Abstract
Objective
To determine the frequency of and predictive factors for optic nerve head edema (ONHE) among patients with headache, neurologic deficit, visual loss, or elevated blood pressure in the emergency department (ED).
Methods
Cross-sectional analysis was done of patients with ONHE in the prospective Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study. Demographics, neuroimaging results, management, and patient disposition were collected. Patients in the ONHE and non-ONHE groups were compared with bivariate and logistic regression analyses.
Results
Of 1,408 patients included, 37 (2.6%, 95% confidence interval 1.9–3.6) had ONHE (median age 31 [interquartile range 26–40] years, women 27 [73%], black 28 [76%]). ONHE was bilateral in 27 of 37 (73%). Presenting complaints were headache (18 of 37), visual loss (10 of 37), acute neurologic deficit (4 of 37), elevated blood pressure (2 of 37), and multiple (3 of 37). The most common final diagnoses were idiopathic intracranial hypertension (19 of 37), CSF shunt malfunction/infection (3 of 37), and optic neuritis (3 of 37). Multivariable logistic regression found that body mass index ≥35 kg/m2 (odds ratio [OR] 1.9, p = 0.0002), younger age (OR 0.5 per 10-year increase, p < 0.0001), and visual loss (OR 5, p = 0.0002) were associated with ONHE. Patients with ONHE were more likely to be admitted (62% vs 19%), to be referred to other specialists (100% vs 54%), and to receive neuroimaging (89% vs 63%) than patients without ONHE (p < 0.001). Fundus photographs in the ED allowed initial diagnosis of ONHE for 21 of 37 (57%) patients. Detection of ONHE on ED fundus photography changed the final diagnosis for 10 patients.
Conclusions
One in 38 patients (2.6%) presenting to the ED with a chief complaint of headache, neurologic deficit, visual loss, or elevated blood pressure had ONHE. Identification of ONHE altered patient disposition and contributed to the final diagnosis, confirming the importance of funduscopic examination in the ED.
Optic nerve head edema (ONHE) is one of the most important red flags among patients presenting to the emergency department (ED).1,2 The presence of ONHE often signifies underlying ocular inflammatory or ischemic disease (e.g., optic neuritis, posterior uveitis, or ischemic optic neuropathy), neurologic disease with elevated intracranial pressure (ICP) (e.g., intracranial tumors, idiopathic intracranial hypertension [IIH], meningitis), or systemic diseases (e.g., malignant hypertension). Hence, detection of ONHE often triggers multiple investigations, including neuroimaging and lumbar puncture, specialty consultations, and hospital admission.
The Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) was a prospective 3-phase study that looked at the feasibility, diagnostic accuracy, and use of nonmydriatic fundus photography among patients presenting to the ED.3–7 These studies showed that nonmydriatic retinal photography in the ED is feasible, is superior to direct ophthalmoscopy, and may improve patient care and outcomes when systematically performed in selected patients.8
There is limited knowledge about the prevalence of ONHE in ED patients. The purpose of our study was to describe the frequency of and predictive factors for ONHE among patients presenting to the ED with a chief complaint of headache, acute neurologic deficit, acute vision loss, or an elevated blood pressure (BP) in the FOTO-ED study. In addition, we evaluated whether ONHE altered the management and disposition of these patients.
Methods
Standard protocol approvals, registrations, and patient consents
The study was approved by our Institutional Review Board. Informed consent was obtained from study participants enrolled in phases I and II of the FOTO-ED study with a modified written consent procedure. Phase III was a quality improvement project reviewed as exempt from Institutional Review Board review at the time of execution, and we obtained approval for a retrospective review of cases included during phase III for this study.
Study population
The present analysis is a cross-sectional study of the subset of patients in the FOTO-ED study with ONHE in 1 or both eyes compared to those without ONHE. The FOTO-ED study was a 3-phase sequential, cross-sectional study conducted between April 2009 and August 2011 (phases I and II) and between March and December 2014 (phase III). The first phase evaluated the routine clinical use of direct ophthalmoscopy by emergency providers (EPs) (350 patients),4 whereas the second phase evaluated the routine use of nonmydriatic ocular fundus photography interpreted by the EPs (354 patients).5 Between the first and second active FOTO-ED enrollment phases, an additional 118 patients meeting all relevant study criteria were included.6 The third phase was a quality improvement project evaluating a web-based educational module on fundus photography interpretation by EPs (586 patients).7 The inclusion criteria for the FOTO-ED study were adult patients presenting to the ED with a chief complaint of headache, focal neurologic deficits, acute vision loss, or diastolic BP ≥120 mm Hg.
Fundus photographs
Photographs of the posterior pole of the ocular fundus (optic disc, macula, and major retinal vessels) were obtained from both eyes of patients with a nonmydriatic ocular fundus camera (Kowa nonmyd-a-D 5-megapixel camera; Kowa Optimed, Inc, Torrance, CA) according to previously described methods.3,4
All photographs were reviewed by at least 2 neuro-ophthalmologists. Photograph quality was rated on a 5-point scale as previously described.9 Fundus photographs identified as having ONHE were subsequently reviewed by 3 neuro-ophthalmologists for laterality (unilateral or bilateral), distribution (segmental or diffuse), and severity per the modified Frisén scale.10 When disc edema was bilateral but asymmetric, the grade in the worse eye was used. Associated optic nerve head pallor was also noted. For the purposes of statistical analysis, severity of the ONHE was graded on a binary scale: severe (Frisén grade ≥3) and mild to moderate (Frisén grades 1–2).
Data collected on all participants
Data regarding demographics (age, sex, race, and body mass index [BMI]), presenting complaints, and referral pattern to the ED were collected prospectively for all patients. Medical history, medications, imaging, diagnosis by EPs, final diagnosis, consultations, length of stay in the ED, and other interventions were ascertained from medical records. Brain imaging interpretations were based on the final radiology reports.
Data collected on patients with ONHE only
Snellen visual acuity, visual field testing (Humphrey visual fields [HVFs] or Goldmann manual perimetry [GVF]), pupillary examination, and concomitant cranial nerve palsies at the time of presentation and follow-up were recorded for the patients with ONHE.
For analysis, Snellen visual acuity was converted to logMAR visual acuity. Formal visual fields were systematically reviewed. Mean deviations were recorded for the HVFs. All visual field defects (both HVFs and GVFs) were graded on a 4-point scale as (1) normal, (2) enlargement of the blind spot, (3) nasal or temporal defect, or (4) diffusely constricted.11 For analysis, in patients with unilateral ONHE, the affected eye was used; for patients with bilateral ONHE, the worse eye was used.
The use of direct ophthalmoscopy or nonmydriatic fundus photography by EPs and the diagnostic accuracy of EPs' interpretation were prospectively recorded. Whether ONHE prompted further evaluations and changed the diagnosis made by EPs at presentation was recorded.
Statistical analysis
Statistical analysis was performed with R (R Foundation for Statistical Computing, R-project.org). Two-tailed values of p ≤ 0.05 were considered statistically significant. Medians and interquartile ranges (IQRs) were reported for continuous data, and percentages were reported for categorical data. Appropriate parametric and nonparametric tests were used to compare groups (medians, Mann-Whitney U test; proportions, χ2 or Fisher exact test).
Binary logistic regression was performed, with the presence of ONHE as the outcome and with age, sex, race, BMI, presenting complaint, and history of systemic risk factors as multiple predictors of interest, controlling for the phase of the FOTO-ED study in which the patient was enrolled. Model selection was performed with the method of Kleinbaum and Klein.12
Results
Demographic and clinical features of patients with ONHE
The FOTO-ED studies included 1,408 patients, among whom 37 (2.6%, 95% confidence interval 1.9–3.6) had ONHE. Median age of patients with ONHE was 31 (IQR 26–40) years; 73% (27 of 37) were women; and 76% (28 of 37) were black. Chief complaints included headache (18 of 37), acute vision loss (10 of 37), acute neurologic deficit (4 of 37), elevated BP (2 of 37), headache and vision loss (2 of 37), and vision loss and neurologic deficit (1 of 37). Median duration of presenting complaints was 6 (IQR 2–15, range 1–120) days.
ONHE was bilateral in 27 of 37 (73%) patients. Among these 27 patients, ONHE was diffuse in 26 (96%) and severe (Frisén grade ≥3) in 23 (85%). Among the 10 patients with unilateral edema, ONHE was diffuse in 8 (80%) and severe in 4 (40%). Six of the 37 (16.2%) patients also had pallor indicating atrophic ONHE. Four (10.8%) had associated cranial nerve palsies (2 patients with IIH, 1 with shunt dysfunction with unilateral or bilateral nerve VI palsies, and 1 with neurosarcoidosis with cranial nerve III, VI, and VII palsies).
Visual function of patients with ONHE
At presentation, median visual acuity (available for 23 patients) was 0.1 logMAR (range 20/20 to no light perception). Formal visual fields were performed in 18 patients and demonstrated a central field defect in 9 (50%), enlargement of the physiologic blind spot in 4, a nasal/temporal field defect in 2, and diffuse constriction in 3.
For the 18 patients with visual acuity data and follow-up of at least 3 months, median improvement in visual acuity was 1 line (range 0–0.3) logMAR. Among 10 patients for whom follow-up visual fields were available, 4 (40%) showed improvement, 3 (30%) were stable, and 3 (30%) were worse.
At last follow-up, 12 of 18 (67%) patients had good recovery, 2 (11%) had final visual acuity of no better than 20/100, and 2 (11%) had severe visual impairment with final visual acuity of no better than 20/200.
ED management and outcomes of patients with ONHE
Twenty-three (62%) patients with ONHE were admitted to the hospital for further evaluation and management. Median hospital length of stay was 2 (IQR 1–3, range 0–21) days. Average follow-up available was 42 (range 0–387) weeks. Seventeen (46%) patients were lost to follow-up.
On average, each patient was referred to 2 physicians (IQR 1–2, range 1–3); however, 5 (13.5%) patients were referred to >2 specialists. Twenty-six (70.3%) were referred to a neuro-ophthalmologist.
Thirty-three (89%) patients underwent neuroimaging. The median number of neuroimaging studies performed was 2 (IQR 1–3, range 0–4). Eleven (30%) patients underwent >2 imaging modalities. Twenty-five of 33 (76%) patients who underwent neuroimaging had an acute abnormality.
Lumbar puncture was performed in 23 patients and was diagnostic in 19 (83%) patients: 15 had elevated CSF opening pressure (OP); 2 showed acute infection (1 each with meningitis and ventriculoperitoneal shunt infection); and 2 had increased lymphocytes and/or oligoclonal bands (patients with optic neuritis). Of the 19 patients with a final diagnosis of IIH, 14 had an elevated CSF-OP, and 2 had borderline OP of 24 cm H2O but had accompanying neuroimaging findings suggestive of elevated ICP. In the remaining 3 patients with the final diagnosis of IIH, CSF-OP was not documented but was recorded as elevated.
Final diagnoses were IIH (19 of 37); CSF shunt malfunction/infection (3 of 37); optic neuritis (3 of 37); 2 each with brain tumor, cerebral venous sinus thrombosis, malignant hypertension, and nonarteritic anterior ischemic optic neuropathy; and 1 each with cerebral infarction, meningitis, neurosarcoidosis, and retinopathy. A life-threatening diagnosis was made in 8 (22%) patients.
Twenty-four (65%) patients were treated medically and 8 (22%) surgically. One patient with a brain tumor refused surgery. Nonarteritic ischemic optic neuropathy was observed in 2 patients. Definitive follow-up information was available for 18 patients 3 months after the ED visit: 1 patient had prolonged morbidity and 1 died.
Referral pattern and EP performance
On average, each patient saw 1 (range 0–4) other physician before referral to the ED. Sixteen of 37 (43%) patients were sent to the ED with a diagnosis of ONHE already made by the referring physicians; ED fundus photographs first established the diagnosis of ONHE in the other 21 patients (57%). EPs detected ONHE in 11 of 16 (69%) patients with a prior known diagnosis of ONHE and in only 5 of 21 (24%) patients in whom ONHE was revealed in the ED by fundus photography. EPs did not diagnose ONHE in any patient using direct ophthalmoscopy (phase I) but accurately detected ONHE in 16 of 23 (70%) patients using fundus photographs themselves (phases II and III). Performance of EPs was not affected by the grade, laterality, or pattern of ONHE (p > 0.8). Among the 21 patients in whom ONHE was first detected by photographs in the ED, the final diagnosis for 7 (33%) was consequently changed to IIH, resulting in altered management and disposition. In another 3 patients who were referred to the ED with a diagnosis of ONHE, intra-ED photographs convinced EPs to pursue further workup with a resultant change in final diagnosis (1 patient initially diagnosed with tension headaches was ultimately diagnosed with IIH, and 2 patients initially diagnosed with IIH were found to have cerebral venous sinus thrombosis).
Comparison to patients without ONHE
Patients with ONHE tended to be younger (median age 31 vs 46 years, p < 0.001), had a higher BMI (34.3 vs 27.9 kg/m2, p < 0.001), and were more frequently black (76% vs 54%, p = 0.01) compared to patients in the non-ONHE group (table 1). Patients with ONHE were more likely to present with acute vision loss (35% vs 16%, p = 0.01) and to have a history of IIH (14% vs 2%, p < 0.001) and systemic thyroid dysfunction (5% vs 0%, p = 0.02) than patients in the non-ONHE group.
Table 1.
Univariate analysis of patients' characteristics between the ONHE and non-ONHE groups
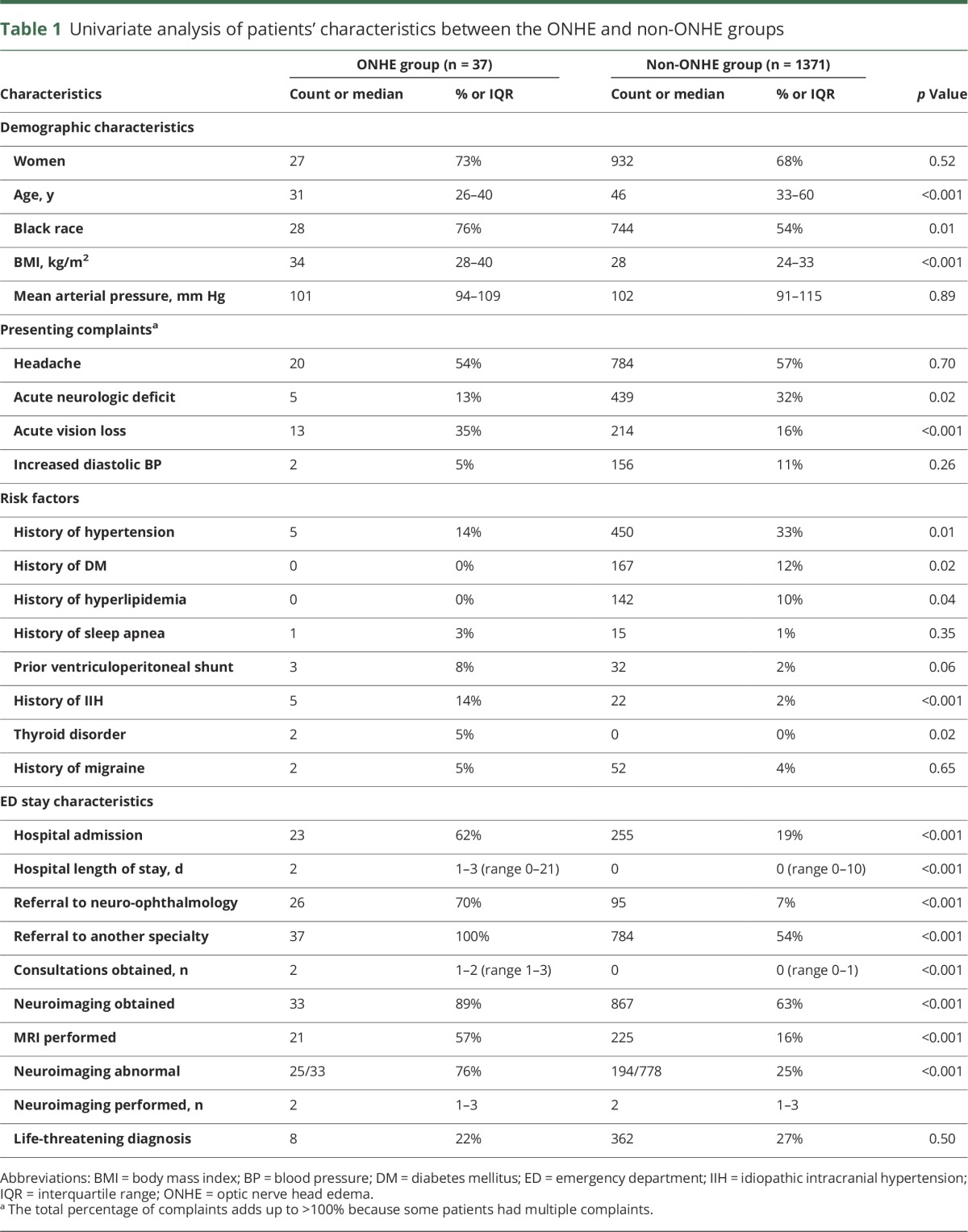
Patients with ONHE were more likely to be admitted to and stay longer in the hospital, to undergo brain imaging, and to have abnormal neuroimaging (table 1). In addition, they were more likely to be referred to other physicians and to be seen in neuro-ophthalmology consultation.
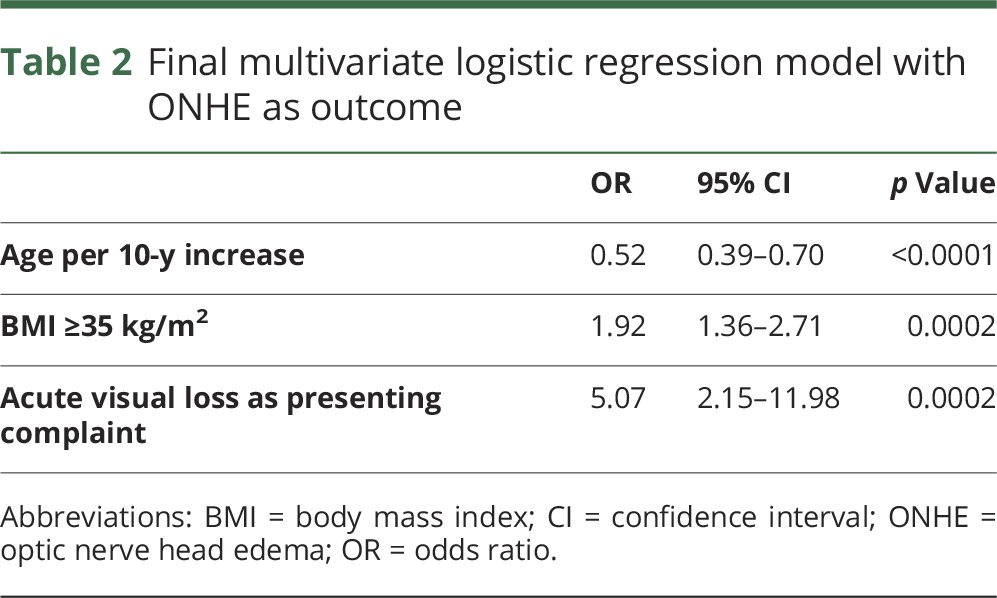
Multivariable logistic regression found that younger age (odds ratio [OR] 0.5 per 10-year increase, p < 0.0001), BMI ≥35 kg/m2 (OR 1.9, p = 0.0002), and acute vision loss (OR 5, p = 0.0002) were independently associated with ONHE.
Discussion
Our study found that 2.6% of patients presenting to the ED with a chief complaint of headache, acute vision loss, focal neurologic deficit, or a diastolic BP ≥120 mm Hg had ONHE. This implies that ≈1 of every 38 patients presenting to the ED with these features has ONHE, reiterating the importance of ocular fundus examination in these patients.
Although there is limited literature reporting the prevalence of ONHE among patients in the ED, prior studies have suggested that ONHE might be observed among 2% to 28% of patients presenting to the ED with neurologic conditions such as intracranial tumors,13 aneurysms,14 or meningitis.15,16 The higher prevalence of ONHE seen in these studies compared with ours likely represents enrichment from their narrower inclusion criteria.
In our study, headache was the most common presenting complaint. Headache is the fourth most common chief complaint among patients presenting to EDs and is the single most common neurologic complaint.17 The presence of ONHE in patients with headache signifies a secondary cause for the headache and the need for further urgent evaluation.2,18,19 In our current study, 19 of 630 (3%) patients with headaches had ONHE. This suggests that ONHE would be present in ≈90,000 of the >3 million patients who visit EDs for headache every year in the United States, underscoring the importance of ocular fundus examination among all patients presenting to the ED with headache for whom ONHE may be the only indication of severe underlying disease.20 Acute vision loss was the second most common complaint seen in patients with ONHE and was the only presenting complaint that was more frequent in the ONHE group than in the non-ONHE group (tables 1 and 2). Although only a few hypertensive patients had ONHE (diagnostic of grade IV hypertensive retinopathy), our prevalence of ONHE in malignant hypertension was similar to prior reports.21,22 Because these patients are at high risk of end-organ damage, including renal failure, heart failure, and stroke, it is important to examine the ocular fundus when the BP is severely elevated to potentially identify this important clue to the severity of the disease.
Table 2.
Final multivariate logistic regression model with ONHE as outcome
In our study, elevated ICP (secondary to IIH, CSF shunt malfunction, or cerebral venous sinus thrombosis) was the underlying etiology among almost all patients with bilateral ONHE. A prior report from an ophthalmic ED in France similarly found IIH to be the most common final diagnosis among 50 consecutive cases of bilateral disc edema.23 In that study, 39 patients had elevated ICP on lumbar puncture, and further workup led to a final diagnosis of IIH in 30 patients and of cerebral venous thrombosis in 9. Because patients with IIH are usually unaware of visual field defects until vision is severely affected, these patients are often misdiagnosed as having primary headache disorders. Indeed, previous studies have reported that a majority of patients ultimately diagnosed with IIH visit the ED multiple times before their disease is diagnosed.24,25 Thus, it is critical that ocular fundus examination be performed lest an ED visit become a missed opportunity to make the correct diagnosis of IIH and to avoid potentially severe visual sequelae.
Unilateral ONHE was caused by increased ICP in 4 of our 10 patients, emphasizing that unilateral ONHE can also reveal intracranial hypertension.26–28 The remainder of our patients with unilateral ONHE included 1 patient with malignant hypertension and 5 patients with unilateral optic neuropathies (3 with optic neuritis and 2 with nonarteritic anterior ischemic optic neuropathy). A higher proportion of optic neuropathies was seen in a study of 52 patients with unilateral ONHE presenting to an ophthalmic emergency room in whom the final diagnoses were anterior ischemic optic neuropathy in 27, papillitis in 17, pseudoedema in 2, and papilledema in 3.29
Overall, EPs accurately detected ONHE in 69% of patients in whom ONHE was previously diagnosed but in only 24% of patients when it was not. However, it is important to note that in the FOTO-ED study phase I, the EPs failed to diagnose any cases of ONHE using direct ophthalmoscopy, emphasizing their substantially better performance when nonmydriatic fundus photography was made available to them during their routine ED care.
As expected, the detection of ONHE had implications for patient management and disposition in the ED. Patients with ONHE not only were more frequently imaged but also more often received consultation and hospital admission. The detection of ONHE on ED fundus photography changed the final diagnosis for 10 patients, a majority of whom had isolated headaches that would have otherwise been misdiagnosed.
We analyzed differences in presenting complaints and clinical features in both groups to identify factors predictive of ONHE and found in our multivariable analysis that younger age, acute vision loss as a presenting complaint, and BMI >35 kg/m2 independently predicted the presence of ONHE among these patients in the ED. History of vascular risk factors was less frequent among patients with ONHE, and prior diagnosis of IIH was more common among patients with ONHE. This is consistent with elevated ICP being the most common underlying mechanism of ONHE in our study.
Despite being the first study to the best of our knowledge to systematically look at the presence of ONHE among patients presenting to the ED, our study had limitations. The study was conducted in a tertiary ED that routinely evaluates patients with more severe disease; thus, the prevalence of serious and life-threatening illnesses may be higher than in a community setting. In addition, even though efforts were taken to include all possible patients, our study population was a convenience sample dependent on the availability of study staff to take photographs in the ED.3 However, even if we assume that the patients who could not be enrolled were substantially different, our findings still have important implications for ED patient care.
Our study found that ONHE occurs relatively frequently in patients presenting to the ED with a chief complaint of headache, neurologic deficit, visual loss, or elevated diastolic BP and emphasizes the importance of ocular fundus examination in this group of patients. More widespread availability of nonmydriatic digital cameras will facilitate easier and more frequent ocular fundus examination in patients presenting to the ED and other settings such as general neurology clinics and headache centers.
Glossary
- BMI
body mass index
- BP
blood pressure
- ED
emergency department
- EP
emergency provider
- FOTO-ED
Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department
- GVF
Goldmann manual perimetry
- HVF
Humphrey visual field
- ICP
intracranial pressure
- IIH
idiopathic intracranial hypertension
- IQR
interquartile range
- ONHE
optic nerve head edema
- OP
opening pressure
- OR
odds ratio
Author contributions
Virender Sachdeva: participated in the design of the study, in the collection, analysis, and interpretation of the data, in the statistical analysis, and in the drafting of the manuscript. Caroline Vasseneix: participated in the design of the study, in the collection, analysis, and interpretation of the data. Rabih Hage and Samuel Bidot: participated in the collection and interpretation of the data and in the critical revision of the manuscript. Lindsay C. Clough: participated in the collection and interpretation of the data. David W. Wright: participated in the design of the study, in the analysis and interpretation of the data, and in the critical revision of the manuscript. Nancy J. Newman and Valérie Biousse: participated in the design of the study, in the analysis and interpretation of the data, and in the drafting and critical revision of the manuscript. Beau B. Bruce: participated in the design of the study, in the collection, analysis, and interpretation of the data, in the statistical analysis, and in the drafting and critical revision of the manuscript.
Study funding
This study was supported in part by Research to Prevent Blindness (Department of Ophthalmology), the Philippe Foundation (R. Hage, S. Bidot, and C. Vasseneix), and NIH grants P30-EY006360 (Department of Ophthalmology), K23-EY019341 (B. Bruce), and UL1-RR025008 (V. Biousse).
Disclosure
V. Sachdeva, C. Vasseneix, R. Hage, S. Bidot, and L. Clough report no disclosures relevant to the manuscript. D. Wright has received speaker fees from Emory University School of Medicine, Department of Defense, National Institute of Neurological Disorders and Stroke, European Congress of NeuroRehabilitation, Academy of Multidisciplinary Neurotraumatology, Uniformed Services University of the Health Sciences, Brain Trauma Foundation, and Coulter Foundation; has served as an advisor for Astrocyte Pharmaceuticals Inc (Scientific Advisory Board) and OneMind; and has received grant support from NIH, Department of Defense, National Football League, and Centers for Disease Control and Prevention. Dr. Wright is also on Emory University's patent for the use of progesterone for traumatic brain injury and the DETECT technology. N. Newman is a consultant for Gensight Biologics (France) and Santhera Pharmaceuticals (Switzerland), serves on the Data Safety Monitoring Board for a Quark Pharmaceuticals (Israel) clinical trial, has provided expert testimony on the topic of optic disc edema, and has received research support from NIH grants (R01-089694, P30-EY006360) and Research to Prevent Blindness Lew R. Wasserman Merit Award. V. Biousse is a consultant for Gensight Biologics (France), received research support from the NIH/Public Health Service (P30-EY006360), NIH (R01-NS089694), and Research to Prevent Blindness. B. Bruce served as a consultant for MedImmune (Data Safety and Monitoring Board) and Bayer (medicolegal), has provided expert testimony on the topic of optic disc edema, and has received research support via his institution from Teva Pharmaceuticals, Pfizer, Novartis, and the NIH (P30-EY006360, R01-NS089694). Go to Neurology.org/N for full disclosures.
References
- 1.Hainer BL, Matheson EM. Approach to acute headache in adults. Am Fam Physician 2013;87:682–687. [PubMed] [Google Scholar]
- 2.Locker TE, Thompson C, Rylance J, Mason SM. The utility of clinical features in patients presenting with nontraumatic headache: an investigation of adult patients attending an emergency department. Headache 2006;46:954–961. [DOI] [PubMed] [Google Scholar]
- 3.Bruce BB, Lamirel C, Wright DW, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med 2011;364:387–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruce BB, Lamirel C, Biousse V, et al. Feasibility of non-mydriatic ocular fundus photography in the emergency department: phase I of the FOTO-ED study. Acad Emerg Med 2011:18:928–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruce BB, Thulasi P, Fraser CL, et al. Diagnostic accuracy and use of non-mydriatic ocular fundus photography by emergency department physicians: phase II of the FOTO-ED study. Ann Emerg Med 2013:62:28–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thulasi P, Fraser CL, Biousse V, Wright DW, Newman NJ, Bruce BB. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology 2013;80:432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bruce BB, Bidot S, Hage R, et al. Fundus photography vs. Ophthalmoscopy Outcomes in the Emergency Department (FOTO-ED) Phase III: web-based, in-service training of emergency providers. Neuro-Ophthalmology (in press, 2018). [DOI] [PMC free article] [PubMed]
- 8.Biousse V, Bruce BB, Newman NJ. Ophthalmoscopy in the 21st century: the 2017 H. Houston Merritt Lecture. Neurology 2018;90:167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lamirel C, Bruce BB, Wright DW, et al. Quality of nonmydriatic digital fundus photography obtained by nurse practitioners in the emergency department: the FOTO-ED study. Ophthalmology 2012;119:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott CJ, Kardon RH, Lee AG, Frisén L, Wall M. Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs. clinical expert assessment using a clinical staging scale. Arch Ophthalmol 2010;128:705–711. [DOI] [PubMed] [Google Scholar]
- 11.Bruce BB, Preechawat P, Newman NJ, Lynn MJ, Biousse V. Racial differences in idiopathic intracranial hypertension. Neurology 2008;70:861–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kleinbaum DG, Klein M. Logistic Regression: A Self-Learning Text, 2nd ed. New York: Springer-Verlag; 2002. [Google Scholar]
- 13.Van Crevel H. Papilledema, CSF pressure, and CSF flow in cerebral tumors. J Neurol Neurosurg Psychiatry 1979;42:493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fahmy JA. Papilledema associated with ruptured intracranial aneurysms. Acta Ophthalmol 1972;50:793–802. [DOI] [PubMed] [Google Scholar]
- 15.Hanna LS, Girgis NI, Yassin MW, et al. Incidence of papilledema and optic atrophy in meningitis. Jpn J Ophthalmol 1981;25:69–73. [Google Scholar]
- 16.Drake RL. Ocular syphilis: III: review of the literature and report of a case of acute syphilitic meningitis and meningoencephalitis with special reference to papilledema. Arch Ophthalmol 1933;9:234–243. [Google Scholar]
- 17.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Care Survey: 2006 emergency department summary. Natl Health Stat Report 2008:1–38. [PubMed] [Google Scholar]
- 18.Fodden DI, Peatfield RC, Milsom PL. Beware the patient with a headache in the accident and emergency department. Arch Emerg Med 1989;6:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramirez-Lassepas M, Espinosa CE, Cicero JJ, Johnston KL, Cipolle RJ, Barber DL. Predictors of intracranial pathologic findings in patients who seek emergency care because of headache. Arch Neurol 1997;54:1506–1509. [DOI] [PubMed] [Google Scholar]
- 20.Lucado J, Paez K, Elixhauaser A. Headaches in U.S. Hospitals and Emergency Departments. 2008: HCUP Statistical Brief No. 111. Rockville: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 21.Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P. Hypertensive urgencies and emergencies: prevalence and clinical presentation. Hypertension 1996;27:144–147. [DOI] [PubMed] [Google Scholar]
- 22.Lip GY, Beevers M, Beevers DG. Complications and survival of 315 patients with malignant-phase hypertension. J Hypertens 1995;13:915–924. [DOI] [PubMed] [Google Scholar]
- 23.Deschamps R, Dehais C, Heran F, et al. Bilateral papilledema. Rev Neurol (Paris) 2008;164:42–46. [DOI] [PubMed] [Google Scholar]
- 24.Koerner JC, Friedman DI. Inpatient and emergency service utilization in patients with idiopathic intracranial hypertension. J Neurophthalmol 2014;34:229–232. [DOI] [PubMed] [Google Scholar]
- 25.Jones JS, Nevai J, Freeman MP, Mcninch DE. Emergency department presentation of idiopathic intracranial hypertension. Am J Emerg Med 1999;17:517–521. [DOI] [PubMed] [Google Scholar]
- 26.Sedwick LA, Burde RM. Unilateral and asymmetric optic disc swelling with intracranial abnormalities. Am J Ophthalmol 1983;96:484–487. [DOI] [PubMed] [Google Scholar]
- 27.Wall M, White WN. Asymmetric papilledema in idiopathic intracranial hypertension: prospective interocular comparison of sensory visual function. Invest Ophthalmol Vis Sci 1998;39:134–142. [PubMed] [Google Scholar]
- 28.Bidot S, Bruce BB, Saindane AM, et al. Asymmetric papilledema in idiopathic intracranial hypertension. J Neuroophthalmol 2015;35:31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tournaire-Marquis E, Rougier MB, Delyfer MN, Korobelnik JF. Unilateral disc edema: retrospective study of fifty-two patients. J Fr Ophthalmol 2012;35:678–683. [DOI] [PubMed] [Google Scholar]


