholar]
- [17].Kang HS, Moneyham L. Attitudes toward and intention to receive the human papilloma virus (HPV) vaccination and intention to use condoms among female Korean college students. Vaccine. 2010;28:811. doi: 10.1016/j.vaccine.2009.10.052. PMID:19879993 [DOI] [PubMed] [Google Scholar]
- [18].Zhuang QY, Wong RX, Chen WM, Guo XX. Knowledge, attitudes and practices regarding human papillomavirus vaccination among young women attending a tertiary institution in Singapore. Singapore Med J. 2016;57:329-33. doi: 10.11622/smedj.2016108. PMID:27353611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bang K-S, Sung S, Koo B, Kim M, Kim Y, Kim J, et al.. Female University Students' HPV-related Knowledge and Influencing Factors on HPV Vaccination. J Korean Oncol Nurs. 2011;11:186-92. doi: 10.5388/jkon.2011.11.3.186 [DOI] [Google Scholar]
- [20].Kim HW. Factors Associated with Human Papillomavirus related Stigma, Shame, and Intent of HPV Test. J Korean Acad Nurs. 2012;42:217-25. doi: 10.4040/jkan.2012.42.2.217. PMID:22699171 [DOI] [PubMed] [Google Scholar]
- [21].Lee KE. Factors Associated with Intention to receive Human Papillomavirus Vaccine in Undergraduate Women: An Application of the Theory of Planned Behavior. J Korean Acad Fundam Nurs. 2014;21:457-65. doi: 10.7739/jkafn.2014.21.4.457 [DOI] [Google Scholar]
- [22].Lee E-J, Park J-S. Knowledge about Cervical Cancer, Health Beliefs and Human Papillomavirus Vaccination Rate in Female University Students. J Korean Oncol Nurs. 2011;11:65-73. doi: 10.5388/jkon.2011.11.1.65 [DOI] [Google Scholar]
- [23].Park J-S, Lee E-J. Predictors of Human Papillomavirus Vaccination in Female University Students. Korean J Women Health Nursing. 2011;17:346-58. doi: 10.4069/kjwhn.2011.17.4.346 [DOI] [PubMed] [Google Scholar]
- [24].Kwan T, Chan K, Yip A, Tam K, Cheung A, Lo S, Lee PW, Ngan HY. Acceptability of human papillomavirus vaccination among Chinese women: concerns and implications. BJOG. 2009;116:501-10. doi: 10.1111/j.1471-0528.2008.01988.x. PMID:19250361 [DOI] [PubMed] [Google Scholar]
- [25].Wong W, Fong B, Chan P. Acceptance of human papillomavirus vaccination among first year female university students in Hong Kong. Sex Health. 2009;6:264-71. doi: 10.1071/SH09017. PMID:19917193 [DOI] [PubMed] [Google Scholar]
- [26].Wang LD-L, Lam WWT, Fielding R. Cervical cancer prevention practices through screening and vaccination: A cross-sectional study among Hong Kong Chinese women. Gynecologic Oncol. 2015;138:311. doi: 10.1016/j.ygyno.2015.05.018 [DOI] [PubMed] [Google Scholar]
- [27].Lee A, Ho M, Cheung CK, Keung VM. Factors influencing adolescent girls' decision in initiation for human papillomavirus vaccination: a cross-sectional study in Hong Kong. BMC Public Health. 2014;14:925. doi: 10.1186/1471-2458-14-925. PMID:25195604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Chan K, Cheung A, Ngan H, Kwan T, Yip A, Tam K, Kwan TT, Young PM. Barriers and facilitators to human papillomavirus vaccination among Chinese adolescent girls in Hong Kong: A qualitative-quantitative study. Sex Transm Infect. 2008;84:227-32. doi: 10.1136/sti.2007.029363. PMID:18256106 [DOI] [PubMed] [Google Scholar]
- [29].Siu JY-M. Barriers to receiving human papillomavirus vaccination among female students in a university in Hong Kong. Culture, Health Sexuality. 2013;15:1071-84. doi: 10.1080/13691058.2013.807518. PMID:23826650 [DOI] [PubMed] [Google Scholar]
- [30].Lee P, Kwan T, Tam K, Chan K, Young P, Lo SS, Cheung AN, Ngan HY. Beliefs about cervical cancer and human papillomavirus (HPV) and acceptability of HPV vaccination among Chinese women in Hong Kong. Prev Med. 2007;45:130-4. doi: 10.1016/j.ypmed.2007.07.013. PMID:17707077 [DOI] [PubMed] [Google Scholar]
- [31].Yao T, Cheung A, Ngan H, Kwan T, Tam K, Chan K. Human papillomavirus vaccine: What are women most concerned about? J Obstet Gynaecol Res. 2012;38:23-30. [DOI] [PubMed] [Google Scholar]
- [32].Kang HS, Shin H, Hyun MS, Kim MJ. Human papilloma virus vaccination: perceptions of young Korean women. J Adv Nursing. 2010;66:1946-52 [DOI] [PubMed] [Google Scholar]
- [33].Kang H-Y, Kim J-S. Knowledge, Attitudes of Human Papillomavirus Vaccine, and intention to obtain vaccine among Korean female undergraduate students. Women Health. 2011;51:759-76. doi: 10.1080/03630242.2011.627091. PMID:22185290 [DOI] [PubMed] [Google Scholar]
- [34].Kang H, Moneyham L. Attitudes, Intentions, and Perceived Barriers to Human Papillomavirus Vaccination Among Korean high school girls and their mothers. Cancer Nursing. 2011;34:202. doi: 10.1097/NCC.0b013e3181fa482b. PMID:21116177 [DOI] [PubMed] [Google Scholar]
- [35].Chow S, Soon R, Park J, Pancharoen C, Qiao Y, Basu P, Ngan HY. Knowledge, attitudes, and communication around human papillomavirus (HPV) vaccination amongst urban Asian Mothers And Physicians. Vaccine. 2010;28:3809-17 [DOI] [PubMed] [Google Scholar]
- [36].Wong LP, Sam IC. Ethnically diverse female university students' knowledge and attitudes toward human papillomavirus (HPV), HPV vaccination and cervical cancer.(Report). Eur J Obstetrics Gynecol. 2010;148:90. doi: 10.1016/j.ejogrb.2009.10.002 [DOI] [PubMed] [Google Scholar]
- [37].Wong L. Knowledge and Attitudes About HPV Infection, HPV Vaccination, and Cervical Cancer Among Rural Southeast Asian Women. Official J Int Soc Behavioral Med. 2011;18:105-11. doi: 10.1007/s12529-010-9104-y [DOI] [PubMed] [Google Scholar]
- [38].Al-Dubai SA, Alshagga MA, Al-Naggar RA, Al-Jashamy K, Baobaid MF, Tuang CP, et al.. Knowledge, attitudes and barriers for human papilloma virus (HPV) vaccines among Malaysian women. Asian Pacific J Cancer Prevention. 2010;11:887-92 [PubMed] [Google Scholar]
- [39].Al-Naggar RA, Bobryshev YV. Practice towards human papillomavirus vaccines among Malaysian women: a survey of a general youth population. Asian Pacific J Cancer Prevention. 2011;12:2045-9 [PubMed] [Google Scholar]
- [40].Wong L, Yusoff A, Edib Z, Sam IC, Zimet G. Nationwide Survey of Knowledge and Health Beliefs regarding Human Papillomavirus among HPV-Vaccinated Female Students in Malaysia. PLoS One. 2016;11:e0163156. doi: 10.1371/journal.pone.0163156. PMID:27656876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Sam IC, Wong LP, Rampal S, Leong YH, Pang CF, Tai YT, Tee HC, Kahar-Bador M. Maternal acceptance of human papillomavirus vaccine in Malaysia. J Adolescent Health. 2009;44:610. doi: 10.1016/j.jadohealth.2008.11.014 [DOI] [PubMed] [Google Scholar]
- [42].Al-Naggar RA, Al-Jashamy K, Chen R. Perceptions and opinions regarding human papilloma virus vaccination among young women in Malaysia. Asian Pacific J Cancer Prevention. 2010;11:1515-21 [PubMed] [Google Scholar]
- [43].Yen C-F, Chen S-F, Lin L-P, Hsu S-W, Chang M-J, Wu C-L, Lin JD. The acceptability of human papillomavirus (HPV) vaccination among women with physical disabilities. Res Dev Disabilities. 2011;32:2020-6. doi: 10.1016/j.ridd.2011.04.006 [DOI] [PubMed] [Google Scholar]
- [44].Kuo PF, Yeh YT, Sheu SJ, Wang TF. Factors associated with future commitment and past history of human papilloma virus vaccination among female college students in northern Taiwan. J Gynecol Oncol. 2014;25:188-97. doi: 10.3802/jgo.2014.25.3.188. PMID:25045431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Lan YL CC, Tsai CH. Female college students' perspectives on self-paid human papillomavirus vaccination based on the theory of planned behaviour. J Chem Pharmaceutical Res. 2013;5:6-11 [Google Scholar]
- [46].Hsu YY, Hsu KF, Cheng YM, Fetzer SJ, Chou CY. Health beliefs of Taiwanese women seeking HPV vaccination. Vaccine. 2010;28:4224. doi: 10.1016/j.vaccine.2010.01.063. PMID:20171307 [DOI] [PubMed] [Google Scholar]
- [47].Tu Y-C, Wang H-H, Lin Y-J, Chan T-F. HPV Knowledge and factors associated with intention to use condoms for reducing HPV Infection Risk among Adolescent Women in Taiwan. Women Health. 2015;55(2):187-202. doi: 10.1080/03630242.2014.979970. PMID:25774655 [DOI] [PubMed] [Google Scholar]
- [48].Tung ILY, Machalek DA, Garland SM. Attitudes, Knowledge and Factors Associated with Human Papillomavirus (HPV) Vaccine Uptake in Adolescent Girls and Young Women in Victoria, Australia.(Research Article)(Report). PLoS One. 2016;11:e0161846. doi: 10.1371/journal.pone.0161846. PMID:27564213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].McNair R, Power J, Carr S. Comparing knowledge and perceived risk related to the human papilloma virus among Australian women of diverse sexual orientations. Australian N Zealand J Public Health. 2009;33:87-93. doi: 10.1111/j.1753-6405.2009.00345.x [DOI] [PubMed] [Google Scholar]
- [50].Brotherton JML, Piers LS, Vaughan L. Estimating human papillomavirus vaccination coverage among young women in Victoria and reasons for non-vaccination. Sexual Health. 2015;13:190-2. doi: 10.1071/SH15131 [DOI] [PubMed] [Google Scholar]
- [51].Pitts MK, Dyson SJ, Rosenthal DA, Garland SM. Knowledge and awareness of human papillomavirus (HPV): attitudes towards HPV vaccination among a representative sample of women in Victoria, Australia. Sexual Health. 2007;4:177-80. doi: 10.1071/SH07023. PMID:17931530 [DOI] [PubMed] [Google Scholar]
- [52].Giles M, Garland S. A study of women's knowledge regarding human papillomavirus infection, cervical cancer and human papillomavirus vaccines. Australian N Zealand J Obstetrics Gynaecol. 2006;46:311-5. doi: 10.1111/j.1479-828X.2006.00598.x [DOI] [PubMed] [Google Scholar]
- [53].Hong Y, Zhang C, Li X, Lin D, Liu Y. HPV and cervical cancer related knowledge, awareness and testing behaviors in a community sample of female sex workers in China. BMC Public Health. 2013;13:696. doi: 10.1186/1471-2458-13-696. PMID:23898889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Gu C, Niccolai LM, Yang S, Wang X, Tao L. Human papillomavirus vaccine acceptability among female undergraduate students in China: the role of knowledge and psychosocial factors. J Clin Nursing. 2015;24:2765-78. doi: 10.1111/jocn.12871 [DOI] [PubMed] [Google Scholar]
- [55].Abudukadeer A, Azam S, Mutailipu AZ, Qun L, Guilin G, Mijiti S. Knowledge and attitude of Uyghur women in Xinjiang province of China related to the prevention and early detection of cervical cancer. World J Surg Oncol. 2015;13:110. doi: 10.1186/s12957-015-0531-8. PMID:25885660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Li J, LLK Ma JF, Wei LH, Niyazi M, Li CQ, Xu AD, Wang J-B, Liang H, Belinson J, Qiao Y-L. Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China.(Report). Vaccine. 2009;27:1210. doi: 10.1016/j.vaccine.2008.12.020. PMID:19135493 [DOI] [PubMed] [Google Scholar]
- [57].Feng S, Xu X, Jin Y, Yao X. Women's Knowledge of Human Papillomavirus (HPV) and Their Attitudes Toward HPV Vaccine. Asia-Pacific J Public Health. 2012;24:522-31. doi: 10.1177/1010539511415838 [DOI] [PubMed] [Google Scholar]
- [58].Montgomery M, Dune T, Shetty P, Shetty A. Knowledge and acceptability of human papillomavirus vaccination and cervical cancer screening among women in Karnataka, India. J Cancer Education. 2015;30:130-7. doi: 10.1007/s13187-014-0745-4 [DOI] [PubMed] [Google Scholar]
- [59].Siddharthar J, Rajkumar B, Deivasigamani K. Knowledge, Awareness and Prevention of Cervical Cancer among Women Attending a Tertiary Care Hospital in Puducherry, India. J Clin Diagnostic Res. 2014;8:Oc01-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Egawa-Takata T, Ueda Y, Morimoto A, Tanaka Y, Matsuzaki S, Kobayashi E, Yoshino K, Sekine M, Enomoto T, Kimura T. Human papillomavirus vaccination of the daughters of obstetricians and gynecologists in Japan. Int J Clin Oncol. 2016;21:53. doi: 10.1007/s10147-015-0869-5. PMID:26155971 [DOI] [PubMed] [Google Scholar]
- [61].Egawa-Takata T, Ueda Y, Morimoto A, Yoshino K, Kimura T, Nishikawa N, Sekine M, Horikoshi Y, Takagi T, Enomoto T. Survey of Japanese mothers of daughters eligible for human papillomavirus vaccination on attitudes about media reports of adverse events and the suspension of governmental recommendation for vaccination. J Obstetrics Gynaecol Res. 2015;41:1965-71. doi: 10.1111/jog.12822 [DOI] [PubMed] [Google Scholar]
- [62].Miyagi E, Motoki Y, Asai-Sato M, Taguri M, Morita S, Hirahara F, et al.. Web-based recruiting for a survey on knowledge and awareness of cervical cancer prevention among young women living in Kanagawa prefecture, Japan. Int J Gynecol Cancer. 2014;24:1347-55. doi: 10.1097/IGC.0000000000000220. PMID:25054449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Pitts M, Smith A, Croy S, Lyons A, Ryall R, Garland S, et al.. Singaporean Women's Knowledge of Human Papillomavirus (HPV) and Attitudes Toward HPV Vaccination. Women Health. 2009;49:334-51. doi: 10.1080/03630240903158420. PMID:19753508 [DOI] [PubMed] [Google Scholar]
- [64].Young AM, Crosby RA, Jagger KS, Richardson MB, Kloha RA, Safarian V. HPV vaccine acceptability among women in the Philippines. Asian Pacific J Cancer Prevention. 2010;11:1781-7 [PubMed] [Google Scholar]
- [65].Johnson DC, Bhatta MP, Gurung S, Aryal S, Lhaki P, Shrestha S. Knowledge and awareness of human papillomavirus (HPV), cervical cancer and HPV vaccine among women in two distinct Nepali communities. Asian Pacific J Cancer Prevention. 2014;15:8287-93. doi: 10.7314/APJCP.2014.15.19.8287 [DOI] [PubMed] [Google Scholar]
- [66].Paul P, LaMontagne DS, Le NT. Knowledge of cervical cancer and HPV vaccine post- vaccination among mothers and daughters in Vietnam. Asian Pacific J Cancer Prevention. 2012;13:2587-92. doi: 10.7314/APJCP.2012.13.6.2587 [DOI] [PubMed] [Google Scholar]
- [67].Charakorn C RS, Lertkhachonsuk A, Thanapprapasr D, Chittithaworn S, Wilailak S. Knowledge of Pap smear, HPV and the HPV vaccine and the acceptability of the HPV vaccine by Thai women.(Report). Asia-Pacific J Clin Oncol. 2011;7:160. doi: 10.1111/j.1743-7563.2011.01392.x [DOI] [PubMed] [Google Scholar]
- [68].Siu JY-M. Perceptions of and barriers to vaccinating daughters against human papillomavirus (HPV) among mothers in Hong Kong. BMC Women's Health. 2014;14:73. doi: 10.1186/1472-6874-14-73. PMID:24890226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Li S, Fan S, Lau Y, Lam T, Yip P, Ip P. HPV vaccination in Hong Kong: uptake and reasons for non-vaccination amongst Chinese Adolescent Girls. Vaccine. 2013;31:5785-8 [DOI] [PubMed] [Google Scholar]
- [70].Kruiroongroj S, Chaikledkaew U, Thavorncharoensap M. Knowledge, acceptance, and willingness to pay for human papilloma virus (HPV) vaccination among female parents in Thailand. Asian Pacific J Cancer Prevention. 2014;15:5469-74. doi: 10.7314/APJCP.2014.15.13.5469 [DOI] [PubMed] [Google Scholar]
- [71].Juntasopeepun P, Davidson PM, Chang S, Suwan N, Phianmongkhol Y, Srisomboon J. Development and psychometric evaluation of the Thai Human Papillomavirus Beliefs Scale. Nursing Health Sci. 2011;13:475-80. doi: 10.1111/j.1442-2018.2011.00642.x [DOI] [PubMed] [Google Scholar]
- [72].Wong LP. Knowledge of and attitudes toward the HPV vaccine among multi‐ethnic women from urban/university and rural areas. Int J Gynecol Obstetrics. 2011;112:146-7. doi: 10.1016/j.ijgo.2010.09.006 [DOI] [PubMed] [Google Scholar]
- [73].Juntasopeepun P, Suwan N, Phianmongkhol Y, Srisomboon J. Factors influencing acceptance of human papillomavirus vaccine among young female college students in Thailand. Int J Gynecol Obstetrics. 2012;118:247-50. doi: 10.1016/j.ijgo.2012.04.015 [DOI] [PubMed] [Google Scholar]
- [74].Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700. doi: 10.1186/1471-2458-14-700. PMID:25004868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Ganmble HL KJ, Parra GR, Randolph ME. Factors influencing familial decision-making regarding human papillomavirus vaccination. J Pediatric Psychol. 2010;35:704-15. doi: 10.1093/jpepsy/jsp108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Hendry M, Lewis R, Clements A, Damery S, Wilkinson C “HPV? Never heard of it!”: a systematic review of girls' and parents' information needs, views and preferences about human papillomavirus vaccination. Vaccine. 2013;31:5152-67. doi: 10.1016/j.vaccine.2013.08.091. PMID:24029117 [DOI] [PubMed] [Google Scholar]
- [77].Cunningham MS, Davison C, Aronson KJ. HPV vaccine acceptability in Africa: A systematic review. Preventive Med. 2014;69:274-9. doi: 10.1016/j.ypmed.2014.08.035 [DOI] [PubMed] [Google Scholar]
- [78].Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among us adolescents: A systematic review of the literature. JAMA Pediatrics. 2014;168:76-82. doi: 10.1001/jamapediatrics.2013.2752. PMID:24276343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Trim K, Nagji N, Elit L, Roy K. Parental Knowledge, Attitudes, and Behaviours towards Human Papillomavirus Vaccination for Their Children: A Systematic Review from 2001 to 2011. Obstetrics Gynecol Int. 2012;2012:12. doi: 10.1155/2012/921236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Hull BP, Hendry AJ, Dey A, Beard FH, Brotherton JM, McIntyre PB. Immunisation Coverage Annual Reports, 2014. Annual Reports. Communicable Disease Intelligence (CDI). 2017;41(1):E68-E90. doi: 10.33321/cdi.2017.41.10. http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-cdi-immunanrep.htm [DOI] [PubMed] [Google Scholar]
- [81].Cunningham MS, Davison C, Aronson KJ. HPV vaccine acceptability in Africa: a systematic review. Prev Med 2014; 69:274-9. doi: 10.1016/j.ypmed.2014.08.035. PMID:25451327 [DOI] [PubMed] [Google Scholar]
- [82].Joura EA, Giuliano AR, Iversen O-E, Bouchard C, Mao C, Mehlsen J, Jr Moreira ED, Ngan Y, Petersen LK, Lazcano-Ponce E, et al.. A 9-Valent HPV Vaccine against Infection and Intraepithelial Neoplasia in Women. N Eng J Med. 2015;372:711-23. doi: 10.1056/NEJMoa1405044 [DOI] [PubMed] [Google Scholar]
- [83].Cancer Council NSW. HPV Vaccine Fact Sheet. Woolloomooloo NSW, Cancer Council NSW; 2015 [assessed 2017 May 5]. https://www.cancercouncil.com.au/1060/cancer-information/cancer-risk-and-prevention/screening-and-early-detection/cervical-cancer-vaccine-fact-sheet/ [Google Scholar]
- [84].Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Med. 2007;45:107-14. doi: 10.1016/j.ypmed.2007.05.013. PMID:17628649 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


