Introduction
Over 10 million injured children receive care in U.S. emergency departments (EDs) each year. (1) When a child is injured they present to one of three types of medical facilities: non-trauma hospitals (community hospitals), adult trauma centers and pediatric trauma centers. Nearly half of the most critically injured children presenting to community hospitals are transferred to a regional trauma center.(2) Regionalization of care has resulted in improvements in patient outcomes of injured adults and children.(3–5)
The inter-hospital transfer of injured children involves the 1) physical movement of the patient, 2) communication of information (verbal, written, and electronic) between providers and 3) transfer of professional responsibility. This process necessitates collaboration between hospital personnel crossing disciplines (i.e. transport, trauma, emergency medicine, pediatrics, critical care, and administration), and professions (i.e. physicians, registered nurses, and pre-hospital personnel).
Delays and deficiencies during the process of transferring injured children can lead to harm.(6–9) In one study, injured children spent an average of three to five hours undergoing diagnostic testing and treatment prior to being transferred to a trauma center.(10, 11) A subset of these patients had repeated imaging at the trauma center, leading to additional radiation exposure.(12–14) Overall, adverse events occur in up to 50% of transferred children and many of these events are preventable.(12–14)
There is substantial scholarship related to the transfer process of adults within a single hospital (ED to floor) or from hospital to home.(9, 11, 15–17) This literature reports the following as opportunities for improvement: standardization, enhanced communication and increased organizational support.(9, 16, 18, 19) In contrast there are limited data on inter-facility transfers (i.e., hospital to hospital) and no data for injured children.(7) The paucity of work is attributable to the challenges of obtaining data from patients and providers across the transfer continuum.(9) The purpose of this study is to explore inter-professional health care providers’ experiences with the process of transferring injured children and describe strategies for improvement.
Methods
This qualitative study was conducted between February 2013 to December 2014 under the AHRQ-funded Center for Healthcare Innovation, Redesign and Learning (CHIRAL), a research center at Yale tasked with the design and evaluation of interventions aimed at improving patient transitions. The research team recruited and interviewed healthcare providers involved in the clinical care of pediatric trauma patients from six community hospitals in Connecticut and Yale New Haven Children’s Hospital Trauma Program, an American College of Surgeons verified Level I pediatric trauma center with 201 pediatric beds. During the study period, this Level I pediatric trauma center received 324 trauma transfers from community EDs. The Institutional Review Board at Yale University reviewed and exempted this study. We report the following methods and results in accordance with the Consolidated Criteria for Reporting Qualitative Research (COREQ). (20) COREQ is a formal reporting checklist useful for promote complete reporting among researchers and indirectly improve the rigor and comprehensiveness of qualitative methods.
Sampling
Our sampling frame consisted of several types of healthcare providers involved in the pediatric trauma transfer process including: physicians, advanced practice providers, nurses, paramedics, administrative, and executive-level staff. Providers with various healthcare roles were purposively selected from across the continuum of care and interviewed to provide a more inclusive and comprehensive perspective of the pediatric trauma transfer process. There were 18 individuals interviewed from the pediatric trauma center, and 16 individuals interviewed from six community hospitals (Table 1).
Table 1.
Demographics of those Interviewed at Study Hospitals
| Role | N | Total N (34) |
Representing: Pediatric Academic Center (N) | Representing: Community Hospital (N) | |
|---|---|---|---|---|---|
| Frontline Provider | Paramedic/Transport | 5 | 23 | 12 | 11 |
| RN - ED | 6 | ||||
| RN - Transport | 4 | ||||
| Advance Practice Provider - ED | 1 | ||||
| MD - ED | 3 | ||||
| MD - Transport | 1 | ||||
| MD - Trauma Surgery | 3 | ||||
| Administration/Leadership | Managers | 1 | 11 | 6 | 5 |
| Assistant managers | 2 | ||||
| Educators | 2 | ||||
| Coordinators | 3 | ||||
| Directors of Departments | 2 | ||||
| Executive level staff | 1 | ||||
Recruitment
Healthcare providers who had recently participated in the transfer process of an injured child were recruited in-person and via email to assess their interest in participating in the study. For the individuals who agreed to participate in the study a telephone or in-person interview was conducted. At the conclusion of the interview, providers were asked for referrals of colleagues with experience transfer process of an injured child. Recruitment continued until researchers reached a point in the analysis of the data that sampling more data would no longer lead to new information related to the study, this is also known as reaching theoretical data saturation.
Interview Procedures
Three researchers experienced in qualitative interviewing conducted a total of 26 interviews. Based on the respondent’s preference and availability, interviews were conducted either by telephone or in-person. All interviews were semi-structured, with pre-written probes that could be tailored based on question responses. Interview questions focused on the provider’s role and perceptions of the pediatric trauma transfer process. Examples of interview questions and probes are provided in Table 2. Interviews were audio recorded using a handheld device and then transcribed verbatim by a professional medical transcription service.
Table 2.
Examples of Interview Questions and Probes
| Question | Probe |
|---|---|
| Can you tell me about your role in pediatric trauma transfers? |
|
| What aspects of the pediatric trauma transfer process currently go smoothly? |
|
| What aspects of the pediatric trauma transfer process have been challenging? |
|
Data analysis
The constant comparative method was employed, comparing coded units to each other within and across coding categories over successive interviews.(21) The constant comparative approach was employed to generate theories and commonalities to explain the transfer process and ideas for improvement. Line-by-line review of the transcripts was conducted first independently and then jointly to develop the coding key; discrepancies were resolved by discussion. The analytic process was continued until no new concepts emerged and data saturation was achieved, resulting in the final code key. The final code key was reapplied to all transcripts. Data reports were then created and analyzed for individual codes and code categories. These evolved into principal themes and sub-themes. Data collection and analytic rigor was upheld with written interview instructions, interview question guides, and formal coding procedures. Members of the research team met weekly to review the interview and coding process. Finally, data collection and trustworthiness was facilitated by data triangulation and through vetting findings with experts in pediatric emergency medicine as well as study participants. ATLAS.ti 7 qualitative software (Scientific Software, Berlin, Germany) was used for data coding, organization, and retrieval.
Results
Thirty-four individuals in various roles participated in the 26 interviews. A breakdown of participant demographics is provided in Table 1. The mean length of the interviews was 20 minutes. Figure 2 describes the Connecticut Pediatric Trauma Transfer Process and provides the foundation for subsequent process refinement.
Figure 2.
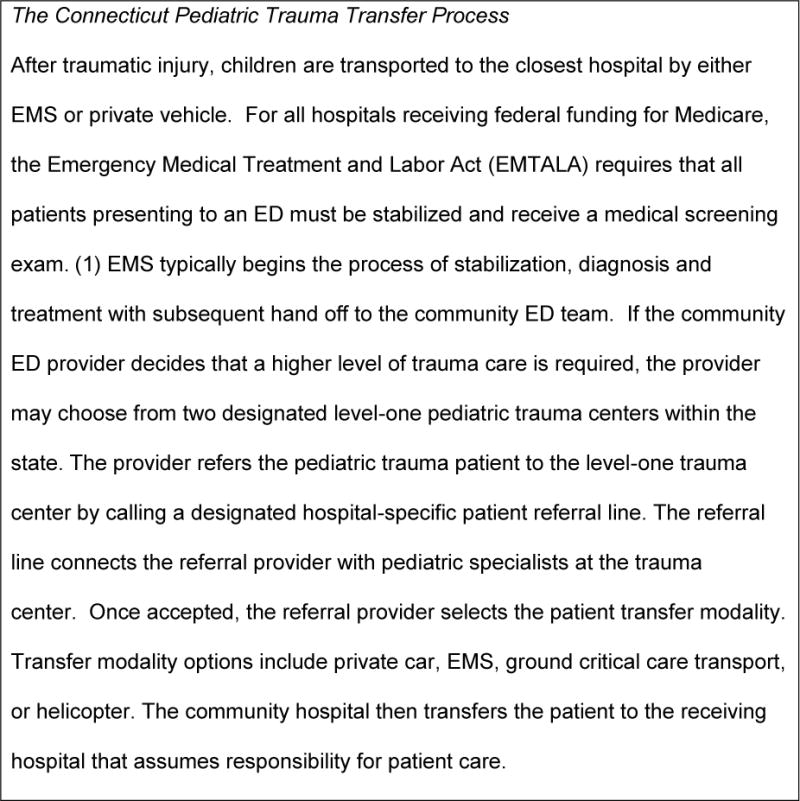
Transfer Process
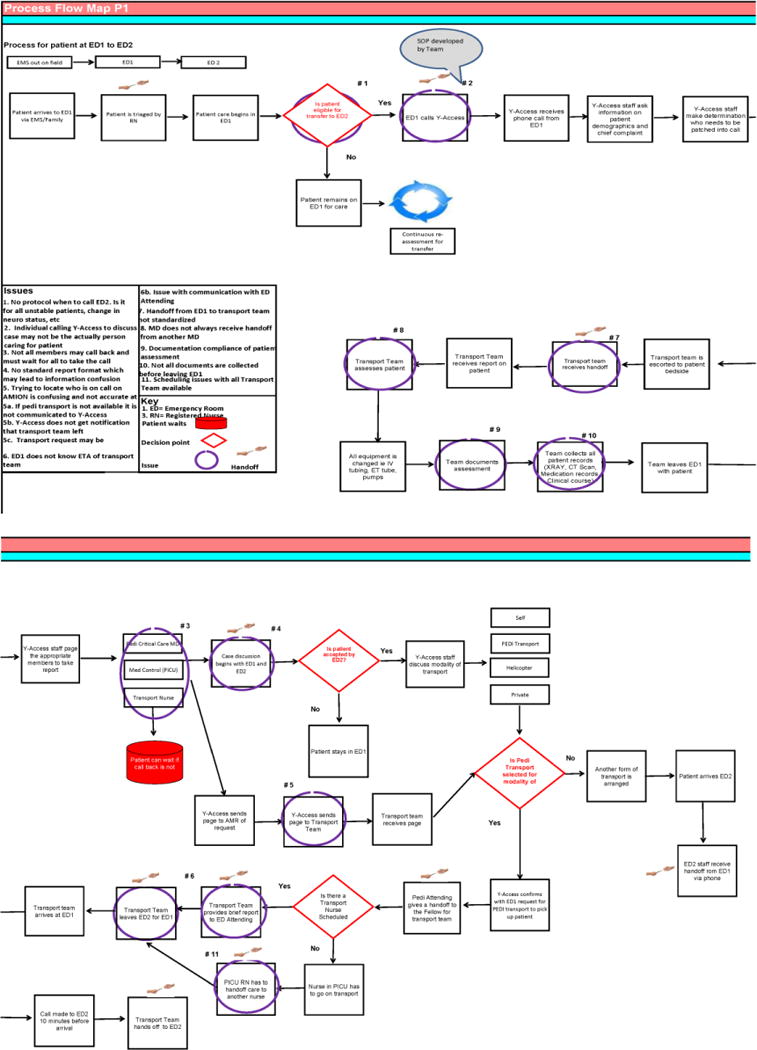
A process map (Figures 1) was created based on the providers’ perspectives and observations. This map describes the physical movement of the patient from the scene of injury through the CED and subsequent transfer to the PED. Indicators on this map identify points of necessary communication between providers. Eleven points of communication identified by participants as potentially problematic are highlighted on this map. Supplementary digital content is provided that uses swim-lane diagrams to provide the process from the perspective of the healthcare providers (Supplemental Fig 1).
Figure 1. Process Map.
Main Themes and Sub-themes
Five primary themes and sub-themes were identified as areas to improve the transfer process (Table 3). These themes may represent opportunities for future process improvement.
Table 3.
Themes and subthemes
| Main Theme | Subthemes |
|---|---|
| Standard Operating Procedure |
|
| Confidence |
|
| Organization/Physical Environment |
|
| Institutional Relationships |
|
| Shared sense making |
|
1) Creation of Standard Operating Procedure
Standard operating procedures (SOPs) were conceptualized as written documents describing the expected processes of care. This theme comprised three key subthemes, including: availability of SOPs, awareness of SOPs, and integration of SOPs into clinical practice.
Availability: Both transferring and receiving hospitals had a shared perspective regarding the importance of facilitating appropriate transfers of care. This idea was also extended to processes of care for certain pediatric patients, as illustrated by this quote from a Registered Nurse working in a CED: “Is some way we could come up with [a] protocol. Just [to ensure] that there’s some understanding that these patients are going out and what needs to be done.”
Awareness of SOP: The development of SOPs was often the result of previous failures, as illustrated below by a paramedic who was involved in the development of a new protocol to address a specific patient condition: “We determined that there [are] just a lot of things a single paramedic is tasked to do with a pediatric cardiac arrest. We changed that model… to put two paramedics on, it was not only the right thing to do, but is our protocol now.”
Integration: This subtheme refers to the factors that help to facilitate the incorporation of SOPs into clinical practice. Having the same knowledge of the patient condition expedited SOPs, which was often predicated on open lines of communication. This is exemplified by an ED Assistant Manager from a PED: “We went to [another] Children’s Hospital recently and saw how they take transfers. It was very interesting ‘cause we actually stood next to somebody taking a transfer and how she was taught to word things was very clear and not demanding.” Nonetheless, several interviewees indicated that patient acuity complicated the implementation and integration of SOPs into clinical practice, despite best communication efforts.
2) Enhancing Shared Sense Making
Shared sense making is conceptualized as the thought of having attunement among members of a care team in which awareness, understanding, and agreement of a patient’s clinical status, interventions needed, and plan of care is achieved. This is a collaborative thought process in which the sharing of information, perceptions and decision-making is achieved through direct communication between providers. For example, one pediatric emergency fellow stated: [transitions are] most smooth when we get a clear doctor to doctor sign-out from the sending hospital and there’s good communication of what’s actually happening.”
Conversely, the opportunity for shared sense making is lost when poor communication skills are practiced between providers. For example, a PED attending reported on the hand-off of a specific case: “…there was no formal report. There was not a debrief or a sign out. They were just sort of giving little snippets of information like they didn’t have an organized process around it”. Community and receiving providers both acknowledged that poor communication hindered the transfer process and the ability to achieve sense making amongst providers. The use of poor communication during handoff was illustrated by a PED manager, who stated: “most problems have some kind of communication as the root of the problem, so whether it was early notification, the right people notified, the right people being here when the patient comes in, delays in getting people here because someone heard it was one thing and it was actually something else.”
Both community and receiving hospital providers perceived that having shared sense making related to patient care ultimately had a positive impact on the overall outcome of the patient. The receiving hospital utilizes a 24-hour access service call line that facilitates direct physician to physician contact, as well as coordination of air or ground transport if needed. Reaching the appropriate individual to contact for the transfer was perceived as vital, and access to this “one-stop shopping” phone line, was commented on as being a useful tool by multiple providers. A CED physician noted: “the transfer line has just made our lives so much easier overall. You get in touch with the right person right away.” Shared sense making through communication with the receiving provider was perceived as vital as illustrated by a community attending: “talking to the provider is important because you can actually explicitly tell that person who’s going to be caring for that patient [and] your thought processes”.
3) Improving Provider Confidence, Expertise, and Skills
Participants pointed to the importance of provider confidence in handling complex medical cases for the sending, receiving, and transporting teams. Confidence was viewed as being tied to skills and expertise, clinical experience, and trust. A key assumption for any pediatric transfer was the rationale for the transfer from a community hospital to a pediatric trauma center. Most participants felt that receiving providers at the children’s hospital held specialized skills, expertise, or resources that the transferring providers did not have. Similarly, interviewees recognized different expertise and skill sets needed for each aspect of the transfer (sender, receiver, transporter), and pinpointed areas of improvement needed within each area. Clinical experience in pediatric cases was perceived as invaluable yet difficult to gain given the relative rarity of pediatric traumas.
Since critically injured pediatric cases occurs infrequently, obtaining and maintaining competency in caring for these children in the community may be challenging. A PED manager stated: “You can’t get confidence without…clinical experience. Pediatric clinical experience is hard to come by because they are much rarer”. Training was perceived as adding limited value when it comes to engendering confidence. To achieve confidence in action, participants thought that providers must be clear about their roles. This theme reverberated in community, transport, and receiving hospital settings, as illustrated by one receiving hospital PED attending: “When someone feels confident that…all those roles are well established and people jump into them and are well trained in them…the training has helped in that people know what they’re supposed to be doing”. Similarly, a pediatric surgical attending demonstrated the value of trusting each other and how this facilitates multidisciplinary teamwork: “Big trauma requires a lot of layered care, everyone, to a certain extent, has to be comfortable doing their job and forgetting about every other job…”
4) Addressing Organization/Physical Environment
The organizational and physical environments relate to the interactions between providers and other structural or environmental elements of the transfer system that may hinder or optimize the transfer process. Providers must determine the most efficient and safest way of transferring an ill or injured patient from one hospital to another. As one community paramedic explained, “There’s a decision [regarding modality] between the physicians. Whoever’s [sending] and whoever’s receiving? I think those elements need to continue to take place“.
With each modality method, including helicopter or ground, unpredictable factors were identified that could impede timeliness; for example, weather or traffic can hinder the arrival of the transport team to the patient or to definitive care. As one paramedic stated “[it is] hard to factor in traffic, any unforeseen circumstances could [cause a] delay”. As for air transport, harsh weather conditions or lack of a transferring facility helipad will impact the decision to use the helicopter. These delays may ultimately cause further harm to the pediatric patient. These factors were perceived to impact overall patient care, as many providers mentioned that having a global awareness of other activities going on in the department is critical for a successful transfer to occur.
5) Fostering Institutional Relationships
Institutional relationships between community emergency departments, the pediatric trauma center, and transport team members were seen as key to successful transfers. High quality institutional relationships were those in which “institutions come together for the benefit of the program and the patient.” Institutional relationships were described as varying in strength and positivity. The strength of the relationship between institutions was perceived to be based on the number and proportion of trauma cases that the community hospital transfers to the receiving hospital. This appeared to be tied to proximity, duration of the relationship, and shared affiliation. A surgeon at the children’s hospital referenced the impact of institutional affiliation in discussing transfers from a recently affiliated community hospital: “Some of the ED physicians like at CED X seem to be doing a lot more referrals now, ‘cause they’re sort of our people in a way. They’re very helpful…” Other factors that affected the intensity of institutional relationships included having access to shared electronic medical records and other technology platforms used for reviewing test and imaging results. Additionally, the perceived ease of connecting to centralized referral dispatch centers, shared expertise, training, and resources all added to improved institutional relationships.
Perceptions of the pediatric trauma center’s respect of community partners were discussed in the context of improvement over time. A paramedic stated: “At one point in time I don’t think that the in-hospital staff knew what we did…For the past seven or ten years, I feel everybody has an idea of what we do and what we are capable of and there is actually mutual respect there.” Community partners expressed confidence and respect for the receiving hospital providers, often referring to them as experts. An educator in a community hospital stated: “[our staff] got the confidence that the patient left with a competent team.” Receiving institution nurses were consistently praised for seeking appropriate information. The receiving hospital appreciated the respect afforded to them by community partners for the most part, but were occasionally met with resistance, as illustrated by one PED nurse: “I think the outlying places are a little reluctant to take our advice. I realize they’re very good at what they do, too. I’m not trying to tell them how to run their show, but I think there could be some improvements with our advice being a little bit better received.” Positive and close institutional relationships facilitated timely and honest feedback on pediatric transfer cases from the receiving center to community partners, and vice versa. A CED Educator states: “I have contacts at [receiving hospital]. I can call over and say, ‘This is just a bump on our end.’ Just so that it doesn’t happen in the future. I think just making those community connects really helps because we’re very dependent on all of our [partners].”
The absence of strong, positive institutional relationships was perceived to jeopardize patient care. One example given was potential delays in initial contact from CED to receiving hospital based on previous negative interactions. A leader from the pediatric trauma center stated: “If you’ve had a physician who is the expert treat you pretty badly in an outlying emergency department, they don’t really wanna…call you again and send their patients there.”
Discussion
The care of injured children was perceived as a complex and dynamic process that involves providers from diverse disciplines across a continuum of care. This qualitative study identified five target areas for improvement in the pediatric transfer process: the use of standard operating procedures, shared sense making, provider confidence, expertise, skills and experience, organization and environmental factors, and institutional relationships.
Providers identified the need for available, transparent, and integrated SOPs in the care of pediatric trauma patients. SOPs could provide structure around who to transfer and how to transfer patients in a predictable and safe manner. Availability of SOPs refers to whether or not guidelines, protocols, and policies are available or exist to facilitate high quality of care. The creation of an SOP for communication practices was expressed as an opportunity for more efficient and higher quality of care. Regionalization of trauma care and existing inter-facility transfer agreements provide the framework for the creation of a single set of SOPs that could be used across institutions in a region. The American College of Surgeons (ACS) provides guidance on selecting the modality of transfer (ground vs air) and team composition. These processes initially were developed as a part of the Emergency Medical Treatment and Labor Act (EMTALA) but now focus on ensuring safe and smooth transitions of care. While these processes are often well described, the work that is performed daily on the front lines by healthcare providers is not always the work that is “imagined” in these policies. Having representatives from transferring facilities, accepting facilities and transport teams working collaboratively to create, evaluate and update cross-institutional SOPs could help to ensure that they are applied to daily practice.
Providers agreed that making community connections are beneficial to the provider teams and the patient. Relationships may occur after a single interaction between providers, or may be the result of a history of interactions among providers. Exploring the degree to which relationships can be improved is one method to increase shared sense making. Relationships were discussed in terms of the level of positivity that interactions between two institutions typically engendered. Levels of teamwork, trust, empathy, collegiality, and respect varied. All members involved in the transfer process including the pediatric trauma center, transport team, and CED expressed the importance of internal teamwork and quality of care. Shared thinking may be facilitated by these relationships through the development of respect and trust. Promoting the cultivation of sense making through each encounter can also be facilitated through the use of tools, decision support technology including a referral line, and other aids that promote deliberation in the context of forming and promoting relationships.(22)
Similarities and differences were explored in provider confidence, skills, expertise and experience involved in the transfer process. Participants from community hospitals discussed an insecurity that arises from lack of experience in caring for pediatric trauma patients. While training was not seen as a panacea, there were specific areas that were thought to be amenable to improvement with education. Many of these were procedural, such as the best way to report, to prepare the patient, to organize documentation and imaging, and to standardize pediatric transfer criteria. Participants believed that collaboration could be enhanced through the use of simulation to increase the frequency of exposure to these patients as well as other forms of team building. Providing constructive, non-confrontational and timely feedback or debriefing on a regular basis between the transferring and receiving institutions can serve to facilitate the development of relationships and thus positively impact patient care.
When transferring a trauma patient, the flow of information often involves the creation of a mental model by the referring care team that is then communicated to the receiving team. This is often accomplished through parallel dialogues within each profession (i.e. MD to MD, RN to RN). Although each team member is responsible for different aspects of the patient’s care, these parallel hand-offs may impede the development of a collective shared mental model among all care providers. Communicating this large volume of data is necessary, but may not be effectively accomplished in silos. Nonetheless, clear and explicit communication methods, such as provider phone conferences, would be fairly easy to implement in practice.
While adequate communication is key to effective inter-facility transfers, it is not the only component necessary. Providers are communicating with each other in complex organizational and environmental systems that are not well designed. Many factors were identified which could potentially affect the timeliness of patients arriving to definitive care. Systems problems during inter-facility transfers are associated with adverse events exposing patients to harm.(23) For example, many transferring hospitals will perform imaging or lab tests to “screen” patients, especially if the transfer process is expected to be time-consuming and/or delayed. These tests are often unnecessarily repeated at the receiving hospital which may causes unnecessary pain, anxiety, and cost.(24) Other transfer-associated adverse events include airway events, cardiopulmonary arrest, equipment failure, hypertension, hypotension, loss of intravenous access, and medication error.(6)
This is the first qualitative study examining inter-professional providers’ experiences with the transfer process for injured children and strategies for improvement. We were able to gather information from clinicians with a broad range of clinical experience, all of whom had cared directly for pediatric patients who underwent a transfer. Nonetheless, the results from this study must be interpreted in the context of the following biases and limitations. There may be a bias in the approach of recruiting patients that was used in the study including in-person recruitment and referrals from recruited participants, which may have influenced the results and therefore the conclusions of the work. Additionally, this study included the evaluation of a single trauma care system in one geographical setting, which may limit the generalizability of the findings. Lastly, a geographically narrow approach to participant identification was had, requiring further investigation for the application of these findings outside of the representative trauma care system. Future work is also needed to engage family members or patients who are key stakeholders in the transfer process. There is limited work to date that includes information and perspectives from families and patients that would be beneficial to the improvement of the trauma transfer process.
Conclusion
This study highlights the complex combination of clinical, interpersonal, and organizational challenges faced by providers caring for injured children. Interventions and ideas to improve the transfer process include those that utilize standard operating procedures, shared sense making, improving provider confidence, expertise, skills and experience, address organization and environmental factors, and improve institutional relationships. Using information based from this study may assist hospitals to improve the transfer process of injured pediatric patients.
Supplementary Material
Acknowledgments
Funding Source: This work was conducted under the Yale Center for Healthcare Innovation, Redesign and Learning and funded by the Agency for HealthCare Research and Design, AHRQ Grant No: HS23554, Project Period: 09/30/14-09/29/18
Abbreviations
- PED
pediatric emergency department
- CED
community emergency department
- SOPs
Standard operating procedures.
Footnotes
Conflict of Interest: None
References
- 1.CDC. [Available from: http://www.cdc.gov/safechild/Child_Injury_Data.html.
- 2.Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care. 2011;49(6):592–8. doi: 10.1097/MLR.0b013e31820fb71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mullins RJ, Mann NC, Hedges JR, Worrall W, Jurkovich GJ. Preferential benefit of implementation of a statewide trauma system in one of two adjacent states. Journal of Trauma-Injury Infection & Critical Care. 44(4):609–16. doi: 10.1097/00005373-199804000-00009. discussion 17. [DOI] [PubMed] [Google Scholar]
- 4.Newgard CD, McConnell KJ, Hedges JR, Mullins RJ. The benefit of higher level of care transfer of injured patients from nontertiary hospital emergency departments. Journal of Trauma-Injury Infection & Critical Care. 63(5):965–71. doi: 10.1097/TA.0b013e31803c5665. [DOI] [PubMed] [Google Scholar]
- 5.Sampalis JS, Denis R, Lavoie A, Frechette P, Boukas S, Nikolis A, et al. Trauma care regionalization: a process-outcome evaluation. Journal of Trauma-Injury Infection & Critical Care. 46(4):565–79. doi: 10.1097/00005373-199904000-00004. discussion 79–81. [DOI] [PubMed] [Google Scholar]
- 6.Barry PW, Ralston C. Adverse events occurring during interhospital transfer of the critically ill. Archives of disease in childhood. 1994;71(1):8–11. doi: 10.1136/adc.71.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Droogh JM, Smit M, Hut J, de Vos R, Ligtenberg JJ, Zijlstra JG. Inter-hospital transport of critically ill patients; expect surprises. Critical Care (London, England) 16(1):R26. doi: 10.1186/cc11191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hunt EA, Heine M, Hohenhaus SM, Luo X, Frush KS. Simulated pediatric trauma team management: assessment of an educational intervention. Pediatr Emerg Care. 2007;23(11):796–804. doi: 10.1097/PEC.0b013e31815a0653. [DOI] [PubMed] [Google Scholar]
- 9.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 297(8):831–41. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 10.Mowery NT, Dougherty SD, Hildreth AN, Holmes JHt, Chang MC, Martin RS, et al. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. Journal of Trauma-Injury Infection & Critical Care. 70(6):1317–25. doi: 10.1097/TA.0b013e3182175199. [DOI] [PubMed] [Google Scholar]
- 11.Sampalis JS, Denis R, Frechette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. Journal of Trauma-Injury Infection & Critical Care. 43(2):288–95. doi: 10.1097/00005373-199708000-00014. discussion 95–6. [DOI] [PubMed] [Google Scholar]
- 12.Cook SH, Fielding JR, Phillips JD. Repeat abdominal computed tomography scans after pediatric blunt abdominal trauma: missed injuries, extra costs, and unnecessary radiation exposure. Journal of pediatric surgery. 2010;45(10):2019–24. doi: 10.1016/j.jpedsurg.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Stewart BA, Fernandes S, Rodriguez-Huertas E, Landzberg M. A preliminary look at duplicate testing associated with lack of electronic health record interoperability for transferred patients. Journal of the American Medical Informatics Association : JAMIA. 2010;17(3):341–4. doi: 10.1136/jamia.2009.001750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA pediatrics. 2013;167(8):700–7. doi: 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. Journal of Hospital Medicine (Online) 2(5):314–23. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 16.Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: A systematic review and task force recommendations. Journal of Hospital Medicine. 2009;4(7):433–40. doi: 10.1002/jhm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fried MJ, Bruce J, Colquhoun R, Smith G. Inter-hospital transfers of acutely ill adults in Scotland. Anaesthesia. 65(2):136–44. doi: 10.1111/j.1365-2044.2009.06165.x. [DOI] [PubMed] [Google Scholar]
- 18.Riesenberg LA, Leisch J, Cunningham JM. Nursing handoffs: A systematic review of the literature. American Journal of Nursing. 2010;110(4):24–34. doi: 10.1097/01.NAJ.0000370154.79857.09. [DOI] [PubMed] [Google Scholar]
- 19.Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C, et al. Residents’ and attending physicians’ handoffs: A systematic review of the literature. Academic Medicine. 2009;84(12):1775–87. doi: 10.1097/ACM.0b013e3181bf51a6. [DOI] [PubMed] [Google Scholar]
- 20.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 21.Birks M, Mills J. Grounded theory: a practical guide. Los Angeles, Calif: Sage; 2011. p. 210. [Google Scholar]
- 22.Sutcliffe KMWK. Organizing and the Process of Sensemaking. Organization Science. 2005;16(4):409–21. [Google Scholar]
- 23.Ong MS, Coiera E. A systematic review of failures in handoff communication during intrahospital transfers. Jt Comm J Qual Patient Saf. 2011;37(6):274–84. doi: 10.1016/s1553-7250(11)37035-3. [DOI] [PubMed] [Google Scholar]
- 24.Jones AC, Woldemikael D, Fisher T, Hobbs GR, Prud’homme BJ, Bal GK. Repeated computed tomographic scans in transferred trauma patients: Indications, costs, and radiation exposure. The journal of trauma and acute care surgery. 2012;73(6):1564–9. doi: 10.1097/TA.0b013e31826fc85f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


