ABSTRACT
Objective: To examine amongst healthcare professionals in England; knowledge of vaccinations in pregnancy, their perceived roles in these programmes and whether they recommend scheduled vaccines to pregnant women.
Design: Cross sectional survey (online questionnaire)
Setting: Healthcare workers in contact with pregnant women in England.
Participants: The survey analysis included 3441 healthcare workers who had been surveyed during May to August 2015. The participants were midwives, practice nurses and health visitors, working in England who were members of the Royal College of Midwives, Royal College of Nursing and the Institute of Health Visiting.
Results: We found that knowledge of vaccination in pregnancy was high in all professional groups. Seventy three percent of all respondents would recommend the influenza vaccine and 74% would recommend the pertussis vaccine to pregnant women. They were more likely to recommend vaccination in pregnancy if they would personally have the influenza and pertussis vaccines themselves and/or if they had the influenza vaccine as a healthcare worker. Practice nurses were significantly more likely to recommend the pertussis and influenza vaccines to pregnant women than midwives and health visitors. Health professionals who had received immunisation training were more confident in giving advice to pregnant women.
Conclusion: Immunisation training is essential if healthcare workers are to be informed and confident in effectively delivering the maternal immunisation programme and thus improving uptake of vaccines in pregnancy. These findings are important in tailoring educational programmes and addressing the training needs of different healthcare professional groups.
KEYWORDS: attitudes, health visitors, midwives, nurses, pregnant, vaccination
Introduction
Vaccination during pregnancy, using inactivated influenza, pertussis and tetanus containing vaccines, is a safe and effective way to protect pregnant women and their infants when either one or both are at risk of these vaccine preventable diseases. In the UK, there are currently maternal vaccination programmes protecting both pregnant women and their young babies against seasonal influenza and protecting babies from birth against pertussis.1-3
Since 2010, UK guidelines recommend that women who are pregnant during the influenza (flu) season, regardless of gestation, should be offered inactivated influenza vaccine.4 Pregnant women, particularly in the last trimester, and young infants, are at increased risk of severe disease and death from influenza.5 Pregnant women can be safely vaccinated against flu6-8 and vaccination is effective in preventing disease in pregnant women and their infants.1,9 Despite recommendations and strong support from professional bodies, flu vaccination coverage during pregnancy in England was 42.3% in the 2015/16 winter season compared to 71% in those aged 65 years and over, in whom vaccination is also recommended.10
In 2012, the UK reported the highest pertussis activity in over two decades, with rates of morbidity and mortality greatest in infants under three months of age. Pertussis-containing vaccines are scheduled at 8, 12 and 16 weeks in infancy. Most cases and all deaths in 2012 occurred in infants before they commenced their primary course of pertussis-containing vaccines.11 As an outbreak control strategy, Public Health England (PHE) introduced a temporary vaccination programme in 2012 offering all pregnant women pertussis-containing vaccine between 28 and 38 weeks of pregnancy to passively protect their infants from birth.12
In 2016, following research into the optimal timing of pertussis vaccination in pregnancy,13 the UK's Joint Committee on Vaccination and Immunisation (JCVI) recommended vaccinating from 16 weeks gestation.14 The vaccine is ideally offered around the fetal anomaly scan at about 20 weeks and up to 32 weeks (though it can be given later) to capture early deliveries.15 Vaccinating in pregnancy is highly effective in protecting infants against pertussis.2,3,11,16 Data on the uptake, effectiveness3 and safety7 of the programme and its impact on disease led to the extension of the UK programme until at least 2019.17
It is important that all pregnant women are fully informed and have the opportunity to be immunised with easy access to immunisation services.18 There is evidence that most women recognise the benefits of vaccination during pregnancy and would be likely to accept vaccination to protect their baby or themselves in pregnancy against a potentially life-threatening disease.19
Health professionals play a key role in informing women and recommending vaccination.19-26 The strong links between healthcare workers' (HCWs) perceptions of vaccination and vaccine uptake has been documented in studies in several countries.18,27-34
Public Health England (PHE) in collaboration with the associated Royal College of Midwives (RCM), Royal College of Nursing (RCN), and the Institute of Health Visiting (iHV) conducted a survey to assess the knowledge, attitudes and practice of HCWs involved in antenatal care and/or vaccination, towards immunisation in pregnancy. We targeted midwives, practice nurses and health visitors (Box One).
Box One: Healthcare workers in contact with pregnant women
Practice nurse –is a registered nurse who is employed by a general practice, or whose services are otherwise retained by a general practice. Practice nurses play a key role in the administration of many routine vaccinations.
Health visitor – is a nurse or midwife who has an additional qualification in Specialist Community Public Health Nursing – Health Visiting (SCPHN-HV). This includes extra training in all aspects of family and public health. They work at a child, family and community level. They provide support and advice for parents from the ante natal period until the child is 5 years old. A health visitor may meet a pregnant woman for the first time during the latter stages of the pregnancy and usually in the first few weeks after.
Midwife – is usually the first (alternatively women may first go to their GP and then be referred to antenatal care) and main contact for the woman during her pregnancy, throughout labour and the early postnatal period. They are responsible for providing care and supporting women to make informed choices about their care.
Our key questions to better understand and support HCWs in delivering the programme were;
-
1)
Do HCWs recommend vaccines to pregnant women?
-
2)
Do HCWs have sufficient knowledge to advise pregnant women?
-
3)
Are HCWs confident in communicating information on vaccines?
Results
Demographic characteristics
The overall response rate was 10% (3493/34,037): midwives (2393/21714, 11%); practice nurses (751/5323, 14%); and health visitors (297/7000, 4%). We excluded 52 responses as we could not assign them a professional category and therefore 3441 responses were included in the analysis. 3415 (99%) were female, 2849 were white (93%) and 1327 were aged 45–54 (43%). The largest professional group was midwives (2393, 70%) followed by practice nurses (751, 22%) and health visitors (297, 9%).The demographic characteristics are summarised in Table 1. We were able to compare the demographic data with registered members from the RCM and RCN. RCM registered members were; 99.6% females, 88% of white ethnicity and 34% aged 45–54. The RCN had 97% females, 83% of white ethnicity and 35% aged 45–54.
Table 1.
Characteristics of respondants to the survey.
| Respondents | Health Visitor | % | Midwife | % | Practice nurse | % | TOTAL | |
|---|---|---|---|---|---|---|---|---|
| Sex | Female | 295 | 99 | 2376 | 99 | 744 | 99 | 3415 |
| Male | 2 | 1 | 17 | 1 | 7 | 1 | 26 | |
| Total | 297 | 2393 | 751 | 3441 | ||||
| Age | 18–24 | 2 | 1 | 75 | 3 | 3 | 0 | 80 |
| 25–34 | 21 | 9 | 394 | 18 | 21 | 3 | 436 | |
| 35–44 | 59 | 25 | 433 | 20 | 83 | 12 | 575 | |
| 45–54 | 103 | 43 | 803 | 37 | 421 | 62 | 1327 | |
| 55–64 | 52 | 22 | 434 | 20 | 141 | 21 | 627 | |
| Aged 65 & over | 2 | 1 | 21 | 1 | 11 | 2 | 34 | |
| Total | 239 | 2160 | 680 | 3079 | ||||
| Area of Practice | East Midlands | 13 | 5 | 169 | 8 | 76 | 11 | 258 |
| London | 38 | 16 | 334 | 15 | 68 | 10 | 440 | |
| North East | 18 | 8 | 93 | 4 | 21 | 3 | 132 | |
| North West | 23 | 10 | 281 | 13 | 62 | 9 | 366 | |
| South East | 52 | 22 | 375 | 17 | 147 | 22 | 574 | |
| South West | 30 | 13 | 277 | 13 | 102 | 15 | 409 | |
| West midlands | 20 | 8 | 225 | 10 | 67 | 10 | 312 | |
| Yorkshire &Humber | 24 | 10 | 194 | 9 | 81 | 12 | 299 | |
| Total | 239 | 2160 | 680 | 3079 | ||||
| Years in role | 0–3 years | 99 | 41 | 510 | 24 | 90 | 13 | 699 |
| 4–9 years | 61 | 26 | 528 | 25 | 272 | 40 | 861 | |
| 20 years & above | 29 | 12 | 521 | 24 | 131 | 19 | 681 | |
| Total | 239 | 2155 | 679 | 3073 | ||||
| Ethincity | White | 209 | 87 | 1990 | 93 | 650 | 97 | 2849 |
| Bangladesh | 0 | 0 | 2 | 0 | 0 | 0 | 2 | |
| Black African | 14 | 6 | 44 | 2 | 3 | 0 | 61 | |
| Chinese | 2 | 1 | 9 | 0 | 3 | 0 | 14 | |
| Indian | 3 | 1 | 7 | 0 | 3 | 0 | 13 | |
| Pakistani | 1 | 0 | 2 | 0 | 3 | 0 | 6 | |
| Mixed | 4 | 2 | 32 | 1 | 4 | 1 | 40 | |
| Other Asian | 2 | 1 | 3 | 0 | 1 | 0 | 6 | |
| Other Black | 1 | 0 | 2 | 0 | 1 | 0 | 4 | |
| Other ethinicity | 0 | 0 | 25 | 1 | 4 | 1 | 29 | |
| Total | 239 | 2149 | 673 | 3061 |
Knowledge of vaccination in pregnancy
Most HCWs (84%, n = 3379) were aware that pertussis and influenza vaccines were recommended during pregnancy. Most practice nurses (91%) correctly answered this question, followed by 85% of midwives and 59% of health visitors.
Overall there was good knowledge of both maternal immunisation programmes, although there were aspects of each programme where respondents were less clear as highlighted in Table 2. These five highlighted questions were analysed further using a model to look at whether a correct response to the question was associated with occupation, training or age. Whilst Question A was poorly answered, Health visitors were more likely to answer this correctly. Practice nurses and midwives were more likely to answer the other four questions correctly with the exception of question R which practice nurses were significantly more likely to answer correctly. For each of the five questions those who answered correctly were significantly more likely to have received training.
Table 2.
Influenza and pertussis knowledge questions and responses by healthcare worker group.
| Influenza and pertussis knowledge questions | Occupation | Correctly answered | % | Incorrectly answered | % | Unsure | % | Total | |
|---|---|---|---|---|---|---|---|---|---|
| A.Flu vaccination in pregnancy can protect a baby against flu disease from birth. | Health visitor | 128 | 54* | 55 | 23 | 56 | 23 | 239 | |
| Midwife | 827 | 38 | 972 | 45 | 365 | 17 | 2164 | ||
| Correct answer = True | Practice nurse | 313 | 46 | 250 | 37 | 112 | 17 | 675 | |
| Total | 1268 | 41 | 1277 | 41 | 533 | 17 | 3078 | ||
| B.Flu is not dangerous for babies. | Health visitor | 208 | 89 | 19 | 8 | 6 | 3 | 233 | |
| Correct answer = False | Midwife | 1887 | 88 | 134 | 6 | 117 | 5 | 2138 | |
| Practice nurse | 588 | 88 | 54 | 8 | 28 | 4 | 670 | ||
| Total | 2683 | 88 | 207 | 7 | 151 | 5 | 3041 | ||
| C.Flu vaccine in pregnancy protects the mother. | Health visitor | 223 | 94 | 3 | 1 | 12 | 5 | 238 | |
| Correct answer = True | Midwife | 2089 | 97 | 31 | 1 | 43 | 2 | 2163 | |
| Practice nurse | 671 | 99 | 4 | 1 | 6 | 1 | 681 | ||
| Total | 2983 | 97 | 38 | 1 | 61 | 2 | 3082 | ||
| D.There is good evidence that flu vaccination in pregnancy is safe. | Health visitor | 213 | 90 | 1 | 0 | 23 | 10 | 237 | |
| Correct answer = True | Midwife | 1968 | 91 | 37 | 2 | 157 | 7 | 2162 | |
| Practice nurse | 664 | 97 | 3 | 0 | 16 | 2 | 683 | ||
| Total | 2845 | 92 | 41 | 1 | 196 | 6 | 3082 | ||
| E.Pregnant women are at increased risk of serious complications from flu. | Health visitor | 206 | 87 | 10 | 4 | 22 | 9 | 238 | |
| Midwife | 2101 | 97 | 25 | 1 | 40 | 2 | 2166 | ||
| Correct answer = True | Practice nurse | 652 | 96 | 13 | 2 | 16 | 2 | 681 | |
| Total | 2959 | 96 | 48 | 2 | 78 | 3 | 3085 | ||
| F.Flu vaccination can be given at any stage of pregnancy. | Health visitor | 124 | 52 | 41 | 17 | 72 | 30 | 237 | |
| Correct answer = True | Midwife | 1769 | 82 | 197 | 9 | 194 | 9 | 2160 | |
| Practice nurse | 631 | 93 | 25 | 4 | 24 | 4 | 680 | ||
| Total | 2524 | 82 | 263 | 9 | 290 | 9 | 3077 | ||
| G.The vaccine can cause flu in pregnant women. | Health visitor | 182 | 78 | 20 | 9 | 31 | 13 | 233 | |
| Correct answer = False | Midwife | 1853 | 86 | 137 | 6 | 171 | 8 | 2161 | |
| Practice nurse | 658 | 97 | 4 | 1 | 19 | 3 | 681 | ||
| Total | 2693 | 88 | 161 | 5 | 221 | 7 | 3075 | ||
| H.Once a woman has received flu vaccine in pregnancy she will not need a further dose of vaccine in subsequent pregnancies. | Health visitor | 200 | 84 | 11 | 5 | 27 | 11 | 238 | |
| Midwife | 1956 | 90 | 105 | 5 | 102 | 5 | 2163 | ||
| Correct answer = False | Practice nurse | 643 | 94 | 24 | 4 | 17 | 2 | 684 | |
| Total | 2799 | 91 | 140 | 5 | 146 | 5 | 3085 | ||
| I.The flu and pertussis vaccine cannot be given at the same time. | Health visitor | 102 | 43 | 27 | 11 | 107 | 45 | 236 | |
| Correct answer = False | Midwife | 1303 | 60* | 264 | 12 | 600 | 28 | 2167 | |
| Practice nurse | 623 | 91* | 23 | 3 | 36 | 5 | 682 | ||
| Total | 2028 | 66 | 314 | 10 | 743 | 24 | 3085 | ||
| K.The pertussis programme for pregnant women in pregnant women has stopped. | Health visitor | 211 | 85 | 1 | 0 | 37 | 15 | 249 | |
| Midwife | 2047 | 93 | 10 | 0 | 136 | 6 | 2193 | ||
| Correct answer = False | Practice nurse | 675 | 97 | 2 | 0 | 16 | 2 | 693 | |
| Total | 2933 | 94 | 13 | 0 | 189 | 6 | 3135 | ||
| L.Whooping cough vaccination in pregnancy is safe for mother and baby. | Health visitor | 212 | 86 | 6 | 2 | 28 | 11 | 246 | |
| Midwife | 2001 | 91 | 30 | 1 | 160 | 7 | 2191 | ||
| Correct answer = True | Practice nurse | 676 | 97 | 3 | 0 | 16 | 2 | 695 | |
| Total | 2889 | 92 | 39 | 1 | 204 | 7 | 3132 | ||
| M.Whooping cough vaccination in pregnancy can protect a baby against whooping cough from birth. | Health visitor | 203 | 82 | 13 | 5 | 33 | 13 | 249 | |
| Midwife | 1963 | 89 | 84 | 4 | 148 | 7 | 2195 | ||
| Correct answer = True | Practice nurse | 676 | 97 | 7 | 1 | 12 | 2 | 695 | |
| Total | 2842 | 91 | 104 | 3 | 193 | 6 | 3139 | ||
| N.In England babies can still die from whoooping cough. | Health visitor | 235 | 95 | 2 | 1 | 10 | 4 | 247 | |
| Correct answer = True | Midwife | 2110 | 97 | 14 | 1 | 56 | 3 | 2180 | |
| Practice nurse | 684 | 99 | 3 | 0 | 7 | 1 | 694 | ||
| Total | 3029 | 97 | 19 | 1 | 73 | 2 | 3121 | ||
| O.Pregnant women are at increased risk of serious complications from whooping cough. | Health visitor | 52 | 20 | 151 | 60 | 48 | 19 | 251 | |
| Midwife | 714 | 33* | 998 | 46 | 476 | 22 | 2188 | ||
| Correct answer = False | Practice nurse | 308 | 45* | 241 | 35 | 138 | 20 | 687 | |
| Total | 1074 | 34 | 1390 | 44 | 662 | 21 | 3126 | ||
| P.Young babies with whooping cough are likely to need hospitlisation. | Health visitor | 232 | 93 | 4 | 2 | 13 | 5 | 249 | |
| Midwife | 2034 | 93 | 53 | 2 | 97 | 4 | 2184 | ||
| Correct answer = True | Practice nurse | 666 | 96 | 15 | 2 | 12 | 2 | 693 | |
| Total | 2932 | 94 | 72 | 2 | 122 | 4 | 3126 | ||
| Q.Whooping cough vaccine should be given in every pregnancy. | Health visitor | 134 | 54 | 38 | 15 | 75 | 30 | 247 | |
| Correct answer = True | Midwife | 1586 | 73* | 262 | 12 | 337 | 15 | 2185 | |
| Practice nurse | 571 | 82* | 73 | 11 | 49 | 7 | 693 | ||
| Total | 2291 | 73 | 373 | 12 | 461 | 15 | 3125 | ||
| R.Whooping cough vaccine is a combination vaccine with diptheria, tetanus and polio. | Health visitor | 84 | 34 | 119 | 48 | 47 | 19 | 250 | |
| Midwife | 688 | 31 | 1069 | 49 | 430 | 20 | 2187 | ||
| Correct answer = True | Practice nurse | 635 | 92* | 40 | 6 | 15 | 2 | 690 | |
| Total | 1407 | 45 | 1228 | 39 | 492 | 16 | 3127 |
A model was created on the highlighted questions looking at whether answering the question was associated with occupation, training and age.
*Indicates the professional group that were significantly more likely to answer the questions correctly. For the 5 questions highlighted, training was significantly associated with a correct response.
Attitudes towards vaccines and their intentions to vaccinate
Eighty-four percent of respondents would accept pertussis vaccine if they were pregnant; fewer would accept the influenza vaccine (73%). Practice nurses were most likely to report that they would accept pertussis and influenza vaccines (92% and 81% respectively), midwives (82%, 71%) and health visitors (78%, 71%).
Seventy-three percent and 74% of respondents indicated they routinely recommend influenza vaccine and pertussis vaccine respectively to pregnant women. There was an association between HCWs who indicated they would accept pertussis vaccine themselves if pregnant and who recommended pertussis vaccine (OR 6.3, CI 4.4–9.0) and influenza (OR 3.4, CI 2.4–4.7) vaccines to pregnant women (Table 3). Training and confidence were excluded as variables from the model due to collinearity.
Table 3.
Logistic regression of factors associated to recommending pertussis and influenza vaccines in pregnancy.
| Model 1: Recommend pertussis vaccine |
Model 2: Recommend the influenza vaccine |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Responses (%) | Univariable Odds ratio (95% CI) | P value | Multivariable Odds ratio (95% CI) | P value | Responses (%) | Univariable Odds ratio (95% CI) | P value | Multivariable Odds ratio (95% CI) | P value | |||||||||
| Did they have the healthcare worker flu vaccine in the 2014/15 season? | n = 2665 | n = 2684 | ||||||||||||||||
| No | 1707 (64) | 1 | 1 | 962 (36) | 1 | |||||||||||||
| Yes | 958 (36) | 3.7 | 3.0 | 4.7 | <0.001 | 1.7 | 1.3 | 2.9 | <0.001 | 1722 (64) | 3.9 | 3.1 | 4.9 | <0.001 | 1.7 | 1.3 | 2.3 | <0.001 |
| Occupation | n = 2814 | n = 2684 | ||||||||||||||||
| Health visitors | 192 (7) | 1 | 1 | 192 (7) | 1 | |||||||||||||
| Midwife | 1940 (69) | 1.1 | 0.8 | 1.6 | 0.564 | 1.2 | 0.8 | 2.0 | 0.374 | 1940 (69) | 1.2 | 0.8 | 1.7 | 0.407 | 1.3 | 0.8 | 2.1 | 0.242 |
| Practice Nurses | 682 (24) | 3.3 | 2.1 | 5.3 | <0.001 | 2.7 | 1.5 | 4.7 | 0.001 | 682 (24) | 2.9 | 1.9 | 4.6 | <0.001 | 2.3 | 1.3 | 3.9 | 0.002 |
| Would they personally have the whooping cough vaccine in pregnancy?* | n = 2545 | n = 2684 | ||||||||||||||||
| Would not have the vaccines in pregnancy | 335 (13) | 1 | 1 | 347 (14) | 1 | |||||||||||||
| Would have the vaccines in pregnancy | 2210 (87) | 9.3 | 7.2 | 12.0 | <0.001 | 6.3 | 4.4 | 9.0 | <0.001 | 2250 (86) | 7.1 | 5.5 | 9.1 | <0.001 | 3.4 | 2.4 | 4.7 | <0.001 |
| Would they personally have the flu vaccine in pregnancy?* | n = 2553 | n = 2577 | ||||||||||||||||
| Would not have the vaccines in pregnancy | 646 (25) | 1 | 1 | 652 (25) | 1 | |||||||||||||
| Would have the vaccines in pregnancy | 1907 (75) | 4.5 | 3.5 | 5.6 | <0.001 | 1.3 | 0.9 | 1.9 | 0.183 | 1925 (75) | 5.2 | 4.1 | 6.5 | <0.001 | 2.2 | 1.6 | 3.0 | <0.001 |
| Age | n = 2657 | n = 2676 | ||||||||||||||||
| 18-24 | 70 (3) | 1 | 1 | 71 (3) | 1 | 1 | ||||||||||||
| 25-34 | 380 (14) | 1.2 | 0.6 | 2.3 | 0.642 | 1.1 | 0.5 | 2.5 | 0.770 | 375 (14) | 1.2 | 0.7 | 2.3 | 0.518 | 1.4 | 0.7 | 2.9 | 0.377 |
| 35-44 | 487 (18) | 1.3 | 0.7 | 2.6 | 0.384 | 1.5 | 0.7 | 3.2 | 0.293 | 489 (18) | 1.6 | 0.9 | 3.0 | 0.115 | 2.2 | 1.1 | 4.4 | 0.330 |
| 45-54 | 1149 (43) | 1.6 | 0.9 | 3.1 | 0.121 | 1.2 | 0.6 | 2.4 | 0.687 | 1156 (43) | 1.9 | 1.1 | 3.4 | 0.032 | 1.6 | 0.8 | 3.0 | 0.188 |
| 55-64 | 543 (20) | 1.4 | 0.7 | 2.6 | 0.330 | 1.0 | 0.5 | 2.1 | 0.957 | 554 (21) | 1.7 | 0.9 | 3.1 | 0.094 | 1.4 | 0.7 | 2.7 | 0.386 |
| >65 | 28 (1) | 3.0 | 0.6 | 14.1 | 0.172 | 2.4 | 0.4 | 12.7 | 0.321 | 31 (1) | 4.2 | 0.9 | 19.6 | 0.66 | 3.8 | 0.7 | 19.7 | 0.108 |
*These questions were asked as theoretical questions.
Those who reported ‘This isn't relevant to my role’ as a response to ‘Do you recommend flu or whooping cough vaccination to pregnant women?’ were first excluded from the above analysis as there are certain roles that may not involve advising on vaccination, such as bereavement counselling. In total 431 and 430 reported that it was not part of their role to recommend influenza and pertussis vaccines respectively including; 25% of health visitors (n = 73), 14% of midwives (n = 333) and 4% practice nurses (n = 29). When the analysis was rerun withthese respondents categorised as not recommending the vaccines the only difference was that midwives became significantly more likely to recommend pertussis (Adjusted OR 1.7 CI 1.3 – 2.4, P<0.001) and influenza vaccine (Adjusted OR1.7 CI 1.3 −2.5 <0.001) than health visitors.
Overall, 1938 of 3088 (63%) respondents indicated they had received influenza vaccination as a HCW during the 2014/15 season. Practice nurses reported the highest uptake at 79% with health visitors at 61% and midwives 58%. HCWs who had received influenza vaccine were significantly more likely to recommend both vaccines to pregnant women (Table 3). Practice nurses were more likely to recommend the vaccines than other professional groups.
Concerns about side effects or personal illness/ allergy were most commonly cited as the reason for not accepting influenza vaccination (472/1091, 43%). The main motivators for being vaccinated were helping colleagues by not being sick at busy times (1224/1861, 66%) protecting themselves (1200/1861, 64%) and protecting patients (1161/1861, 62%).
Role with pregnant women
The most commonly cited involvement with pregnant women was answering questions (70%), followed by discussing vaccinations (66%), advising where women could be vaccinated (60%), checking whether pregnant women had received the right vaccinations (55%) and providing information (52%).Table 4 shows roles with pregnant women and vaccination as reported by the individual professional groups.
Table 4.
HCWs role with pregnant women and vaccination.
| Health Visitor (%) | Midwife (%) | Practice Nurse (%) | |
|---|---|---|---|
| I provide them with written information (%) | 53 (19) | 1300 (57) | 356 (50) |
| I discuss vaccination with them (%) | 86 (32) | 1485 (65) | 598 (84) |
| I answer any questions they may have (%) | 134 (49) | 1576 (69) | 602 (84) |
| I advise women where they can be vaccinated (%) | 102 (37) | 1579 (69) | 302 (42) |
| I check whether pregnant women have had the right vaccinations (%) | 65 (24) | 1300 (57) | 442 (62) |
| None of the above (%) | 75 (27) | 386 (17) | 51 (7) |
| Total | 273 | 2295 | 714 |
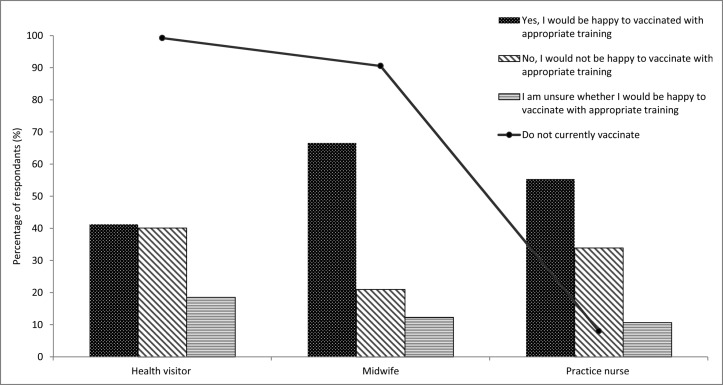
The majority (92%) of practice nurses indicated that they vaccinate pregnant women compared to 9% of midwives and 1% of health visitors. Of the 91% of midwives who did not currently vaccinate pregnant women, 67% would be happy to do so. Ninety-nine percent of health visitors did not currently vaccinate and 41% would be happy to do so. Of the 8% of practice nurses that do not administer vaccinations, 55% would be happy to vaccinate (Fig. 1).
Figure 1.
Respondents who do not currently vaccinate pregnant women and the proportions of these that would be happy to vaccinate with appropriate training, by professional group.
All groups indicated that midwives have the main responsibility for advising pregnant women on vaccination (86%). Thirty percent of practice nurses felt they themselves should have the main role in advising pregnant women.
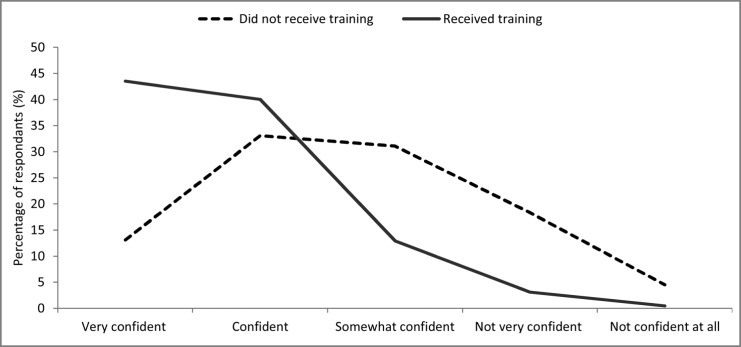
Of 3304 professionals surveyed, 1853 (56%) said they had not received training on vaccinations in pregnancy: 83% of health visitors, 62% of midwives, and 27% of practice nurses. Trained HCWs were generally more confident about giving advice in pregnancy (Fig. 2). Of those who had received training, 84% (95% CI 81%–86%) were confident advising pregnant women compared to 46% (95% CI 44%–48%) who had not received training.
Figure 2.
The confidence of respondents in giving advice to pregnant women according to whether they had or had not received training.
Discussion
It is important to understand the views of HCWs involved in advising and/or offering vaccines to pregnant women, to bridge the gap between vaccine recommendation and implementation. We found that a high proportion (74%) of practice nurses, midwives and health visitors recommend pertussis vaccine to pregnant women and 73% recommend influenza vaccine. At the time of the survey, coverage of the prenatal pertussis vaccines was 57.7%35 and coverage of the influenza vaccine was 41.3% in 2014/2015.36 National coverage in pregnant women has recently improved with earlier timing of pertussis vaccination and was 72.6% in March 2017.37 However influenza vaccine uptake was still only 44.8% in January 2017.38
This survey showed that practice nurses were well informed about maternal immunisation programmes and were more likely to recommend the influenza and pertussis vaccines to pregnant women than other professional groups. Administering immunisations is core to the practice nurse role and may underpin their positive attitudes to immunisations in pregnancy. Practice nurses were more likely to have received training and were more confident advising pregnant women. Health visitors on the other hand, usually have more contact postnatally and were less likely to have received vaccination training. In a relatively recent change, as part of the 5 key contacts39 the role of health visitors now includes a mandated contact at 28 weeks of pregnancy. Together with the advice to offer vaccination earlier, from around 20 weeks gestation,15 this visit offers an important opportunity to ensure that pregnant women have been vaccinated, provide additional information and advice about immunisation in pregnancy and to signpost women to vaccination.
In an uncomplicated pregnancy, midwives can provide all the antenatal care for a pregnant woman and play an important role in promoting vaccines. Pregnant women who receive a positive recommendation for vaccination from a healthcare provider are more likely to receive the vaccine.18,20 A UK survey of pregnant women and women with young children found these women were willing to be vaccinated and citing midwives in particular as their preferred source of information.19
Respondents in our survey also identified midwives as the professionals who should have the main responsibility for advising pregnant women on vaccination. However only 60% of midwives were confident giving advice compared to 82% of practice nurses; influenced by immunisation training they had received. Around 10% of midwives were vaccinating pregnant women; nearly 70% not currently vaccinating would be happy to do so with appropriate training. Whilst midwives may be willing to vaccinate, there are certain constraints which could currently hinder their ability to do so including; short appointment slots, lack of reimbursement, ensuring safe storage of vaccines in settings without storage facilities available. There are, however, an increasing number of areas in England where vaccination in pregnancy is locally commissioned from maternity services.
In the UK, the National Institute for Health and Care Excellence (NICE) has published draft guidelines to improve uptake of the flu vaccination.40 These emphasise the need to educate HCWs about flu vaccination, highlighting specifically; eligibility, transmission, safety and effectiveness and benefits of vaccination for people at high risk, including pregnant women. The draft guidelines outline that HCWs in contact with pregnant women should receive this training, raise awareness of the importance of flu vaccination and maximise opportunistic appointments such as antenatal visits. There are specific recommendations on improving occupational flu vaccination uptake including challenging misconceptions such as the vaccine can cause flu.
National estimated annual coverage of influenza vaccine among HCWs was 54.9% in 2014/15 at the time of the survey.41 GP practice nurses achieved highest uptake (64.4%). The uptake of influenza vaccine reported in our study was comparatively high with practice nurses reporting 79%. This may reflect that the 10% of members who completed our survey had generally more positive views about vaccination than non-responders.
The most common reason for accepting influenza vaccination was that this could help colleagues by not being sick at busy times; to our knowledge this has not previously been reported as a main motivation for influenza vaccination among HCWs. This is important because HCWs who received influenza vaccine were more likely to recommend vaccines to pregnant women.22 This highlights the importance of addressing potential barriers and beliefs in HCWs themselves regarding vaccination. It is therefore encouraging that uptake in HCWs has improved, reaching 63.4% in 2016/17.42
This study provided a valuable insight into respondents’ views. However, the limitations of cross-sectional studies apply, providing only a snapshot view. It is not possible to assess changes in opinions over time and the impact of programme changes, such as earlier pertussis immunisation in pregnancy in the UK. Due to the outbreak situation there was a rapid introduction of this programme with limited opportunities for tailored training pre-implementation.43 Efforts have since been made to improve training in healthcare professionals, particularly midwives, in the years after completion of the survey and this is likely to have affected views.
The survey is subject to selection and representation bias, for example the respondents might be largely those involved in or particularly interested in immunisation with polarised views. The main limitation was a relatively low response rate (10%). The survey was sent to all HCWs who were registered with the professional bodies and, for some, immunisation may not have been a key part of their role. To improve our response rate we could have further targeted HCWs through methods such newsletters and websites. However it is difficult to control denominators through these more open channels of communication. We did not have demographic details from the iHV and therefore cannot determine the representativeness for health visitors. Demographic data from the RCN and RCM, suggest those of white ethnicity and practice nurses aged between 45–54 were over-represented in our survey.
Although the low response rate does not affect the internal validity of the study findings, it may limit the generalisability of the results. This was a large study and similar UK studies investigating health professionals’ views of vaccines have been much smaller. The only other comparable study,27 included 3059 respondents and looked at influenza vaccination uptake among HCWs and their attitudes and beliefs towards vaccination.
PHE is engaging with professional groups to raise awareness of the programmes through professional magazines, oral and poster presentations at midwifery forums/conferences and development of online training resources for immunisation in pregnancy. PHE is producing; Patient Group Directions44 for vaccination of pregnant women, an updated patient information leaflet45 and updated antenatal and newborn screening resource cards for midwives that cover vaccination in pregnancy.46 These initiatives aim to improve knowledge of maternal vaccination programmes in midwives in particular and, with mandated contact at 28 weeks gestation for health visitors, it is important that resources are similarly developed to target this professional group. To fully assess the impact of these resources another survey could be undertaken.
The recent improvements in maternal pertussis vaccine uptake suggest efforts to engage with midwives in particular, together with programme changes, have had a positive impact. Since this survey was conducted, more training has taken place and therefore knowledge (see Table 2) and understanding of the programmes is likely to have improved consistent with increasing vaccine uptake.
Conclusions
-
•
A large proportion of HCWs recommended vaccination to pregnant women with practice nurses significantly more likely to do so;
-
•
Having influenza vaccine in their role as HCWs and their theoretical acceptance of pertussis vaccine were also significant factors in the likelihood of HCWs recommending vaccination to pregnant women.
-
•
The correlation between receipt of immunisation training and HCWs’ knowledge and confidence in recommending immunisation in pregnancy is important for both commissioners and providers of immunisation services and future public health strategies to improve maternal and infant health.
Method
Study design
Using an online questionnaire, we surveyed health visitors, midwives, and practice nurses working in England and members of one of three different professional bodies; 21,714 members of the RCM, 7000 members of the iHV and 5323 Practice nurses registered with the RCN. The survey ran from May to August 2015.
The survey was an anonymous self-administered, web-based questionnaire on the SelectSurvey platform (https://selectsurvey.net/). It was piloted amongst a small sample of each professional group prior to administering the main survey. The survey questions were re-ordered after the pilot study.
An invitation email (containing the link to the web based questionnaire) was sent to the iHV and RCN who forwarded the email to their registered members. PHE emailed RCM members directly to invite them to participate via a link to the survey. One subsequent reminder was emailed to the members of the three professional bodies. The questions were developed based on a literature review,19,47 similar previous surveys48,49 for parents and current vaccination guidelines. The questionnaire consisted of 35 close ended questions on five topics 1) knowledge of vaccines recommended in pregnancy 2) perceptions of their role in advising and administering immunisations in pregnant women 3) motivating factors for accepting and rejecting seasonal influenza vaccine for HCWs 4) comfort levels with advising on and administration of influenza and pertussis vaccines and 5) demographics.
Data analysis
The outcome variable selected for multiple logistic regression was whether the respondent recommended pertussis and/or influenza vaccine to pregnant women based on the question ‘do you recommend flu or whooping cough vaccination to pregnant women?’. The response options were ‘Yes I routinely recommend the vaccine’, ‘I recommend the vaccine if a women asks my opinion’, ‘I do not give my opinion as it is the woman's choice’ ‘I routinely advise against receiving the vaccine’ and ‘I advise against having the vaccine if the woman asks my opinion’. The first two options were grouped as recommending the vaccines and the last 3 were grouped as not recommending the vaccine. Respondents who indicated ‘This isn't relevant to my role’ were excluded from the analysis and the model was then rerun including these respondents as not recommending the vaccines, to look for any differences.
Chi-square test was used to identify significant associations between recommending the vaccine and different explanatory variables, such as age and whether they had received flu vaccination for HCWs. The variables with P<0.001 in univariate analyses were entered into a multiple logistic regression analysis to identify factors associated with recommending the vaccines to pregnant women. Data were analysed using STATA software.
This study was not classified as a research study as defined by National Research Ethics Service (NRES) (http://www.hra.nhs.uk/) and therefore did not require ethics approval.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Dabrera G, Zhao H, Andrews N, Begum F, Green H, Ellis J, Elias K, Donati M, Zambon M, Pebody R. Effectiveness of seasonal influenza vaccination during pregnancy in preventing influenza infection in infants, England, 2013/14. Euro Surveill. 2014;19(45):20959. doi: 10.2807/1560-7917.ES2014.19.45.20959. PMID:25411687 [DOI] [PubMed] [Google Scholar]
- 2.Dabrera G, Amirthalingam G, Andrews N, Campbell H, Ribeiro S, Kara E, Fry NK, Ramsay M. A case-control study to estimate the effectiveness of maternal pertussis vaccination in protecting newborn infants in England and Wales, 2012–2013. Clin Infect Dis. 2015;60(3):333-7. doi: 10.1093/cid/ciu821. PMID:25332078 [DOI] [PubMed] [Google Scholar]
- 3.Amirthalingam G, Andrews N, Campbell H, Ribeiro S, Kara E, Donegan K, Fry NK, Miller E, Ramsay M. Effectiveness of maternal pertussis vaccination in England: An observational study. Lancet. 2014;384(9953):1521-8. doi: 10.1016/S0140-6736(14)60686-3. PMID:25037990 [DOI] [PubMed] [Google Scholar]
- 4.Department of Health, Public Health England, NHS England The national flu immunisation programme 2016/17. 2016. [Google Scholar]
- 5.Pebody RG, McLean E, Zhao H, Cleary P, Bracebridge S, Foster K, Charlett A, Hardelid P, Waight P, Ellis J, et al.. Pandemic influenza A (H1N1) 2009 and mortality in the United Kingdom: Risk factors for death, April 2009 to March 2010. Euro Surveill. 2010;15(20):pii=19571. doi: 10.2807/ese.15.20.19571-en [DOI] [PubMed] [Google Scholar]
- 6.Tamma PD, Ault KA, del Rio C, Steinhoff MC, Halsey NA, Omer SB. Safety of influenza vaccination during pregnancy. Am J Obstet Gynecol. 2009;201(6):547-52. doi: 10.1016/j.ajog.2009.09.034. PMID:19850275 [DOI] [PubMed] [Google Scholar]
- 7.Donegan K, King B, Bryan P. Safety of pertussis vaccination in pregnant women in UK: Observational study. BMJ. 2014;349:g4219. doi: 10.1136/bmj.g4219. PMID:25015137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sakala IG, Honda-Okubo Y, Fung J, Petrovsky N. Influenza immunization during pregnancy: Benefits for mother and infant. Hum Vaccin Immunother. 2016;12(12):3065-71. doi: 10.1080/21645515.2016.1215392. PMID:27494630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaman K, Roy E, Arifeen SE, Rahman M, Raqib R, Wilson E, Omer SB, Shahid NS, Breiman RF, Steinhoff MC. Effectiveness of maternal influenza immunization in mothers and infants. N Engl J Med. 2008;359(15):1555-64. doi: 10.1056/NEJMoa0708630. PMID:18799552 [DOI] [PubMed] [Google Scholar]
- 10.Public Health England Influenza immunisation programme for England: GP patient groups. Data collection survey: Season 2015 to 2016. 2016. [Google Scholar]
- 11.Amirthalingam G. Strategies to control pertussis in infants. Arch Dis Child. 2013;98(7):552-5. doi: 10.1136/archdischild-2012-302968. PMID:23698594 [DOI] [PubMed] [Google Scholar]
- 12.Department of Health Pregnant women to be offered whooping cough vaccination. 2012. Available from: https://www.gov.uk/government/news/pregnant-women-to-be-offered-whooping-cough-vaccination.
- 13.Eberhardt CS, Blanchard-Rohner G, Lemaitre B, Boukrid M, Combescure C, Othenin-Girard V, Chilin A, Petre J, de Tejada BM, Siegrist CA. Maternal immunization earlier in pregnancy maximizes antibody transfer and expected infant seropositivity against pertussis. Clin Infect Dis. 2016;62(7):829-36. doi: 10.1093/cid/ciw027. PMID:26797213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joint Commitee on Vaccination and Immunisation (JCVI) Minute of the meeting on 3rd Feb 2016. 2016. [Google Scholar]
- 15.Public Health England Immunisation against infectious disease. The Green Book. 2016. https://www.gov.uk/government/publications/pertussis-the-green-book-chapter-24. [Google Scholar]
- 16.Baxter R, Bartlett J, Fireman B, Lewis E, Klein NP. Effectiveness of vaccination during pregnancy to prevent infant pertussis. Pediatrics. 2017;139(5). doi: 10.1542/peds.2016-4091. PMID:28557752 [DOI] [PubMed] [Google Scholar]
- 17.Department of Health, Public Health England, NHS England Continuation of temporary programme of pertussis (whooping cough) vaccination of pregnant women 2013. 2013. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/197839/130510_Pertussis_continuation_letter_FINAL.pdf.
- 18.Wiley KE, Massey PD, Cooper SC, Wood NJ, Ho J, Quinn HE, Leask J. Uptake of influenza vaccine by pregnant women: A cross-sectional survey. Med J Aust. 2013;198(7):373-5. doi: 10.5694/mja12.11849. PMID:23581957 [DOI] [PubMed] [Google Scholar]
- 19.Campbell H, Hoek AJV, Bedford H, Craig L, Yeowell A-L, Green D, et al.. Attitudes to immunisation in pregnancy among women in the UK targeted by such programmes. Br J Midwifery. 2015;23(8):566-73. doi: 10.12968/bjom.2015.23.8.566. [DOI] [Google Scholar]
- 20.Blanchard-Rohner G, Meier S, Ryser J, Schaller D, Combescure C, Yudin MH, Burton-Jeangros C, de Tejada BM, Siegrist CA. Acceptability of maternal immunization against influenza: The critical role of obstetricians. J Matern Fetal Neonatal Med. 2012;25(9):1800-9. doi: 10.3109/14767058.2012.663835. PMID:22339083 [DOI] [PubMed] [Google Scholar]
- 21.Eppes C, Wu A, Cameron KA, Garcia P, Grobman W. Does obstetrician knowledge regarding influenza increase HINI vaccine acceptance among their pregnant patients? Vaccine. 2012;30(39):5782-4. doi: 10.1016/j.vaccine.2012.06.032. PMID:22743135 [DOI] [PubMed] [Google Scholar]
- 22.Lu AB, Halim AA, Dendle C, Kotsanas D, Giles ML, Wallace EM, Buttery JP, Stuart RL. Influenza vaccination uptake amongst pregnant women and maternal care providers is suboptimal. Vaccine. 2012;30(27):4055-9. doi: 10.1016/j.vaccine.2012.04.012. PMID:22521842 [DOI] [PubMed] [Google Scholar]
- 23.Wiley KE, Cooper SC, Wood N, Leask J. Understanding pregnant women's attitudes and behavior toward influenza and pertussis vaccination. Qual Health Res. 2015;25(3):360-70. doi: 10.1177/1049732314551061. PMID:25246330 [DOI] [PubMed] [Google Scholar]
- 24.Sampson R, Wong L, Macvicar R. Parental reasons for non-uptake of influenza vaccination in young at-risk groups: A qualitative study. Br J Gen Pract. 2011;61(588):e386-91. doi: 10.3399/bjgp11X583155. PMID:21722445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schindler M, Blanchard-Rohner G, Meier S, Martinez de Tejada B, Siegrist CA, Burton-Jeangros C. Vaccination against seasonal flu in Switzerland: The indecision of pregnant women encouraged by healthcare professionals. Revue d'Épidémiologie et de Santé Publique. 2012;60(6):447-53. doi: 10.1016/j.respe.2012.03.008. PMID:23141298 [DOI] [PubMed] [Google Scholar]
- 26.Marsh HA, Malik F, Shapiro E, Omer SB, Frew PM. Message framing strategies to increase influenza immunization uptake among pregnant African American women. Matern Child Health J. 2014;18(7):1639-47. doi: 10.1007/s10995-013-1404-9. PMID:24337776 [DOI] [PubMed] [Google Scholar]
- 27.Shrikrishna D, Williams S, Restrick L, Hopkinson NS. Influenza vaccination for NHS staff: Attitudes and uptake. BMJ Open Respir Res. 2015;2(1):e000079. doi: 10.1136/bmjresp-2015-000079. PMID:26019875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ishola DA Jr., Permalloo N, Cordery RJ, Anderson SR. Midwives' influenza vaccine uptake and their views on vaccination of pregnant women. J Public Health (Oxf). 2013;35(4):570-7. doi: 10.1093/pubmed/fds109. PMID:23365262 [DOI] [PubMed] [Google Scholar]
- 29.Mytton OT, O'Moore EM, Sparkes T, Baxi R, Abid M. Knowledge, attitudes and beliefs of health care workers towards influenza vaccination. Occup Med. 2013;63(3):189-95. doi: 10.1093/occmed/kqt002. PMID:23447033 [DOI] [PubMed] [Google Scholar]
- 30.Shrikrishna D, Williams S, Restrick L, Hopkinson NS. Influenza vaccination for NHS staff: Attitudes and uptake. BMJ Open Respir Res. 2015;2(1):e000079. doi: 10.1136/bmjresp-2015-000079. PMID:26019875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Collins J, Alona I, Tooher R, Marshall H. Increased awareness and health care provider endorsement is required to encourage pregnant women to be vaccinated. Hum Vaccin Immunother. 2014;10(10):2922-9. doi: 10.4161/21645515.2014.971606. PMID:25483464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Healy CM, Rench MA, Montesinos DP, Ng N, Swaim LS. Knowledge and attitiudes of pregnant women and their providers towards recommendations for immunization during pregnancy. Vaccine. 2015;33(41):5445-51. doi: 10.1016/j.vaccine.2015.08.028. PMID:26307234 [DOI] [PubMed] [Google Scholar]
- 33.Beel ER, Rench MA, Montesinos DP, Mayes B, Healy CM. Knowledge and attitudes of postpartum women toward immunization during pregnancy and the peripartum period. Hum Vaccin Immunother. 2013;9(9):1926-31. doi: 10.4161/hv.25096. PMID:23782490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meharry PM, Colson ER, Grizas AP, Stiller R, Vazquez M. Reasons why women accept or reject the trivalent inactivated influenza vaccine (TIV) during pregnancy. Matern Child Health J. 2013;17(1):156-64. doi: 10.1007/s10995-012-0957-3. PMID:22367067 [DOI] [PubMed] [Google Scholar]
- 35.Public Health England Pertussis vaccination programme for pregnant women: Vaccine coverage estimates in England, June to September 2015. 2015. Available from: https://www.gov.uk/government/publications/pertussis-immunisation-in-pregnancy-vaccine-coverage-estimates-in-england-october-2013-to-march-2014.
- 36.Public Health England Seasonal flu vaccine uptake in GP patients in England: Winter season 2014 to 2015. 2015. [Google Scholar]
- 37.Public Health England Pertussis Vaccination Programme for Pregnant Women update: Vaccine coverage in England, January to March 2017. 2017. www.gov.uk.
- 38.Public Health England Seasonal flu vaccine uptake in GP patients: Provisional monthly data for 1 Septemeber 2016 to 31 January 2017 by area team and CCG. 2017. [Google Scholar]
- 39.Public Health England, Department of Health Health visiting programme: Pathway to support professional practice and deliver new service offer: Health visiting and midwifery partnership–pregnancy and early weeks. 2015. [Google Scholar]
- 40.(NICE) NIfHaCE Flu vaccination: Increasing uptake: Draft guidance consultation 2017. 2017. Available from: https://www.nice.org.uk/guidance/indevelopment/gid-phg96/consultation/html-content.
- 41.Public Health England Seasonal flu vaccine uptake amongst frontline healthcare workers (HCWs) in England: Winter season 2014 to 2015. 2015. [Google Scholar]
- 42.Public Health England Seasonal flu vaccine uptake in healthcare workers 2016 to 2017: Provisional monthly data for 1 September 2016 to 28 February 2017. 2017. [Google Scholar]
- 43.Amirthalingam G, Letley L, Campbell H, Green D, Yarwood J, Ramsay M. Lessons learnt from the implementation of maternal immunization programs in England. Hum Vaccin Immunother. 2016;12(11):2934-9. doi: 10.1080/21645515.2016.1210730. PMID:27454010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Public Health England Immunisation patient group direction (PGD) templates 2015. 2015. Available from: https://www.gov.uk/government/collections/immunisation-patient-group-direction-pgd.
- 45.Public Health England Pregnancy: How to help protect you and your baby 2016. 2016. Available from: https://www.gov.uk/government/publications/pregnancy-how-to-help-protect-you-and-your-baby.
- 46.Public Health England Resource Cards 2016. 2016. Available from: https://cpdscreening.phe.org.uk/resource-cards.
- 47.Campbell H, Edwards A, Letley L, Bedford H, Ramsay M, Yarwood J. Changing attitudes to childhood immunisation in English parents. Vaccine. 2017;35(22):2979-85. doi: 10.1016/j.vaccine.2017.03.089. PMID:28442229 [DOI] [PubMed] [Google Scholar]
- 48.Public Health England. Vaccination against pertussis (whooping cough) for pregnant women www.gov.uk: Public Health England. 2016. Available from: https://www.gov.uk/government/publications/vaccination-against-pertussis-whooping-cough-for-pregnant-women.
- 49.Public Health England. Influenza vaccination in pregnancy: Advice for healthcare professionals www.gov.uk: Public Health England. 2014. Available from: https://www.gov.uk/government/publications/vaccination-against-pertussis-whooping-cough-for-pregnant-women.